Abstract
Purpose
To describe the current state of design characteristics determined to be desirable by the Agency for Health Research and Quality (AHRQ) in U.S. adult medical, surgical, and intensive care units (ICUs).
Design
Descriptive study of patient visibility; distance to hygiene, toileting, charting, and supplies; unit configuration; percentage of private rooms; and presence or absence of carpeting in 56 ICUs and 81 medical-surgical units in six metropolitan areas.
Methods
Data were collected via observation, measurement, and interviews. Unit configurations were classified via an iterative process. Descriptive data were analyzed according to ICU and non-ICU status using SPSS (Version 15).
Findings
Analysis of unit configurations indicated eight unit designs. Statistical analysis showed inter- and intrahospital variation in unit configurations, percentage private rooms, carpeting, visibility, and distance to supplies and charting. Few units met the AHRQ designated design elements studied.
Conclusions
A wide gap exists between desirable characteristics in ICUs and medical-surgical units. Future research is needed to explore operationalization of unit design elements as risk adjustments, how design elements contribute to patient outcomes, and how design elements influence one another.
Clinical Relevance
There is room for improvement on almost every design variable, particularly on medical-surgical units. Future planning should take into consideration the interaction of bed capacity and unit configuration.
Keywords: Unit design, ICU, medical-surgical unit, hospital design
Physical design of hospital nursing care units' can influence safety and care-delivery costs. Experts from the US have noted that a renewed emphasis on design is needed (Anjali, 2006a, 2006b, 2006c; Hamilton, 2003; Hendrich, Fay, & Sorrells, 2004). Changing patient demographics, staffing patterns, and technology must be considered during the current hospital building surge to meet safety, efficiency, and equity goals (Robert Wood Johnson Foundation, 2004; Ulrich, Xiaobo, Zimring, Anjali, & Choudhary, 2004). Authors of the AHRQ's "Transforming Hospitals: Designing for Safety and Quality" initiative have projected that over the next 10 years, the US will spend $250 billion to construct or modify hospitals (AHRQ, 2007). Research gaps related to potentially interactive elements of unit design have made determining an optimal design difficult, but progress has been made in identifying design characteristics that influence outcomes. Among the nursing-unit characteristics deemed by AHRQ to influence patient and staff outcomes are: providing single rooms, work areas for staff that are not long distances from the bedside, frequent staff hand-hygiene stations, "visibility" of patients from nurse work areas, and noise reduction via ceiling tiles and carpeting (AHRQ, 2007).
Our purpose in this paper is to describe the current state of these design characteristics in U.S. adult medical-surgical (M-S) and intensive care units (ICUs). Our goals are to inform future researchers about unit designs, provide a benchmark to judge if buildings in this decade resulted in improvements, and provide a basis to assess nursing environments.
Background
Unit configuration
Institute of Medicine (IOM) officials described eight designs (Page & Page, 2004) based on the work of James and Tatton-Brown (1986). The simple open (Nightingale) design consists of an open ward without individual patient rooms. Beds face toward a nurses' work area. In the corridor (continental) design, patients are located on one or both sides of a corridor with four to six beds per room. The corridor design may be in a "T," "C," or "L" shape. The duplex configuration (Nuffield) is similar to the corridor design but is split into two sections with each including its own station and shared support space. The racetrack (double corridor) design has nursing work and support spaces between two corridors. This is believed to be one of the most common designs in the US (Page & Page, 2004). The courtyard is a racetrack design that includes a courtyard for ventilation in the middle of the unit. The cruciform (cluster) design is a modification of the corridor plan to ensure that as many patients as possible are gathered around the nursing station while providing privacy enhancements such as walls and doors. The radial design is a circle that permits a "fishbowl" view of each room from the nurses' station. The triangle design has support space in the middle of the triangle formed by three connecting corridors with access to patient rooms.
Although data exist regarding advantages and disadvantages of some of these designs, especially in ICUs (Page & Page, 2004; Rashid, 2006), the literature does not include comprehensive descriptions of how often these designs occur nor if and how these designs incorporate AHRQ unit characteristics were deemed to contribute to outcomes. No comprehensive data are available regarding unit design variation within hospitals, an important gap given the assumption of many outcome studies that resources are institutionally homogeneous.
