Abstract
Background
Individuals with comorbid substance use and posttraumatic stress disorder may differentially benefit from integrated trauma-focused interventions based on specific presenting characteristics such as substance use type and PTSD severity. The current study is a secondary analysis of a NIDA Clinical Trials Network study exploring the effectiveness of two interventions for women with comorbid PTSD and substance use disorders.
Method
Generalized estimating equations were used to examine the effect of baseline alcohol misuse on PTSD outcome measures over time for all randomized participants.
Results
Women entering treatment with baseline alcohol misuse had higher Post Traumatic Stress Disorder Symptom Scale (PSS-SR) total scores (t = 2.43, p < .05), cluster C (avoidance/numbing) scores (t = 2.63, p < .01), and cluster D (hyper-arousal) scores (t = 2.31, p < .05). For women with alcohol misuse, after treatment week one, PSS-SR scores were significantly lower in the Seeking Safety intervention during treatment (χ2(1) = 4.00, p < .05) and follow-up (χ2(1) = 4.87, p < .05) compared to those in the health education intervention. Alcohol misusers in the Seeking Safety group who had higher baseline hyper-arousal severity improved more quickly than those with lower baseline hyper-arousal severity during treatment (χ2(1) = 4.06, p < .05).
Conclusions
These findings suggest that the type of substance abuse at treatment entry may inform treatment selection, predict treatment response among those with co-occurring PTSD and substance use disorders, and indicate a more severe clinical picture.
Keywords: Posttraumatic Stress, Substance Abuse, Alcohol Misuse, Co-morbidity, Cognitive-behavioral Therapy
1. Introduction
Despite the growing number of behavioral and psychopharmacologic treatment outcome studies targeting substance abuse and posttraumatic stress disorder (PTSD) symptoms, there remains little consensus for best practices. Researchers and providers who study and treat individuals with trauma histories and addiction must contend with several sets of frequently alternating symptoms. Thus far, treatment outcome studies have demonstrated reductions in PTSD symptoms alone (Hien et al., 2009), reductions in both substance abuse and PTSD symptoms (Hien et al., 2004; Triffleman et al., 1999), and a sequential process whereby initial reductions in PTSD symptoms lead to reductions in substance abuse severity (Back et al., 2006). Overall, however, findings have been disappointing with respect to identifying treatments which consistently, and in a clinically meaningful way, reduce symptoms along either or both symptom domains.
We have argued in greater detail elsewhere (Hien et al., 2009) that a number of limitations in conducting comorbidity research diminish the likelihood that the standard intent-to-treat analysis methodology will produce clinically significant findings. These limitations include mismatch between severity of psychopathology and types and lengths of treatment (i.e., short-term treatments for long-term problems). For example, in the largest multisite behavioral trial of group therapy for PTSD among women substance users in the community, the National Institute on Drug Abuse (NIDA) Clinical Trials Network “Women and Trauma Study,” overall findings did not provide support for the superiority of the trauma-focused therapy over an active health education curriculum. These findings have been taken by some to suggest that Seeking Safety, the trauma-focused treatment tested in the trial, is not effective for those with PTSD and substance use disorders; potentially significant public health and policy decisions may be made on the basis of these overall findings. However, in the case of the “Women and Trauma Study,” nearly half of the sample was abstinent from substance use at study enrollment since inclusion criteria only required substance use in the past six months. Thus, it remained to be seen whether the treatments would have fared differently if all participants were actively using substances at the time of enrollment.
To address this question, we conducted a secondary data analysis (Hien et al., 2010) utilizing a subsample of participants from the original clinical trial who had active substance use at baseline (n = 274 of the original 353 participants). The substance use measure used in this analysis captured the prior 30 days, which differed from the 7-day measure (with biological confirmation) used in the primary intent to treat analysis. Clinically significant treatment response thresholds were defined a priori and based on prior research (Brady et al., 2000; Nunes et al., 1998). Treatment changes were modeled to examine PTSD and substance use changes over the six treatment weeks and, secondarily, the impact of treatment response (i.e., clinically significant PTSD or substance use symptom change during the treatment phase) during follow-up. Findings from this analysis did reveal significant benefits on substance use outcomes over the 12-month follow-up period for participants in trauma-focused treatment who had more severe substance use at the start of treatment and who experienced reductions in their PTSD symptoms as a result of treatment. This analysis highlights the importance of assessing pre-treatment symptom characteristics and in-treatment symptom change processes, both of which may influence treatment outcomes.
