Abstract
Background: although the majority of hip fractures are the result of a fall, whether repeated falls in the year post-fracture adversely influence recovery of social participation is not known.
Design: analysis of data from a longitudinal cohort study.
Subjects: community-dwelling women aged ≥65 years, admitted to one of two hospitals in Baltimore with a new, non-pathological fracture of the proximal femur between 1992 and 1995.
Methods: information on falls was collected from a falls diary. At the baseline, 6- and 12-month evaluations, subjects were asked about the number of times in the 2 weeks prior to the evaluation they had participated in 10 categories of social activities. We examined the association of repeated falls with social participation using generalized estimating equations. The effect of physical and psychological functions was examined by including measures of lower extremity functional performance and depressive symptoms into the model.
Results: the analyses included 196 women, mean age = 80.2 years. Eighty-one subjects fell. The subjects with >1 fall between evaluations participated in a mean (95% CI) of 3.5 (0.12, 6.9) and 4.3 (0.9, 7.7) fewer social activities at 6 and 12 months post-fracture, respectively, compared to those who did not fall (P = 0.0003). These results were attenuated by adjustment for depressive symptoms, but not by lower extremity functional performance.
Conclusions: in the year post-fracture, repeated falls in women were associated with decreased social participation independent of lower extremity function. Depressive symptoms in repeated fallers may partly explain this association.
Keywords: accidental falls,; hip fracture; social activities; aged; elderly
Introduction
Falls in elders are associated with several dangerous consequences including hip fracture [1]. The return to pre-fracture social activity participation is one aspect of hip fracture recovery that is often overlooked, but may have important implications for quality of life post-fracture. Social engagement in later life is associated with fewer depressive symptoms as well as a longer survival [2]. The loss of lower extremity function that frequently follows a hip fracture can inhibit the recovery of previous social activity. Falls in the year post-fracture may disrupt this recovery process since falls have been associated with activity avoidance [3] and depressive symptoms in older adults [4], factors that might influence participation in social activities.
Although nearly all adults who suffer a hip fracture have experienced an injurious fall [5], not all will continue to fall. Whether individuals who suffer falls in the year post-fracture are less likely to participate in social activities is not known, and whether this association may be explained by worse lower extremity function post-fracture or an increase in depressive symptoms in those who fall is also not known. A better understanding of the influence of factors, such as falls, lower extremity functioning and depressive symptoms on the recovery of social functioning, may provide opportunities to improve outcomes for hip fracture patients. We examined data from a prospective cohort from the Baltimore Hip Studies (BHS), in which women were followed for a year post-fracture, to explore whether falls in the year post-fracture impact the recovery of social participation.
Methods
Subjects were drawn from the third cohort in the BHS (BHS-3). Between 1992 and 1995, 205 Caucasian women, aged ≥65 years, admitted to one of two hospitals in Baltimore with a new fracture of the proximal femur agreed to participate in a prospective study. Women with distal femur fractures, admissions >48 h after the fracture and men were excluded from this study. During the 3 years, 407 eligible white female subjects were identified and 205 women (50%) agreed to participate.
Subjects were evaluated by the trained BHS-3 staff within 10 days of hospitalisation for hip fracture and then again at 2, 6 and 12 months post-fracture. Proxy data were collected whenever subject data were unavailable or the subject was cognitively impaired [Mini-Mental State Exam (MMSE) [6] score <17]. The study protocol was approved by the Institutional Review Boards of both hospitals and of the University of Maryland. A more detailed description of this cohort may be found elsewhere [7].
Fall assessments
Study participants were given a fall calendar and were told to record the date and time of any fall [8]. Study staff reviewed the fall calendars during the year post-hip fracture and recorded the number of falls that had occurred since the previous evaluation. They also inquired about falls not listed in the calendar and gathered more detailed information regarding the circumstances and resulting injuries of any falls.