Other design characteristics
In 2005, AHRQ publicized a commissioned report about hospital environments (Nelson, West, & Goodman, 2005). The report included a summary of all published research (N = 328 reports) about those environments and patient and staff outcomes, including safety, satisfaction, and efficiency as well as clinical outcomes. Although many gaps were noted, the presence and use of specific resources were found to be at least somewhat related to several outcomes. In 2007, AHRQ, building on this work, released a DVD highlighting specific research-based positive design elements (AHRQ, 2007). We selected other design elements based on citations in AHRQ literature. Given that our study was conducted before and during the AHRQ work, not every AHRQ-identified design feature was included in our work.
Methods
Study aims included a description of the context for physical restraint use, device disruption, and falls; and data about unit design. Characteristics were collected at 40 randomly selected, non-federal hospitals of greater than 99 average daily patient census in six metropolitan areas representative of the U.S. population. The areas represented were the Western, Southern, Midwestern, and Northeastern regions. (Details about the methods are available in Minnick, Mion, Johnson, Catrambone, & Leipzig, 2007).
The investigators collected unit-specific information based on visual observation, distance measurements, and unit director interviews at one general ICU, one medical and one surgical unit per hospital. In hospitals without a general ICU, data were collected on one medical and one surgical ICU. In hospitals with more than one medical and surgical unit, data were collected on the units with the highest rate of physical-restraint use. This procedure resulted in including 56 ICUs and 81 M-S units. Inter-rater reliability of greater than 0.98 was maintained by restricting data collection to the investigators. The study met all human subjects' requirements of the investigators' institutions and participating hospitals.
Patient “visibility”
The researcher and an assistant ascertained this by standing at each nurse charting area (station) and counting the beds that met the criteria that the upper third of the bed could be seen when either the door or room blinds were open. This definition was selected because the ability to see the head, hands, and chest is key to cueing nursing action in the event of respiratory distress and unsafe acts. All beds available for service plus those in use were included. The work area (nursing station) was defined as the place where nursing staff charted data beyond that recorded on flow sheets. If a bed was monitored by a camera (less than 1% of beds) that allowed the view described above, it was counted.
Distance measurement
Based on earlier work by Minnick, Roberts, Young, Kleinpell, and Marcantonio (1997), the researcher and an assistant measured distances from the head of the patient's bed to supplies, chart (not flow sheet), fresh water, and disposal of gastrointestinal and urinary waste using standard metal tape measures. Supplies were defined as the basic consumables (bandages, swabs, and so on) needed for nursing care. Special measurements were taken if the item or resource was room-based (e.g., room-based charting capacity). If the item or resource was room based and the room was private, the distance was measured from the patient's bed to the item. If rooms on a unit varied in size, the largest, mid, and smallest room distance measures were obtained. In semiprivate or ward situations, measurements were made from the room's center. In cases without a room-based resource (e.g., charting at a nurse's station), measurements were made from the rooms that were the longest, mid, and shortest distances.
Configuration and carpeting
The presence of carpet in halls and patients' rooms was recorded. Ceiling tile acoustic properties were not measured because of resource limitations. No attempt was made to assign a geometric configuration type at the time of data collection. The researcher and assistant made a simple diagram that included the main corridors, defined as those used by patients and visitors to reach patient rooms, the location of rooms off of these corridors, and the locations of work and support areas. The number of beds per room and number of rooms were recorded. Support service areas included supply storage facilities, monitor rooms, staff lockers and bathrooms, and meeting spaces.
Unit Configuration Classification Process
Three of the coinvestigators independently reviewed the design configuration sketches (n = 137) of group units based on (a) similarities in the relationship of patient rooms to work areas and (b) unit entry and exit points to reflect nurse-relevant design typologies. These relationships were chosen because nurses have identified them as work influencers (Minnick, Roberts, Curran, & Ginzberg, 1989). Comparison of investigator design groupings resulted in consensus on nine configuration types. The investigators created a grid that included the nine types and a sketch of each that was used for a second independent classification review.