Another reason that comorbid PTSD and substance use disorder research may not have yielded more definitive outcomes involves the tendency to collapse substance use categories. In addition to the fact that most individuals in community substance abuse treatment (and in this trial) are poly-substance users, their selection of substances may vary and be driven, in part, by the specific symptom clusters of PTSD (e.g., Back et al., 2003; Saladin et al., 1995; Stewart et al., 1999; Taft, et al., 2007). PTSD symptoms are often quite disparate. For example, patients may experience symptoms related to intrusive thoughts and memories of the trauma, while others are avoidant or emotionally numb.
The few studies to date that have examined relationships between substance use and PTSD characteristics have primarily focused on comparisons of alcohol use with illicit substances. In all of these comparisons, the alcohol-dependent group reports a higher number of hyper-arousal and avoidance symptoms (Back et al., 2003, Saladin et al., 1995, Stewart et al., 1999) than those with other drug dependencies, and in one outcome study (Brady et al., 2005) revealed differential outcomes when type of alcohol dependence was taken into consideration. These kinds of findings suggest a functional relationship between PTSD symptom severity and the avoidance and hyper-arousal symptom clusters, especially among alcohol abusers.
Yet, it has been difficult to examine subgroups of substance users in relation to changes in the symptom clusters of PTSD due to small treatment research samples and the need for homogenous inclusion criteria in efficacy trials. The current analysis offers a unique opportunity to contribute to the PTSD/addiction treatment field by exploring PTSD symptoms and the relationship to baseline alcohol misuse. Most specifically, we were interested in identifying whether individuals with alcohol misuse in the “Women and Trauma Study” had differential treatment responses to the trauma-focused versus women’s health education groups on PTSD symptoms in comparison to those with no misuse. Further, we hypothesized that those with alcohol misuse would have more hyper-arousal symptoms at baseline, and that these symptoms would be most likely to change over the follow-up period for those in trauma-specific therapy in contrast to those in the health education groups.
2. Methods
2.1 Participants
Data for this analysis was derived from a study conducted within the NIDA Clinical Trials Network (for additional study details see Hien et al., 2009). Seven community-based intensive outpatient substance abuse treatment programs located throughout the United States recruited and randomized 353 female participants. Eligible participants had at least one lifetime traumatic event and met DSM-IV criteria for either full or sub-threshold PTSD in the past 30 days. Sub-threshold PTSD differs from full PTSD in that participants could meet either criterion C (avoidance of trauma reminders and emotional numbing) or criterion D (hyper-arousal), but not both as in the full diagnostic requirement. Participants also had to be between the ages of 18-65, have used alcohol or an illicit substance within the prior 6-months, and meet current drug or alcohol abuse/dependence criteria. Women were excluded if they had impaired mental cognition (evaluated using the Mini-Mental Status Exam [Folstein et al., 1975]), significant risk of suicidal/homicidal behavior, history of schizophrenia-spectrum diagnosis, or active psychosis.
2.2 Procedures
Participants completed an initial screening interview to assess eligibility, followed by a baseline assessment and randomization. Randomization assignment was stratified by prescription psychotropic medication use and having an alcohol use disorder only (as opposed to both alcohol and drug use disorders or drug use disorder only) at baseline. Women were randomized into one of two 12-session group interventions. Treatment consisted of two 90-minute sessions per week for 6 weeks. Participants completed brief, weekly assessments during treatment to collect substance use and PTSD symptom data and were reassessed at 1-week, 3-, 6-, and 12-months post treatment. Baseline and post treatment interviews were conducted by independent assessors who remained blind to randomization assignment.