Social activities
At each evaluation, the subjects were asked about the number of times in the previous 2 weeks they had done the following activities: (i) gone to the movies, concerts, plays or sporting events; (ii) gone to fairs, museums or exhibits; (iii) attended meetings, appointments, classes or lectures; (iv) gone to church or temple services; (v) gone on pleasure drives or picnics; (vi) played cards, bingo etc. with others; (vii) gone to family/friends’ homes for a meal; (viii) participated in active sports or swimming; (ix) worked in the garden/yard or at a hobby and (x) done community or volunteer work.
These items were derived from a measure of social functioning developed by House [9] that has been associated with mortality. It has previously been used to measure recovery of social function after hip fracture [9, 10].
At the baseline evaluation, the subjects reported on their participation during the 2 weeks prior to the fracture in these same activities. As has been done in previous hip fracture studies [1], a summary score of social participation was calculated as the total number of times in which the subject participated in any of the 10 activity categories during the 2-week period in question.
Covariates
Physical function
Pre-fracture self-reported lower extremity function
At the baseline evaluation, subjects responded to questions regarding their need for assistance during the week prior to the fracture with 12 lower extremity tasks: (i) walking 10 feet or across a room; (ii) walking one block on a level sidewalk; (iii) climbing five stairs; (iv) getting into a car; (v) getting in/out of bed; (vi) rising from an armless chair; (vii) putting on pants; (viii) putting socks/shoes on both feet; (ix) reaching for an item on the ground from a sitting position; (x) getting in/out of a bath or shower; (xi) taking a bath, shower, or sponge bath and (xii) getting on/off the toilet. From these responses, a summary scale of activities of daily living requiring lower extremity functioning (LE-ADL) was calculated as a count of the number of tasks in which the person required either human or equipment assistance or both or was completely unable to perform. The scale thus ranges from 0 to 12 with higher scores representing greater impairment.
Post-fracture observed lower extremity functional performance
Timed performance of nine lower extremity tasks was assessed at each post-fracture evaluation: (i) reach for an item on the ground from a sitting position; (ii) put a sock on the fractured-side foot; (iii) put a shoe on the fractured-side foot; (iv) rise from an armless chair; (v) walk 10 feet; (iv) step up four steps; (vii) step down four steps; (viii) get on the toilet and (ix) get off the toilet. The times for performance on each task were compared to the range of times performed by all subjects in order to obtain a score of 1–3, with higher scores indicating better performance and individuals unable to perform the task receive a 0 [11]. Therefore, performance of these tasks was scored on a scale of 0–4 to create a summary score of lower extremity function, the Lower Extremity Gain Scale (LEGS). This score ranges from 0 to 36 with higher scores indicating better performance and a difference of 2.6 points on this scale is believed to be clinically important [12].
Depressive symptoms
Depressive symptoms were assessed at each time point using the Geriatric Depression Scale (GDS), a 15-item version [13].
Others
Age was assessed at the baseline evaluation. The data on the pre-fracture presence of eight chronic medical conditions that have previously been found to be adversely associated with functional recovery in hip fracture patients [14] were collected from the hospital record. The data on the presence or absence of 23 possible in-hospital complications was similarly collected from a review of the hospital record. A list of the selected co-morbidities and complications can be found elsewhere [14]. At each evaluation, subjects reported on whether they had used anxiolytic or sedative medications and on alcohol consumption. Mental status was assessed at each evaluation using the MMSE [6].
Statistical analyses
The total number of falls that had occurred prior to each evaluation was calculated. Because, on average, social functioning has been found to recover between the 6 and 12 months post-fracture period [1], falls in the 0–6 month and 6–12 month time periods were examined for their relationship with social functioning at 6 and 12 months post-fracture, respectively. Since >1 fall in a 6-month period may reflect worse functional status [15, 16], the subjects were divided into three groups (no falls, 1 fall, >1 fall) based on the number of falls they experienced in each of the 6-month intervals of the follow-up period.
Baseline characteristics of patients were compared between fall groups using the chi-square test and Fisher's exact test (for categorical and dichotomous variables) and using t-tests (for continuous variables).