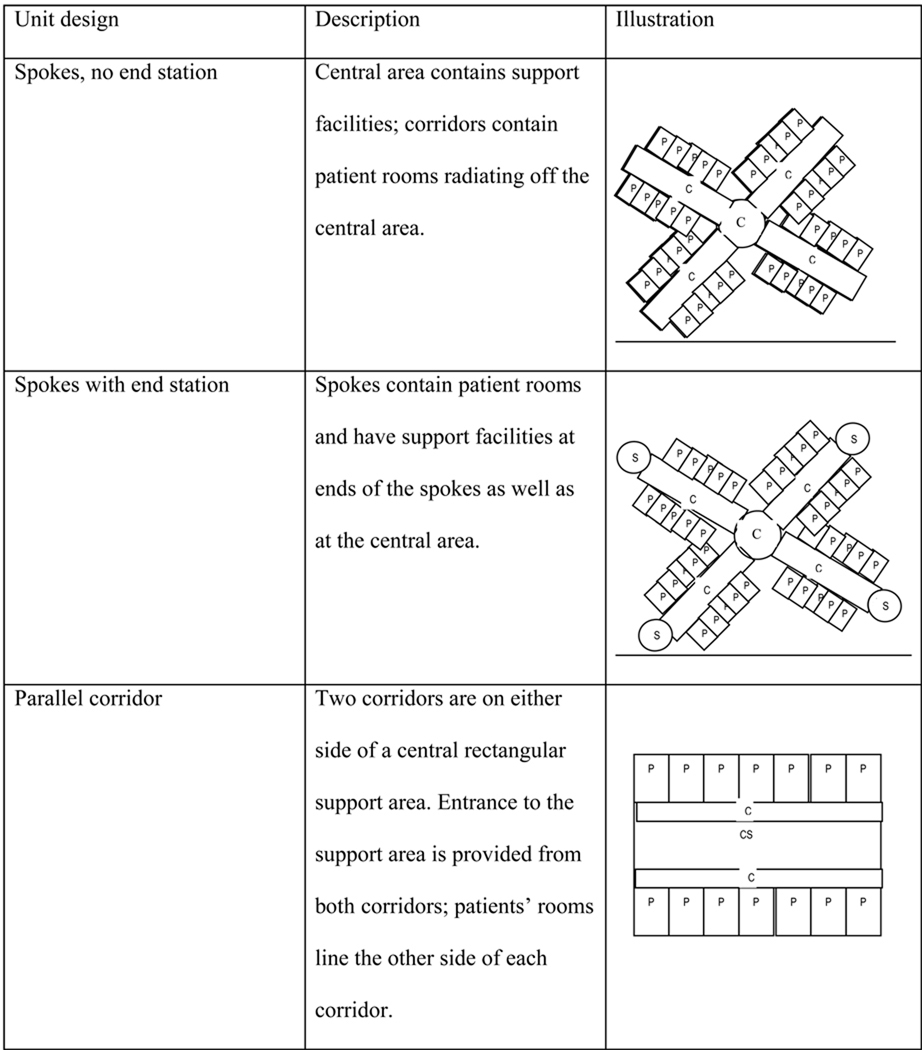
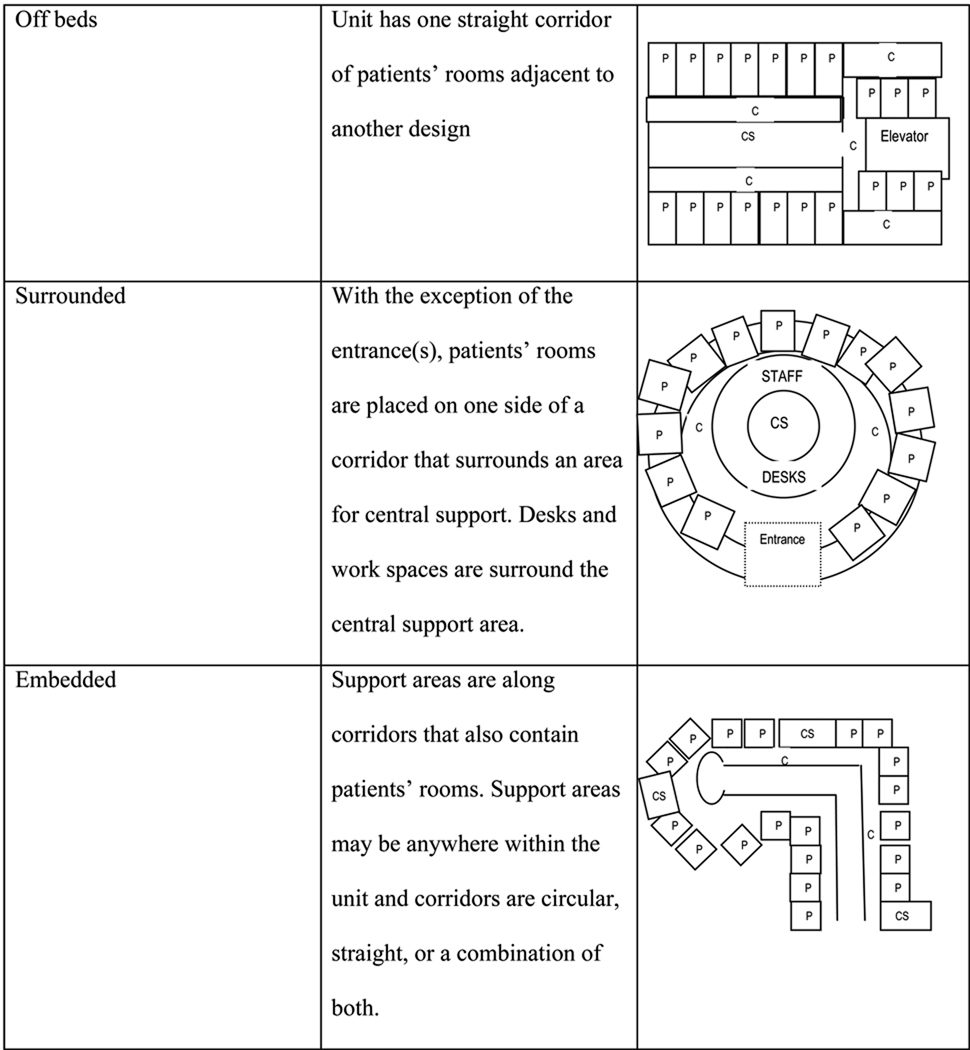
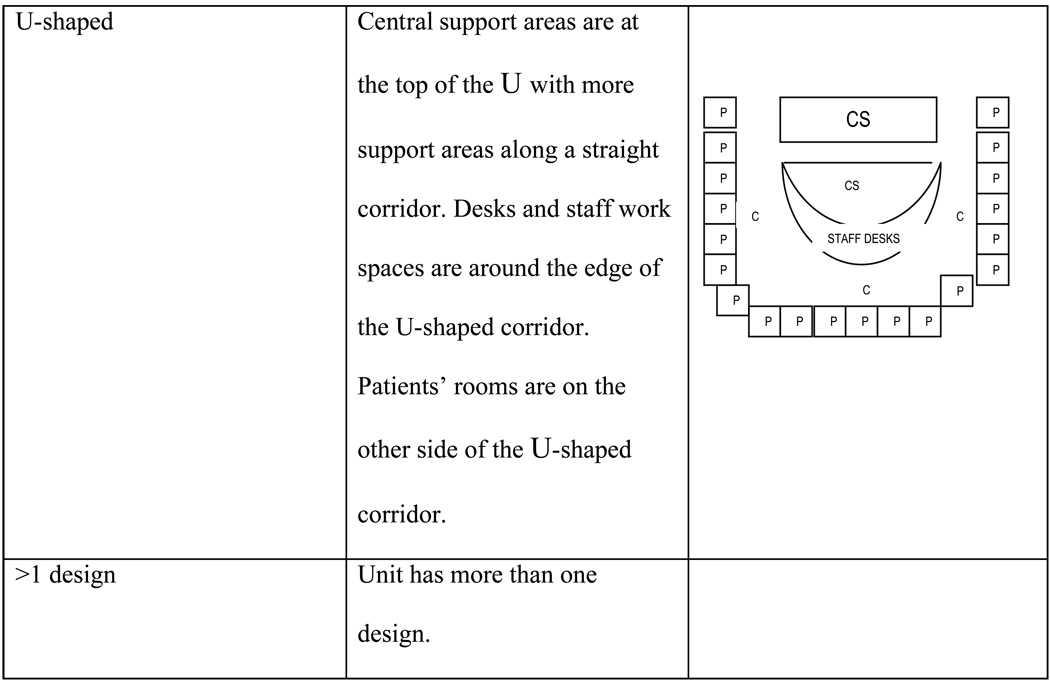
In all, 42 units were coded as the same type by all three raters. In a second group session, consensus about an additional 14 units was reached. Two additional categories were created. The remaining 81 units were coded the same by all investigators. The 11 categories were then analyzed and discussed by the grant's national advisory panel (n = 9), composed of experts in nursing, acute-care medicine, hospital architecture, and safety. Based upon the group's recommendation that differences in three types were minor and unlikely to influence care, the classifications were consolidated into eight types (Figure). Using the eight types, the researchers classified the units with unanimous inter-rater agreement.
