Abstract
The increasing need for kidney transplants has led to innovations such as donor exchange programs. These programs offer transplant recipients with incompatible donors an opportunity to receive a compatible kidney. They also provide an alternative to costly desensitization protocols that have unproven long-term outcomes. Donor exchange programs have multiple options including simple two-pair exchanges, more complicated domino exchanges, or chain donations. The United States is currently limited by regional programs that provide for kidney donor exchanges. However, with the increasing public interest in and need for kidney transplants, general nephrologists will be approached with questions about these donor exchange programs. The goal of this review is to discuss donor exchange programs including their role in expanding the donor pool, the various types of exchanges, regional centers that provide these programs, and the process involved in patient enrollment. A general knowledge of donor exchange programs will help providers in discussing options with patients approaching end-stage kidney disease and transplant.
Recent evidence indicates that even if all deceased patients in the U.S. actually donated their kidneys, the supply would still be insufficient to meet the growing demand.1 Despite the enormous demand for deceased donor kidneys, the number of kidney transplants from deceased donors performed in the U.S. has remained relatively unchanged, averaging approximately 10,000 per year for the last 7 years.2 A significant increase in this number of deceased donors over the next few years is not expected.
Living organ donation not only promises to increase the pool of donor organs, but may improve the overall efficacy of transplants, because organs obtained from living donors typically produce better outcomes for recipients. The half-life, or projected time to 50% graft survival of kidney allografts from living donors is approximately 23 years, compared with 13 years among allografts from deceased donors.2, 3 These advantages are even greater for patients receiving transplants prior to initiating dialysis.4-7
One key obstacle to expanding the use of living donors is the incompatibility between transplant candidates and potential living donors due to blood type mismatch or the presence of pre-formed antibodies against donor antigens in the transplant candidate (also referred to as crossmatch-positive). Such incompatibility may account for 35% of potential transplant candidate-donor pairs being declined.8, 9 This has led to the next logical step of developing living donor exchange programs, first proposed in 1986.10 Such living donor exchange programs allow two incompatible transplant candidate-donor pairs to exchange living donor organs such that the resulting pairs achieve compatibility.8, 11-14 These programs, initially started in South Korea and the Netherlands, have slowly expanded to the United States in the last decade.
The introduction and evolution of kidney donor exchange in the United States has been slow, in part due to legal questions. In 1984, the U.S. Congress passed the National Organ Transplant Act (NOTA)14A which provided medical criteria for organ transplants and established a single transplant network to distribute deceased donor organs. As part of the act, NOTA prohibits any human organ transfer for “valuable consideration”. Since methods such as list-exchanges and paired exchanges provide benefits to recipients who provide a living kidney donor in the exchange, this could theoretically be considered a violation of NOTA. To avoid this problem, the Charlie W. Norwood Living Organ Donation Act in 200714B was passed to permit the development of paired exchange programs.
There are several other concerns in regards to kidney exchange programs. Ethical issues arise when particular groups are deprived by these paired exchanges. Another issue is the resources needed for paired exchanges that are often neglected. This review will describe kidney exchange programs and the process involved.
Types of Incompatibility
One of the major barriers to living donation between a donor and recipient is either blood type mismatch or the presence of a positive crossmatch. A positive crossmatch is due to the presence of a pre-existing antibody to a donor antigen. To get around this, protocols have been developed for desensitization of recipients with high pre-formed donor-specific antibodies or for ABO-incompatible transplants.
Desensitization protocols were developed to reduce the heightened risk of antibody-mediated rejection in recipients with a positive crossmatch to their donor. Several different methods to reduce pre-transplant antibodies have been described. Several centers use plasmapheresis alternating with intravenous immune globulin prior to transplant until the crossmatch becomes negative.15, 16 Jordan et al. used intravenous immune globulin alone to convert their crossmatch status from positive to negative.17 Another method uses rituximab and intravenous immune globulin to decrease the total panel reactive antibody (PRA) level while awaiting transplant.18 However, high titers of preformed donor-specific antibodies that are likely resistant to reduction by current protocols precludes patients from being eligible for desensitization. Also, not all costs associated with desensitization are covered by insurance companies, so this may not be an option for many patients.
