Abstract
Background
Frontotemporal dementia spectrum disorders are a set of neurodegenerative disorders affecting the frontal and anterior temporal lobes. They are often fatal, and currently no medications have been shown to slow their progression. Recent developments in understanding these disorders may aid in developing treatments.
Objective
To discuss the development of drug therapies for frontotemporal dementia spectrum disorders, both those under current investigation and those that could be targets for future investigation.
Methods
This review is divided into four sections: First, a brief review of frontotemporal dementia spectrum disorders; second, a discussion of the challenges in the development of drug therapies third, a review of the current clinical trials; and finally a discussion of some recent discoveries, which have sparked new areas of investigation.
Conclusions
Hopefully, advances in understanding of frontotemporal dementia spectrum disorders and clinical trial design will aid the development of new treatments.
Keywords: frontotemporal dementia, medication treatment, neurodegenerative disorders, neuroprotection
1. Background
Frontotemporal dementia (FTD) spectrum disorders refers to a set of progressive neurodegenerative processes affecting primarily the frontal lobes and/or anterior temporal lobes (Figure 1) [1]. They are clinically defined syndromes, including behavioral-variant FTD, primary progressive aphasia, and semantic dementia, that can be associated with several different neuropathologies [1–3]. In this review, we will refer to FTD spectrum disorders as ‘FTD’ and to a specific disorder by its name (e.g., behavioral variant FTD). As one would expect from the brain areas affected, the symptoms of FTD include personality and behavior changes [4], language dysfunction [5,6], and cognitive dysfunction [7], especially in the areas of executive function [8] and social cognition [9,10]. The prevalence of FTD is between 3.6 (in 50- to 59-year-olds) [11] and 15 (in 45- to 64-year-olds) [12] cases per 100,000. In persons under 65, FTD is the second most common type of dementia [13].
Figure 1.
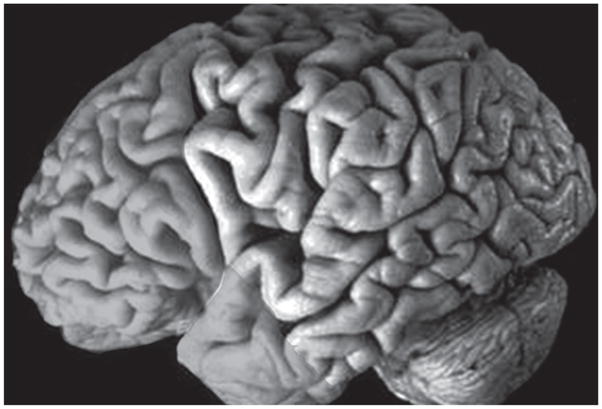
Brain areas typically affected in frontotemporal dementia (prefrontal cortex and anterior temporal lobes).
Patients with FTD are sometimes separated into those with primarily behavioral symptoms (called behavioral or frontal variant FTD (fvFTD)) and those with primarily language symptoms (primary progressive aphasia) [14]. Those with language dysfunction are frequently subdivided depending on whether they display predominantly a non-fluent (progressive non-fluent aphasia [PNFA]) or a fluent (semantic dementia) aphasia [14]. A third language variant, logopenic progressive aphasia, is used in some classifications [15]. It is characterized by slow speech and impaired syntactic comprehension and naming.
The different clinical presentations of FTD are associated with pathology affecting different brain areas. The primarily behavioral presentation of FTD has been associated with degeneration in the frontal lobes (thus the term ‘frontal variant’) [16]. However, some evidence suggests that anterior temporal lobe degeneration is associated with its own behavioral syndrome corresponding to the functions of this region [17–19]. PNFA has been associated with atrophy in the left inferior frontal cortex and insula, semantic dementia with anterior temporal and perirhinal damage [20], and logopenic progressive aphasia with atrophy in the left posterior temporal cortex and inferior parietal lobule [15].
Patients with FTD usually demonstrate atrophy, often severe, in frontal or anterior temporal lobes or both on gross neuropathological examination [3,21]. Macroscopic atrophy of basal ganglia and loss of pigmentation in the substantia nigra is observed in some cases. The pattern and extent of the atrophy usually reflects the severity and duration of the disease. Immunohistochemistry is used to identify the different pathological subtypes that can cause the clinical presentation of FTD. In most cases, antibodies label the protein deposits in the brain. However, proteins targeted for degradation are ubiquitinated and a number of neuro-degenerative diseases are characterized by collections of ubiquitinated proteins. The majority of FTD patients show tau-negative, ubiquitinated inclusions (termed FTLD-U) in cells in the affected areas of the cortex [22]. Previously, some of these patients were classified as ‘dementia lacking distinctive histology’ or DLDH. However, recent evidence suggests that the lack of ubiquitin immunostaining in many of these cases may have been due to the low sensitivity of older methods of ubiquitin immunostaining [23]. When these DLDH cases are restained with newer methods, the majority show some ubiquitin immunoreactivity, suggesting that DLDH is a rarer pathologic etiology of FTD than previously thought [23]. The ubiquitinated protein in the inclusions has recently been identified as usually being TAR DNA binding protein (TDP-43) [24,25]. TDP-43 is a nuclear protein that appears to be involved in transcription regulation [24]. TDP-43 has also been identified as a constituent of inclusions associated with sporadic forms of amyotropic lateral sclerosis (ALS) [24]. In one study, 5 of 36 FTD patients met criteria for ALS [26]. The pathologic classification of FTLD-U includes cases of FTD that present with pathological changes associated with motor neuron disease (termed FTLD-MND) [23]. In addition to motor neuron disease, FTD can co-occur with Parkinsonism [27].
The second most common neuropathology associated with the FTD clinical syndrome is characterized by inclusions of hyperphosphorylated tau (including Pick’s disease, characterized by round argyrophilic neuronal cytoplasmic inclusions (Pick bodies) and large ballooned neurons (Pick cells)[28]). A minority of cases with prominent tau pathology is associated with mutations in the microtubule-associated protein tau (MAPT) gene on chromosome 17 and some cases with FTLD-U are associated with progranulin (PGRN) mutations [29]. The majority of patients with fvFTD and semantic dementia have FTLD-U on autopsy [20,29], whereas PNFA is more frequently associated with tau pathology [30]. In the future, the pathological classification of these and related disorders may be split into ‘tauopathies’ and ‘TDP-43 proteinopathies’ [31].
2. Challenges
There are three possible types of efficacious treatments for FTD and other neurodegenerative disorders: Symptomatic treatments that ameliorate symptoms but do not alter the disease course, neuroprotective treatments that slow decline, and treatments that lead to recovery of function. Advantages of symptomatic treatments include that they can improve the quality of life of patients and their families, they can be tested relatively rapidly for efficacy, and they are more likely than disease-modifying treatments to be independent of the underlying pathologic process (a particular problem for FTD, discussed further below). The disadvantage is obvious – they do not affect the underlying disease and probably lose symptomatic efficacy as the illness progresses. Neuro-protective treatments have the advantage of slowing the progression of the illness but generally require long trials to test for efficacy [32]. Treatments that lead to recovery of function are the goal for the development of treatments for neurodegenerative diseases but have so far proven elusive.