Figure.
Characteristics and Sample Illustrations of Unit Design Classifications
Results
Using SPSS (Version 15), we noted that the descriptive results varied by ICU or non-ICU status. We conducted all analyses based on this dichotomy.
Configurations
The variation in distribution among ICUs and M-S units was large (Table 1). Four designs were predominant in ICUs. Four other designs were most prevalent in M-S units. Parallel corridor configurations accounted for 43% of M-S units with "surrounded" and "spokes, no end stations" as distant seconds. ICUs were more diverse with no configuration representing one fourth of the units studied.
Table 1.
Frequency of Distinct Design Configurations by Type of Unit
| Unit typesa | ||
|---|---|---|
| Configuration | N (%) ICUs | N (%) M-S Units |
| Spokes, no end station | 11 (20) | 15 (19) |
| Spokes, end station | 4 (7) | 2 (3) |
| Parallel corridor | 10 (18) | 35 (43) |
| Off beds | 4 (7) | 9 (11) |
| Surrounded | 10 (18) | 13 (16) |
| Embedded | 2 (4) | 5 (6) |
| U-shaped | 13 (23) | 2 (3) |
| > 1 design | 2 (4) | 0 (0) |
| Total | 56 (100) | 81 (100) |
ICU = intensive care units; M-S = adult medical or surgical units.
Private Rooms
The mean percentage of ICU private rooms was 86.7% (SD 28.5) and 43.6% (SD 38.7) in M-S units. The mean number of beds was 17.3 (SD 8.7) in the ICUs; and 32.9 (SD 8.6) in the M-S units. The minimum ICU bed number was 8 and the maximum 47. Comparable statistics for M-S units were 13 and 60.
Patient visibility
The average percentage of beds allowing patients to be seen was 63.4% (SD 31.2) in the ICUs and 5.3% (SD 14.7) in M-S units.
Carpeting
Main corridors were carpeted in 20% (n = 11) of ICUs and 39.5% (n = 32) of M-S units. We noted carpet in less than 5% of all patient rooms. Almost all were in M-S units. Within these units, not every room was carpeted.
Distances
Almost every unit had hand-hygiene facilities within 10 feet of every bed. No differences were noted between ICUs and M-S units. The average distance from bedside to a body-waste disposal facility was 14 feet (SD 14.5) in ICUs versus 11.9 (SD 10.6) in M-S units. This difference was because M-S rooms were slightly more likely to have an en-suite toilet than were ICU rooms. The M-S unit mean distance to supplies (52.6 feet; SD 30.6) was much greater than in ICUs (18.2 feet, SD 17.9). The average distance to charting materials in M-S units (27.6 feet, SD 22.3) was more than double that of ICUs (12.5 feet, SD 19.8). Almost all differences were because of the greater likelihood that room-based supplies (83% of ICUs versus 17% in M-S units) and room-based computers or paper charting facilities were provided for each ICU room.
Intra-hospital and intra-unit variation
In the 14 hospitals in which we studied two ICUs, three had the same configurations for both ICUs. Of the 38 hospitals for which data for two M-S units were available, 16 (42%) had the same unit configuration. ICU pairs had the same "carpet in hallway" status in 13 of the 14 hospitals; this was also the case in 35 of the 38 M-S unit pairs. In 12 of the 14 hospitals in which two ICUs were studied, less than 10 feet of difference in average distance to the charting facility was noted. In 11 of the 14 hospitals, the ICU pairs were also very similar concerning the distance to dispose of body waste. In 6 of the 14, the distance to supplies was similar.
