Abstract
Objectives
1) To determine the rates of past year non-partner violent assault (NPV), both victimization and aggression. 2) To assess variables associated with NPV, particularly with regards to substance use.
Method
A cross sectional computerized standardized survey study was conducted to assess NPV, physical and mental health, and substance use among patients presenting to an inner-city ED over two years. Patients (age 19–60) with normal vital signs in an urban ED from 9am–11pm were eligible; pregnant patients and those with a chief complaint of psychiatric evaluation were excluded. Logistic regression analyses were conducted to predict any NPV
Results
10,744 patients were enrolled (80 % response rate); 14% of the sample reported any past year NPV (9% perpetration; 11% victimization). Findings from regression analyses found participants with any past year NPV (victimization or aggression) were more likely than their counterparts to be younger (OR 1.1), male (2.2), single (1.5), unemployed (1.1), present to the ED for injury (1.9), report poor physical health (1.32) poor mental health (1.9). They were less likely to be African-American (0.8). Alcohol use (1.7), marijuana use (2.4), cocaine use (3.1), prescription drug use (1.4) and past treatment (1.7) were associated with experiencing past year NPV.
Conclusions
Fourteen percent of patients seeking care in this inner-city ED experience violence with a non-partner. Substance use and cocaine specifically, was the strongest predictor of any NPV.
Background
Each year more than 37 million patients visit emergency departments (EDs) with injuries.1 Of these visits, approximately 17% are related to violence or assault. Research from multiple disciplines suggests that violent injury is non-random and is best predicted by the past experience and behavior.2 Among fatal injuries, 20% are related to interpersonal violence.3 Assault-related injuries have reached epidemic numbers, exceeding 2 million persons annually4 with homicide a leading cause of death among young adults.5 Often, in non-intimate partner violence, the victim and assailant know each other, with friends or relatives involved in the majority of gun-related violence.6–8 Nationally more individuals report victimization by friends or acquaintances, then by spouses or dating partners.9 Among women in the ED, prior research finds that half of assault-related injuries were perpetrated by a non-partner,10 underscoring the importance of understanding violence outside of intimate partner relationships.
A potentially critical factor in violence is alcohol and illicit drug use.11, 12 High rates of alcohol use and alcohol intoxication at the time of the event were found among individuals incarcerated for violent offenses.13, 14 Among cocaine users in the ED, Cunningham et al. (2007)15 found non-partner violence (NPV) was significantly related to greater binge drinking, diagnosis of substance or dependence, greater legal involvement, and higher rates of seeking medical attention for intentional injuries. Chermack et al. (2001)16 found significant associations between NPV and demographic variables (e.g., minority status, years of education), days of substance use (e.g., cocaine), and overall psychological distress in a substance use treatment sample. To date, no ED-based studies have evaluated violence in a non-partner context among a general sample of ED patients.
Importance
Although there has been an increase in the number of studies on violent assault (both aggression and victimization) and substance use among ED patients, most of the violence related research has focused on intimate partner violence (IPV).17–19 Patients who are admitted to a trauma service overnight following a violent injury have been found to have a high risk of adverse outcomes in the subsequent year with one study reporting that 13% were incarcerated, 44% experienced a repeat violent injury, and 20% were victims of homicide.20
Other ED-based studies of violent injury among non partners have focused only on patients injured severely enough to require a trauma consult or hospital admission, thus missing a huge section of the injured population who are treated and released. Furthermore, prior research on non-IPV has focused on the injury (laceration, gun shot wound, or contusion) that brought the patient to the ED, thereby limiting the ability to understand other recent episodes of violence. Data are lacking on the involvement of violence among the majority of patients treated in an inner city ED for medical illness or non life threatening injury, which would inform injury prevention efforts. The ED presents an opportunity to interface with patients at high risk for violence. This ED visit may be the only health system interaction prior to interfacing with the criminal justice system; yet, currently little is known about the prevalence or characteristics of violence among non-partners seeking ED care for injury or illness.
Although many patients with violent injuries from an assault are victims experiencing an isolated tragic event, others may be recurrently involved with violence and could benefit from targeted referral-based interventions appropriate to their history and risk factors. For example, studies have demonstrated that the psychological and descriptive profiles of both assailants and victims of intentional injury are quite similar; frequently the victims are the offenders in other assaults.21, 22 Patients involved in violence in non-partner relationships are also likely to be involved in aggression or victimization in partner relationships.23, 24 Data regarding the relationship between violence and substance use in a consecutive sample of patients presenting over a two-year period to an inner city ED could provide valuable information to determine the need for, and content of, future violent injury prevention programs.
Goals of This Investigation
The primary aims of this study were: 1) To determine the prevalence of past year non-partner violent assault (NPV), both victimization and aggression, and, 2) To assess variables associated with NPV, particularly with regards to substance use.
The prevalence of NPV in national surveys appear to be equal to or greater than IPV rates.8, 9 It is critical to understand the experiences with NPV among adult ED patients to better inform the assessment, treatment, and prevention of violence-related injury. Specifically, based on previous research, we hypothesized that male gender,16 younger age,25, 26 unemployment,27, 28 fewer years of education,27, 29 and less income16 would be associated with NPV. We expected that both poorer mental and physical health would be associated with NPV.30, 31 Finally, given findings from clinical and laboratory research,32, 33 we hypothesized that participants with a past year history of NPV would be more likely to have used alcohol, cocaine, cannabis, and/or prescription drugs (opiates/ depressants sedatives), compared to those with no NPV.
Methods
Study Design
An observational cross-sectional survey study was conducted. Patients (ages 19–60) seeking care for injury or medical complaints were approached by research staff to participate in this computerized survey study. Bachelor level research staff recruited patients who were in treatment spaces in the ED from 9am – 11pm, seven days a week over a full two-year period. This does not include patients treated at study ED on days not covered by research recruiting staff (excluding major holidays, RA vacation days, RA sick days). During hours when an RA was present, consecutive patients in treatment spaces were systematically sampled. After obtaining written consent, the 10–15 minute screen was administered to eligible patients.