2.3 Interventions
2.3.1 Seeking Safety Treatment
(Najavits, 2002) is a short-term manualized therapy using cognitive-behavioral strategies to reduce substance use and the negative impact of trauma exposure. Each session is similarly structured, beginning with a check-in on safety and coping, the introduction of a quotation used as a point of inspiration, a presentation of the session topic and materials, and a checkout used to reinforce progress and provide feedback. Seeking Safety includes basic education on substance use disorders and PTSD; action skills to prevent drug use and control PTSD symptoms; and cognitive restructuring with particular attention to maladaptive thoughts associated with substance use and trauma symptoms, relationship issues, and the development of effective communication skills to build a healthy support network.
2.3.2. Women’s Health Education
(Miller et al., 1998) is a psychoeducational intervention that focuses on general health topics pertinent to women (e.g., female anatomy, human sexual behavior, pregnancy and childbirth, nutrition, and diabetes). The Women’s Health Education provides equivalent facilitator attention, expectancy of benefit, and issue oriented focus, but does not provide theory driven techniques, such as cognitive behavioral therapy, or psychoeducation specific to substance abuse and PTSD. All sessions have the same structure and include an introduction of the topic, review of between session assignments, topic presentation using multiple formats, participant exercises to facilitate group discussion and goal-setting.
2.4 Measures
2.4.1 Sociodemographics
Basic demographic data, including age and race/ethnicity were collected at the screening assessment. Education was collected at baseline using the Addiction Severity Index (ASI-Lite, revised from the 1992 ASI Fifth Edition; McLellan et al., 1997).
2.4.2 Post Traumatic Stress Disorder
PTSD at baseline was assessed via the 17-item Post Traumatic Stress Disorder Symptom Scale-Self Report (PSS-SR), an inventory that assesses the frequency and intensity of PTSD symptoms (Foa et al., 1993). The PSS-SR was administered weekly during treatment and at all follow-up time points. The PSS-SR can be converted into PTSD diagnostic clusters; reexperiencing (B), avoidance and numbing (C), and hyper-arousal (D).
2.4.3 Substance Use
Alcohol and substance use data were collected for the prior 30 days at baseline using the ASI-Lite (McLellan et al., 1997). Participants self-reported the number of days of alcohol use and illicit substance use. Illicit substance use was calculated based on the highest number of days reported for any of the following substances: cocaine, heroin, marijuana, sedatives, and stimulants.
2.4.4 Alcohol Misuse
Alcohol misuse was defined as either (1) daily alcohol use in the prior 30 days or (2) at least one day of alcohol use to intoxication in the prior 30 days. This data was derived from the ASI-Lite. Given that standard number of alcohol drinks per day was not collected in this trial and that all participants met criteria for substance abuse or dependence, daily use or use to intoxication was selected as a proxy for misuse of alcohol.
2.5 Statistical Methods
Demographic information and symptom severity by alcohol misuse status at baseline were compared using a t-test for continuous variables and chi-square test for categorical variables.
The data analytic strategy was applied similarly for each of four models. The main outcome variables were PSS-SR severity and PTSD symptom clusters generated from the PSS-SR. The generalized estimating equations (GEEs) (Diggle et al., 1994) were used to examine the effect of alcohol misuse at baseline on the outcome measures over time for the intention-to-treat (ITT) sample of all randomized participants. Each outcome was modeled as a function of alcohol misuse, treatment, time of assessment, and baseline value of that outcome (prior to randomization). All models included pre-selected baseline covariates: race/ethnicity, age, and education level.1 The possible interactions among baseline alcohol misuse, treatment, the baseline level of the outcome measure, and time were tested and included in the final model only if statistically significant (p < .05). The GEE methodology is able to handle correlated data arising from repeated measurements, requires no parametric distribution assumption, and provides robust inference with respect to misspecification of the within-subject correlation. All inferences above from incomplete or missing data are presumed valid provided that the data are missing at random (Little & Rubin, 2002). Since the two treatment groups did not differ by treatment attendance, study retention, or follow-up completion, the inference for the treatment effect was valid.
Site was tested as an additional fixed effect in each model. The models also included an indicator of the study phase (i.e., intervention vs. follow-up) and possible interactions with treatment and time of assessment. PROC GENMOD in SAS 9.1.3 (SAS, 2003) was used to conduct all analyses.