When differences between ICU pairs were noted, they tended to be significant. In 5 hospitals the differences between the average distance to supplies was more than 20 feet. Although mean distances to charting facilities and body-waste disposal sites were similar for almost all M-S pairs, average distance to supplies was different by 10 or more feet in half of the hospitals. In 3 hospitals, the mean difference between the M-S unit pairs was more than 40 feet. Unit differences within hospitals were usually related to (a) placement of units in buildings or wings of different designs and (b) the tendency to refit previously identical units. Some units had converted patient rooms to supply rooms. Some units had mobile computers while others in the same institution did not.
Variation in AHRQ recommended facilities by configuration status (Table 2). The carpeting of main hallways was not associated with configuration status. The ICUs that were configured as "spokes, no end stations" had the longest combined average distances from bed to supplies, charting, and waste disposal. They also had a smaller percentage of rooms that provided visibility. In M-S configuration comparisons, the U-shape, found on only two units, was clearly an outlier for combined distances and had the smallest percentage of private rooms. The "parallel corridor open/closed" and "surrounded" configurations had larger percentages of beds that met the visibility criteria because at least one bed directly across from the charting area was such that the room door swung in a direction that allowed a view of the top of the bed. More rooms would have had good visibility if the doors were re-hung.
Table 2.
Unit Design Category and Selected Design Features
| Mean (SD) |
||||
|---|---|---|---|---|
| SCW | % Private Room Beds |
% Visible | No. Beds | |
| ICU | ||||
| Spokes, no end station (n = 11) | 66.4 (45.8) | 80.6 (36.0) | 48.3 (42.0) | 19.0 (12.1) |
| Parallel corridor (n = 10) | 37.5 (19.8) | 90.1 (25.0) | 69.8 (30.3) | 17.0 (7.5) |
| Surrounded (n = 10) | 43.6 (23.5) | 97.7 (7.0) | 63.4 (35.5) | 17.6 (4.2) |
| U-shaped (n = 13) | 38.6 (22.9) | 84.1 (34.0) | 64.2 (24.8) | 14.6 (6.3) |
| Other (n = 12) | 40.7 (34.0) | 86.7 (29.0) | 71.0 (25.5) | 18.9 (11.3) |
| M-S unit | ||||
| Spokes, no end station (n =1 5) | 97.5 (30.3) | 52.2 (37.6) | <1 | 36.9 (8.3) |
| Parallel corridor (n = 35) | 98.0 (47.2) | 31.2 (32.7) | 9.2 (20.6) | 31.9 (9.2) |
| Surrounded (n = 13) | 84.8 (46.9) | 55.3 (44.3) | 7.1 (11.7) | 27.9 (7.1) |
| Off beds (n = 9) | 135.0 | |||
| 65.0 | 15.6 (4.4) | 1.5 (2.2) | 27.9 (7.1) | |
| Other (n = 9) | 80.8 (31.4) | 77.0 (40.0) | <1 | 39.1 (6.5) |
Note. The mean SCW is the sum measured in feet of the average distance from a patient bed to clean supplies, charting facility, and body-waste disposal. The percentage of beds in private rooms was calculated by dividing the number of private-room beds by all beds. Visibility was calculated by dividing the number of beds that allowed a view of the patient’s head and hands (upper third of body) from a charting area. Bed is any bed deemed to be in use or eligible for use at the time of the study.
Discussion and Recommendations
The study is limited in that we studied units in non-federal hospitals of more than 99 average daily census in urban areas. Smaller, rural and federal hospitals may use different designs and have a different frequency of desirable characteristics. The design did not allow for examining every unit, thus the degree to which design differences within a single institution may be understated. The study design did not allow for including other design aspects (e.g., acoustical tile, air filtration, grab-bars, sitting stations in hallways, and artwork) noted by AHRQ as improving outcomes (AHRQ, 2007).
