Abstract
A real-time PCR assay, BurkDiff, was designed to target a unique conserved region in the B. pseudomallei and B. mallei genomes containing a SNP that differentiates the two species. Sensitivity and specificity were assessed by screening BurkDiff across 469 isolates of B. pseudomallei, 49 isolates of B. mallei, and 390 isolates of clinically relevant non-target species. Concordance of results with traditional speciation methods and no cross-reactivity to non-target species show BurkDiff is a robust, highly validated assay for the detection and differentiation of B. pseudomallei and B. mallei.
Introduction
The bacterial species Burkholderia pseudomallei and B. mallei, though genetically very similar, have divergent lifestyles. B. pseudomallei is a soil saprophyte and facultative pathogen and the cause of melioidosis, while B. mallei is an obligate pathogen and the cause of glanders. Melioidosis is mostly a disease of humans and animals in Southeast Asia and Northern Australia, where B. pseudomallei is present in the environment; infection mainly results from percutaneous inoculation or inhalation or aspiration of the organism. Clinical manifestations of melioidosis can be asymptomatic, localized to virtually any organ, or disseminated, though the primary presentations are pneumonia and sepsis, where mortality rates are significant [1], [2]. Glanders is mainly an equine disease found in much of the world, except for North America, Europe and Australia, with transmission to humans occurring primarily through direct contact with animals and aerosols [3], [4]. Clinical manifestations of glanders in humans are similar to those of melioidosis [1], [5]. Both species of bacteria cause fast-progressing diseases and both are intrinsically resistant to several antibiotics. As such, the rapid detection and identification of these species is essential for immediate appropriate patient therapy. Both species are also potential bioterrorism agents, deemed by the U.S. Centers for Disease Control and Prevention Category B Select Agents [6], for which no human vaccine is available. In this context, rapid differentiation of melioidosis and human glanders is paramount for epidemiological surveillance and forensic investigation.
Identification of B. pseudomallei and B. mallei and the diagnosis of melioidosis and glanders currently depend on time-consuming culture of the organism. Confirmation by biochemical assays can add a week onto definitive species identification [1]. Rapid biochemical assays have resulted in misdiagnosis of melioidosis, a mistake not easily detected due to the myriad clinical manifestations of the disease, and the lack of vigilance for these organisms in non-endemic regions [7], [8]. Serologic assays can be erroneous [8], are contingent on a delayed immune response, and are useful really only in non-endemic areas, where seroconversion due to previous exposure is improbable [1]. Antigen-specific assays, including direct immunofluorescent microscopy [9] and latex agglutination [10], have proven to be rapid and sensitive, but are not as yet available commercially.
Molecular methods to identify B. pseudomallei and B. mallei now exist that utilize various platforms: Sanger sequencing [11], multiplex PCR [12], real-time PCR [13], [14], [15], [16], and isothermal DNA amplification [17]. Several of these assays show promise as rapid alternatives to biochemical tests; however few have been extensively validated for robustness and specificity. B. pseudomallei and B. mallei are relatively genetically promiscuous, making development of robust, specific single-locus assay diagnostics challenging [18], [19].
A single-reaction real-time PCR Taqman allelic discrimination assay was previously developed to identify and differentiate B. pseudomallei and B. mallei [20]. Further analysis of this assay against larger strain collections revealed some false positive identification: a strain of B. oklahomensis types as B. pseudomallei, and the B. thailandensis-like strain MSMB43 types as B. mallei (unpublished data).
Here we introduce a new more highly validated allelic discrimination assay, referred to as BurkDiff, to provide a higher level of specificity for accurate identification of B. pseudomallei and B. mallei and simultaneous differentiation when necessary. Alternatively, as these two species often occupy disparate niches under normal circumstances, BurkDiff can be used as a single-probe assay for definitive identification of B. pseudomallei or B. mallei.
Methods
We used the methods described by Pearson et al. [21] to compare 23 B. pseudomallei and 10 B. mallei genomes to search for shared orthologous SNPs, then filtered them by mismatch value (the distance to the next SNP in bases). We further analyzed the resultant pool of SNPs and their flanking regions with a GenBank BLAST search, and finally chose one for assay development and validation.