3. Results
3.1 Baseline Differences between Participants with and without Alcohol Misuse
Table 1 presents differences in demographics, substance use severity, and PTSD symptoms for participants categorized as alcohol misusers or non-misusers at baseline. Women who misused alcohol at baseline were more likely to be older (t = 3.71, p < .001), slightly more educated (t = 2.01, p < .05), and have more days of substance use (t = 5.76, p < .001). Alcohol misusers also had higher PSS-SR total scores (t = 2.43, p < .05), cluster C (avoidance/numbing) scores (t = 2.63, p < .01), and cluster D (hyper-arousal) scores (t = 2.31, p < .05). There were no significant differences between the two groups by race/ethnicity or PSS-SR cluster B scores.
Table 1.
Demographic, Substance Use, and PTSD Characteristics at Baseline by Alcohol Misuse Categorization (N=353)
| Alcohol Misuse N=111 | No Alcohol Misuse N=242 | |||
|---|---|---|---|---|
| Mean (SD) or % | χ2 / t-test | p-value | ||
| Treatment (%) | 3.92 | 0.048 | ||
| Seeking Safety | 57.66 | 46.28 | ||
| Women’s Health | 42.34 | 53.72 | ||
| Age (years) | 41.87 (8.57) | 37.98 (9.37) | 3.71 | <.001 |
| Race/Ethnicity (%) | 0.28 | 0.963 | ||
| African American/Black | 33.33 | 34.30 | ||
| Caucasian | 45.05 | 45.87 | ||
| Latina/Hispanic | 6.31 | 6.61 | ||
| Multi-racial / Other | 15.32 | 13.22 | ||
| Education (years) | 12.92 (2.52) | 12.36 (2.39) | 2.01 | 0.046 |
| Days of Substance Use (past 30 days) | 11.78(10.94) | 5.19(9.52) | 5.76 | <.001 |
| PSS-SR Severity (total) | 48.41 (14.78) | 44.19 (15.34) | 2.43 | 0.016 |
| PSS-SR: Cluster B | 10.98 (4.24) | 10.44 (4.37) | 1.09 | 0.274 |
| PSS-SR: Cluster C | 19.35 (7.13) | 17.24 (6.93) | 2.63 | 0.009 |
| PSS-SR: Cluster D | 18.07 (5.75) | 16.50 (6.01) | 2.31 | 0.022 |
3.2 PTSD Symptoms and Symptom Cluster Outcomes
The GEE model of PTSD symptoms over time revealed a significant two-way interaction effect (χ2(1) = 4.29, p <.01) between alcohol misuse at baseline and treatment group, which indicated that the treatment effects during the first week of treatment were different for participants who were alcohol misusers versus those without alcohol misuse (See Table 2). Among participants without alcohol misuse at baseline, PSS-SR scores significantly improved for those in the Women’s Health Education group compared to those in Seeking Safety during the first week of treatment (χ2(1) = 7.77, p < .01), but then decreased more quickly for Seeking Safety over the remainder of treatment. There were no significant differences between the treatment groups at the end of treatment or at follow-up (12 months post-treatment). Among participants with alcohol misuse at baseline, there were no significant differences in PSS-SR scores during the first week of treatment between the two treatment groups (χ2(1) = 0.01, p = .92). However, the PSS-SR scores were significantly lower for those in Seeking Safety during the remainder of treatment (χ2(1) = 4.00, p < .05) and during follow-up (χ2(1) = 4.87, p < .05) compared to those in the health education group (See Figure 1).
Table 2.
The effects of Alcohol Misuse by Treatment on Total Posttraumatic Stress Symptoms from Baseline through Treatment and Follow-up (N=353)
| Covariates | Chi-square | p-value |
|---|---|---|
| Age | 1.44 | .231 |
| Race/ethnicity | 0.58 | .902 |
| Education | 4.61 | .032 |
| Treatment (SS v WHE) | 7.77 | .005 |
| Treatment Week | 6.64 | .010 |
| Alcohol Misuse (BL) | 3.35 | .067 |
| Follow-up | 3.95 | .047 |
| PSS-SR (BL) | 65.32 | .001 |
| PSS-SR (BL) × Week | 10.03 | .002 |
| Alcohol Misuse (BL) × Treatment | 4.29 | .039 |
| Treatment Week × Follow-up | 7.98 | .005 |
| Treatment Week × Treatment | 4.00 | .046 |
| Follow-up × Treatment | 4.87 | .027 |
| Treatment × Treatment Week × Follow-Up | 4.34 | .037 |
Figure 1.