A strength of this study was reliance on personal measurement rather than reliance on architectural plans. Although unit leaders supplied us with schematic pictures or blueprints, in no case was the printed design fully implemented. The most common deviations were conversions of double to single rooms, conversion of patients' rooms to storage or work areas, addition of viewing glass, and computing stations in corridors.
Opportunity for improvement
The results show that there is opportunity for improvement on almost every AHRQ design variable studied with the exception of hand hygiene. A wide gap exists in desirable characteristics between ICUs and M-S units, indicating that greater emphasis should be placed on M-S unit improvement.
Among the designs, the "spokes, no end station" had the longest distances, worst visibility, and fewest private rooms. This design is one that should require much scrutiny before being adopted in new designs. Although others (Hendrich et al., 2004; Page & Page, 2004) have noted that parallel corridors often require more walking, this was not true in our study of ICUs. We believe this discrepancy is because of (a) the tendency to place supplies and charting materials within patients' rooms, (b) the placement of multiples of the same work area along the inner supply rectangle, and (c) the relatively small unit size. In contrast, the parallel corridor design on large M-S units was found to have among the longest walking distances. Our recommendation is to consider the potential interaction of bed capacity with configuration in future research.
Based on the large variation of characteristics such as number of beds, distance to supplies, charting, and waste disposal within each design category, we do not recommend that design configuration be used as an unadjusted variable. For example, a great difference probably exists in the amount of walking required on a "parallel-corridor" unit that serves 46 patients in private rooms with only one nursing station versus a parallel-corridor unit that serves 24 patients and has provisions for charting in each room.
Relationship of IOM-cited design categories and study classifications
We did not note any courtyard or duplex designs. No unit met all of the criteria of a simple open (Nightingale) form because no unit was only a completely open ward. In many units that did have placement of glass-walled rooms across from nursing station/staff work space (e.g., surrounded design) the service areas were behind the nursing stations, not located off the unit as defined in the simple open design. The "U shape" designs we noted were not simple open design because not all patients were in wards.
No corridor (continental) designs specified as having four to six beds per room were noted. The "embedded design" was similar in that rooms were placed along corridors of various configurations (squares, rectangles, triangles, and combinations thereof) but different in that nursing stations, work areas, and other support areas were placed at many locations around the unit. The IOM-cited radial design has characteristics much like our "surrounded" and "U-shaped" categories in that all include a greater opportunity to view every patient but in most not every patient could be seen from the nursing work area. The double corridor (racetack) was not noted, although it has many similarities to the "parallel corridor" category. The chief difference was that in the "parallel corridor" units, we did not find a single nursing station. At least two were present in other situations and many ends of corridors and patients' rooms had been converted to stations. In a few cases, additional supply rooms were created from what had been patients' rooms at the ends of corridors.
Two configurations that have not been described before are "off beds" and "more than one configuration." These unit types deserve special consideration in future studies. We noted that the "off beds" design usually resulted in greater walking distances for nurses assigned to the off-beds corridor than those of nurses assigned to the basic design area. The difference was because of the need to return to the basic-design area for supplies and charting. For example, one ICU had a surrounded design on one floor (the original ICU) and a half-parallel corridor on another floor (opened to respond to increased ICU demand). Nurses were assigned regularly between the two areas and some supplies could only be obtained from the original unit because of inadequate storage on the expanded portion. Unit leaders told us that the presence of more than one design was usually because of fiscal or census pressures.
One recommendation for researchers interested in the role of nurse labor on patient outcomes is to explore how unit design elements can be operationalized as risk adjustments. Variation within hospitals leads us to recommend that any risk adjustment be made on a unit, not hospital or service, basis. All investigators face the challenge of determining if the resources studied in this project and those identified by IOM leaders and other safety initiatives are clustered. If design clusters exist, the cluster may exert more influence on outcomes than any single element. A new paradigm for studying nurse-sensitive outcomes could emerge.
Although new building programs are subject to many design standards, the question about what to do with the many units that will not be remodeled or replaced soon remains. Although design features such as carpeting may be added relatively easily, others, such as private rooms, are more difficult to obtain within the limitations of a fixed-wall environment, especially if high bed demand exists. Some features could be attained at only moderate expense; e.g., increase visibility by rehanging doors.