Using Primer Express 3.0 software (Life Technologies, Foster City, CA), we designed a Taqman SNP dual-probe allelic discrimination assay in which one probe was designed to hybridize with the B. mallei allele (5′-FAM-CTGAAACGCGCAGCG-3′-MGB) and the other to the B. pseudomallei allele (5′-VIC-CTGAAACGCGAAGCG-3′-MGB). Real-time PCR was carried out in 10 uL reactions containing 900 nM of both forward (5′-CGAGCGCATCGTACTCGTA-3′) and reverse (5′- CAAGTCGTGGATGCGCATTA-3′) primers, 200 nM of each probe, 1X Applied Biosystems Genotyping Mastermix, and 0.5 ng template. Thermal cycling and endpoint analysis was performed on an AB 7900HT sequence detection system (Life Technologies) using the following conditions: 50°C for 2 min, 95°C for 10 min, and 40 cycles of 95°C for 15 s and 58°C for 1 min.
To evaluate the utility of this SNP and its locus as a diagnostic marker for B. pseudomallei and B. mallei, we used the Taqman allelic discrimination assay to genotype a collection of human, animal, and environmental isolates of B. pseudomallei (n = 469) and B. mallei (n = 49) from a broad geographic range (Table 1). Additionally we assessed specificity by screening isolates of near-neighbor species (n = 62), and isolates of species of similar clinical presentation or normal flora (n = 328) (Table 2). All isolates were originally identified by standard microbiological techniques in the laboratory of origin.
Table 1. Number and origin of B. pseudomallei, B. mallei, and genetic near-neighbor strains used in this study.
| Species | Country | Isolated from | No. of isolates | TaqMan result (SNP state) |
| B. mallei | China | Human | 2 | C |
| China | Animal | 4 | C | |
| China | Unknown | 2 | C | |
| France | Unknown | 1 | C | |
| Hungary | Animal | 1 | C | |
| Hungary | Unknown | 1 | C | |
| India | Animal | 3 | C | |
| India | Unknown | 1 | C | |
| Pakistan | Unknown | 6 | C | |
| Turkey | Human | 4 | C | |
| Turkey | Animal | 1 | C | |
| Turkey | Unknown | 10 | C | |
| UK | Unknown | 1 | C | |
| USA | Human | 4 | C | |
| USA | Animal | 1 | C | |
| USA | Unknown | 3 | C | |
| Unknown | Animal | 2 | C | |
| Unknown | Unknown | 2 | C | |
| Total | 8 | 49 | ||
| B. pseudomallei | Australia | Human | 131 | A |
| Australia | Animal | 10 | A | |
| Australia | Environmental | 57 | A | |
| Australia | Unknown | 6 | A | |
| Bangladesh | Human | 2 | A | |
| Cambodia | Unknown | 2 | A | |
| China | Unknown | 3 | A | |
| Ecuador | Human | 2 | A | |
| Ecuador | Animal | 1 | A | |
| Fiji | Human | 1 | A | |
| India | Unknown | 1 | A | |
| Indonesia | Environmental | 1 | A | |
| Kenya | Human | 1 | A | |
| Kenya | Environmental | 2 | A | |
| Laos | Unknown | 2 | A | |
| Madagascar | Environmental | 2 | A | |
| Malaysia | Human | 2 | A | |
| Malaysia | Environmental | 3 | A | |
| Malaysia | Unknown | 15 | A | |
| Mauritius | Human | 1 | A | |
| Pakistan | Human | 2 | A | |
| Papua New Guinea | Human | 1 | A | |
| Papua New Guinea | Unknown | 1 | A | |
| Puerto Rico | Human | 2 | A | |
| Singapore | Human | 2 | A | |
| Singapore | Environmental | 1 | A | |
| Sweden | Human | 1 | A | |
| Thailand | Human | 89 | A | |
| Thailand | Environmental | 105 | A | |
| Unknown | Human | 1 | A | |
| Unknown | Environmental | 2 | A | |
| Unknown | Unknown | 2 | A | |
| USA | Human | 6 | A | |
| Venezuela | Human | 1 | A | |
| Vietnam | Human | 4 | A | |
| Vietnam | Animal | 1 | A | |
| Vietnam | Unknown | 3 | A | |
| Total | 22 | 469 | ||
| B. cepacia | USA | 2 | Negative | |
| B. oklahomensis | USA | 2 | Negative | |
| B. thailandensis | 58 | Negative | ||
| Total | 62 |
Table 2. Species and number of differential diagnostic and background flora strains screened across BurkDiff to validate the assay's specificity.