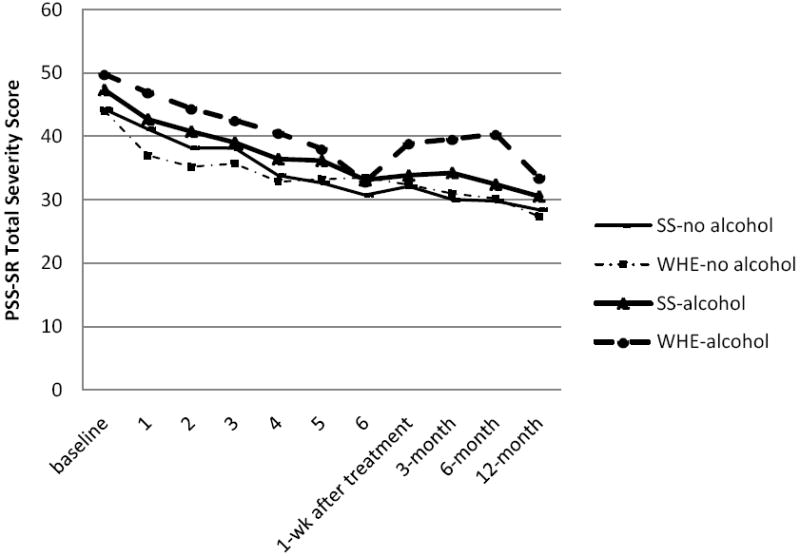
PSS-SR Total Severity by Baseline Alcohol Misuse and Treatment Type (Seeking Safety vs. Women’s Health Education).
There was also a significant three-way interaction between treatment group, time, and follow-up study phase (χ2(1) = 4.34, p < .037). For both alcohol misusers and non-misusers, PSS-SR total scores improved significantly during the 6-week treatment phase (χ2(1) = 6.64, p = .01), but not during the follow-up phase (χ2 (1) = 1.74, p = .19). The PSS-SR improvement during treatment was stronger for those in Seeking Safety compared to Women’s Health Education (χ2(1) = 4.00, p < .05).
The interaction between baseline PSS-SR severity and time was also significant (χ2(1) = 10.03, p < .01) such that participants with higher baseline PSS-SR severity scores improved more quickly than those with lower baseline PSS-SR severity scores during the treatment.
Further analyses were done to model the effect of alcohol misuse on PSS-SR symptom cluster scores. The treatment effects on each symptom cluster score were similar to the effects on the total PSS-SR scores. The improvement of hyper-arousal cluster (D) scores by week during treatment was significantly stronger in Seeking Safety than Women’s Health (χ2(1) = 4.57, p = .03), whereas this was not the case for either of the other two clusters (re-experiencing cluster [χ2(1) = 3.29, p = .07] and avoidance/numbing cluster [χ2(1) = 3.53, p = .06]). There were no differences between alcohol misusers and alcohol non-misusers by PTSD symptom sub-cluster during treatment. However, there was a trend for the hyper-arousal cluster scores. Specifically, there was a four-way interaction among baseline hyper-arousal cluster scores, treatment, time, and alcohol misuse (χ2(1) = 3.67, p < .06), which indicated that the treatment effects on hyper-arousal scores among alcohol misusers differed by the baseline level of the cluster score. Among alcohol misusers, participants in Seeking Safety group with higher baseline hyper-arousal severity improved more quickly than those with lower baseline hyper-arousal severity during treatment (χ2(1) = 4.06, p < .05). The effect of baseline hyper-arousal severity did not differ by treatment group among alcohol non-misusers (χ2(1) = 0.64, p < .62).