Experience with ABO-incompatible transplants has shown improving outcomes over time. Initial experience showed poor outcomes and the need for splenectomy in these types of transplants to avoid severe antibody-mediated rejection.19 However, protocols have emerged using plasmapheresis/ intravenous immune globulin and rituximab20 that eliminate the need for splenectomy. These newer protocols have made ABO-incompatible transplants cost-effective in the long-term, compared with the costs associated with dialysis.21 However, there are limited data for long-term graft survival, and these individuals are more likely to experience antibody-mediated rejection15, 22, 23, which has been associated with a higher incidence of transplant glomerulopathy.24 Therefore, desensitization is not an option for all patients.
Types of Donor Exchanges
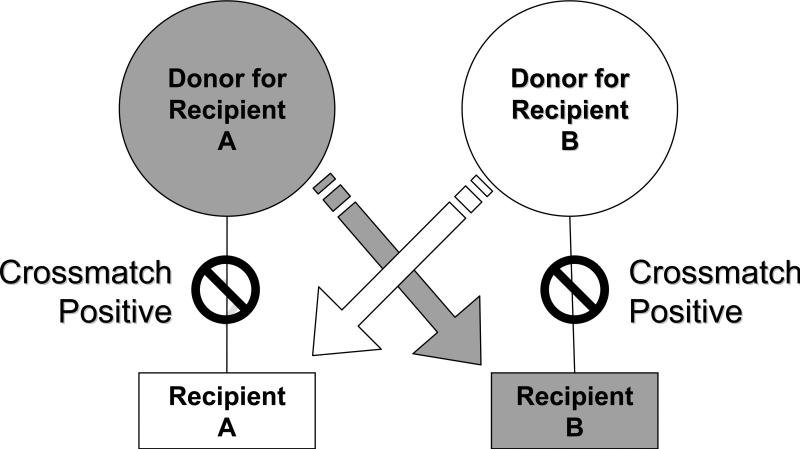
Multiple permutations of donor exchange have been described and implemented to accommodate the most number of recipients. Rapaport first described kidney paired donation where two incompatible donor-recipient pairs exchange donors to create two compatible pairs (Figure 1).10 In a donor exchange program, if the eligibility criteria for incompatibility was strictly limited to blood type, only type A and B pairs would mutually benefit from paired donation. However, if the eligibility criteria for incompatibility were expanded to crossmatch-positive donor-recipient pairs, then blood type AB recipients and type O donors also benefit from paired donation. Therefore, exchange programs allow for both blood type mismatched and crossmatch-positive donor-recipient pairs.
Figure 1.
Kidney Paired Donation whereby two potential transplant recipients exchange incompatible living donors, thereby resulting in two compatible recipient-donor pairs.
To expand the potential pool of donors and potential matches, other variations of paired donation have been conducted. Paired donations may include 3-way or higher exchanges, similar to the two-pair donation Rapaport described.25 Delmonico et al. described a program involving live donor/deceased donor list exchange where the incompatible living donor donates to an individual on the deceased donor list. In return, this donor's incompatible recipient is moved to the top of the list.26 One example where ethical issues arise is the list-exchange where an incompatible donor of a common blood type (e.g., blood type A) donates to someone near the top of the deceased donor waiting list. In exchange, this donor's incompatible recipient with a rarer blood type (e.g, blood type O) is placed near the top of the deceased donor waiting list, bypassing many other potential recipients with the rarer blood type. There is some concern that individuals on the waiting list for a rarer blood type will have to wait longer because incompatible recipients are being moved ahead of them. Another type of exchange that may be viewed as controversial is an imbalanced paired donation. This is where a compatible pair, in hopes of receiving a younger kidney or avoiding a high immunologic risk donation, is matched with an incompatible pair, thereby resulting in two compatible transplant pairs.27 This type of exchange has been viewed as unethical by some transplant center directors28, possibly because paired donation may not provide any medical benefit to the compatible pair and may take away some emotional benefit of an individual donating directly to a relative.
A variation of non-directed donation includes a non-directed donor starting a chain (Figure 2). In this process, a non-directed donor donates their kidney to recipient A with an incompatible donor. The incompatible donor for recipient A then donates their kidney to recipient B of another incompatible pair. This process continues until no other suitable pairs are found. A 4-way domino was performed in 2008 over a 14 hour period at the Toronto General Hospital in Toronto, Canada. In this domino transplant, the coordinator worked for 14 consecutive hours to coordinate the 4 transplants using 2 operating rooms (S.J.K. unpublished observation, 2010). The transplant center at Johns Hopkins recently reported ongoing chains in multiple centers, both chains starting from a non-directed donor.29
Figure 2.