Because participants can contribute more than one data point in these analyses, generalized estimating equations (GEE) [17] were used to model the longitudinal relationship between the fall category (no falls, 1 fall, >1 fall), in both 6-month time periods, and social participation at the end of these periods (6 and 12 months post-fracture, respectively) in order to account for correlations across the two time periods within individuals. Generalized F-tests were used to compare social activity trajectories between the fall categories, and time-specific confidence intervals were calculated when a significant difference (P < 0.05) between social activity trajectories was observed. All models adjusted for age, the number of co-morbid medical conditions, post-surgical complications, MMSE score, time post-fracture, pre-fracture social activity level and self-reported pre-fracture lower extremity function.
Because falls may further influence lower extremity function [18], we examined whether an association of falls on participation in social activities is explained by worse post-fracture lower extremity function by including the LEGS score at the current evaluation into the model. Similarly, because social activity restriction has been reported to be more common in individuals with depressive symptoms following a fall [19] that may be associated with fear of falling [20], we examined whether depressive symptoms explained the observed association by including GDS scores at the current evaluation into the model. Because injuries from falls might affect the ability to participate in social activities, the presence of an injurious fall during the evaluation period was included in the model. Psychotropic medication use and regular alcohol consumption are believed to increase fall risk [21, 22]; therefore, use of medications for sleep or anxiety and the daily use of alcohol were also included in the model.
The validity of GEE results are contingent on missing data being missing completely at random (MCAR) as defined by Rubin [23]. A sensitivity analysis of the MCAR assumption using weighted estimating equations (WEEs) was performed [24], as has been done in previous studies using this hip fracture cohort [14, 25, 26].
All analyses were performed using the statistical package SAS version 9.1 (SAS Institute, Cary, NC).
Results
Falls data were collected from 196 participants over the first 6 months, and from 156 participants from 6 to 12 months post-fracture. Of these individuals, 117 provided complete covariate information for inclusion in the primary analysis. The baseline characteristics of participants are shown in Table 1. In the 12 months post-fracture, 81 individuals (41%) fell at least once. Of these individuals, 37 (46%) reported that they had sustained an injury as a result of a fall (Table 2); with bruises or bleeding reported in 11 participants (30%), fractures reported in 7 participants (19%), a head injury reported in 4 participants (11%) and an unspecified injury occurred in 4 participants (11%).
Table 1.
Baseline characteristics of the study sample
| No falls (N = 138) | 1 fall (N = 29) | > 1 fall (N = 27) | ||
|---|---|---|---|---|
| Age [mean (SD)] | 80.0 (7.4) | 79.1 (8.6) | 87.0 (5.3) | P = 0.01 (>1 fall vs. no falls) |
| Co-morbidities (N (%)) | ||||
| Cardiovascular disease | 48 (35) | 9 (31) | 14 (52) | P = 0.19 |
| Osteoarthritis | 50 (36) | 8 (27) | 8 (29) | P = 0.58 |
| Stroke | 13 (9) | 1 (3) | 4 (15) | P = 0.34 |
| Congestive heart failure | 15 (11) | 7 (24) | 7 (26) | P = 0.04 |
| Dementia | 15 (11) | 2 (7) | 9 (33) | P = 0.004 |
| Diabetes | 17 (12) | 4 (14) | 6 (22) | P = 0.39 |
| Peripheral vascular disease | 5 (4) | 3 (10) | 2 (7) | P = 0.28 |
| COPD | 30 (22) | 5 (17) | 4 (15) | P = 0.65 |
| Pre-fracture LE-ADL score [mean (SD)] | 4.4 (3.4) | 4.8 (3.4) | 5.6 (3.2) | P = 0.09 (>1 fall vs. no falls) |
| Pre-fracture social activities [mean (SD)] | 10.5 (8.7) | 10.9 (12.6) | 6.5 (5.3) | P = 0.12 (>1 fall vs. no falls) |
| MMSE [mean (SD)] | 24.7 (4.5) | 22.1 (6.7) | 22.9 (5.6) | P = 0.02 (1 fall vs. no falls) |
| GDS [mean (SD)] | 3.7 (2.8) | 4.4 (3.9) | 5.1 (3.2) | P = 0.09 (>1 fall vs. no falls) |
| In-hospital complications [Mean (SD)] | 0.43 (1.1) | 0.72 (1.2) | 0.85 (1.0) | P = 0.07 (>1 fall vs. no falls) |
Differences between fall groups were assessed using the chi-square test (for categorical variables) and using t-tests (for continuous variables). SD = standard deviation; LE-ADL = lower extremity activities of daily living; MMSE = Mini-Mental Status Examination; GDS = geriatric depression scale
Table 2.