The treatments tested so far for FTD have been ‘borrowed’ from those used to treat other illnesses, mostly Alzheimer’s disease and psychiatric illnesses. We reviewed the mechanisms and efficacy of tested treatments for FTD in a previous paper [33]. See also [34] and [35] for further discussion of neurotransmitter-based treatments for FTD. In summary, there is no published data showing evidence of neuroprotection or recovery of function for any of the agents tested and weak evidence of improvement of behavioral symptoms with the use of certain psychiatric medications [33]. Autopsy, imaging and cerbrospinal fluid studies suggest deficiencies in the serotonergic neurotransmitter system in FTD and FTLD [33,36]. Interestingly, several of the clinical symptoms of FTD (e.g., appetite changes and apathy) can also be observed with serotonergic dysfunction. There is some evidence of dopaminergic abnormalities in FTD as well [33,36] but the cholinergic system appears relatively intact (especially compared with Alzheimer’s disease) [33,36]. Accordingly, although there is variation in clinical practice (e.g., some physicians place FTD patients on cholinesterase inhibitors and memantine), there is no current standard-of-care treatment that all patients with FTD are given. This is in contrast to other neurodegenerative disorders for which there are medications of clear symptomatic efficacy (e.g., Parkinson’s disease), or debatable evidence of neuroprotection (e.g., Alzheimer’s disease).
Some of the challenges for the development of therapeutics for FTD are shared with other neurodegenerative disorders and some are unique to FTD [32]. Shared challenges include the difficulty of regenerating postmitotic neurons, a dearth of intermediate markers of medication efficacy, a lack of understanding of the basic mechanisms of many of these illnesses, and the difficulty developing appropriate cell lines and animal models. Furthermore, resources, including funding and groups of patients to participate in studies, are limited.
One of the greatest challenges of drug development for FTD is the pathological and clinical heterogeneity of the FTD clinical syndrome [3,32]. For many of the symptoms of FTD (e.g., deficits in social cognition), there is currently a dearth of good measures. In addition, many of the measures used to study FTD were developed primarily for Alzheimer’s disease (e.g., the Neuropsychiatric inventory (NPI) [37]) and may not fully capture the symptom profile of FTD. Behavioral symptoms may be more subject to placebo effect than, for example, motor measures [38]. Finally, the behavioral symptoms of FTD can make participation in lengthy therapeutic trials difficult.
The pathological heterogeneity of FTD is a central issue in the development of new drug therapies for FTD [32]. Disease-modifying or recovery-of-function treatments will probably be specific to certain pathological processes. With the exception of some relatively uncommon clinical presentations (e.g., FTD-MND, familial cases where the pathology in the family is known), the clinical presentation does not indicate the neuropathological process. This is likely to be a less important issue if a relatively benign treatment is developed, in which case all FTD patients will probably be given the treatment with the knowledge that it will help only a minority of the patients. However, it becomes a more pressing issue if treatments for FTD are developed that are associated with significant toxicity. Furthermore, without an in vivo indication of the underlying pathological process affecting FTD patients, clinical trials of treatments that are specific to a given neuropathologic process will require larger number of subjects to be sufficiently powered than if subjects can be selectively included on the basis of their underlying pathological process [32]. Language variant FTD may be more commonly associated with Alzheimer’s pathology than behavioral variant FTD [39]. But if so, it represents an unusual spatial topography for Alzheimer’s disease, which may make topographically related treatments for Alzheimer’s disease less effective for these patients.
3. Current clinical trials in FTD
Several agents are under current clinical investigation for FTD. In this section we review the rationale for some of these medications. These trials are all reported in ClinicalTrials.gov.
3.1 Memantine (Namenda)
Memantine was developed for the treatment of Alzheimer’s disease. However, its mechanism of action, low-to-moderate affinity noncompetitive N-methyl-D-aspartate (NMDA) antagonism [40], is not specific to Alzheimer’s disease and could transcend specific neuropathologies in FTD [33]. An initial open-label trial was completed [41] and there is an ongoing multicenter, randomized, double-blind, placebo-controlled investigation of memantine for FTD funded by Forest Laboratories [42]. In addition to this trial, a French Phase II investigation is currently being conducted [43].
3.2 Galantamine
A Phase II trial, sponsored by Janssen-Ortho Inc., (Canada) and Johnson & Johnson, to test the safety, tolerability, and efficacy of galantamine for FTD was recently completed [44]. Galantamine is a cholinesterase inhibitor which appears to also allosterically modulate nicotinic cholinergic receptor sites. This nicotinic modulation appears to modulate the release of other neurotransmitters, including serotonin, which has been demonstrated to be deficient in FTD [33]. They found galantamine not to be effective for fvFTD but observed a possible trend of efficacy in the aphasic subgroup [44].
3.3 Dopaminergic treatments
Two trials are investigating the augmentation of the dopaminergic neurotransmitter system to improve symptoms in FTD. The dopamine system is of interest in FTD for several reasons: There is PET and autopsy evidence of dopaminergic deficiencies in FTD (reviewed in [33]), up to 30% of FTD patients show clinical evidence of basal ganglia dopaminergic dysfunction (i.e., Parkinsonism, although the majority of frontotemporal dementia with parkinsonism linked to chromosome 17 (FTDP-17) patients are levodopa-unresponsive) [27], the frontal cortex is richly innervated with dopaminergic receptors [45], and meso-cortical dopaminergic projections influence the cognitive function of the frontal lobes [46]. One of the trials tests the effects of amantadine, a medication that increases the amount of dopamine in the cortex, on behavioral symptoms in FTD [47]. Another currently ongoing trial tests the effects of a medication, tolcapone, that probably increases dopamine selectively in the frontal lobes [48,49] and has shown an effect on executive function in healthy subjects, on behavior, cognition, and functional MRI findings in FTD patients [50,51].
4. The effect of recent discoveries in FTD
In this section, we review recent discoveries in basic and translational science that could affect the next generation of clinical trials for FTD. We focus on therapeutics that are either currently available, or may soon be available (Table 1), to test in humans rather than areas of research that may hold promise but may not be currently translatable to humans.
Table 1.
Potential treatments for FTD based on recent genetic discoveries about the illness.
| Mutation | Mechanism of potential treatment | Example |
|---|---|---|
| PGRN | Progranulin/granulin supplementation | |
| Immunosuppression | FK506 | |
| Inhibition of TDP-43 aggregation | ||
| MAPT | Glycogen synthase kinase-3 inhibition | Lithium, valproate |
| Microtubule stabilization | paclitaxel |
4.1 Biomarkers and drug discovery
Establishment of new methods for the early diagnosis of FTD is an important step towards development of a tailored therapy and early intervention. Early diagnosis of the pathological process may become possible through detection of biomarkers such as proteins linked to the pathology of the disease in the cerebrospinal fluid and possibly blood, or detection of the protein deposits with MRI or positron emission tomography (PET). There is recent evidence that blood PGRN, and plasma TDP-43, levels can be elevated in neurodegenerative conditions, and low levels may reflect loss-of-function mutations [52,53]. This and similar findings may provide targets for future therapeutic measures.