| Species | No. of strains | Species | No. of strains |
| Abiotrophia/Granulicatella grp | 1 | Neisseria gonorrhoeae | 4 |
| Achromobacter xylosoxidans | 1 | Neisseria meningitidis | 3 |
| Acinetobacter baumanni | 7 | Pasteurella multocida | 1 |
| Bacillus anthracis | 1 | Propionibacterium sp. | 1 |
| Bacillus cereus | 1 | Providencia stuartii | 1 |
| Bacillus sp. | 2 | Pseudomonas aeruginosa | 7 |
| Bacteroides fragilis | 1 | Rhizopus oryzae | 1 |
| Bacteroides uniformis | 1 | Rothia mucilaginosa | 1 |
| Bordetella bronchiseptica | 1 | Salmonella enterica | 1 |
| Brucella abortus | 1 | Shigella dysenteriae | 1 |
| Brucella suis | 1 | Staphylococcus arlettae | 1 |
| Candida albicans | 5 | Staphylococcus aureus | 55 |
| Candida glabrata | 2 | Staphylococcus capitis | 1 |
| Candida parapsilosis | 3 | Staphylococcus cohnii | 1 |
| Candida tropicalis | 1 | Staphylococcus epidermidis | 8 |
| Chryseobacterium indologenes | 1 | Staphylococcus equorum | 1 |
| Coagulase negative Staphylococcus | 16 | Staphylococcus gallinarum | 1 |
| Coccidioides immitis | 1 | Staphylococcus haemolyticus | 3 |
| Coccidioides posadasii | 2 | Staphylococcus hominis | 1 |
| Corynebacterium diphtheriae | 1 | Staphylococcus kloosii | 1 |
| Corynebacterium jeikeium | 1 | Staphylococcus lugdunensis | 1 |
| Coxiella burnetii | 2 | Staphylococcus saprophyticus | 2 |
| Enterobacter aerogenes | 2 | Staphylococcus xylosus | 3 |
| Enterobacter cloacae | 10 | Stenotrophomonas maltophilia | 1 |
| Enterococcus faecalis | 9 | Streptococcus agalactiae | 9 |
| Enterococcus faecium | 6 | Streptococcus anginosus | 2 |
| Escherichia coli | 11 | Streptococcus equi | 1 |
| Francisella tularensis | 2 | Streptococcus gordonii | 1 |
| Haemophilus influenzae | 4 | Streptococcus mitis | 2 |
| Haemophilus parainfluenzae | 2 | Streptococcus mutans | 1 |
| Human gDNA | 2 | Streptococcus oralis | 1 |
| Klebsiella oxytoca | 1 | Streptococcus pneumoniae | 56 |
| Klebsiella pneumoniae | 8 | Streptococcus pyogenes | 13 |
| Lactococcus lactis | 1 | Streptococcus salivarius | 2 |
| Legionella pneumophila | 1 | Streptococcus thermophilus | 1 |
| Listeria monocytogenes | 1 | Streptococcus uberis | 1 |
| Micrococcus sp. | 1 | Streptococcus viridans grp | 8 |
| Moraxella catarrhalis | 7 | Vancomycin Resistant Enterococcus | 4 |
| Mycobacterium avium | 1 | Yersinia pestis | 1 |
| Mycoplasma pneumoniae | 1 | Yersinia pseudotuberculosis | 1 |
| Total | 328 |
Out of the 328 strains from approximately 80 species, none amplified.
The limit of detection of the Taqman assay was assessed using a dilution series of DNA from isolates of B. pseudomallei and B. mallei. DNA was quantified using an in-house 16S real-time qPCR assay (unpublished). Template amounts ranging from 106 to 100 genome copies per reaction were used for limit of detection determination.
Results
Genome comparisons revealed 1,235 SNPs with shared character states among all B. mallei genomes that differ from the character state shared by all B. pseudomallei genomes. Filtering the 1,235 SNPs using a mismatch value of 100 resulted in a pool of 74 SNPs. The GenBank BLAST search revealed the exclusivity of one of the regions to B. pseudomallei and B. mallei, so it was selected for assay development and validation.