Setting
The study site was an inner-city Level 1 trauma center ED in Flint, Michigan, with an annual ED census of approximately 50,000 adult patients (of which ~50–60 % are African American). Hurley Medical Center is the only public hospital in the city. Flint is comparable in terms of poverty and crime to the other urban centers such as Detroit, Hartford, Camden, St Louis, Oakland.34 The population of Flint is 50% African-American.35 The study protocol was approved by Institutional Review Boards (IRB) for Research with Human Participants at the University of Michigan and the Hurley Medical Center; Certificates of Confidentiality were obtained from NIAAA and NIDA.
Selection of Participants
All potentially eligible adult patients presenting to the ED for medical illness or injury were approached to complete a computerized survey as part of a larger randomized controlled trial linking patients to substance use treatment. Patients who were ambulatory or arrived by ambulance were eligible, providing they were not triaged to the resuscitation bays. Patients were excluded if they were pregnant, had abnormal vital signs, or were unable to provide informed consent (e.g. unconscious, police custody). Patients seeking care solely for psychiatric evaluations (i.e. chief complaint suicidal ideation, psychosis) were not eligible. In this manner, this study focuses on the rates of violence and substance use among patients who would not receive further mental health evaluation or intervention in the ED. Patients who were acutely intoxicated at the initial ED presentation were approached following clearing of mental status. Patients who declined to participate provided their gender and race as well as reasons for refusing to participate. (Our IRB did not allow collection of additional data regarding patients who declined participation without written consent.) Data for this paper were obtained for two full years of recruitment (April, 2006 –March, 2008).
Methods of Measurement
Potential NPV risk domains were selected based on theoretical models of violence and prior findings,33, 36–39 and included demographics (age, minority status, gender), health factors (physical and mental health history), and substance use history (i.e., alcohol, cocaine, cannabis, past 3-month treatment) factors (see Appendix A for theoretical model).
Participants completed a computerized survey, with aid from a RA if needed, regarding demographics (age, gender, race/ethnicity, marital status, income, and years of education completed),40 health status, substance use, and violence (see Appendix B for survey). The survey took ~10–15 minutes to complete and was in English only (consistent with the study site population). Participants completed the survey in a treatment room. The site IRB did not allow surveys to be completed in the waiting room. RA staff paused the computer when medical staff was present or if participant went to testing, and was available to answer questions. The survey did not impact patient flow.
Assault: NPV victimization and aggression
NPV victimization was assessed by one item from the Partner Violence Screen (PVS)41 and adapted for non-partners: “In the past year, have you been hit, kicked, punched, or otherwise hurt by friends, strangers, neighbors, people in bars, coworkers, bosses?”. In a similar manner, NPV aggression was assessed by asking: “In the past year, have you hit, kicked, punched, or otherwise hurt friends, strangers, neighbors, people in bars, coworkers, bosses?” Although this one item screen has not be validated, the full length PVS has adequate sensitivity (54.5–71.4) and specificity (80.3–84.4) as compared to more lengthy measures for use in ED settings.42
Physical and Mental Health Functioning
The SF-12 Health Survey which has been validated in an ED setting43 was used to assess physical and mental health functioning over the prior 4 weeks.44–46 For analysis purposes, a cut-off at the 25th percentile on the SF-12 was used to indicate low/high functioning in each domain.
Alcohol and Drug Use
Frequency of substance use (past 4 weeks) and related symptoms of abuse/dependence were determined by items from the Substance Abuse Outcomes Module47 The SAOM was used to measure alcohol and drug use (illicit and prescription use) along with questions to ascertain separate DSM-IV diagnoses for alcohol, cocaine, and marijuana abuse and dependence. Prescription drug use included: Opiates (i.e. Morphine, Codeine, Vicodin, , OxyContin, Darvocet, Percodan, Fentanyl, etc ) and Sedative/Depressants ( i.e. , Xanax, Librium, Quaaludes, Halcion, sleeping pills, nerve pills, downers, barbiturates etc). One additional item from the SAOM investigates the timing of substance use and fighting “I got into physical fights while using alcohol or drugs”. The SAOM has demonstrated reliability (internal reliability coefficient 0.58–0.90, test-retest reliability 0.56–0.99) and validity (concurrent validity 0.5–0.8, predictive validity 0.5–0.9).47
In order to tease apart differential effects of the most commonly used substances (alcohol, marijuana, and cocaine) in our sample, we constructed the following three variables: alcohol use only (these patients did not use marijuana or cocaine), marijuana use (with or with out alcohol), and cocaine use (with or without marijuana or alcohol). This 3 category approach was chosen to represent an increasing severity of substance use (patients with any cocaine use are hypothesized to be a different patient population then those who report, any marijuana use without other illicit drugs, or alcohol alone without illicit drug use). Participants also reported if they had been in treatment for substance use in the past 3 months.
Chief Complaint
Trained research staff recorded the reason for the current ED visit (medical or injury) at the time of the survey administration as stated by the patient. Patients were not asked if their visit was the result of violence.
Data Analysis
Data analyses were conducted with SAS version 9.1 for Windows (Cary, NC). Responses to demographic responses were dichotomized into the following categories for analysis: African American (yes/no); married/ living together (yes/ no); any college education or more (yes/ no); income less than $20,000 (yes/no), health insurance (yes/ no), employed (yes /no). Age was analyzed as a continuous variable. Demographic variables were dichotomized to ease clinical interpretation, based on the current literature on NPV and substance use.26, 28, 48
First, we present prevalence of past year assault (NPV) in this sample. Second, characteristics of patients with and without past year NPV victimization, and with and without NPV aggression are presented. Third, due to the similarity of victimization and aggression results, these variables were collapsed into any NPV, and bivariate associations evaluating participants with and without any non-partner violence were conducted. Finally, three separate logistic regression analyses were conducted to predict: any NPV (presented in main results), non-partner aggression, and non-partner victimization. See technical Appendix C for details of analysis, handling of missing values, and regression diagnostics.