4. Discussion
In the present study, a secondary analysis of the relationship between alcohol misuse and PTSD symptoms among a sample of women in treatment for addiction and trauma-related disorders revealed significant treatment effects for the Seeking Safety trauma group therapy in comparison to the Women’s Health Education group therapy. In line with findings from the primary outcome analysis of the “Women and Trauma Study” (Hien et al., 2009), among those with no alcohol misuse at baseline, there were no differences in PTSD outcomes at the end of treatment or during the follow-up period between the two behavioral group therapy interventions; all participants appeared to benefit from the study interventions in reducing PTSD symptoms. In contrast, among those with alcohol misuse, there was a significant and differential benefit of Seeking Safety over Women’s Health Education, such that those in the trauma-focused therapy groups had significantly greater reductions in their PTSD symptoms. Further, among those in the health education group, in direct contrast to the main outcome findings (Hien et al., 2009), women with alcohol misuse did not appear to significantly reduce their PTSD symptoms. Those in trauma-focused Seeking Safety therapy groups did benefit, with clinically significant reductions in PTSD symptoms. These findings suggest that identifying the type of substance use and abuse that patients present with at treatment entry may be an important factor in determining treatment selection and predicting treatment response among those with co-occurring PTSD and substance use disorders. Further, alcohol use may indicate a more severe clinical presentation among this population of women; whereby poly-substance use, more severe substance use, or a longer substance use history may require more integrated treatment approaches.
Alcohol misuse (defined as either daily use or one day of drinking to intoxication within the past 30 days at baseline assessment) was present in one third of the sample of substance abusers in this study. Women who misused alcohol at baseline reported significantly greater overall PTSD symptom severity, and specifically, had significantly more avoidance/numbing and hyper-arousal symptoms than those who did not misuse alcohol. These findings support prior research which suggest specific alcohol-to-PTSD symptom cluster functional relationships (e.g., Back et al., 2003; Saladin et al., 1995; Stewart et al., 1999; Taft, et al., 2007). Consistent with the self-medication model (Jacobsen et al., 2001; Khantzian, 1999), alcohol, which is a central nervous system depressant, may be used to ameliorate avoidance and hyper-arousal symptoms of PTSD which can be biologically-driven and quite refractory to treatment. Finding that alcohol misuse differentiates this heterogeneous treatment group of women in drug treatment has important clinical implications; it suggests that identifying co-occurring and potentially harmful alcohol use may be an important clinical indicator for different kinds of treatment. Treatments such as Seeking Safety which focus on teaching alternative coping strategies to address specific symptoms may be particularly helpful. Indeed, when comparing Seeking Safety to Women’s Health Education on efficacy of PTSD symptom cluster reduction, there was a trend for the trauma-focused treatment to be more effective in reducing hyper-arousal symptoms. Further, women with more severe symptoms benefited most from the trauma-focused therapy. Similar to previous findings (Back et al., 2006), improvements in hyper-arousal symptoms were related to improvements in alcohol use severity, further supporting a self-medication model.
The findings that women with more severe PTSD and both alcohol misuse and other substance use profited from the trauma-focused therapy differentially from those receiving health education groups is consistent with an additional secondary analysis from this trial (Hien et al., 2010) reported earlier. That is, Seeking Safety was found to be significantly more effective for those with heavier substance use at baseline and more severe substance use problems. Notably, in the current analysis, among the alcohol-misusing women, there was also greater illicit substance use. Thus, alcohol misuse may possibly be viewed as a proxy for greater severity of both PTSD and substance use symptoms.
The fact that Seeking Safety, an integrated, present-focused treatment, provided superior benefits to those with more active and severe PTSD symptoms may also be understood by examining the elements and structure of the treatment itself. The International Society for Traumatic Stress Studies Practice Guidelines (2009) identifies Seeking Safety as the only effective treatment model for co-occurring PTSD and substance use disorders. In the general field of trauma studies, there is a growing consensus for a stage model of trauma therapy. Phase I treatments emphasize safety, stabilization, and coping skills development, while phase II treatments (e.g., trauma-processing therapies) directly confront trauma-related thoughts, memories, and feelings (e.g., van der Kolk et al., 1999; Courtois and Ford, 2009). Seeking Safety is viewed as an early stage treatment model, which may be most appropriate for those who are actively using and have high symptom severity. Later stage trauma therapies such as Cognitive Processing Therapy and Prolonged Exposure Therapy may be more appropriate for those whose substance use disorder has stabilized and who are not actively using. Later phase therapy may also be necessary to help patients more fully resolve PTSD symptoms. Further research will be needed to explore questions related to identifying factors which aid patient matching for the most efficacious treatment planning.