4.2 Genetics
FTD has been genetically linked to chromosomes 3, 9 and 17 [54]. However, many cases of FTD are not familial [55]. Mutations in the chromatin modifying protein 2B (CHMP2B) gene on chromosome 3 were identified in a large Danish pedigree with FTLD [56]. Mutations in the valosin-containing protein (VCP) gene on chromosome 9p21-12 have been reported to cause inclusion body myopathy with Paget’s disease of bone and frontotemporal dementia (IBMPFD) [57]. Previously, linkage of families with autosomal dominant FTD to a 9.8 Mb region on chromosome 9p13.2-21.3 has been reported [58,59] with no mutation in VCP. In a recent study, multiple families with FTD and ALS were shown to have various mutations in the IFT74 gene on 9p21.2 [60]. There have been reports of a gene for ALS being localized on chromosome 9q34 [61] and linkage of familial amyotropic lateral sclerosis with frontotemporal dementia on chromosome 9q21-q22 [62], which could not be replicated in other studies [63].
Mutations in two genes on chromosome 17 have been associated with FTLD. Mutations in MAPT are responsible for 10 – 20% of familial FTD cases and all the mutation carriers have MAPT pathology [64]. However, there were a large number of families with linkage to chromosome 17q21 with no MAPT mutation and no significant tau pathology [65]. Recently, the identification of PGRN gene on chromosome 17, showed that mutations in this gene can be responsible for illness in these families [66]. As mutations in MAPT and PGRN are the most frequent genetic causes of FTD known to date, we continue with more detailed discussion of these two genes.
4.2.1 MAPT
MAPT is located on chromosome 17q21. The gene spans ~120 kb and consists of 16 exons [67]. Over 30 MAPT mutations have been identified [68]. Tau protein is predominantly expressed in neurons of the peripheral and central nervous system. The role of tau protein is stabilizing microtubules, providing neuronal polarity and signal transduction [69]. In the adult human nervous system the alternative splicing of exons 2, 3 and 10 results in six different transcripts. As exon 10 encodes one of the four microtubule binding domains of the tau protein, the alternative splicing of exon 10 creates two types of protein; proteins with three (exon 10 –, 3R) or four (exon 10+, 4R) microtubule binding domains. In normal adult brain the ratio of 3R/4R is ~ 1. In the neurological disorders associated with tau (tauopathies), neurofibrillary tangles are pathological hallmarks of the disease. However, in different tauopathies, the ratio of 3R/4R in tangles is not 1. In AD, tangles are made of both 3R and 4R tau with predominance of 3R tau [70]. In progressive supranuclear palsy (PSP), corticobasal degeneration (CBD), agyrophilic grain disease (AGD) and FTDP-17, the insoluble tangles are mainly composed of 4R tau [71–73]. The intronic sequences flanking MAPT exon 10 have an unusual structure which differs from the splicing consensus sequence. Mutations in the 5′ and 3′ splice sites, as well as some exonic mutations, change the inclusion of exon 10 in MAPT transcript. At the 5′ of exon 10, a mutation at position – 10 has been identified in a FTD patient [74]. This mutation causes overexpression of 4R tau. Mutations affecting splice site at the 3′ site of exon 10, generally strengthen the weak splice site, resulting in inclusion of exon 10 in transcript [75,76]. Besides the intronic mutations, coding mutations also affect the splicing of exon 10. The dK280 mutation leads to increase of the 3R tau [77]. The N279K mutation increases the inclusion of exon 10 in TAU transcript [78]. Among other mutations in the coding region of exon 10 are the P301P, P301L and P301S, affecting the amino acid P301. As the P301P is a non pathogenic mutation, P301L causes a less aggressive phenotype than P301S [79]. These mutations display a strong inhibitory effect on tau-promoted microtubule assembly [80,81] and promote tau assembly into filaments [82] but do not affect the splicing of exon 10.
4.2.2 Progranulin
Mutations in the PGRN gene on chromosome 17 have been associated with FTD and FTLD-U pathology [66]. Approximately 5% of patients seen in the community, and 15% of patients seen at tertiary referral centers, have a known PGRN mutation [83]. The progranulin protein undergoes post-translational splicing resulting in preserved ‘granulin’ domains [84]. The difference in function between the full-length and spliced proteins is not yet fully understood [84]. Progranulin is expressed in many tissues throughout the body, especially in cells with a high mitotic rate [85]. There is evidence that progranulin can act as a growth factor [86,87] and is involved in wound healing [88]. High PGRN expression is associated with more aggressive tumor growth [87]. Although further evidence is needed, some have hypothesized that progranulin can act as a nerve growth factor and that it may be involved in CNS inflammation [84].
The phenotype and pathology associated with PGRN mutations continues to be elucidated. Recent reports indicate that PGRN mutation carriers can have clinical syndromes including FTD (63%), primary progressive aphasia (PPA), corticobasal degeneration syndrome (CBDS), Lewy body dementia, or Alzheimer’s disease [89]. PGRN mutation carriers had hallucinations, apraxia and amnesia more often than other FTD patients [89,90]. Mean age of onset was greater for PGRN mutation carriers than MAPT mutation carriers [90,91]. Pathologically, cases with PGRN mutations showed extensive type 3 TDP-43-positive pathology, including neuronal cytoplasmic and intranuclear inclusions and dystropic neurites [91].
The discovery that mutations in the PGRN gene can result in FTD has already had important implications for the development of treatments for FTD. First, all of the mutations found to date appear to result in a loss of function of one of the PGRN alleles, that is, lead to haploinsufficiency of the production of progranulin throughout the lives of persons with the mutation which, for unknown reasons, does not manifest clinically until mid-life [84]. While there are significant technical and safety concerns to address, the mechanism of PGRN mutations (haploinsufficiency) suggests that symptoms could possibly be prevented or ameliorated if progranulin can be supplemented in the presymptomatic phase in mutation carriers. The development of animal models with progranulin haploinsufficiency will be important for this research to develop.
Another implication of the association between PGRN and FTD is that it could enable investigators to collect a group of living subjects that has the FTLD-U pathology. This could be useful for testing treatments that are specifically targeted to this pathology [32]. Conversely, PGRN mutation carriers could be excluded from trials of tau-specific treatments.
4.3 Tau kinases
Several kinases phosphorylate tau, some at specific sites, while others can phosphorylate tau at several sites, although with different efficiencies at different sites [92]. One kinase that has received attention as a potentially therapeutic target for FTD is glycogen synthase kinase-3 (GSK-3) [93]. GSK-3 phosphorylates tau and may have effects on neuron survival independent of tau [94]. In cell cultures, lithium [95] and valproic acid [96], two drugs that are currently FDA approved for use in other illnesses, inhibited GSK-3. Also, in a mouse model, administration of lithium resulted in decreased tangle formation [97–99]. The interest in the use of lithium as a potential treatment for FTD was increased by an open-label study that showed preservation of function and decreased mortality associated with lithium augmentation treatment in patients with ALS [100].
There are several issues to consider in the potential therapeutic use of lithium for FTD, however. Its mechanism is complex [101] and has several actions besides GSK-3 inhibition such as inositol depletion [102], as well as direct effects on second messenger [103] and neurotransmitter systems such as serotonin receptors [104,105]. Tolerability can be low, especially in the elderly [106]. Even in younger persons, the side effect profile is unfortunate for its potential for therapeutic use in FTD; lithium impairs executive function and inhibition in euthymic bipolar subjects [107]. Even if one posits that the negative effects of lithium on cognition reflects a side effect that does not affect its potential neuroprotective effect, any trial of lithium would have to provide protection over a sufficient amount of time to overcome the negative initial effects of lithium on frontal lobe function. Valproic acid, which has also been proposed as a possible therapeutic agent for FTD, also negatively affects cognition in the psychiatric populations in which it has been used [108].