Results
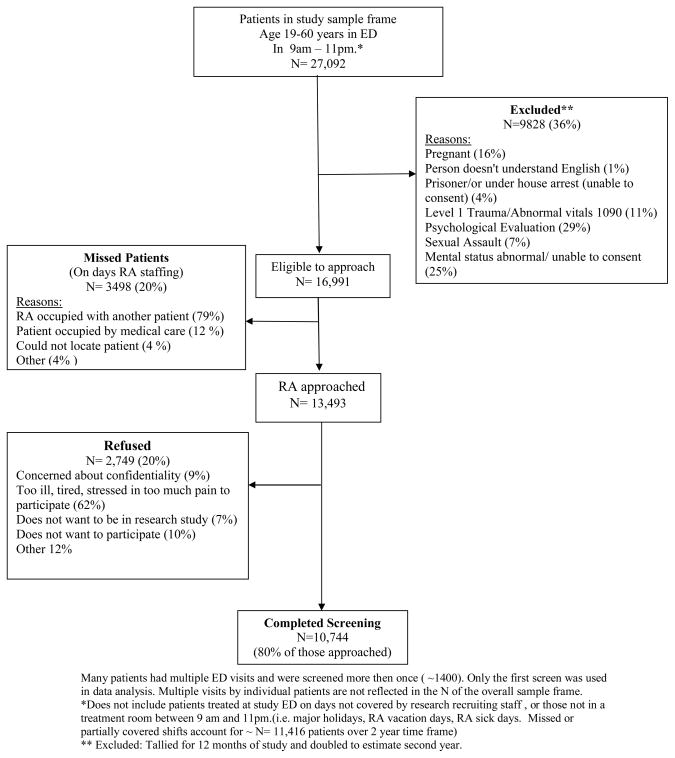
During a two-year period of recruitment, 13,493 patients were approached, 80% (n=10,744) consented to participate in screening; 20% (n=2,749) declined. Figure 1 illustrates patient flow. Among those who declined, 46% were male and 55% were African American.
Figure 1. Recruitment Flow.
Many patients had multiple ED visits and were screened more then once (~1400). Only the first screen was used in data analysis. Multiple visits by individual patients are not reflected in the N of the overall sample frame.
*Does not include patients treated at study ED on days not covered by research recruiting staff , or those not in a treatment room between 9 am and 11pm.(i.e. major holidays, RA vacation days, RA sick days. Missed or partially covered shifts account for ~ N= 11,416 patients over 2 year time frame)
** Excluded: Tallied for 12 months of study and doubled to estimate second year.
Characteristics of Study Participants
On average, the study participants were relatively young (mean age=36.4 years, SD=11.5), female (56%), and 56% African-American (40% Caucasian, 3% other races). Typical of the study city, only 2% of sample was Hispanic/Latino. The proportion of subjects who declined participation did not differ by sex or race. Just over a quarter (27%) presented to the ED for an acute injury. Sixteen percent of the total sample met DSM-IV criteria for either abuse or dependence on alcohol or illicit drugs.
Main Results
Prevalence of NPV
Overall 14% (n=1475) of patients surveyed seeking ED evaluation reported violence with a non-partner in the past year (Table 1). Among participants reporting NPV, 42% (n=618) experienced both victimization and aggression, 21% (n=315) reported only aggression and 37% (n=542) reported only victimization. The majority of those reporting NPV were men; however, more than 1/3 of those (38%) experiencing NPV were women. In addition, men accounted for 64% (738/1160) of the NPV victimization reported and 65% (609/933) of the NPV aggression.
Table 1.
Past Year Non-Partner Violence
| Female N=6027 (%) | Male N=4717 (%) | Total N=10,744(%) | |
|---|---|---|---|
| Victimization | |||
| “Have you been hit, kicked, punched, or otherwise hurt” | 422 (7) | 738 (16) | 1160 (11) |
| Aggression | |||
| “Have you hit, kicked, punched, or otherwise hurt” | 324 (5) | 609 (13) | 933 (9) |
| Any Non-Partner Violence | 557(9) | 918 19) | 1475 (14) |
Non-Partner Violence is defined as violence among friends, strangers, neighbors, people in bars, co-workers etc; does not include violence against a partner or spouse. Percentages used in the table are column percentages.
NPV Aggression & Victimization
Results of parallel bivariate analyses of participants, who engaged in NPV aggression compared to no NPV, and NPV victimization compared to no NPV, were similar (Appendix D). Therefore, further analysis presented here focus on any NPV (collapsed victimization and aggression).
Description of Participants with NPV and no NPV
Characteristics of patients with and without NPV are presented in table 2. Participants with past year NPV presented more often to the ED for an injury than a medical complaint; among participants presenting for injury, 21% (n=622/2936) reported past year NPV. Twenty percent of participants with past 30 day any prescription drug use note NPV (17 % of those with NPV report prescription opiate use, 7 % of those with NPV report prescription sedative use). Twenty five percent (n=365) of those with NPV noted they “got into physical fights while using alcohol or drugs” within the past year as compared to 2% (n=206) of those without NPV.
Table 2.