Non-directed donor can start a chain or domino of transplants for incompatible pairs. For logistical reasons, all transplants in a chain need not occur at the same time. The chain may continue endlessly until an incompatible donor decides not to donate and breaks a chain. The chain may be intentionally broken by donating to a patient on the deceased donor waiting list. When creating an endless chain, it is ideal not to stop a chain at an incompatible donor with AB blood type since that donor's kidney may only be accepted by a AB blood type recipient. Such a recipient with an incompatible donor is rare to find.
Current programs
Multiple programs around the world have used variations of the exchanges listed above. National programs include South Korea30, Netherlands31, and, most recently, Canada.32 In the United States, several regional networks have been established (Table 1).26 Several large individual transplant centers have conducted exchange programs within their own centers such as Columbia University in New York, California Pacific Medical Centers and University of Wisconsin. The latter two have also joined regional networks. California Pacific Medical Center reported excellent outcomes from 21 transplants that have been conducted using these exchange programs.33
Table 1.
Donor Exchange Programs in the United States and Canada
| Program | Region of the U.S or Canada | Website |
|---|---|---|
| Region 1 of UNOS | New England | nepke.org/ |
| Washington Regional Transplant Community | Washington, D.C. | www.beadonor.org/ |
| Alliance for Paired Donation | Multiple states around the country | www.paireddonation.org/ |
| North American Paired Donation Network | Multiple states around the country | www.paireddonationnetwork.org/ |
| Johns Hopkins | Collaborates with several other transplant centers | www.hopkinsmedicine.org/transplant/Programs/InKTP/ |
| National Kidney Registry | Multiple states around the country | www.kidneyregistry.org |
| North Central Donor Exchange Cooperative | MN, WI, ND, SD, IA | www.ncdec.org |
| Living Donor Paired Exchange Registry | Canada | www.ccdt.ca/english/ldpe/ |
Abbreviations: UNOS, United Network for Organ Sharing
South Korea started their program in 1991 with a single pair swap between donors of two patients on dialysis.34 This program expanded by using a computer database with all the incompatible donor-recipient pairs that were evaluated. The result was a reported 101 paired donations from 1995-2003, increasing from 2% of all living donor transplants in 1995 to 11% in 2003. 30 In 2005, the program switched to a web-based program with monthly match-runs used to identify individuals compatible based on their HLA antigens and blood type. A significant problem noted by this group was the use of local HLA laboratories at respective transplant centers. The use of different HLA labs led to numerous matches that were thought to be compatible on the initial match run that ended up being crossmatch positive when tested at the same center.
The Netherlands program includes 7 transplant centers in which the Dutch Transplantation Foundation developed and runs the allocation algorithm used to match donor/recipient pairs.35 The algorithm calculates a match probability for each recipient based on their degree of sensitization by the PRA of the recipient, blood group type, and HLA unacceptable antigens. The rank list for donor/recipient pairs is then sorted by match probability with the lowest probability being ranked the highest. Similar to the program in South Korea, match runs are conducted every 3 months. In addition, a feature that helped increase successful matches was a centralized HLA laboratory, which reduced the number of false positive matches on their initial match run. At their last report in 2009, this program found 169 matches, with 131 proceeding to transplant.36
The National Living Donor Paired Exchange Registry in Canada was established in 2009. A 4-way domino kidney transplant involving three cities across Canada was performed soon after the registry was activated. Since then, multiple domino and paired exchanges have been successfully undertaken and most parts of the country are now participating. To minimize the problem with false positive matches reported by the South Korea program, members of the HLA and transplant nephrology communities in Canada are in the process of standardizing HLA antibody detection methodologies among all transplant centers (S.J.K., unpublished observation, 2010).
With the success of the national programs in South Korea and the Netherlands, the Johns Hopkins program has been a strong proponent of a national exchange program. Segev, et al. have looked at the potential of regional and national kidney paired donation programs in matching incompatible pairs.9 Using simulations of incompatible donor/recipient pairs, a national program would increase the number of matches by 47%.