4.4 Microtubule stabilization
Given the apparent negative effect of tau hyperphosphorylation on microtubule stability, there has been interest in agents that can stabilize microtubules [93]. One such agent is paclitaxel (Onxol, Taxol), a medication used to treat certain types of neoplasm that promotes microtubule assembly by enhancing the action of tubulin dimers [109]. A disadvantage of paclitaxel is that it can be associated with significant toxicity, including bone marrow suppression [109].
4.5 Inflammation
The potential role of progranulin in inflammation suggests that inflammation may play a role in FTD and anti-inflammatory agents may have efficacy to decrease progression of FTD [110]. One trial showed a protective effect of the immunosuppressant FK506 in tau transgenic (tg) mice [111].
4.6 TDP-43
Similarly, the discovery of TDP-43 has been a major advance in our knowledge of FTD that has implications for the development of treatments. First, it may help elucidate the mechanism with which the rarer genetic associations with FTD such as mutations in valosin-containing protein (VCP) result in illness – there is some evidence that mutations in this gene affect the TDP-43 system [112]. Second, medications that inhibit the aggregation of TDP-43, although to our knowledge there are none currently known, could have efficacy for FTD in patients with FTLD-U, in addition to other ‘TDP-43 proteinopathies’.
5. Conclusions/expert opinion
Developing treatments for FTD is difficult, as evidenced by lack of successful treatments to date. Other authors have stressed the importance of objective standardized criteria for diagnosis, standardized outcome measures in order to compare trials, an adequate number of subjects to sufficiently power trials (probably requiring multi-center collaboration), a sufficient trial duration, and the presence of control conditions [32]. We agree with these points; small, uncontrolled clinical trials of therapeutics for FTD are subject to placebo (especially for behavioral symptoms) and publication bias and are thus difficult to interpret [33]. We also agree that standardization of outcome measures and diagnostic criteria is very useful for trial design. Ideally, standard measures should have flexibility in order to incorporate advances in the design of measures. For example, the cognitive battery tested by Knopman et al. [33] does not currently include measures of social cognition. Hopefully, valid measures of this important area of deficiency in FTD will be developed in the coming years and integrated into clinical trials.
Consensus research criteria for FTD have been proposed [14], which should be helpful for trial design and the development of standardized diagnostic tools. We believe, however, that the criteria for behavioral variant FTD should have a specific exclusion criterion that the symptoms are not better accounted for by a psychiatric illness. Psychiatric illness is commonly a differential diagnosis of FTD, and FTD is frequently initially misdiagnosed as psychiatric illness [113]. As currently written [14] many, if not most, patients with Major Depressive Disorder would meet criteria for probable or possible FTD [114].
While we agree with the assertion by other authors that standardization of trial design will increase the utility of future trials, knowledge of the characteristics of the drug to be tested should also be integrated into trial design. As stated above, lithium and valproic acid trials may need to be longer than trials of other potentially neuroprotective agents to ‘overcome’ the initial negative effects of these medications on cognition. Furthermore, medications that have been tested in other populations can provide data to allow more exact power calculations for FTD trials, as our laboratory did in the design of a trial for the use of tolcapone in FTD [51]. Another example of using already gathered information to inform clinical research on FTD would be an epidemiological study of the incidence of FTD and AD in the thousands of people that have been taking lithium for bipolar disorder. This could be undertaken with the hypothesis that if lithium is truly neuroprotective, these people should have a lower incidence of these tauopathies than patients with bipolar disorder who did not receive lithium. To our knowledge, such a study has not been performed but could provide an initial and relatively inexpensive evaluation of the potential neuroprotective effects of lithium.
Intermediate markers of treatment efficacy are necessary and could increase the efficiency and decrease the costs of clinical trials for FTD. While a review of potential biomarkers for FTD is beyond the scope of this review, development of imaging biomarkers will be dependent on the testing of imaging techniques combined with a greater understanding of the neuropsychology of FTD; An evaluation of the imaging findings associated with treatment efficacy requires knowledge of the brain areas associated with symptoms. Imaging technologies could also aid clinical trials by helping to recruit pathologically homogenous groups of patients [115].
In summary, we hope that a balance of standardization and innovation in clinical trial design for FTD will provide the best means to test therapeutic options for this devastating illness.
Acknowledgments
This study was supported by the intramural program of The National Institutes of Health/The National Institute of Neurological Disorders and Stroke.
Footnotes
Declaration of interest
The authors declare no conflicts of interest and have received no payment for the production of this manuscript.
Bibliography
Papers of special note have been highlighted as either of interest (•) or of considerable interest (••) to readers.
- 1.Lund/Manchester. Clinical and neuropathological criteria for frontotemporal dementia. The Lund and Manchester Groups. J Neurol Neurosurg Psychiatry. 1994;57:416–8. doi: 10.1136/jnnp.57.4.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neary D, Snowden JS, Gustafson L, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51:1546–54. doi: 10.1212/wnl.51.6.1546. [DOI] [PubMed] [Google Scholar]
- 3.McKhann GM, Albert MS, Grossman M, et al. Clinical and pathological diagnosis of frontotemporal dementia: report of the Work Group on Frontotemporal Dementia and Pick’s Disease. Arch Neurol. 2001;58:1803–9. doi: 10.1001/archneur.58.11.1803. [DOI] [PubMed] [Google Scholar]
- 4.Le Ber I, Guedj E, Gabelle A, et al. Demographic, neurological and behavioural characteristics and brain perfusion SPECT in frontal variant of frontotemporal dementia. Brain. 2006;129:3051–65. doi: 10.1093/brain/awl288. [DOI] [PubMed] [Google Scholar]
- 5.Knibb JA, Hodges JR. Semantic dementia and primary progressive aphasia: a problem of categorization? Alzheimer Dis Assoc Disord. 2005;(19 Suppl 1):S7–14. doi: 10.1097/01.wad.0000183085.22562.13. [DOI] [PubMed] [Google Scholar]
- 6.Mesulam MM. Primary progressive aphasia–a language-based dementia. N Engl J Med. 2003;349:1535–42. doi: 10.1056/NEJMra022435. [DOI] [PubMed] [Google Scholar]
- 7.Libon DJ, Xie SX, Moore P, et al. Patterns of neuropsychological impairment in frontotemporal dementia. Neurology. 2007;68:369–75. doi: 10.1212/01.wnl.0000252820.81313.9b. [DOI] [PubMed] [Google Scholar]
- 8.Elderkin-Thompson V, Boone KB, Hwang S, Kumar A. Neurocognitive profiles in elderly patients with frontotemporal degeneration or major depressive disorder. J Int Neuropsychol Soc. 2004;10:753–71. doi: 10.1017/S1355617704105067. [DOI] [PubMed] [Google Scholar]
- 9.Wittenberg D, Possin KL, Rascovsky K, et al. The early neuropsychological and behavioral characteristics of frontotemporal dementia. Neuropsychol Rev. 2008;18:91–102. doi: 10.1007/s11065-008-9056-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neary D, Snowden J, Mann D. Frontotemporal dementia. Lancet Neurol. 2005;4:771–80. doi: 10.1016/S1474-4422(05)70223-4. [DOI] [PubMed] [Google Scholar]
- 11.Rosso SM, Donker Kaat L, Baks T, et al. Frontotemporal dementia in The Netherlands: patient characteristics and prevalence estimates from a population-based study. Brain. 2003;126:2016–22. doi: 10.1093/brain/awg204. [DOI] [PubMed] [Google Scholar]
- 12.Ratnavalli E, Brayne C, Dawson K, Hodges JR. The prevalence of frontotemporal dementia. Neurology. 2002;58:1615–21. doi: 10.1212/wnl.58.11.1615. [DOI] [PubMed] [Google Scholar]
- 13•.Bird T, Knopman D, VanSwieten J, et al. Epidemiology and genetics of frontotemporal dementia/Pick’s disease. Ann Neurol. 2003;54:S29–31. doi: 10.1002/ana.10572. A good paper on the epidemiology of FTD. [DOI] [PubMed] [Google Scholar]
- 14••.The Clinical Diagnosis and Imaging/Biomarkers Group. Summary and Suggestions for Future Resource Development and Research Initiatives Frontotemporal Dementia Workshop. [Last accessed September 24 2008]; Available from: http://www.ninds.nih.gov/news_and_events/proceedings/Frontotemporal_Dementia_Workshop.htm. A very useful summary document giving expert opinion on priorities for the investigation of FTD. All of the sections are of considerable interest.