Bivariate Comparisons of Any Non-Partner Violence Based on Demographics, Health Status, and Substance Use (N=10,744).
| Variables | Any Non-Partner Violence (n=1475) | No Violence (n=9269) | ||
|---|---|---|---|---|
| Demographics | Mean | (±}SD) | Mean | (±}SD) |
| Age | 31.53 | (10.5) | 37.11 | (11.5) |
| n | (%) | n | (%) | |
| Male | 918 | (62.2) | 3799 | (41.0) |
| African Americana | 734 | (49.8) | 5237 | (56.5) |
| Married or Living Together | 337 | (22.9) | 3109 | (33.5) |
| Some College or College Grad | 469 | (31.8) | 3495 | (37.7) |
| Health Insurance (yes)a | 1029 | (69.9) | 7286 | (78.7) |
| Annual Income < $20,000a | 803 | (74.4) | 4090 | (64.2) |
| Employeda | 630 | (42.8) | 4348 | (46.9) |
|
Reason for Current ED Visit | ||||
| Injury | 622 | (42.2) | 2314 | (25.0) |
|
SF-12 Health Status | ||||
| Physical Health (≤ 25th Percentile) | 352 | (23.9) | 2334 | (25.2) |
| Mental Health (≤ 25th Percentile) | 518 | (35.1) | 2168 | (23.4) |
|
Substance Use in the Past 30 Days* | ||||
| Alcohol Only | 472 | (32.0) | 2732 | (29.5) |
| Marijuana (+/− alcohol) | 473 | (32.1) | 1510 | (16.3) |
| Cocaine (+/− alcohol or marijuana) | 126 | (8.5) | 325 | (3.5) |
| Other illicit drugs * | 32 | (2.2) | 49 | (0.5) |
| Prescription drug use** | 299 | (20.3) | 1252 | (13.5) |
|
Substance Abuse and/or Dependence | ||||
| Alcohol | 514 | (34.9) | 845 | (9.1) |
| Cocaine | 137 | (9.3) | 280 | (3.0) |
| Marijuana | 200 | (13.6) | 412 | (4.4) |
|
Substance Use Treatment | ||||
| In Past 3 Months | 129 | (8.8) | 321 | (3.5) |
Percentages used in the table are column percentages
Some subjects did not respond or skipped this question
Reference category = ’No Substance Use’
Other illicit drugs ( ie club drugs, inhalants, methamphetamine, heroin or hallucinogens)
Prescription drug use:opiates ie morphine, codeine, vicodin, Darvon, OxyContin, Darvocet, Percodan, Fentanyl, Sedative Depressants ie Xanax, Librium, Valium, Quaaludes, Halcion, sleeping pills, nerve pills downers barbiturates etc)
Logistic Regression Analysis Predicting NPV
Logistic regression models predicting involvement in past year NPV were conducted with all variables entered simultaneously. The model was significant (χ2 (15) = 1143.82, p<.0001) (Table 3). Participants who experienced past year NPV had twice the odds of being male or seeking ED care for an injury. They were younger, less likely to be African American, living with a partner or employed, and had an increased association with poor physical and mental health. Regarding substance use, any use of cocaine increased the odds of NPV by 3 times (2.41, 3.98) with NPV. In addition to that, alcohol, marijuana and prescription drug users were also more likely to increase the odds of NPV. Having substance use treatment in the past 3 months was associated with (OR 1.7) with NPV.
Table 3.
Logistic Regression Analysis Predicting Any Non-Partner Violence.
| Any Non-Partner Violence* |
|||
|---|---|---|---|
| OR | 95% CI | ||
|
Demographics | |||
| Age | 0.95 | 0.95 | 0.96 |
| Male | 2.20 | 1.94 | 2.50 |
| African American | 0.80 | 0.71 | 0.91 |
| Married or Living Together | 0.64 | 0.55 | 0.73 |
| Some College or College Grad | 1.07 | 0.94 | 1.22 |
| Health Insurance ( yes) | 0.97 | 0.84 | 1.11 |
| Employed | 0.84 | 0.74 | 0.95 |
|
Chief Complaint | |||
| Injury | 1.94 | 1.71 | 2.19 |
|
Mental Health | |||
| Physical Health (≤ 25th Percentile) | 1.32 | 1.14 | 1.54 |
| Mental Health (≤ 25th Percentile) | 1.90 | 1.67 | 2.17 |
|
Substance Use in the Past 30 Days | |||
| Alcohol Only ** | 1.73 | 1.49 | 2.01 |
| Marijuana (+/− alcohol) ** | 2.36 | 2.02 | 2.76 |
| Cocaine (+/− alcohol or marijuana) ** | 3.10 | 2.41 | 3.98 |
| Prescription drug use | 1.43 | 1.22 | 1.68 |
|
Substance Use Treatment | |||
| In Past 3 Months | 1.70 | 1.34 | 2.15 |
Age is a continuous variable
Reference category = No Non- Partner Violence
Reference category = No Substance Use
Prescription drug use:opiates morphine, codeine, vicodin, Demerol, Darvon, OxyContin, Darvocet, Tylenol 2,3,4, Stadol, Percodan, Fentanyl,Sedative Depressants, , Xanax, Librium, Valium, Quaaludes, Halcion, sleeping pills, nerve pills downers barbiturates etc)
Model = (χ2 (15) = 1143.82, p < .0001).
Parallel regressions analyses predicting non-partner victimization and aggression separately were also performed. The pattern of results was consistent across victimization and aggression; all models were significant and the findings for victimization and aggression did not differ from the findings of overall NPV (see appendix D).