Although a national program has not yet been established in the U.S., private organizations and transplant centers have collaborated to develop donor exchange programs that cover multiple regions around the country (Table 1). Region 1 of UNOS covers 14 transplant centers in the New England area. This program is operated by the New England Organ Bank, the New England area organ procurement organization (OPO). The program is unique in that it allows for both paired living donor exchanges and list exchanges. The Ohio Solid Organ Transplant Consortium is another program that used a web-based computerized matching program to match incompatible pairs. This program has since expanded outside the initial 8 transplant programs in Ohio to become the Paired Donation Consortium. The Alliance for Paired Donation is another group that spans several states in the U.S. and was one of the first to introduce altruistic donation between compatible and incompatible pairs as well as altruistic donors that lead to non-simultaneous extended altruistic donor chains.29 The National Kidney Registry was started by a father who searched multiple kidney exchange programs to provide a kidney for his 10 year old daughter, who eventually benefited from a paired donation. After the successful transplant to his daughter, he wanted to create a common registry to simplify the process of finding a compatible match.37 Also in existence is the North Central Donor Exchange Cooperative (NCDEC), which covers Minnesota, Wisconsin, Iowa, and the Dakotas. While most donor exchange programs provide similar services, their implementation may be slightly different. We will focus on the process and challenges encountered during the development and operation of the NCDEC which may not necessarily represent the practice decisions of other exchange programs.
Process of Participating in the NCDEC
When the recipient initially discusses a transplant, the pre-transplant coordinator at Hennepin County Medical Center presents paired donation among their options. Potential donors are also presented this option during their evaluation in case they are immunologically incompatible with their intended recipient. If the pair is incompatible, the incompatible donor and recipient are then offered the opportunity to join the match program. If interested, the pair must give a special consent to share their information with other centers to find a compatible exchange. In the case of multiple incompatible donors, usually the best donor, selected by the local transplant surgeon, is offered the opportunity. These individuals are typically the youngest with the least co-morbidities and most willing to donate. Selecting one donor helps to keep the cost of the pre-transplant work-up manageable. However a transplant program can list several incompatible donors for a single recipient. If the incompatible donor and recipient consent to the match program, their data is entered into a database. The data entered into the database includes age, blood type, and HLA type for both the incompatible donor and the recipient. We also include recipient PRA and unacceptable HLA antigens. Each of the transplant centers submits unacceptable antigens for the recipients that were detected using a sensitive test used to detect pre-existing antibodies to the HLA antigens. By knowing these unacceptable antigens, a virtual crossmatch is done between the known antigens of potential donors against the unacceptable antigens of potential recipients. This method minimizes positive crossmatches between the donor and the recipient after a match run.
Match runs are conducted monthly if a new pair is entered into the database. The match run has a few rules to ensure mutually agreed-upon, socially equitable exchanges. The match run program will not match donors to a transplant candidate more than 20 years younger than the candidate's incompatible donor. This prevents a transplant candidate from receiving a much younger donor than they brought to the exchange. Donor age has been found to be an important factor in living donor allograft survival.38 If a match is found, the transplant teams are informed and then they start reviewing the donor characteristics and proceed to an actual cross-match to be conducted by the individual transplant centers.
Recipients participating in some donor exchange programs may be required to accept the anonymity of the donor. In a study of participants of one kidney exchange program, 78% of recipients were satisfied that the procedure had taken place anonymously to avoid extra stress or concerns about the anonymous donor.39 If the donor wishes to remain anonymous, the transplant center needs to be aware of the logistical issues of keeping the pairs in separate sections of the hospital during the pre-operative and post-operative periods. All this requires intensive work on the part of the transplant coordinator, so much so that other exchange programs found this process to be almost impossible in a single center, and they arrange for the donors and recipients to meet prior to transplant.40 If donors and recipients in the NCDEC consent to meet, this is arranged among the NCDEC centers. The NCDEC recommends waiting at least until 6 months after the surgery to allow for both recipients to complete the high risk period for acute rejections.
Coordination of the multiple transplants at one time can also consume a significant amount of coordinator time. This is a significant concern, particularly among smaller transplant programs.41 The process of establishing the NCDEC required input from many of the participating sites, in order to develop a working plan along with programmer support to create a web-based data entry tool and a match run program. The NCDEC also collaborates with other exchange programs in order to maximize the possibility of finding compatible donors for the highly sensitized patients who are participating in the NCDEC.