- 15.Gorno-Tempini ML, Dronkers NF, Rankin KP, et al. Cognition and anatomy in three variants of primary progressive aphasia. Ann Neurol. 2004;55:335–46. doi: 10.1002/ana.10825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seeley WW, Crawford R, Rascovsky K, et al. Frontal paralimbic network atrophy in very mild behavioral variant frontotemporal dementia. Arch Neurol. 2008;65:249–55. doi: 10.1001/archneurol.2007.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zahn R, Moll J, Krueger F, et al. Social concepts are represented in the superior anterior temporal cortex. Proc Natl Acad Sci USA. 2007;104:6430–5. doi: 10.1073/pnas.0607061104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seeley WW, Bauer AM, Miller BL, et al. The natural history of temporal variant frontotemporal dementia. Neurology. 2005;64:1384–90. doi: 10.1212/01.WNL.0000158425.46019.5C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosso SM, Roks G, Stevens M, et al. Complex compulsive behaviour in the temporal variant of frontotemporal dementia. J Neurol. 2001;248:965–70. doi: 10.1007/s004150170049. [DOI] [PubMed] [Google Scholar]
- 20.Hodges JR, Patterson K. Semantic dementia: a unique clinicopathological syndrome. Lancet Neurol. 2007;6:1004–14. doi: 10.1016/S1474-4422(07)70266-1. [DOI] [PubMed] [Google Scholar]
- 21.Pick A. Uber die Beziehungen der senilen Hirnatrophie zur Aphasie. Prager Medizinische Wochenschrift. 1892;17:165–7. [Google Scholar]
- 22.Cairns NJ, Bigio EH, Mackenzie IR, et al. Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathol (Berl) 2007;114:5–22. doi: 10.1007/s00401-007-0237-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23•.Mackenzie JR, Shi J, Shaw CL, et al. Dementia lacking distinctive histology (DLDH) revisited. Acta Neuropathol. 2006;112(5):551–9. doi: 10.1007/s00401-006-0123-3. A paper that revisits and revises the diagnosis of DLDH. [DOI] [PubMed] [Google Scholar]
- 24.Neumann M, Sampathu DM, Kwong LK, et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science. 2006;314:130–3. doi: 10.1126/science.1134108. [DOI] [PubMed] [Google Scholar]
- 25.Mackenzie IR, Foti D, Woulfe J, Hurwitz TA. Atypical frontotemporal lobar degeneration with ubiquitin-positive, TDP-43-negative neuronal inclusions. Brain. 2008;131:1282–93. doi: 10.1093/brain/awn061. [DOI] [PubMed] [Google Scholar]
- 26.Lomen-Hoerth C, Anderson T, Miller B. The overlap of amyotrophic lateral sclerosis and frontotemporal dementia. Neurology. 2002;59:1077–79. doi: 10.1212/wnl.59.7.1077. [DOI] [PubMed] [Google Scholar]
- 27.Hodges JR, Davies RR, Xuereb JH, et al. Clinicopathological correlates in frontotemporal dementia. Ann Neurol. 2004;56:399–406. doi: 10.1002/ana.20203. [DOI] [PubMed] [Google Scholar]
- 28.Alzheimer A. Uber eigenartige Krankheitsfalle des spate en Alters. Zeitschrift fur die Gesamte Neurologie und Psychiatrie. 1911;4:356–85. [Google Scholar]
- 29.Mackenzie IR, Rademakers R. The molecular genetics and neuropathology of frontotemporal lobar degeneration: recent developments. Neurogenetics. 2007;8(4):237–48. doi: 10.1007/s10048-007-0102-4. [DOI] [PubMed] [Google Scholar]
- 30.Josephs KA, Duffy JR, Strand EA, et al. Clinicopathological and imaging correlates of progressive aphasia and apraxia of speech. Brain. 2006;129:1385–98. doi: 10.1093/brain/awl078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Pathology Working Group. Summary and Suggestions for Future Resource Development and Research Initiatives Frontotemporal Dementia Workshop. [Last accessed September 24 2008]; Available from: http://www.ninds.nih.gov/news_and_events/proceedings/Frontotemporal_Dementia_Workshop.htm.
- 32••.Knopman DS, Boeve BS, Caselli RJ, et al. Longitudinal tracking of FTLD: toward developing clinical trial methodology. Alzheimer Dis Assoc Disord. 2007;21:S58–63. doi: 10.1097/WAD.0b013e31815bf69d. A paper that makes concrete suggestions regarding the investigation of FTD using evidence-based principles. [DOI] [PubMed] [Google Scholar]
- 33.Huey ED, Putnam KT, Grafman J. A systematic review of neurotransmitter deficits and treatments in frontotemporal dementia. Neurology. 2006;66:17–22. doi: 10.1212/01.wnl.0000191304.55196.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Freedman M. Frontotemporal dementia: recommendations for therapeutic studies, designs, and approaches. Can J Neurol Sci. 2007;34:S118–24. doi: 10.1017/s0317167100005680. [DOI] [PubMed] [Google Scholar]
- 35.Merrilees J. A model for management of behavioral symptoms in frontotemporal lobar degeneration. Alzheimer Dis Assoc Disord. 2007;21(4):S64–69. doi: 10.1097/WAD.0b013e31815bf774. [DOI] [PubMed] [Google Scholar]
- 36.Chow TW. Treatment approaches to symptoms associated with frontotemporal degeneration. Curr Psychiatry Rep. 2005;7(5):376–80. doi: 10.1007/s11920-005-0040-5. [DOI] [PubMed] [Google Scholar]
- 37.Cummings JL, Mega M, Gray K, et al. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44:2308–14. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- 38.Dworkin RH, Katz J, Gitlin MJ. Placebo response in clinical trials of depression and its implications for research on chronic neuropathic pain. Neurology. 2005;65:S7–19. doi: 10.1212/wnl.65.12_suppl_4.s7. [DOI] [PubMed] [Google Scholar]
- 39•.Kertesz A, McMonagle P, Blair M, et al. The evolution and pathology of frontotemporal dementia. Brain. 2005;128:1996–2005. doi: 10.1093/brain/awh598. An interesting paper that traces the evolution of FTD spectrum disorder diagnoses. [DOI] [PubMed] [Google Scholar]
- 40.Rogawski MA, Wenk GL. The neuropharmacological basis for the use of memantine in the treatment of Alzheimer’s disease. CNS Drug Rev. 2003;9:275–308. doi: 10.1111/j.1527-3458.2003.tb00254.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diehl-Schmid J, Forstl H, Perneczky R, et al. A 6-month, open-label study of memantine in patients with frontotemporal dementia. Int J Geriatr Psychiatry. 2008;23(7):754–9. doi: 10.1002/gps.1973. [DOI] [PubMed] [Google Scholar]
- 42. [Last accessed September 24 2008]; Available from: www.clinicaltrials.gov/ct2/show/NCT00545974?term=frontotemporal+dementia&rank=
- 43. [Last accessed September 24 2008]; Available from: www.clinicaltrials.gov/ct2/show/NCT00200538?term=frontotemporal+dementia&rank=11.