Identifying priorities for these actions within a resource-constrained health care system is necessary. Future researchers should provide comparisons of resource investments by outcome. Our observation that personnel on units had already started to change the physical environment indicates that staff members have begun to seek solutions. What is missing is research that can show estimates not only of how these changes may influence outcomes but also how multiple design elements influence one another. Nurse researchers have a vital role in informing hospital and nursing administrators as well as funders about this topic. Although architects, system designers, and others have important roles in determining hospital design, nurse researchers bring special insight into identifying clinical and workforce issues that may influence the utility of any design and, ultimately, patient outcomes.
Acknowledgements
The project was supported by Grant 1R01AG19715-01 from the National Institute on Aging. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Institute on Aging, NIH.
Contributor Information
Cathy Catrambone, Gamma Phi, Assistant Professor, College of Nursing; Rush University, Chicago, IL.
Mary E. Johnson, Gamma Phi, Associate Professor, College of Nursing; Rush University, Chicago, IL.
Lorraine C. Mion, Alpha Mu, Independence Professor of Nursing, School of Nursing; Vanderbilt University, Nashville, TN.
Ann F. Minnick, Gamma Phi, Chenault Professor of Nursing, School of Nursing; Vanderbilt University, Nashville, TN.
References
- Agency for Healthcare Research and Quality. Transforming hospitals: Designing for safety and quality. 2007 Retrieved <date>, from http://www.ahrq.gov/qual/transform.htm.
- Anjali J. The impact of light on outcomes in healthcare settings. Concord, CA: The Center for Health Design; 2006a. [Google Scholar]
- Anjali J. The impact of the environment on infections in healthcare facilities. Concord, CA: The Center for Health Design; 2006b. [Google Scholar]
- Anjali J. The role of the physical and social environment in promoting health, safety, and effectiveness in the healthcare workplace. Concord, CA: The Center for Health Design; 2006c. [Google Scholar]
- Hamilton K. The four levels of evidence-based practice. Healthcare Design. 2003;3(4):18–26. [Google Scholar]
- Hendrich AL, Fay J, Sorrells AK. Effects of acuity-adaptable rooms on flow of patients and delivery of care. American Journal of Critical Care. 2004;13(1):35–45. [PubMed] [Google Scholar]
- James WP, Tatton-Brown W. Hospitals: Design and development. Oxford, GB: Architectural Press; 1986. [Google Scholar]
- Minnick A, Roberts MJ, Curran CR, Ginzberg E. What do nurses want? Priorities for action. Nursing Outlook. 1989;37(5):214–218. [PubMed] [Google Scholar]
- Minnick AF, Roberts MJ, Young WB, Kleinpell RM, Marcantonio RJ. What influences patients' reports of three aspects of hospital services? Medical Care. 1997;35(4):399–409. doi: 10.1097/00005650-199704000-00009. [DOI] [PubMed] [Google Scholar]
- Minnick AF, Mion LC, Johnson ME, Catrambone C, Leipzig R. Prevalence and variation of physical restraint use in U.S. acute-care settings. Journal of Nursing Scholarship. 2007;39(1):30–37. doi: 10.1111/j.1547-5069.2007.00140.x. [DOI] [PubMed] [Google Scholar]
- Nelson C, West T, Goodman C. The hospital built environment: What role might funders of health services research play. Washington, DC: U.S. Department of Health and Human Services; 2005. [Google Scholar]
- Page A, Page AEK. Keeping patients safe: Transforming the work environment of nurses. National Academy Press; 2004. [PubMed] [Google Scholar]
- Rashid M. A decade of adult intensive care unit design: A study of the physical design features of the best-practice examples. Critical Care Nursing Quarterly. 2006;29(4):282–311. doi: 10.1097/00002727-200610000-00003. [DOI] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation. Evidence-Based hospital design improves healthcare outcomes for patients, families, and staff. Princeton, NJ: Author; 2004. [Google Scholar]
- Ulrich R, Xiaobo Q, Zimring C, Anjali J, Choudhary R. Abstracts table supplement. Princeton, NJ: Robert Wood Johnson Foundation; 2004. The role of the physical environment in the hospital of the 21st century: A once-in-a-lifetime opportunity. [Google Scholar]