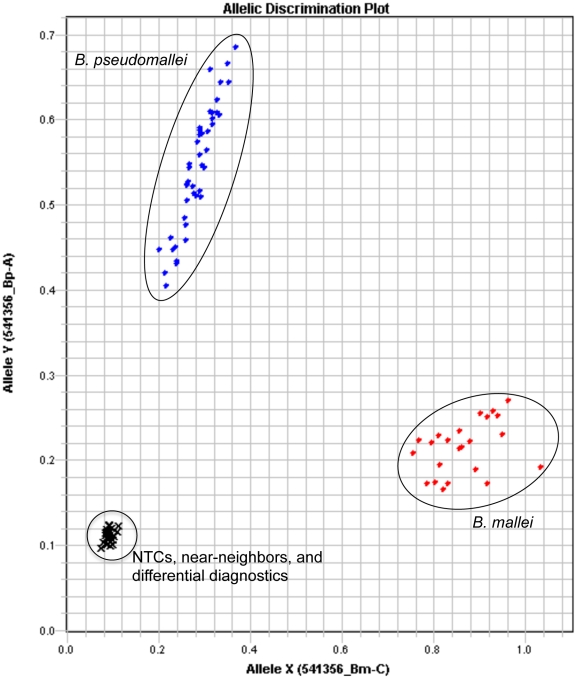
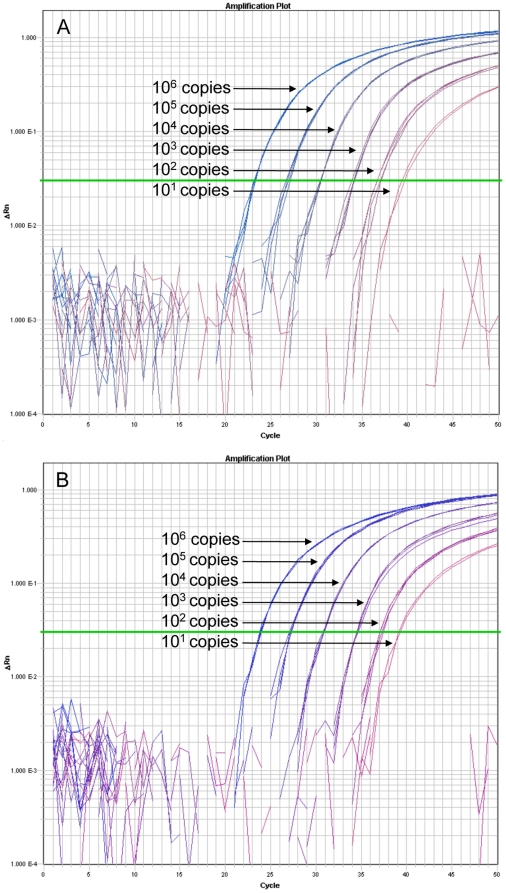
Out of the isolates screened with BurkDiff, all 469 B. pseudomallei strains were shown to contain the allele with the SNP state A, and all 49 B. mallei strains were shown to contain that with the SNP state C (Table 1, Figure 1). No amplification of DNA from the 390 non-target species was detected, including the B. oklahomensis and the B. thailandensis-like strain MSMB43, both of which cross-reacted with a previously published allelic discrimination assay [20]. The limit of detection analysis showed consistent detection and allelic discrimination of B. pseudomallei and B. mallei at DNA template levels as low as 102 genome copies with sporadic amplification and genotyping at <102 genome copies (Figure 2).
Figure 1. BurkDiff allelic discrimination plot.
Results from the assay across 45 B. pseudomallei and 23 B. mallei strains are shown, along with 2 no template controls (NTCs) and 26 near-neighbor and differential diagnostic species.
Figure 2. Amplification plots of BurkDiff.
Quadruplicates of 10-fold serial dilutions of DNA from a crude heat lysis extraction of A. B. mallei strain 2002734303 and B. B. pseudomallei strain 2002721637 were screened on BurkDiff to determine the limit of detection of the assay. Two of 4 replicates at the 101 copies template amount did not amplify for both species.