4.1 Limitations and Future Research Directions
The sample for this study is primarily comprised of participants with poly-substance use and was not originally designed to examine women with alcohol use disorders specifically. As such, the alcohol misuse variable is based on general drinking trends rather than preferred methods such as number of drinks per drinking day or number of heavy drinking days. However, the clear differences between participants who were classified as alcohol misusers versus non-misusers lend support for the adequacy of this designation. Indeed, among those in the alcohol misuse group, 88% (n=98) met current (past 6-months) criteria for an alcohol use disorder.
Future research with women who have co-occurring PTSD and substance use disorders should identify subgroups of substance users and the functional relationships between type of substance use, severity of substance use, and the specific PTSD symptom clusters. Moreover, examination of the specific mechanisms of Seeking Safety that are responsible for overall PTSD symptom improvement, and specifically hyper-arousal symptoms, among women with alcohol misuse is essential to providing more targeted treatment. Finally, research on how treatment models can be enhanced to better address specific PTSD symptom clusters is needed.
4.2 Implications
Overall, these findings clearly add to a growing body of evidence for the necessity of comprehensive assessment at treatment entry to individually tailor substance abuse and co-occurring trauma-related disorder treatments; specific examination of alcohol misuse appears to be particularly important among those with PTSD, regardless of other substance use. Findings also demonstrate that despite many clinical fears, not only are trauma-focused cognitive-behavioral therapies (e.g., phase I) safe to apply with those suffering from PTSD and substance use disorders without escalating symptoms of either, but those with more severe and active substance use problems may even differentially benefit from a trauma-focused model over one which does not directly address these symptoms. This study suggests that an integrated trauma model, such as Seeking Safety, may be a sound, first line, clinical approach to managing PTSD among women with active alcohol misuse.
Footnotes
Further analyses examined an additional effect of the frequency of attending 12-step meetings, but it was not significantly different and was not included in the final models.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Back SE, Brady KT, Sonne SC, Verduin ML. Symptom improvement in co-occurring PTSD and alcohol dependence. J Ment Dis. 2006;194(9):690–696. doi: 10.1097/01.nmd.0000235794.12794.8a. [DOI] [PubMed] [Google Scholar]
- Back SE, Sonne SC, Killeen TK, Dansky BS, Brady KT. Comparative profiles of women with PTSD and comorbid cocaine or alcohol dependence. Am J Drug Alcohol Abuse. 2003;29(1):169–189. doi: 10.1081/ada-120018845. [DOI] [PubMed] [Google Scholar]
- Brady KT, Pearlstein T, Asnis GM, Baker D, Rothbaum B, Sikes CR, Farfel GM. Effcacy and safety of sertraline treatment of post-traumatic stress disorder: a randomized controlled trial. JAMA. 2000;283:1837–1844. doi: 10.1001/jama.283.14.1837. [DOI] [PubMed] [Google Scholar]
- Brady KT, Sonne S, Anton RF, Randall LC, Back SE, Simpson K. Sertraline in the treatment of co-occurring alcohol dependence and posttraumatic stress disorder. Alcohol Clin Exp Res. 2005;29(3):395–401. doi: 10.1097/01.alc.0000156129.98265.57. [DOI] [PubMed] [Google Scholar]
- Courtois CA, Ford JD, van der Kolk BA. Treating Complex Traumatic Stress Disorder. Guilford, New York: 2009. [Google Scholar]
- Diggle PJ, Liang KY, Zeger SL. Analysis of longitudinal data. Oxford University Press; Oxford, UK: 1994. [Google Scholar]