- 44.Kertesz A, Morlog D, Light M, et al. Galantamine in frontotemporal dementia and primary progressive aphasia. Dement Geriatr Cogn Disord. 2008;25:178–85. doi: 10.1159/000113034. [DOI] [PubMed] [Google Scholar]
- 45.Williams SM, Goldman-Rakic PS. Widespread origin of the primate mesofrontal dopamine system. Cereb Cortex. 1998;8:321–45. doi: 10.1093/cercor/8.4.321. [DOI] [PubMed] [Google Scholar]
- 46.Tan HY, Chen Q, Goldberg TE, et al. Catechol-O-methyltransferase Val158Met modulation of prefrontal-parietal-striatal brain systems during arithmetic and temporal transformations in working memory. J Neurosci. 2007;27:13393–401. doi: 10.1523/JNEUROSCI.4041-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. [Last accessed September 24 2008]; Available from: www.clinicaltrials.gov/ct2/show/NCT00127114?term=frontotemporal+dementia&rank=10.
- 48.Gogos JA, Morgan M, Luine V, et al. Catechol-O-methyltransferase-deficient mice exhibit sexually dimorphic changes in catecholamine levels and behavior. Proc Natl Acad Sci USA. 1998;95:9991–6. doi: 10.1073/pnas.95.17.9991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huotari M, Gogos JA, Karayiorgou M, et al. Brain catecholamine metabolism in catechol-O-methyltransferase (COMT)-deficient mice. Eur J Neurosci. 2002;15:246–56. doi: 10.1046/j.0953-816x.2001.01856.x. [DOI] [PubMed] [Google Scholar]
- 50.Apud JA, Mattay V, Chen J, et al. Tolcapone improves cognition and cortical information processing in normal human subjects. Neuropsychopharmacology. 2006;32:1011–20. doi: 10.1038/sj.npp.1301227. [DOI] [PubMed] [Google Scholar]
- 51. [Last accessed September 24 2008]; Available from: www.clinicaltrials.gov/ct2/show/NCT00604591?term=frontotemporal+dementia&rank=9.
- 52.Coppola G, Karydas A, Rademakers R, et al. Gene expression study on peripheral blood identifies progranulin mutations. Ann Neurol. 2008;64(1):92–6. doi: 10.1002/ana.21397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Foulds P, McAuley E, Gibbons L, et al. TDP-43 protein in plasma may index TDP-43 brain pathology in Alzheimer’s disease and frontotemporal lobar degeneration. Acta Neuropathol. 2008;116(2):141–6. doi: 10.1007/s00401-008-0389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hardy J, Momeni P, Traynor BJ. Frontal temporal dementia: dissecting the aetiology and pathogenesis. Brain. 2006;129:830–1. doi: 10.1093/brain/awl035. [DOI] [PubMed] [Google Scholar]
- 55.Huey ED, Grafman J, Wassermann EM, et al. Characteristics of frontotemporal dementia patients with a progranulin mutation. Ann Neurol. 2006;60:374–80. doi: 10.1002/ana.20969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Skibinski G, Parkinson NJ, Brown JM, et al. Mutations in the endosomal ESCRTIII-complex subunit CHMP2B in frontotemporal dementia. Nat Genet. 2005;37:806–8. doi: 10.1038/ng1609. [DOI] [PubMed] [Google Scholar]
- 57.Watts GD, Wymer J, Kovach MJ, et al. Inclusion body myopathy associated with Paget disease of bone and frontotemporal dementia is caused by mutant valosin-containing protein. Nat Genet. 2004;36:377–81. doi: 10.1038/ng1332. [DOI] [PubMed] [Google Scholar]
- 58.Vance C, Al-Chalabi A, Ruddy D, et al. Familial amyotrophic lateral sclerosis with frontotemporal dementia is linked to a locus on chromosome 9p13.2–21.3. Brain. 2006;129:868–76. doi: 10.1093/brain/awl030. [DOI] [PubMed] [Google Scholar]
- 59.Morita M, Al-Chalabi A, Andersen PM, et al. A locus on chromosome 9p confers susceptibility to ALS and frontotemporal dementia. Neurology. 2006;66:839–44. doi: 10.1212/01.wnl.0000200048.53766.b4. [DOI] [PubMed] [Google Scholar]
- 60.Momeni P, Schymick J, Jain S, et al. Analysis of IFT74 as a candidate gene for chromosome 9p-linked ALS-FTD. BMC Neurol. 2006;6:44. doi: 10.1186/1471-2377-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Blair IP, Bennett CL, Abel A, et al. A gene for autosomal dominant juvenile amyotrophic lateral sclerosis (ALS4) localizes to a 500-kb interval on chromosome 9q34. Neurogenetics. 2000;3(1):1–6. doi: 10.1007/pl00022976. [DOI] [PubMed] [Google Scholar]
- 62.Hosler BA, Siddique T, Sapp PC, et al. Linkage of familial amyotrophic lateral sclerosis with frontotemporal dementia to chromosome 9q21-q22. JAMA. 2000;284(13):1664–9. doi: 10.1001/jama.284.13.1664. [DOI] [PubMed] [Google Scholar]
- 63.Ostojic J, Axelman K, Lannfelt L, Froelich-Fabre S. No evidence of linkage to chromosome 9q21-22 in a Swedish family with frontotemporal dementia and amyotrophic lateral sclerosis. Neurosci Lett. 2003;340(3):245–7. doi: 10.1016/s0304-3940(03)00126-5. [DOI] [PubMed] [Google Scholar]
- 64.Poorkaj P, Grossman M, Steinbart E, et al. Frequency of tau gene mutations in familial and sporadic cases of non-Alzheimer dementia. Arch Neurol. 2001;58:383–7. doi: 10.1001/archneur.58.3.383. [DOI] [PubMed] [Google Scholar]
- 65.Rosso SM, Kamphorst W, de Graaf B, et al. Familial frontotemporal dementia with ubiquitin-positive inclusions is linked to chromosome 17q21-22. Brain. 2001;124:1948–57. doi: 10.1093/brain/124.10.1948. [DOI] [PubMed] [Google Scholar]
- 66••.Baker M, Mackenzie IR, Pickering-Brown SM, et al. Mutations in progranulin cause tau-negative frontotemporal dementia linked to chromosome 17. Nature. 2006;442:916–9. doi: 10.1038/nature05016. This paper first disclosed that progranulin mutations could cause FTD. [DOI] [PubMed] [Google Scholar]
- 67.Andreadis A, Brown WM, Kosik KS. Structure and novel exons of the human tau gene. Biochemistry. 1992;31:10626–33. doi: 10.1021/bi00158a027. [DOI] [PubMed] [Google Scholar]
- 68.Available from: http://www.molgen.ua.ac.be/ADMutations/default.cfm?MT=1&ML=1&Page=MutByQuery&Query=tblContexts.GeneSymbol%20In%20('MAPT')&Selection=Gene%20In%20(MAPT)&CFID=136313&CFTOKEN=48500543
- 69.Brandt R, Hundelt M, Shahani N. Tau alteration and neuronal degeneration in tauopathies: mechanisms and models. Biochim Biophys Acta. 2005;1739:331–54. doi: 10.1016/j.bbadis.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 70.Delacourte A, Robitaille Y, Sergeant N, et al. Specific pathological Tau protein variants characterize Pick’s disease. J Neuropathol Exp Neurol. 1996;55:159–68. doi: 10.1097/00005072-199602000-00004. [DOI] [PubMed] [Google Scholar]