Discussion
The universality of the clinical manifestations of human melioidosis and glanders precludes patient presentation as a definitive diagnostic for these diseases [3], [22]. Diagnosis by traditional methods can be too time-consuming, or require special equipment [1]. The intrinsic resistance of B. pseudomallei and B. mallei to many widely-used antibiotics and the swift downward progression of untreated or inappropriately-treated B. pseudomallei- and B. mallei-infected patients necessitate the rapid, specific identification of these species in the clinic [1], [3]. The likelihood of infection with B. pseudomallei and B. mallei may not be equal given the circumstances; factors such as geographical distribution, prevalence, and risk factors for the diseases would be used in clinical practice for diagnosis. However there are scenarios in which the two species' distinction is necessary. The trade restrictions imposed when animal glanders is diagnosed, but not animal melioidosis, and the potential use of B. pseudomallei or B. mallei as a bioterrorism agent both underscore the need to differentiate between the two species for reporting purposes and forensic tracking [22], [23]. Rapid species identification may assist with appropriate initial patient treatment for human glanders. Currently physicians prescribe the lengthy drug regimen particular for melioidosis to human glanders patients [3], despite the differing in vitro antibiotic susceptibility profiles of the two causative agents [24]. Of the rapid molecular methodologies with the capabilities of identifying and differentiating between B. pseudomallei and B. mallei, BurkDiff is unique in being single-step, single-reaction. In cases in which circumstances eliminate the possibility of one of the two species, BurkDiff can be used as a single-probe assay for specific identification.
The increasingly cosmopolitan nature of human activity inevitably exposes non-endemic area residents to B. pseudomallei and B. mallei, increasing the need for heightened awareness of these organisms outside their areas of endemicity, as has been demonstrated by numerous cases of imported melioidosis [25], [26]. Most of these cases can be attributed to exposure during travel to tropical areas. However, global trade in commodities such as animals, plants and soils, and food items is also a possible transmission source resulting in disease in individuals with no travel history [27]. Diagnostic capabilities in non-endemic areas are becoming essential, not only for rapid, appropriate patient treatment, but for the safety of laboratory workers culturing the unknown organism for diagnosis [26]. Molecular assays, including BurkDiff, are rapid, sensitive, and specific, requiring only the appropriate thermal cycler and reagents common to many labs and obviating the need for direct culture of a dangerous pathogen. In fact, BurkDiff was successfully used among a panel of real-time assays targeting B. pseudomallei in the confirmation and characterization of a melioidosis case in an Arizona resident with no travel history [27].
Our use of whole genome sequence data allowed for targeted identification of phylogenetically informative markers (i.e., SNPs) to distinguish between B. pseudomallei and B. mallei, a preferred method to random identification of SNPs in conserved genes, as was done previously [20]. Additionally, in silico analyses of the markers allowed for the design of a highly specific assay. The illustrated specificity of BurkDiff to B. pseudomallei and B. mallei suggests that insertion of the genomic region that this assay targets occurred during or subsequent to the B. pseudomallei/B. mallei evolutionary split from its close genetic relative B. thailandensis [28]. Our data also suggest that the SNP targeted by BurkDiff is from a subsequent point mutation that occurred after the B. mallei lineage diverged from B. pseudomallei [28]. The number and diversity of the B. pseudomallei and B. mallei isolates successfully genotyped using BurkDiff suggest the genomic insertion is evolutionarily stable and therefore a good target for identifying the species, while the point mutation could now be considered a canonical SNP (canSNP), a point mutation that marks a point of evolutionary divergence of two taxa and is inherently stable and thus definitive [29].
BurkDiff adds to the growing number of molecular based assays, especially real-time PCR, that have been designed to detect B. pseudomallei and/or B. mallei. Using several of these assays in combination for definitive identification could be important, as the Burkholderiaceae are highly recombining organisms [15], [19], [30], and as more and more strains are uncovered, the robustness and sensitivity of these assays will be challenged.