Limitations
Although this study presents important information on the prevalence of NPV in an ED sample, there are several limitations that need to be addressed. First, given the cross-sectional design of this study and the mixed time frames assessed by various instruments, it is impossible to infer causality or temporal relationships of the associations found between NPV and associated correlates. Second, findings from this inner-city ED may not be generalizable to EDs outside of this setting, especially those in areas that substantially differ from where this study occurred (e.g., rural settings), and implication for screening and intervention may not apply in those settings. Third, the shortened version of the PVS requires validation and may be less sensitive then the full PVS. This brief measure, along with the exclusion of pregnant patients, those presenting with psychiatric chief complaints, and those presenting overnight, may potentially underestimate the frequency of NPV in the sample. Fourth, the analysis does not include an interaction term to address the possible interaction of substance use and mental health, which may lead to biased estimates. Fifth, data is self reported; however, recent reviews have concluded that reliability and validity of self-reported alcohol, tobacco, and other drug use is high,49–53 and patients are more likely to report drug use using computerized surveys and when privacy/confidentiality is assured.54–56 Fifth, although assessment of NPV was conducted using brief, self-administrated questions which maximize feasibility in a study of over 10,000 ED patients, replication of these findings with longer, more detailed instruments (e.g., Revised Conflict Tactics Scale II;57 Timeline Aggression module29) and multiple study sites is needed.
Discussion
This study represents one of the first to examine past year assault among a large consecutive cohort of medical and injured ED patients. This data suggest that a significant proportion of patients presenting to an inner-city ED have been involved in violence with a non-partner in the past year: 14% of all patients sampled and 21% of injured patients sampled. The prevalence of NPV found in this sample is higher than NPV prevalence found in community samples (e.g., 5.6%)58 and is equal to or higher than studies assessing past year IPV in the ED setting,59, 60
This data suggests that more patients who are experiencing NPV (42%) are experiencing both non-partner victimization and aggression than either type of non-partner violence alone (e.g., episodes of being the aggressor and being the victim). Of note, however, is that the context in which the aggressive behaviors occurred was not assessed; it is not clear whether the aggression and victimization occurred with the same person, as part of the same conflict, or with different people. Further, there is no way to ascertain if the participant was acting in self-defense. Despite this, the correlates of victimization and aggression of violence are very similar, supporting the concept of the cycle of violence or bi-directionality (for review see Straus, 200761 or Daday et al. 200821).
Although men reported higher rates of NPV than women, many women also reported violence (victimization and aggression) in non-partner relationships. Prior work suggests that patients who are experiencing NPV may also be experiencing violence in their intimate relationships.23, 62 The elevated prevalence of NPV found in this study suggest that the ED may be an ideal venue in which to identify and intervene with NPV, as is done routinely for IPV. For example, identification and intervention with men experiencing NPV may be protective in their current or future relationships, and advance intimate partner violence prevention efforts as well as decrease the individual’s future injury-related morbidity.
Although some research suggests that correlates of violence are similar for partner and non-partner violence (e.g., age, alcohol/drug problems, overall mental health),63 others note subtle differences in violence depending on relationship type, gender, and psychiatric status.62, 64 For example, prior research in substance use treatment settings and ED samples find that men report greater NPV than women.16, 31, 39 As noted by Graham and Wells (2003),65 male violence may be seen as more normative and acceptable than female violence in certain social settings (e.g., bars) and may also be related to concepts such as “face saving” and not wanting to “back down” from a violent confrontation, particularly when in the presence of others.
Although the temporal association of violence and the substance use reported in this study is not known, substance use and violence often co- occur in individuals, and often neither the violence nor the substance use are isolated events. Criminal justice data note that 5% of assailants were reportedly under the influence of drugs at the time of their crime.66 Findings indicated that a quarter of the participants noted that they have experienced fighting (relationship type not specified; non- partner, or partner) while using alcohol or drugs. These findings are in keeping with clinical and laboratory studies, which have generally found a relationship between physical aggression, alcohol, and cocaine.29, 33, 67, 68
More specifically, studies have demonstrated that alcohol and cocaine use are related to the frequency with which aggression occurs and the severity of the injuries sustained.69–73 There is evidence to suggest that the acute pharmacological effects of cocaine may increase aggressiveness.67 Non-ED studies have found evidence for acute cocaine consumption and aggression.29, 74 Marijuana use is also related to both aggression and victimization (for a review see Hoaken et al., 200375); this association is likely due to contextual factors and self-selection/self-medication, as well as to marijuana withdrawal.76
Theories focusing on the relationship between alcohol and other drug use and violence highlight the role of a variety of risk domains, including acute intoxication effects, social/contextual factors (relationship type, partner/non-partner), and other individual difference factors (gender, depression).33, 77 In general, substance users (particularly cocaine users) are frequent victims of violence71, 78 and are at increased risk for injuries sustained while under the influence. The relationship of substance use and violence are unlikely to be solely explained by the pharmacology of the drug. The exacerbated rates of violence experienced by substance users are likely not solely related to the timing of intoxication, but rather to clustering of high risk behaviors in the individual. For example, obtaining and/or using illegal substances involve a social/environmental context with people and places where NPV is likely to occur. Baskin-Sommers (2006)79 have suggested that aggression may be partially explained by the tendency of drug users to become more exposed to and desensitized by violence due to interacting with individuals already immersed in a violent drug culture. Thus, there may be greater opportunities for users of illicit substances to be experience violence, regardless of whether they were intoxicated at the time of the occurrence of violence. These assertions require validation with studies using calendar approaches to tease out the influences of acute consumption and NPV.29, 74
To the best of our knowledge, this is the first ED study to disentangle cocaine and marijuana use in relation to NPV, as opposed to being combined into one “illicit drug” category, as well as to show an association of NPV (in both victimization and aggression) and use of prescription drugs. Future studies evaluating any prescription drug use the role of prescription drug misuse (and specifically opiate dependence), and the relationship of prescription use to other illicit drugs and NPV are needed to further evaluate this association.
The regression analysis shows that, accounting for other variables in the model, there is a pattern of increasing association of violence from any prescription drug use, to alcohol only, to marijuana, to cocaine users. The association of cocaine use in particular to both NPV aggression and victimization is highlighted in this data. Although this relationship may not be surprising, it highlights the need to address drug use in general, and cocaine use specifically among patients presenting with violence.