Follow-up measures
| 6-Months | 12-Months | |||||||
|---|---|---|---|---|---|---|---|---|
| No falls | One fall | >1 fall | No fall | One fall | >1 fall | |||
| (N = 138) | (N = 29) | (N = 27) | (N = 109) | (N = 24) | (N = 23) | |||
| Social activities [Mean (SD)] | 10.2 (10.0) | 8.9 (11.1) | 3.5 (5.7) | P = 0.02 (>1 Fall vs. no falls) | 10.1 (10.2) | 8.5 (10.9) | 3.9 (5.0) | P = 0.03 (>1 fall vs. no falls) |
| LE-ADL [Mean (SD)] | 7.0 (3.3) | 8.0 (2.7) | 8.7 (3.0) | P = 0.03 (>1 Fall vs. no falls) | 6.9 (3.4) | 6.7 (2.9) | 9.2 (2.9) | P = 0.005 (>1 fall vs. no falls) |
| GDS [Mean (SD)] | 3.5 (3.0) | 4.3 (3.1) | 5.0 (3.4) | P = 0.09 (>1 Fall vs. no falls) | 3.4 (2.9) | 3.9 (2.8) | 5.6 (3.7) | P = 0.01 (>1 fall vs. no falls) |
| Injurious falls [N (%)] | N/A | 7 (27) | 10 (56) | P = 0.07 | N/A | 12 (55) | 9 (56) | P = 1.0 |
| Used sleep medications [N (%)] | 36 (35) | 6 (29) | 2 (12) | P = 0.16 | 18 (27) | 1 (5) | 6 (40) | P = 0.03 |
| Used medications for anxiety [N (%)] | 29 (28) | 7 (33) | 4 (24) | P = 0.79 | 8 (15) | 3 (15) | 3 (21) | P = 0.85 |
| Daily alcohol consumption [N (%)] | 13 (13) | 3 (14) | 1 (6) | P = 0.66 | 7 (10) | 3 (14) | 2 (13) | P = 0.87 |
Differences between fall groups were assessed using the chi-square test and Fisher's exact test (for categorical and dichotomous variables) and using t-tests (for continuous variables). SD = standard deviation; LE-ADL = lower extremity activities of daily living; GDS = geriatric depression scale.
Social function improved during the year post-fracture with the mean (SD) number of social activities reported by study participants as 6.8 (8.4), 9.2 (10.0) and 8.9 (10.0) at 2, 6 and 12 months post-hip-fracture, respectively.
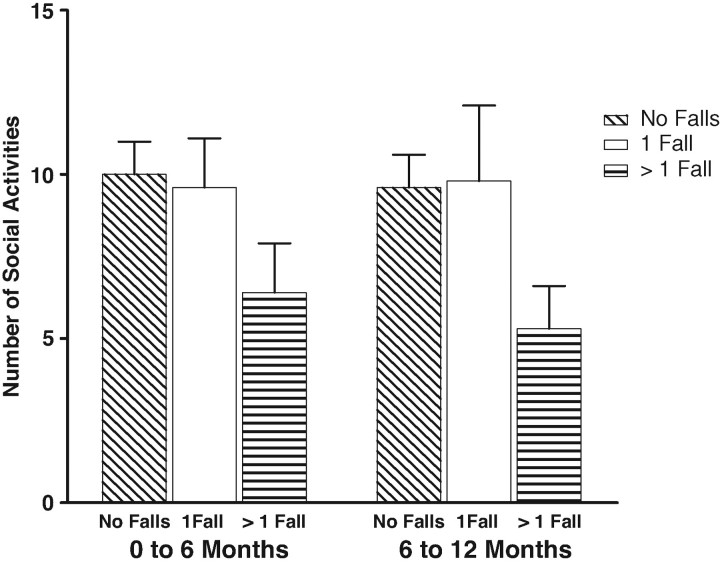
Adjusted for covariates, there was no difference in social participation between subjects with one fall compared to those with no falls (P = 0.92 for longitudinal analysis). Subjects who fell more than once, however, participated in fewer social activities in the year post-hip fracture than those who did not fall (P = 0.01 for longitudinal analysis). On average, those who fell more than once in the first and last 6-month periods post-hip fracture reported participation in a mean (95% CI) of 3.5 (0.12, 6.9) and 4.3 (0.9, 7.7) fewer social activities compared to non-fallers at the 6 and 12 months post-fracture evaluations, respectively (Figure 1).