Future Directions
A national program does not yet exist in the United States. However, a pilot program by UNOS is being developed. The pilot program will initially enroll four consortiums of donor exchange programs that have experience in kidney paired donation and test the practice for 1 year before wide-scale implementation to all interested OPTN and UNOS programs. These four consortium members include the exchange program of the New England Organ Bank, Alliance for Paired Donation, The Johns Hopkins University and another group of transplant centers represented by UCLA. The Johns Hopkins University consortium includes their exchange group as well as the NCDEC along with several other transplant centers.
The pilot program for a national exchange program hopes to address several concerns, including donor travel, follow up care, and shipping of kidneys. With regard to shipping kidneys, some donors may not be able to travel to another state for donation. However, for a national program to succeed, this issue needs to be addressed. One option is for the kidney to travel rather than the donor. The primary concern is that cold-ischemia times would be longer than typical living donor transplants. Waki, et al. looked at living donor kidneys with cold ischemia times ranging from 0-6, 7-12, and 13-24 hours and found no significant difference in graft survival between the group.42 Simpkins, et al. looked specifically at living donor kidneys with cold ischemia times up to 8 hours.43 They found higher rates of delayed graft function with increased cold ischemia time, but no difference in serum creatinine, acute rejection, or long-term graft survival. These two studies both concluded that longer cold ischemia times associated with shipping organs will have no detrimental effects. This issue is brought up with the donor and recipient as part of the consent process. The NCDEC and other exchanges work with their local organ procurement organizations to help with the shipping of the living donor organs. As for follow up care, the surgeons at the recipient transplant center participating in the NCDEC were willing to follow donors they did not operate on.
Summary
The shortage of organs has led to innovative methods that allow more patients to undergo kidney transplants. Kidney paired exchanges, from the simplest two incompatible paired exchange to the complexity of simultaneous multi-way exchanges or extended donor chains, have emerged out of various regional exchange programs in the U.S. As the news media reports paired exchange success stories,44 patients will be approaching their nephrologists about how they can participate in these programs. The importance of a national program is recognized by UNOS and a pilot program is in development with the hope of a national program by the end of 2010. In the mean time, incompatible recipient-donor pairs can discuss kidney paired donation with their local nephrologists. Some potential questions or issues regarding donor exchange programs are presented in Table 2. While the specific details of donor exchange programs should be left to the transplant center, the local nephrologist should be aware of the closest transplant center that participates in a regional donor exchange program so their patients can benefit from these programs. The onus for a timely referral to such exchange programs will probably fall on the local nephrologist, however such a referral may greatly benefit the incompatible recipient-donor pairs in their practice.
Table 2.
Key Issues in Donor Exchange Programs for the Practicing Nephrologist
| Question for the Patient or Nephrologist | Potential Issues |
|---|---|
| Should the recipient go to a center that offers desensitization protocols and donor exchange? | Ideally, the recipient should go to a program that offers donor exchange as an option. If the recipient is unable to find an exchange, than consider a center with a desensitization program. However, while desensitization protocols are available, they still have higher rates of antibody mediated rejections than compatible transplants and long-term outcomes are unknown. |
| Is it important to refer to a patient to a center that has done many donor exchanges? | While there are many centers, very few programs have done a large number of donor exchanges. Since most exchange programs are centralized and likely similar in their procedures, the preference should be towards centers that have better transplant outcomes rather than experience with donor exchanges. |
| Will the donor be willing to travel to another center to donate their kidney to someone else? | If the exchange occurs at different centers, the donor may be required to travel to the other recipient's center for donation. |
| Will the recipient accept a shipped kidney? | Though graft outcomes are typically similar to normal living donor kidneys, there is little data regarding long-term outcomes of shipping kidneys from living donors. |
| Will the recipient accept waiting a little longer for a transplant? | Coordination between 2 incompatible pairs may take longer (ie, work or school obligations may delay surgery for 1 pair). |
| Will taking a kidney from an older donor affect my graft outcome? | Registry data suggests that as donor age increases, graft survival decreases. Exchange with a much older donor may affect long-term graft survival. |
Acknowledgements
Support: Dr Akkina was supported by a research grant from the American Society of Transplantation and the National Institute of Diabetes and Digestive and Kidney Diseases, Award Number K23DK084121. Dr Israni is a Robert Wood Johnson Foundation Physician Faculty Scholar. Dr Kim is supported by the Clinician-Scientist Training Award, Canadian Institutes of Health Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: The authors declare that they have no relevant financial interests.