Finally, patients reporting NPV in this sample also report poor mental health, which was a strong marker of NPV, even when other demographic and substance use variables were considered. Studies of participants with substance use disorders found that for both men and women, psychiatric distress was associated with aggression and victimization with both partners and non-partners, although findings are stronger for women than men.16, 28, 31, 79–81
In comparison to intimate partner violence, recent NPV (victimization and aggression) among adults has been relatively unaddressed among ED populations outside of those presenting for acute assault-related injury. However, NPV has been studied in other health care settings such as primary care82 and walk-in clinics69 found rates of NPV victimization to be high (45%of young adult males and 48% overall respectively). One prior retrospective ED study of female-to-female violence amongst women83 found that approximately 9% of women presenting to the ED for any reason had been victimized, and of these women, only 5% identified their assailant as being an intimate partner. This study finds also that a surprisingly high number of women seeking ED care have recently been involved in NPV.
Identifying and intervening with patients who have experienced recent NPV and are therefore at increased risk of future violence and injury has significant public health implications. Although there is a paucity of data on effective treatment interventions targeting violence in ED samples, there is evidence to support that addressing substance use is related to reductions in violence, even if the reported substance use and violence were not temporally related initially. For example, studies have found that patients who decrease their substance use (following treatment engagement) experience substantial reductions in violence over time.28, 48, 84, 85 Interventions based on cognitive and behavioral strategies can impact both substance use and violence.86–89 Therefore identifying individuals who report recent substance use and recent violence in the ED may offer an opportunity for intervention.
EDs often serve primary care functions; in this capacity, the ED may be a setting for interventions to interrupt the cycle of violence among patients treated routinely for fistfights, bar fights, and neighborhood disagreements. ED-based substance use interventions may be beneficial in preventing future injury,90 and other more intensive case management interventions have been shown to decrease criminal justice outcomes and violence involvement among admitted trauma inpatients.91 Findings from the regression analysis highlight the impact of substance use beyond that of traditional demographic risk factors (age, gender, employment status). Future studies are needed to evaluate the impact of substance use treatment on patient experiences with violence and associated injury mortality and morbidity.
In Retrospect
Although this study identifies broad domains of possible prevention strategies, data that elucidates treatment readiness should be assessed in future studies. In addition, future studies should evaluate the characteristics and type of injury and injury severity in relation to NPV.
Conclusions
Findings from this large, consecutive cohort of ED patients over 2 full calendar years demonstrates that a substantial number patients (14%) seeking care in an inner-city ED experience violence with a non-partner. Associated risk factors did not differ by victimization or aggression, and cocaine use was the strongest predictor of NPV.
Supplementary Material
Acknowledgments
Role of Funding Source: This work was supported by grants from the National Institute on Alcohol Abuse and Alcoholism, NIAAA (#AA014665) and the National Institute on Drug Abuse, NIDA (#DA 016591).
We would like to thank the medical staff and patients at Hurley Medical Center for their support of this research, and Pat Bergeron for her assistance with manuscript preparation.
Footnotes
Conflict of Interest: All authors declare that they have no conflicts of interest.
Contributors: Drs. Cunningham, Murray, and Walton wrote the initial draft of the manuscript. Drs. Blow, Booth, Walton, and Chermack conceptualized the study and are investigators on the grant funding this work. Dr. Wojnar assisted in editing the manuscript. All authors contributed to and have approved the final manuscript.
References
- 1.Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 emergency department summary. Adv Data. 2007 Jun 29;386:1–32. [PubMed] [Google Scholar]
- 2.Gallagher CA. Injury recurrence among untreated and medically treated victims of violence in the USA. Soc Sci Med. 2005 Feb;60(3):627–635. doi: 10.1016/j.socscimed.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Cherpitel CJ. Alcohol and violence-related injuries: an emergency room study. Addiction. 1993 Jan;88(1):79–88. doi: 10.1111/j.1360-0443.1993.tb02765.x. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department. of Health and Human Services PHS. Healthy People 2000: National promotion and disease prevention objectives. Washington, DC: U.S. Department of Health and Human Services - DHHS; 1991. (PHS) 91–50212. [Google Scholar]
- 5.Centers for Disease Control and Prevention, National Center for Injury Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) Centers for Disease Control and Prevention; 2006. [Accessed April 23, 2008]. [[online]] [cited 2006 Feb 8]. Available at www.cdc.gov/ncipc/wisqars. [Google Scholar]
- 6.Fingerhut LA, Kleinman JC. International and interstate comparisons of homicide among young males. JAMA. 1990;26:3292–3295. [PubMed] [Google Scholar]
- 7.Kellermann AL, Rivara FP, Rushforth NB, et al. Gun ownership as a risk factor for homicide in the home. N Engl J Med. 1993 Oct 7;329(15):1084–1091. doi: 10.1056/NEJM199310073291506. [DOI] [PubMed] [Google Scholar]
- 8.Bureau of Justice Statistics OoJP. Crime and Victim Statistics 2005. Washington, DC: Bureau of Justice Statistics; 2005. [Google Scholar]