Acknowledgments
The authors wish to thank Mark Mayo of Menzies School of Health Research for contributing to the Burkholderia strain collection, and Derek Sarovich of Northern Arizona University and Jennifer Nibecker and Craig Asplund of TGen for their help in and out of the laboratory.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This study was supported in part by National Institutes of Health (NIH) grants U01-AI075568 (Keim) and U54-A165359 (Tuanyok). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Cheng AC, Currie BJ. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005;18:383–416. doi: 10.1128/CMR.18.2.383-416.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.White NJ. Melioidosis. Lancet. 2003;361:1715–1722. doi: 10.1016/s0140-6736(03)13374-0. [DOI] [PubMed] [Google Scholar]
- 3.Gilad J. Burkholderia mallei and Burkholderia pseudomallei: the causative micro-organisms of glanders and melioidosis. Recent Pat Antiinfect Drug Discov. 2007;2:233–241. doi: 10.2174/157489107782497335. [DOI] [PubMed] [Google Scholar]
- 4.Srinivasan A, Kraus CN, DeShazer D, Becker PM, Dick JD, et al. Glanders in a military research microbiologist. N Engl J Med. 2001;345:256–258. doi: 10.1056/NEJM200107263450404. [DOI] [PubMed] [Google Scholar]
- 5.Whitlock GC, Estes DM, Torres AG. Glanders: off to the races with Burkholderia mallei. FEMS Microbiol Lett. 2007;277:115–122. doi: 10.1111/j.1574-6968.2007.00949.x. [DOI] [PubMed] [Google Scholar]
- 6.Rotz LD, Khan AS, Lillibridge SR, Ostroff SM, Hughes JM. Public health assessment of potential biological terrorism agents. Emerg Infect Dis. 2002;8:225–230. doi: 10.3201/eid0802.010164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weissert C, Dollenmaier G, Rafeiner P, Riehm J, Schultze D. Burkholderia pseudomallei misidentified by automated system. Emerg Infect Dis. 2009;15:1799–1801. doi: 10.3201/eid1511.081719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brent AJ, Matthews PC, Dance DA, Pitt TL, Handy R. Misdiagnosing melioidosis. Emerg Infect Dis. 2007;13:349–351. doi: 10.3201/eid1302.061290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wuthiekanun V, Desakorn V, Wongsuvan G, Amornchai P, Cheng AC, et al. Rapid immunofluorescence microscopy for diagnosis of melioidosis. Clin Diagn Lab Immunol. 2005;12:555–556. doi: 10.1128/CDLI.12.4.555-556.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wuthiekanun V, Anuntagool N, White NJ, Sirisinha S. Short report: A rapid method for the differentiation of Burkholderia pseudomallei and Burkholderia thailandensis. Am J Trop Med Hyg. 2002;66:759–761. doi: 10.4269/ajtmh.2002.66.759. [DOI] [PubMed] [Google Scholar]
- 11.Gee JE, Sacchi CT, Glass MB, De BK, Weyant RS, et al. Use of 16S rRNA gene sequencing for rapid identification and differentiation of Burkholderia pseudomallei and B. mallei. J Clin Microbiol. 2003;41:4647–4654. doi: 10.1128/JCM.41.10.4647-4654.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee MA, Wang D, Yap EH. Detection and differentiation of Burkholderia pseudomallei, Burkholderia mallei and Burkholderia thailandensis by multiplex PCR. FEMS Immunol Med Microbiol. 2005;43:413–417. doi: 10.1016/j.femsim.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 13.Thibault FM, Valade E, Vidal DR. Identification and discrimination of Burkholderia pseudomallei, B. mallei, and B. thailandensis by real-time PCR targeting type III secretion system genes. J Clin Microbiol. 2004;42:5871–5874. doi: 10.1128/JCM.42.12.5871-5874.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Novak RT, Glass MB, Gee JE, Gal D, Mayo MJ, et al. Development and evaluation of a real-time PCR assay targeting the type III secretion system of Burkholderia pseudomallei. J Clin Microbiol. 2006;44:85–90. doi: 10.1128/JCM.44.1.85-90.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tomaso H, Scholz HC, Al Dahouk S, Eickhoff M, Treu TM, et al. Development of a 5′-nuclease real-time PCR assay targeting fliP for the rapid identification of Burkholderia mallei in clinical samples. Clin Chem. 2006;52:307–310. doi: 10.1373/clinchem.2005.059196. [DOI] [PubMed] [Google Scholar]