- 71.Buee Scherrer V, Hof PR, Buee L, et al. Hyperphosphorylated tau proteins differentiate corticobasal degeneration and Pick’s disease. Acta Neuropathol. 1996;91:351–9. doi: 10.1007/s004010050436. [DOI] [PubMed] [Google Scholar]
- 72.Wada H, Nakajoh K, Satoh-Nakagawa T, et al. Risk factors of aspiration pneumonia in Alzheimer’s disease patients. Gerontology. 2001;47:271–6. doi: 10.1159/000052811. [DOI] [PubMed] [Google Scholar]
- 73.Togo T, Sahara N, Yen SH, et al. Argyrophilic grain disease is a sporadic 4-repeat tauopathy. J Neuropathol Exp Neurol. 2002;61:547–56. doi: 10.1093/jnen/61.6.547. [DOI] [PubMed] [Google Scholar]
- 74.Malkani R, D’Souza I, Gwinn-Hardy K, et al. MAPT mutation in a regulatory element upstream of exon 10 causes frontotemporal dementia. Neurobiol Dis. 2006;22:401–3. doi: 10.1016/j.nbd.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 75.Hutton M, Lendon CL, Rizzu P, et al. Association of missense and 5′-splice-site mutations in tau with the inherited dementia FTDP-17. Nature. 1998;393:702–5. doi: 10.1038/31508. [DOI] [PubMed] [Google Scholar]
- 76.Spillantini MG, Murrell JR, Goedert M, et al. Mutation in the tau gene in familial multiple system tauopathy with presenile dementia. Proc Natl Acad Sci USA. 1998;95:7737–41. doi: 10.1073/pnas.95.13.7737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Momeni P, Pittman A, Lashley T, et al. Clinical and pathological features of an Alzheimer’s disease patient with the MAPT ΔK280 mutation. Neurobiol Aging. 2007 August 27; doi: 10.1016/j.neurobiolaging.2007.07.013. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dawson HN, Cantillana V, Chen L, Vitek MP. The tau N279K exon 10 splicing mutation recapitulates frontotemporal dementia and parkinsonism linked to chromosome 17 tauopathy in a mouse model. J Neurosci. 2007;27(34):9155–68. doi: 10.1523/JNEUROSCI.5492-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hutton M. “Missing” tau mutation identified. Ann Neurol. 2000;47:417–8. [PubMed] [Google Scholar]
- 80.Buguiani O, Murrell JR, Giaccone G, et al. Frontotemporal dementia and corticobasal degeneration in a family with a P301S mutation in tau. J Neuropathol Exp Neurol. 1999;58:667–77. doi: 10.1097/00005072-199906000-00011. [DOI] [PubMed] [Google Scholar]
- 81.Hasegawa M, Smith MJ, Goedert M. Tau proteins with FTDP-17 mutations have a reduced ability to promote microtubule assembly. FEBS Lett. 1998;437:207–10. doi: 10.1016/s0014-5793(98)01217-4. [DOI] [PubMed] [Google Scholar]
- 82.Goedert M, Jakes R, Crowther RA. Effects of frontotemporal dementia FTDP-17 mutations on heparin- induced assembly of tau filaments. FEBS Lett. 1999;450:306–11. doi: 10.1016/s0014-5793(99)00508-6. [DOI] [PubMed] [Google Scholar]
- 83•.Rademakers R, Baker M, Gass J, et al. Phenotypic variability associated with progranulin haploinsufficiency in patients with the common 1477C→T (Arg493X) mutation: an international initiative. Lancet Neurol. 2007;6(10):857–68. doi: 10.1016/S1474-4422(07)70221-1. An interesting paper on the genetics and phenotype associated with the most common progranulin mutation. [DOI] [PubMed] [Google Scholar]
- 84.Eriksen JL, Mackenzie IR. Progranulin: normal function and role in neurodegeneration. J Neurochem. 2008;104:287–97. doi: 10.1111/j.1471-4159.2007.04968.x. [DOI] [PubMed] [Google Scholar]
- 85.Daniel R, He Z, Carmichael KP, et al. Cellular localization of gene expression for progranulin. J Histochem Cytochem. 2000;48:999–1009. doi: 10.1177/002215540004800713. [DOI] [PubMed] [Google Scholar]
- 86.Bateman A, Belcourt D, Bennett H, et al. Granulins, a novel class of peptide from leukocytes. Biochem Biophys Res Commun. 1990;173:1161–8. doi: 10.1016/s0006-291x(05)80908-8. [DOI] [PubMed] [Google Scholar]
- 87.He Z, Bateman A. Progranulin (granulin-epithelin precursor, PC-cell-derived growth factor, acrogranin) mediates tissue repair and tumorigenesis. J Mol Med. 2003;81:600–12. doi: 10.1007/s00109-003-0474-3. [DOI] [PubMed] [Google Scholar]
- 88.Zhu J, Nathan C, Jin W, et al. Conversion of proepithelin to epithelins: roles of SLPI and elastase in host defense and wound repair. Cell. 2002;111:867–78. doi: 10.1016/s0092-8674(02)01141-8. [DOI] [PubMed] [Google Scholar]
- 89•.Le Ber I, Camuzat A, Hannequin D, et al. Phenotype variability in progranulin mutation carriers: a clinical, neuropsychological, imaging, and genetic study. Brain. 2008;131:732–46. doi: 10.1093/brain/awn012. All three of these papers in this issue of Brain (see references [91] and [92] below) elucidate the phenotype associated with progranulin mutations. [DOI] [PubMed] [Google Scholar]
- 90•.Pickering-Brown SM, Rollinson S, Du Plessis D, et al. Frequency and clinical characteristics of progranulin mutation carriers in the Manchester frontotemporal lobar degeneration cohort: comparison with patients with MAPT and no known mutations. Brain. 2008;131:721–31. doi: 10.1093/brain/awm331. All three of these papers in this issue of Brain (see references [90] and [92] elucidate the phenotype associated with progranulin mutations. [DOI] [PubMed] [Google Scholar]
- 91•.Beck J, Rohrer JD, Campbell T, et al. A distinct clinical, neuropsychological, and radiological phenotype is associated with progranulin gene mutations in a large UK series. Brain. 2008;131:706–20. doi: 10.1093/brain/awm320. All three of these papers in this issue of Brain (see references [90] and [91]) elucidate the phenotype associated with progranulin mutations. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Anderton BH, Betts J, Blackstock WP, et al. Sites of phosphorylation in tau and factors affecting their regulation. Biochem Soc Symp. 2001:73–80. doi: 10.1042/bss0670073. [DOI] [PubMed] [Google Scholar]
- 93.The Therapeutics Working Group. Summary and Suggestions for Future Resource Development and Research Initiatives Frontotemporal Dementia Workshop. 2007 Available from: www.ninds.nih.gov/news_and_events/proceedings/Frontotemporal_Dementia_Workshop.htm.