Figure 1.
Adjusted* mean (±SEM) number of social activities by fall status. *Adjusted for age, co-morbidity, post-surgical complications, MMSE score, time post-fracture, pre-fracture social activity level and pre-fracture LE-ADL score.
Adjustment for the LEGS score did not attenuate the observed association (data not shown); however, adjustment for depressive symptoms did result in an attenuation of the association between repeated falls and social activity participation of 11% and 14%, with repeated fallers reporting a mean (95% CI) of 3.1(−0.5, 6.8) and 3.7 (−0.3, 7.0) fewer social activities at 6 and 12 months post-fracture, respectively.
Adjustment for psychotropic medication use, regular alcohol consumption or the presence of injurious falls did not significantly alter the observed association between falls and recovery of social functioning (data not shown). The sensitivity analysis yielded similar results and the same conclusions as the GEE analysis (data not shown).
Discussion
In these analyses from the BHS, women who fell only once during each 6-month follow-up time period reported similar levels of social activities as those who did not fall; however, those who fell more than once reported participation in fewer social activities than those who did not fall at each of the 6 and 12 month evaluations. Adjustment for a global measure of lower extremity functional performance did not attenuate this association, suggesting that the decreased social participation in this group was not explained by worse lower extremity function. Adjustment for depressive symptoms, as measured by the GDS scale, did however result in an attenuation of this association by ∼11–14%, suggesting that the observed association may be explained, in part, by an increase in depressive symptoms in those with multiple falls.
The association of multiple (>1) falls with decreased social participation is consistent with previous studies that found that in community-dwelling elders, multiple falls, but not a single fall, were associated with the increased risk for activity avoidance, including avoidance of social activities [3].
Although poorer physical functioning has been associated with physical activity restriction [27], in the analyses presented here, the association of multiple falls with social activity participation persisted even after adjusting for lower extremity functioning, suggesting that another mechanism may explain this relationship.
Depressive symptoms and depression are also believed to negatively impact functional recovery after hip fracture surgery [28], and in our analyses, adjustment for depressive symptoms resulted in an attenuation of the observed relationship. This suggests that an increase in depressive symptoms in those with multiple falls may play a role. Multiple fallers are believed to also be at greater risk for fear of falling than those with one or fewer falls [3], and fear of falling has been seen to have a significant impact on activity restriction in both individuals who have and have not fallen [29, 30]. This fear, that may be present for those who fall, especially those who fall more than once, may be a factor in the causal pathway to social activity restriction. Because individuals who are fearful of falling are also believed to be more likely to show depressive symptoms or a depressed mood [4], this may explain why depressive symptom scores partially attenuated the association in the current analysis.
The lack of a measure of fear of falling in the BHS-3 dataset is a limitation of these analyses, and re-evaluation of these results in hip fracture patients, in whom a validated measure of fear of falling is used, would be important. Also all of the subjects included in these analyses were white women and thus we are unable to assess whether similar associations exist in men or in women of other ethnicities. Another limitation is that the social functioning measure is not a standard measure that has been rigorously validated. Further research would benefit from the use of a standard measure of social functioning in order to compare the results more effectively to the current literature. We also have no information on pre-fracture depression or depressive symptoms and are therefore unable to assess how pre-existing depression might influence the observed associations. The age of the data can be viewed as a potential limitation to the interpretation of the analyses; however, although there have been significant changes to in-hospital care of hip-fracture patients in the years since 1995, analyses of more recent cohorts from the BHS suggests that the post-discharge pattern of recovery remains very similar. As a result, it is unlikely that the association of falls with the recovery of social functioning has changed during this time and the interpretation of the main analyses presented here are likely to still be of relevance today.