- 16.Supaprom C, Wang D, Leelayuwat C, Thaewpia W, Susaengrat W, et al. Development of real-time PCR assays and evaluation of their potential use for rapid detection of Burkholderia pseudomallei in clinical blood specimens. J Clin Microbiol. 2007;45:2894–2901. doi: 10.1128/JCM.00291-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chantratita N, Meumann E, Thanwisai A, Limmathurotsakul D, Wuthiekanun V, et al. Loop-mediated isothermal amplification method targeting the TTS1 gene cluster for detection of Burkholderia pseudomallei and diagnosis of melioidosis. J Clin Microbiol. 2008;46:568–573. doi: 10.1128/JCM.01817-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holden MTG, Titball RW, Peacock SJ, Cerdeño-Tárraga AM, Atkins T, et al. Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proc Natl Acad Sci. 2004;101:14240–14245. doi: 10.1073/pnas.0403302101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nierman WC, DeShazer D, Kim HS, Tettelin H, Nelson KE, et al. Structural flexibility in the Burkholderia mallei genome. Proc Natl Acad Sci. 2004;101:14246–14251. doi: 10.1073/pnas.0403306101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.U'Ren JM, Van Ert MN, Schupp JM, Easterday WR, Simonson TS, et al. Use of a real-time PCR TaqMan assay for rapid identification and differentiation of Burkholderia pseudomallei and Burkholderia mallei. J Clin Micobiol. 2005;43:5771–5774. doi: 10.1128/JCM.43.11.5771-5774.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pearson T, Giffard P, Beckstrom-Sternberg S, Auerbach R, Hornstra H, et al. Phylogeographic reconstruction of a bacterial species with high levels of lateral gene transfer. BMC Biology. 2009;7:78–91. doi: 10.1186/1741-7007-7-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US Army Medical Research Institute of Infectious Diseases. USAMRIID's medical management of biological casualties handbook, sixth ed. 2005;26 Available: http://www.usamriid.army.mil. Accessed 2010 May. [Google Scholar]
- 23.Neubauer H, Sprague LD, Joseph M, Tomaso H, Al Dahouk S, et al. Development and clinical evaluation of a PCR assay targeting the metalloprotease gene (mprA) of B. pseudomallei. Zoonoses Public Health. 2007;54:44–50. doi: 10.1111/j.1863-2378.2007.01008.x. [DOI] [PubMed] [Google Scholar]
- 24.Thibault FM, Hernandez E, Vidal DR, Girardet M, Cavallo JD. Antibiotic susceptibility of 65 isolates of Burkholderia pseudomallei and Burkholderia mallei to 35 antimicrobial agents. J Antimicrob Chemother. 2004;54:1134–1138. doi: 10.1093/jac/dkh471. [DOI] [PubMed] [Google Scholar]
- 25.Cahn A, Koslowsky B, Nir-Paz R, Temper V, Hiller N, et al. Imported melioidosis, Israel, 2008. Emerg Infect Dis. 2009;15:1809–1811. doi: 10.3201/eid1511.090038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. Imported melioidosis - South Florida, 2005. Morbid Mortal Weekly Rep. 2006;55:873–876. [PubMed] [Google Scholar]
- 27.Engelthaler DM, Bowers JR, Schupp JA, Pearson T, Ginther J, et al. Emerg Infect Dis. In press; 2010. Molecular investigations of an autochthonous case of melioidosis in Southern Arizona, USA. [Google Scholar]
- 28.Godoy D, Randle G, Simpson AJ, Aanensen DM, Pitt TL, et al. Multilocus sequence typing and evolutionary relationships among the causative agents of melioidosis and glanders, Burkholderia pseudomallei and Burkholderia mallei. J Clin Microbiol. 2003;41:2068–2079. doi: 10.1128/JCM.41.5.2068-2079.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Keim P, Van Ert MN, Pearson T, Vogler AJ, Huynh LY, et al. Anthrax molecular epidemiology and forensics: using the appropriate marker for different evolutionary scales. Infect Genet Evol. 2004;4:205–213. doi: 10.1016/j.meegid.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 30.Tuanyok A, Leadem BR, Auerbach RK, Beckstrom-Sternberg SM, Beckstrom-Sternberg JS, et al. Genomic islands from five strains of Burkholderia pseudomallei. BMC Genomics. 2008;9:566–579. doi: 10.1186/1471-2164-9-566. [DOI] [PMC free article] [PubMed] [Google Scholar]