- 94.Gotschel F, Kern C, Lang S, et al. Inhibition of GSK3 differentially modulates NF-κB, CREB, AP-1 and β-catenin signaling in hepatocytes, but fails to promote TNF-α-induced apoptosis. Exp Cell Res. 2008;314:1351–66. doi: 10.1016/j.yexcr.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 95.Gomez-Ramos A, Dominguez J, Zafra D, et al. Inhibition of GSK3 dependent tau phosphorylation by metals. Curr Alzheimer Res. 2006;3:123–7. doi: 10.2174/156720506776383059. [DOI] [PubMed] [Google Scholar]
- 96.Kim AJ, Shi Y, Austin RC, Werstuck GH. Valproate protects cells from ER stress-induced lipid accumulation and apoptosis by inhibiting glycogen synthase kinase-3. J Cell Sci. 2005;118:89–99. doi: 10.1242/jcs.01562. [DOI] [PubMed] [Google Scholar]
- 97.Engel T, Goni-Oliver P, Gomez de Barreda E, et al. Lithium, a potential protective drug in Alzheimer’s disease. Neurodegener Dis. 2008;5:247–9. doi: 10.1159/000113715. [DOI] [PubMed] [Google Scholar]
- 98.Engel T, Goni-Oliver P, Lucas JJ, et al. Chronic lithium administration to FTDP-17 tau and GSK-3β overexpressing mice prevents tau hyperphosphorylation and neurofibrillary tangle formation, but pre-formed neurofibrillary tangles do not revert. J Neurochem. 2006;99:1445–55. doi: 10.1111/j.1471-4159.2006.04139.x. [DOI] [PubMed] [Google Scholar]
- 99.Le Corre S, Klafki HW, Plesnila N, et al. An inhibitor of tau hyperphosphorylation prevents severe motor impairments in tau transgenic mice. Proc Natl Acad Sci USA. 2006;103:9673–8. doi: 10.1073/pnas.0602913103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Fornai F, Longone P, Cafaro L, et al. Lithium delays progression of amyotrophic lateral sclerosis. Proc Natl Acad Sci USA. 2008;105:2052–7. doi: 10.1073/pnas.0708022105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Phiel CJ, Klein PS. Molecular targets of lithium action. Annu Rev Pharmacol Toxicol. 2001;41:789–813. doi: 10.1146/annurev.pharmtox.41.1.789. [DOI] [PubMed] [Google Scholar]
- 102.Berridge MJ, Downes CP, Hanley MR. Neural and developmental actions of lithium: a unifying hypothesis. Cell. 1989;59:411–9. doi: 10.1016/0092-8674(89)90026-3. [DOI] [PubMed] [Google Scholar]
- 103.Ward ME, Musa MN, Bailey L. Clinical pharmacokinetics of lithium. J Clin Pharmacol. 1994;34:280–5. doi: 10.1002/j.1552-4604.1994.tb01994.x. [DOI] [PubMed] [Google Scholar]
- 104.Haddjeri N, Szabo ST, de Montigny C, Blier P. Increased tonic activation of rat forebrain 5-HT(1A) receptors by lithium addition to antidepressant treatments. Neuropsychopharmacology. 2000;22:346–56. doi: 10.1016/S0893-133X(99)00138-4. [DOI] [PubMed] [Google Scholar]
- 105.Massot O, Rousselle JC, Fillion MP, et al. 5-HT1B receptors: a novel target for lithium. Possible involvement in mood disorders. Neuropsychopharmacology. 1999;21:530–41. doi: 10.1016/S0893-133X(99)00042-1. [DOI] [PubMed] [Google Scholar]
- 106.Macdonald A, Briggs K, Poppe M, et al. A feasibility and tolerability study of lithium in Alzheimer’s disease. Int J Geriatr Psychiatry. 2008;23:704–11. doi: 10.1002/gps.1964. [DOI] [PubMed] [Google Scholar]
- 107.Mur M, Portella MJ, Martinez-Aran A, et al. Persistent neuropsychological deficit in euthymic bipolar patients: executive function as a core deficit. J Clin Psychiatry. 2007;68:1078–86. doi: 10.4088/jcp.v68n0715. [DOI] [PubMed] [Google Scholar]
- 108.Senturk V, Goker C, Bilgic A, et al. Impaired verbal memory and otherwise spared cognition in remitted bipolar patients on monotherapy with lithium or valproate. Bipolar Disord. 2007;9(Suppl 1):136–44. doi: 10.1111/j.1399-5618.2007.00481.x. [DOI] [PubMed] [Google Scholar]
- 109.Rowinsky EK, Donehower RC. Paclitaxel (Taxol) N Engl J Med. 1995;332:1004. doi: 10.1056/NEJM199504133321507. [DOI] [PubMed] [Google Scholar]
- 110.Ahmed Z, Mackenzie IR, Hutton ML, Dickson DW. Progranulin in frontotemporal lobar degeneration and neuroinflammation. J Neuroinflammation. 2007;4(7):1–13. doi: 10.1186/1742-2094-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yoshiyama Y, Higuchi M, Zhang B, et al. Synapse loss and microglial activation precede tangles in a P301S tauopathy mouse model. Neuron. 2007;53:337–51. doi: 10.1016/j.neuron.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 112.The Genetics Working Group. Summary and Suggestions for Future Resource Development and Research Initiatives Frontotemporal Dementia Workshop. [Last accessed September 24 2008];2007 Available from: www.ninds.nih.gov/news_and_events/proceedings/Frontotemporal_Dementia_Workshop.htm.
- 113.Rankin KP, Santos-Modesitt W, Kramer JH, et al. Spontaneous social behaviors discriminate behavioral dementias from psychiatric disorders and other dementias. J Clin Psychiatry. 2008;69:60–73. doi: 10.4088/jcp.v69n0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Diagnostic and statistical manual of mental disorders DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 115•.Boxer AL, Boeve BF. Frontotemporal dementia treatment: current symptomatic therapies and implications of recent genetic, biochemical, and neuroimaging studies. Alzheimer Dis Assoc Disord. 2007;21:S79–87. doi: 10.1097/WAD.0b013e31815c345e. An interesting assessment of the use of recent technologies (including imaging) in the investigation of treatments for FTD. [DOI] [PubMed] [Google Scholar]