- 9.Federal Bureau of Investigation. National Incident-Based Reporting System, 2000. National Archive of Criminal Justice Data, U.S. Department of Justice, Federal Bureau of Investigation; 2002. [Google Scholar]
- 10.Grisso JA, Schwarz DF, Hirschinger N, et al. Violent injuries among women in an urban area. NEJM. 1999 Dec 16;341(25):1899–1905. doi: 10.1056/NEJM199912163412506. [DOI] [PubMed] [Google Scholar]
- 11.Elliott DS. Serious violent offenders: Onset, developmental course and termination. Criminology. 1994;32:1–21. [Google Scholar]
- 12.White HR, Loeber R, Stouthamer-Loeber M, et al. Developmental associations between substance use and violence. Dev Psychopathol. 1999 Fall;11(4):785–803. doi: 10.1017/s0954579499002321. [DOI] [PubMed] [Google Scholar]
- 13.Weiczorek WF, Welte JW, Abel EI. Alcohol, drugs, and murder: A study of convicted homicide offenders. Journal of Criminal Justice. 1990;18(3):217–227. [Google Scholar]
- 14.Welte JW, Miller BA. Alcohol use by violent and property offenders. Drug and alcohol dependence. 1987;19(4):313–324. doi: 10.1016/0376-8716(87)90018-4. [DOI] [PubMed] [Google Scholar]
- 15.Cunningham R, Walton MA, Tripathi SP, et al. Past-year violence typologies among patients with cocaine-related chest pain. Am J Drug Alcohol Abuse. 2007;33(4):571–582. doi: 10.1080/00952990701407512. [DOI] [PubMed] [Google Scholar]
- 16.Chermack ST, Walton MA, Fuller BE, et al. Correlates of expressed and received violence across relationship types among men and women substance abusers. Psychol Addict Behav. 2001 Jun;15(2):140–151. doi: 10.1037//0893-164x.15.2.140. [DOI] [PubMed] [Google Scholar]
- 17.Brown RA, Monti PM, Myers MG, et al. Depression among cocaine abusers in treatment: relation to cocaine and alcohol use and treatment outcome. The American journal of psychiatry. 1998 Feb;155(2):220–225. doi: 10.1176/ajp.155.2.220. [DOI] [PubMed] [Google Scholar]
- 18.Fals-Stewart W, Kashdan TB, O'Farrell TJ, et al. Behavioral couples therapy for drug-abusing patients: effects on partner violence. Journal of substance abuse treatment. 2002 Mar;22(2):87–96. doi: 10.1016/s0740-5472(01)00218-5. [DOI] [PubMed] [Google Scholar]
- 19.Moore TM, Stuart GL. Illicit substance use and intimate partner violence among men in batterers' intervention. Psychol Addict Behav. 2004 Dec;18(4):385–389. doi: 10.1037/0893-164X.18.4.385. [DOI] [PubMed] [Google Scholar]
- 20.Sims DW, Bivins BA, Obeid FN, et al. Urban trauma: a chronic recurrent disease. J Trauma. 1989;29(7):940–946. [PubMed] [Google Scholar]
- 21.Daday JK, Broidy LM, Crandall CS. Emergency department utilization among victims and offenders involved in non-lethal violence. Soc Sci Med. 2008 Mar;66(5):1197–1203. doi: 10.1016/j.socscimed.2007.11.017. [DOI] [PubMed] [Google Scholar]
- 22.Rivara FP, Shepherd JP, Farrington DP, et al. Drug use in trauma victims. Ann Emerg Med. 1995 Nov;26(5):609–614. doi: 10.1016/s0196-0644(95)70013-7. [DOI] [PubMed] [Google Scholar]
- 23.Chermack ST, Murray R, Winters JJ, et al. Treatment needs of men and women with violence problems in substance use disorder treatment. Substance Use and Misuse. doi: 10.1080/10826080902960007. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stalans LJ, Seng M. Identifying subgroups at high risk of dropping out of domestic batterer treatment: the buffering effects of a high school education. Int J Offender Ther Comp Criminol. 2007 Apr;51(2):151–169. doi: 10.1177/0306624X06290204. [DOI] [PubMed] [Google Scholar]
- 25.Fonseca CA, Schmaling KB, Stoever C, et al. Variables associated with intimate partner violence in a deploying military sample. Military medicine. 2006 Jul;171(7):627–631. doi: 10.7205/milmed.171.7.627. [DOI] [PubMed] [Google Scholar]
- 26.Murray RL, Chermack ST, Walton MA, et al. Psychological aggression, physical aggression, and injury in nonpartner relationships among men and women in treatment for substance-use disorders. Journal of studies on alcohol and drugs. 2008 Oct;69(6):896–905. doi: 10.15288/jsad.2008.69.896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magdol L, Moffitt TE, Caspi A, et al. Gender differences in partner violence in a birth cohort of 21-year-olds: bridging the gap between clinical and epidemiological approaches. Journal of consulting and clinical psychology. 1997 Feb;65(1):68–78. doi: 10.1037//0022-006x.65.1.68. [DOI] [PubMed] [Google Scholar]
- 28.Walton MA, Chermack ST, Blow FC. Correlates of received and expressed violence persistence following substance abuse treatment. Drug and alcohol dependence. 2002 Jun 1;67(1):1–12. doi: 10.1016/s0376-8716(02)00016-9. [DOI] [PubMed] [Google Scholar]
- 29.Chermack ST, Blow FC. Violence among individuals in substance abuse treatment: the role of alcohol and cocaine consumption. Drug and alcohol dependence. 2002 Mar 1;66(1):29–37. doi: 10.1016/s0376-8716(01)00180-6. [DOI] [PubMed] [Google Scholar]
- 30.Breiding MJ, Black MC, Ryan GW. Chronic disease and health risk behaviors associated with intimate partner violence-18 U.S. states/territories, 2005. Annals of epidemiology. 2008 Jul;18(7):538–544. doi: 10.1016/j.annepidem.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 31.Walton MA, Cunningham RM, Chermack ST, et al. Correlates of violence history among injured patients in an urban emergency department: gender, substance use, and depression. J Addict Dis. 2007;26(3):61–75. doi: 10.1300/J069v26n03_07. [DOI] [PubMed] [Google Scholar]
- 32.Boles SM, Miotto K. Substance abuse and violence: A review of the literature. Aggression and Violent Behavior. 2003;8(2):155–174. [Google Scholar]
- 33.Chermack ST, Giancola PR. The relation between alcohol and aggression: an integrated biopsychosocial conceptualization. Clin Psychol Rev. 1997;17(6):621–649. doi: 10.1016/s0272-7358(97)00038-x. [DOI] [PubMed] [Google Scholar]
- 34.Federal Bureau of Investigation. Crime in the United States 2006: Uniform Crime Report 2006. U.S. Department of Justice; Available at: http://www.fbi.gov/ucr/cius2006/index.html. [Google Scholar]
- 35.Michigan Department of Community Health. Census 2000. 2002 Oct 31; Available at: http://www.mdch.state.mi.us/pha/osr/CHI/POP/Fcensus2.ASP, 10/31/2002.