- Foa E, Riggs DS, Dancu CV, Constance V, Rothbaum BO. Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. J Trauma Stress. 1993;6:459–473. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. J Psychiatric Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promising treatments for women with comorbid PTSD and substance use disorders. Am J Psychiatry. 2004;161:1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Hien DA, Cohen LR, Campbell ANC. Methodological innovation to increase the utility and efficiency of psychotherapy research for patients with co-occuring mental health and substance use disorders. Professional Psychology: Research and Practice. 2009;40(5):502–509. doi: 10.1037/a0014966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Jiang H, Campbell ANC, Hu MC, Miele GM, Cohen LR, Brigham GS, Capstick C, Kulaga A, Robinson J, Suarez-Morales L, Nunes E. Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA’s Clinical Trials Network. Am J Psychiatry. 2010;167:95–101. doi: 10.1176/appi.ajp.2009.09091261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell A, Cohen L, Miele G, Killeen T, Brighman G, Zhang Y, Hansen C, Hodgkins C, Hatch-Maillette M, Brown C, Kulaga A, Kristman-Valente A, Chu M, Sage R, Robinson J, Liu D, Nunes EV. Multi-site randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. J Consult Clin Psychol. 2009;77(4):607–619. doi: 10.1037/a0016227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Society for Traumatic Stress Studies Practice Guidelines. Treatment of PTSD with comorbid disorders: Guideline 18. In: Foa EB, Keane TM, Friedman MJ, Cohen JA, editors. Effective treatments for PTSD. Guilford, New York: 2009. pp. 606–613. [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorders: A review of the literature. Am J Psychiatry. 2001;158:1184–1190. doi: 10.1176/appi.ajp.158.8.1184. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. Treating Addiction as a Human Process. Aronson; London: 1999. [Google Scholar]
- Little RJA, Rubin DB. Statistical Analysis with Missing Data. Wiley; New York: 2002. [Google Scholar]
- McLellan AT, Alterman AI, Cacciola J, Metzger D, O’Brien CP. A new measure of substance abuse treatment: Initial studies of the treatment services review. J Nerv Ment Dis. 1992;180:101–110. doi: 10.1097/00005053-199202000-00007. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Cacciola JS, Zanis D. The Addiction Severity Index-“Lite” (ASI-“Lite”) Center for the Studies of Addiction, University of Pennsylvania/Philadelphia VA Medical Center; 1997. [Google Scholar]
- Miller S, Pagan D, Tross S. Women’s Health Education: Peer activism for female partners of injection drug users. Columbia University; New York: 1998. Unpublished treatment manuscript. [Google Scholar]
- Najavits LM. Seeking Safety: A Treatment Manual for PTSD and Substance Abuse. Guilford Press; New York: 2002. [Google Scholar]
- Nunes EV, Quitkin FM, Donovan SJ, Deliyannides D, Ocepek-Welikson K, Koenig T, Brady R, McGrath PJ, Woody G. Imipramine treatment of opiate-dependent patients with depressive disorders: a placebo-controlled trial. Arch Gen Psychiatry. 1998;55:153–160. doi: 10.1001/archpsyc.55.2.153. [DOI] [PubMed] [Google Scholar]
- Saladin ME, Brady KT, Dansky BS, Kilpatrick DG. Understanding comorbidity between PTSD and substance use disorders: Two preliminary investigations. Addict Behav. 1995;20:643–655. doi: 10.1016/0306-4603(95)00024-7. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Conrod PJ, Pihl RO, Dongier M. Relations between posttraumatic stress symptom dimensions and substance dependence in a community-recruited sample of substance-abusing women. Psychol Addict Behav. 1999;13:78–88. [Google Scholar]
- Taft CT, Kaloupek DG, Schumm JA, Marshall AD, Panuzio J, King DW, Keane TM. J Abnorm Psychol. 2007;116(3):498–507. doi: 10.1037/0021-843X.116.3.498. [DOI] [PubMed] [Google Scholar]
- Triffleman E, Carroll K, Kellogg S. Substance dependence posttraumatic stress disorder therapy. An integrated cognitive-behavioral approach. J Subst Abuse Treat. 1999;17(1):3–14. doi: 10.1016/s0740-5472(98)00067-1. [DOI] [PubMed] [Google Scholar]
- van der Kolk BA, McFarlane AC, van der Hart O, Rice-Smith E. Treatment of posttraumatic stress disorder and other trauma-related disorders. In: Speigle D, editor. Efficacy and Cost Effectiveness of Psychotherapy. American Psychiatric Press, Inc; Washington, DC: 1999. pp. 63–72. [Google Scholar]