In conclusion, we found that in women, the presence of multiple falls was associated with participation in fewer social activities in the year post-hip fracture independent of lower extremity function. An increase in depressive symptoms in those with multiple falls may explain, in part, this relationship. Future research on social activity recovery using a specific measure of fear of falling is needed to further evaluate these associations.
Key points
Resumption of social activities is an important aspect of recovery from hip fracture.
Older women who fell two or more times in a 6-month period after hip fracture participated in fewer social activities than those who did not fall.
This association was not explained by worse lower extremity function in those who fell, but was partially explained by an increase in depressive symptoms in those with repeated falls.
References
- 1.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol Med Sci. 2000;55A:M498–507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 2.Glass TA, Mendes de Leon C, Marottoli RA, Berkman LF. Population based study of social and productive activities as predictors of survival among elderly Americans. BMJ. 1999;319:478–83. doi: 10.1136/bmj.319.7208.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zijlstra GAR, van Haastregt JCM, van Eijk JTM, van Rossum E, Stalenhoef PA, Kempen GIJM. Prevalence and correlates of fear of falling, and associated avoidance of activity in the general population of community-living older people. Age Ageing. 2007;36:304–9. doi: 10.1093/ageing/afm021. [DOI] [PubMed] [Google Scholar]
- 4.Gagnon N, Flint AJ, Naglie G, Devins GM. Affective correlates of fear of falling in elderly persons. Am J Geriatr Psychiatry. 2005;13:7–14. doi: 10.1176/appi.ajgp.13.1.7. [DOI] [PubMed] [Google Scholar]
- 5.Fox KM, Hawkes WG, Hebel JR, et al. Mobility after hip fracture predicts health outcomes. J Am Geriatr Soc. 1998;46:169–73. doi: 10.1111/j.1532-5415.1998.tb02534.x. [DOI] [PubMed] [Google Scholar]
- 6.Folstein MF, Folstein SE, McHugh PR. ‘Mini-Mental state’—A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 7.Fox KM, Magaziner J, Hawkes WG, et al. Loss of bone density and lean body mass after hip fracture. Osteoporos Int. 2000;11:31–5. doi: 10.1007/s001980050003. [DOI] [PubMed] [Google Scholar]
- 8.Magaziner J, Zimmerman SI, Gruber-Baldini A, Hebel JR, Fox KM. Proxy reporting in five areas of functional status: comparison with self-reports and observations of performance. Am J Epidemiol. 1997;146:418–28. doi: 10.1093/oxfordjournals.aje.a009295. [DOI] [PubMed] [Google Scholar]
- 9.House JS, Robbins C, Metzner HL. The association of social relationships and activities with mortality: prospective evidence from the Tecumseh Community Health Study. Am J Epidemiol. 1982;116:123–40. doi: 10.1093/oxfordjournals.aje.a113387. [DOI] [PubMed] [Google Scholar]
- 10.Mortimore E, Haselow D, Dolan M, et al. Amount of social contact and hip fracture mortality. J Am Geriatr Soc. 2008;56:1069–74. doi: 10.1111/j.1532-5415.2008.01706.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zimmerman S, Hawkes WG, Hebel JR, Fox KM, Lydick E, Magaziner J. The Lower Extremity Gain Scale: a performance-based measure to assess recovery after hip fracture. Arch Phys Med Rehabil. 2006;87:430–6. doi: 10.1016/j.apmr.2005.10.026. [DOI] [PubMed] [Google Scholar]