References
- 1.Sheehy E, Conrad SL, Brigham LE, et al. Estimating the number of potential organ donors in the United States. N Engl J Med. 2003 Aug 14;349(7):667–674. doi: 10.1056/NEJMsa021271. [DOI] [PubMed] [Google Scholar]
- 2.US Renal Data System . USRDS 2009 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2009. [Google Scholar]
- 3.Hariharan S, Johnson CP, Bresnahan BA, Taranto SE, McIntosh MJ, Stablein D. Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med. 2000 Mar 2;342(9):605–612. doi: 10.1056/NEJM200003023420901. [DOI] [PubMed] [Google Scholar]
- 4.Mange KC, Joffe MM, Feldman HI. Effect of the use or nonuse of long-term dialysis on the subsequent survival of renal transplants from living donors. N Engl J Med. 2001 Mar 8;344(10):726–731. doi: 10.1056/NEJM200103083441004. [DOI] [PubMed] [Google Scholar]
- 5.Vats AN, Donaldson L, Fine RN, Chavers BM. Pretransplant dialysis status and outcome of renal transplantation in North American children: a NAPRTCS Study. North American Pediatric Renal Transplant Cooperative Study. Transplantation. 2000 Apr 15;69(7):1414–1419. doi: 10.1097/00007890-200004150-00035. [DOI] [PubMed] [Google Scholar]
- 6.Donnelly P, Oman P, Henderson R, Opelz G. Living donor kidney transplantation in predialysis patients: experience of marginal donors in Europe and the United States. Transplant Proc. 1996 Dec;28(6):3566–3570. [PubMed] [Google Scholar]
- 7.Cacciarelli TV, Sumrani N, DiBenedetto A, Hong JH, Sommer BG. Influence of length of time on dialysis before transplantation on long-term renal allograft outcome. Transplant Proc. 1993 Aug;25(4):2474–2476. [PubMed] [Google Scholar]
- 8.Ross LF, Rubin DT, Siegler M, Josephson MA, Thistlethwaite JR, Jr., Woodle ES. Ethics of a paired-kidney-exchange program. N Engl J Med. 1997 Jun 12;336(24):1752–1755. doi: 10.1056/NEJM199706123362412. [DOI] [PubMed] [Google Scholar]
- 9.Segev DL, Gentry SE, Warren DS, Reeb B, Montgomery RA. Kidney paired donation and optimizing the use of live donor organs. JAMA. 2005 Apr 20;293(15):1883–1890. doi: 10.1001/jama.293.15.1883. [DOI] [PubMed] [Google Scholar]
- 10.Rapaport FT. The case for a living emotionally related international kidney donor exchange registry. Transplant Proc. 1986 Jun;18(3) Suppl. 2):5–9. [PubMed] [Google Scholar]
- 11.Sells RA. Paired-kidney-exchange programs. N Engl J Med. 1997 Nov 6;337(19):1392–1393. doi: 10.1056/NEJM199711063371915. [DOI] [PubMed] [Google Scholar]
- 12.Ross LF, Woodle ES. Ethical issues in increasing living kidney donations by expanding kidney paired exchange programs. Transplantation. 2000 Apr 27;69(8):1539–1543. doi: 10.1097/00007890-200004270-00001. [DOI] [PubMed] [Google Scholar]
- 13.de Klerk M, Keizer K, Weimar W. Donor exchange for renal transplantation. N Engl J Med. 2004 Aug 26;351(9):935–937. doi: 10.1056/NEJM200408263510921. [DOI] [PubMed] [Google Scholar]
- 14.Kranenburg LW, Visak T, Weimar W, et al. Starting a crossover kidney transplantation program in the Netherlands: ethical and psychological considerations. Transplantation. 2004 Jul 27;78(2):194–197. doi: 10.1097/01.tp.0000129259.02340.f7. [DOI] [PubMed] [Google Scholar]
- 14A.National Organ Transplant Act, 42 USC §274. 2009.
- 14B.Charlie W. Norwood Living Organ Donation Act, Pub L No. 110–144, 121 Stat 1814.