- 12.Hawkes WG, Williams GR, Zimmerman S, et al. A clinically meaningful difference was generated for a performance measure of recovery from hip fracture. J Clin Epidemiol. 2004;57:1019–24. doi: 10.1016/j.jclinepi.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 13.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1983;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 14.Miller RR, Cappola AR, Shardell MD, et al. Persistent changes in interleukin-6 and lower extremity function following hip fracture. J Gerontol A Biol Sci Med Sci. 2006;61:1053–8. doi: 10.1093/gerona/61.10.1053. [DOI] [PubMed] [Google Scholar]
- 15.Stalenhoef PA, Diederiks JPM, Knottnerus JA, Kester ADM, Crebolder HFJM. A risk model for the prediction of recurrent falls in community-dwelling elderly: a prospective cohort study. J Clin Epidemiol. 2002;55:1088–94. doi: 10.1016/s0895-4356(02)00502-4. [DOI] [PubMed] [Google Scholar]
- 16.Vassallo M, Sharma JC, Allen SC. Characteristics of single fallers and recurrent fallers among hospital in-patients. Gerontology. 2002;48:147–50. doi: 10.1159/000052833. [DOI] [PubMed] [Google Scholar]
- 17.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 18.Martin FC, Hart D, Spector T, Doyle DV, Harari D. Fear of falling limiting activity in young-old women is associated with reduced functional mobility rather than psychological factors. Age Ageing. 2005;34:281–7. doi: 10.1093/ageing/afi074. [DOI] [PubMed] [Google Scholar]
- 19.Williams C, Tinetti M, Kasl S, Peduzzi P. The role of pain in the recovery of instrumental and social functioning after hip fracture. J Aging Health. 2006;18:743–62. doi: 10.1177/0898264306293268. [DOI] [PubMed] [Google Scholar]
- 20.Lach HW. Incidence and risk factors for developing fear of falling in older adults. Public Health Nurs. 2005;22:45–52. doi: 10.1111/j.0737-1209.2005.22107.x. [DOI] [PubMed] [Google Scholar]
- 21.Berry SD, Miller RR. Falls: epidemiology, pathophysiology, and relationship to fracture. Curr Osteoporos Rep. 2008;6:149–54. doi: 10.1007/s11914-008-0026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mukamal KJ, Mittleman MA, Longstreth WTJ, Newman AB, Fried LP, Siscovick DS. Self-reported alcohol consumption and falls in older adults: cross-sectional and longitudinal analyses of the cardiovascular health study. J Am Geriatr Soc. 2004;52:1174–9. doi: 10.1111/j.1532-5415.2004.52318.x. [DOI] [PubMed] [Google Scholar]
- 23.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–92. [Google Scholar]
- 24.Robins JM, Rotnitzky A, Zhao LP. Analysis of semiparametric regression models for repeated outcomes in the presence of missing data. J Am Stat Assoc. 1995;90:106–21. [Google Scholar]
- 25.Miller RR, Hicks GE, Shardell MD, et al. Association of serum vitamin D levels with inflammatory response following hip fracture–The Baltimore Hip Studies. J Gerontol A Biol Sci Med Sci. 2007;62:1402–6. doi: 10.1093/gerona/62.12.1402. [DOI] [PubMed] [Google Scholar]
- 26.Miller RR, Shardell MD, Hicks GE, et al. Association between interleukin-6 and lower extremity function after hip fracture—the role of muscle mass and strength. J Am Geriatr Soc. 2008;56:1050–6. doi: 10.1111/j.1532-5415.2008.01708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bruce D, Devine A, Prince R. Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc. 2002;50:84–9. doi: 10.1046/j.1532-5415.2002.50012.x. [DOI] [PubMed] [Google Scholar]
- 28.Zimmerman SI, Smith HD, Gruber-Baldini A, et al. Short-term persistent depression following hip fracture: a risk factor and target to increase resilience in elderly people. Soc Work Res. 1999;23:187–96. [Google Scholar]
- 29.Murphy S, Dubin J, Gill T. The development of fear of falling among community-living older women: predisposing factors and subsequent fall events. J Gerontol: Med Sci. 2003;58A:943–7. doi: 10.1093/gerona/58.10.m943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist. 2002;42:17–23. doi: 10.1093/geront/42.1.17. [DOI] [PubMed] [Google Scholar]