- 15.Thielke JJ, West-Thielke PM, Herren HL, et al. Living donor kidney transplantation across positive crossmatch: the University of Illinois at Chicago experience. Transplantation. 2009 Jan 27;87(2):268–273. doi: 10.1097/TP.0b013e3181919a16. [DOI] [PubMed] [Google Scholar]
- 16.Montgomery RA, Zachary AA, Racusen LC, et al. Plasmapheresis and intravenous immune globulin provides effective rescue therapy for refractory humoral rejection and allows kidneys to be successfully transplanted into cross-match-positive recipients. Transplantation. 2000 Sep 27;70(6):887–895. doi: 10.1097/00007890-200009270-00006. [DOI] [PubMed] [Google Scholar]
- 17.Jordan SC, Vo A, Bunnapradist S, et al. Intravenous immune globulin treatment inhibits crossmatch positivity and allows for successful transplantation of incompatible organs in living-donor and cadaver recipients. Transplantation. 2003 Aug 27;76(4):631–636. doi: 10.1097/01.TP.0000080685.31697.FC. [DOI] [PubMed] [Google Scholar]
- 18.Vo AA, Wechsler EA, Wang J, et al. Analysis of subcutaneous (SQ) alemtuzumab induction therapy in highly sensitized patients desensitized with IVIG and rituximab. Am J Transplant. 2008 Jan;8(1):144–149. doi: 10.1111/j.1600-6143.2007.02017.x. [DOI] [PubMed] [Google Scholar]
- 19.Alexandre G, Squifflet J, De Bruyere M, Latinne D, Moriau M, Ikabu N. Splenectomy as a prerequisite for successful human ABO-incompatible renal transplantation. Transplant Proc. 1985;17:138–143. [Google Scholar]
- 20.Sonnenday CJ, Warren DS, Cooper M, et al. Plasmapheresis, CMV hyperimmune globulin, and anti-CD20 allow ABO-incompatible renal transplantation without splenectomy. Am J Transplant. 2004 Aug;4(8):1315–1322. doi: 10.1111/j.1600-6143.2004.00507.x. [DOI] [PubMed] [Google Scholar]
- 21.Gloor JM, Stegall MD. ABO incompatible kidney transplantation. Curr Opin Nephrol Hypertens. 2007 Nov;16(6):529–534. doi: 10.1097/MNH.0b013e3282f02218. [DOI] [PubMed] [Google Scholar]
- 22.Gloor JM, Winters JL, Cornell LD, et al. Baseline donor-specific antibody levels and outcomes in positive crossmatch kidney transplantation. Am J Transplant. 2010 Mar;10(3):582–589. doi: 10.1111/j.1600-6143.2009.02985.x. [DOI] [PubMed] [Google Scholar]
- 23.Galliford J, Chan K, Lawrence C, et al. Antibody Mediated Rejection after ABO Incompatible Living Donor Renal Transplantation Is Mainly Associated with HLA Donor Specific Antibodies. Am J Transplant. 2010;10(s4):164. [ATC Abstract 421] [Google Scholar]
- 24.Gloor JM, Cosio FG, Rea DJ, et al. Histologic findings one year after positive crossmatch or ABO blood group incompatible living donor kidney transplantation. Am J Transplant. 2006 Aug;6(8):1841–1847. doi: 10.1111/j.1600-6143.2006.01416.x. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan I, Houp JA, Montgomery RA, Leffell MS, Hart JM, Zachary AA. A computer match program for paired and unconventional kidney exchanges. Am J Transplant. 2005 Sep;5(9):2306–2308. doi: 10.1111/j.1600-6143.2005.00991.x. [DOI] [PubMed] [Google Scholar]
- 26.Delmonico FL, Morrissey PE, Lipkowitz GS, et al. Donor kidney exchanges. Am J Transplant. 2004 Oct;4(10):1628–1634. doi: 10.1111/j.1600-6143.2004.00572.x. [DOI] [PubMed] [Google Scholar]
- 27.Kranenburg LW, Zuidema W, Weimar W, et al. One donor, two transplants: willingness to participate in altruistically unbalanced exchange donation. Transpl Int. 2006 Dec;19(12):995–999. doi: 10.1111/j.1432-2277.2006.00378.x. [DOI] [PubMed] [Google Scholar]
- 28.Westermann-Clark EV, Hanto R, Donelan K, et al. Three Kidney Transplant Controversies: Results of a National Survey of Transplant Center Directors. Am J Transplant. 2009;9:387–388. [Google Scholar]
- 29.Rees MA, Kopke JE, Pelletier RP, et al. A nonsimultaneous, extended, altruistic-donor chain. N Engl J Med. 2009 Mar 12;360(11):1096–1101. doi: 10.1056/NEJMoa0803645. [DOI] [PubMed] [Google Scholar]
- 30.Park K, Lee JH, Huh KH, Kim SI, Kim YS. Exchange living-donor kidney transplantation: diminution of donor organ shortage. Transplant Proc. 2004 Dec;36(10):2949–2951. doi: 10.1016/j.transproceed.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 31.de Klerk M, Keizer KM, Claas FH, Witvliet M, Haase-Kromwijk BJ, Weimar W. The Dutch national living donor kidney exchange program. Am J Transplant. 2005 Sep;5(9):2302–2305. doi: 10.1111/j.1600-6143.2005.01024.x. [DOI] [PubMed] [Google Scholar]
- 32.Canadian Blood Services [January 28, 2010, 2009];Canadian Blood Services Launches Living Donor Paired Exchange Registry. 2009 http://www.blood.ca/CentreApps/Internet/UW_V502_MainEngine.nsf/web/0F5E4DFB20C9711B8525755B0055A428?OpenDocument.
- 33.Ueda K, Jaber L, John D, et al. 5 Year Follow Up of Paired Kidney Exchange at a Single Center. Am J Transplant. 2009;9:434–434. [ATC Abstract 844] [Google Scholar]
- 34.Park K, Moon JI, Kim SI, Kim YS. Exchange donor program in kidney transplantation. Transplantation. 1999 Jan 27;67(2):336–338. doi: 10.1097/00007890-199901270-00027. [DOI] [PubMed] [Google Scholar]
- 35.Keizer KM, de Klerk M, Haase-Kromwijk BJ, Weimar W. The Dutch algorithm for allocation in living donor kidney exchange. Transplant Proc. 2005 Mar;37(2):589–591. doi: 10.1016/j.transproceed.2004.12.096. [DOI] [PubMed] [Google Scholar]
- 36.Ferrari P, de Klerk M. Paired kidney donations to expand the living donor pool. J Nephrol. 2009 Nov-Dec;22(6):699–707. [PubMed] [Google Scholar]
- 37.National Kidney Registry [September 15, 2009, 2009];Natinal Kidney Registry - Facilitating Living Donor Transplants. http://www.kidneyregistry.org.
- 38.Muster HA, Kasiske BL, Snyder JJ, Israni AK. Living Unrelated Donor Characteristics: Implications for Living Donor Paired Exchange Programs. Am J Transplant. 2006;6:788. [WTC Abstract 2180] [Google Scholar]
- 39.Massey EK, Zuidema W, Visscher J, IJzermans JNM, Weimar W. Psychological Aspects of Receipt of an Anonymous Living Kidney Via a Domino-Paired Kidney Exchange Procedure. Am J Transplant. 2009;9:435–435. [ATC Abstract 849] [Google Scholar]
- 40.Lucan M. Five years of single-center experience with paired kidney exchange transplantation. Transplant Proc. 2007 Jun;39(5):1371–1375. doi: 10.1016/j.transproceed.2007.02.081. [DOI] [PubMed] [Google Scholar]
- 41.Westermann-Clark EV, Hanto R, Donelan K, et al. Survey of US Transplant Centers on Barriers to Implementation of Kidney Paired Donation, List Paired Donation, and Desensitization Protocols. Am J Transplant. 2009;9:434–434. [ATC Abstract 843] [Google Scholar]
- 42.Waki K, Terasaki PI. Paired kidney donation by shipment of living donor kidneys. Clin Transplant. 2007 Mar-Apr;21(2):186–191. doi: 10.1111/j.1399-0012.2006.00621.x. [DOI] [PubMed] [Google Scholar]
- 43.Simpkins CE, Montgomery RA, Hawxby AM, et al. Cold ischemia time and allograft outcomes in live donor renal transplantation: is live donor organ transport feasible? Am J Transplant. 2007 Jan;7(1):99–107. doi: 10.1111/j.1600-6143.2006.01597.x. [DOI] [PubMed] [Google Scholar]
- 44.Aratani L. Dominoes Align for for Key Kidney Transplant. [September 15, 2009, 2009];The Washington Post [Newspaper]. 2009 http://www.washingtonpost.com/wpdyn/content/article/2009/07/07/AR2009070702696.html.