- 36.Chermack ST, Wyrobeck JM, Walton MA, et al. Distal and Proximal Factors Related to Aggression Severity among Patients in Substance Abuse Treatment: Family History, Alcohol Use and Expectancies. Addictive behaviors. 2006 May;31(5):845–858. doi: 10.1016/j.addbeh.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 37.Cogan R, Ballinger BC., 3rd Alcohol problems and the differentiation of partner, stranger, and general violence. J Interpers Violence. 2006 Jul;21(7):924–935. doi: 10.1177/0886260506289177. [DOI] [PubMed] [Google Scholar]
- 38.Cunradi C, Ames G, Moore R. Prevalence and correlates of interpersonal violence victimization in a junior enlisted Navy cohort. Violence Vict. 2005 Dec;20(6):679–694. [PubMed] [Google Scholar]
- 39.Cunningham R, Walton MA, Maio RF, et al. Violence and substance use among an injured emergency department population. Acad Emerg Med. 2003 Jul;10(7):764–775. doi: 10.1111/j.1553-2712.2003.tb00071.x. [DOI] [PubMed] [Google Scholar]
- 40.Smith GR, Ross RL, Rost KM. Psychiatric outcomes module: substance Abuse Outcomes Module (SOAM) In: Sederer LI, Dickey B, editors. Outcomes assessment in clinical practice. Baltimore, MD: Williams & Wilkins; 1996. pp. 85–88. [Google Scholar]
- 41.Feldhaus KM, Koziol-McLain J, Amsbury HL, et al. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. Jama. 1997 May 7;277(17):1357–1361. [PubMed] [Google Scholar]
- 42.Morrison LJ, Allan R, Grunfeld A. Improving the emergency department detection rate of domestic violence using direct questioning. J Emerg Med. 2000 Aug;19(2):117–124. doi: 10.1016/s0736-4679(00)00204-3. [DOI] [PubMed] [Google Scholar]
- 43.Alter HJ, Braun R, Zazzali JL. Health status disparities among public and private emergency department patients. Acad Emerg Med. 1999 Jul;6(7):736–743. doi: 10.1111/j.1553-2712.1999.tb00445.x. [DOI] [PubMed] [Google Scholar]
- 44.Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2. Boston, MA: The Health Institute, New England Medical Center; 1995. [Google Scholar]
- 45.Fleming M, Barry K, Manwell L, et al. A trial of early alcohol treatment (Project TrEAT): A randomized trial of brief physician advice in community-based primary care practices. Journal of the American Medical Association. 1997;277:1039–1045. [PubMed] [Google Scholar]
- 46.Haywood KL, Garratt AM, Fitzpatrick R. Quality of life in older people: a structured review of generic self-assessed health instruments. Qual Life Res. 2005 Sep;14(7):1651–1668. doi: 10.1007/s11136-005-1743-0. [DOI] [PubMed] [Google Scholar]
- 47.Smith GR, Burnam MA, Mosley CL, et al. Reliability and validity of the substance abuse outcomes module. Psychiatr Serv. 2006 Oct;57(10):1452–1460. doi: 10.1176/ps.2006.57.10.1452. [DOI] [PubMed] [Google Scholar]
- 48.Chermack ST, Murray RL, Walton MA, et al. Partner aggression among men and women in substance use disorder treatment: correlates of psychological and physical aggression and injury. Drug and alcohol dependence. 2008 Nov 1;98(1–2):35–44. doi: 10.1016/j.drugalcdep.2008.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gray TA, Wish ED. Substance Abuse Need for Treatment among Arrestees (SANTA) in Maryland. College Park, MD: Center for Substance Abuse Research; 1998. [Google Scholar]
- 50.Thornberry TP, Krohn MD. The self-report method of measuring delinquency and crime. In: Duffee D, editor. Measurement and Analysis of Crime and Justice: Criminal Justice 2000. Washington, DC: US Department of Justice, Office of Justice Programs; 2000. pp. 33–83. [Google Scholar]
- 51.Buchan BJ, MLD, Tims FM, et al. Cannabis use: consistency and validity of self-report, on-site urine testing and laboratory testing. Addiction. 2002 Dec;97 (Suppl 1):98–108. doi: 10.1046/j.1360-0443.97.s01.1.x. [DOI] [PubMed] [Google Scholar]
- 52.Dennis M, Titus JC, Diamond G, et al. The Cannabis Youth Treatment (CYT) experiment: rationale, study design and analysis plans. Addiction. 2002 Dec;97 (Suppl 1):16–34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- 53.Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health. 2003 Dec;33(6):436–457. doi: 10.1016/s1054-139x(03)00052-1. [DOI] [PubMed] [Google Scholar]
- 54.Darke S. Self-report among injecting drug users: a review. Drug and alcohol dependence. 1998 Aug 1;51(3):253–263. doi: 10.1016/s0376-8716(98)00028-3. discussion 267–258. [DOI] [PubMed] [Google Scholar]
- 55.O'Farrell TJ, Fals-Stewart W, Murphy M. Concurrent validity of a brief self-report Drug Use Frequency measure. Addictive behaviors. 2003 Mar;28(2):327–337. doi: 10.1016/s0306-4603(01)00226-x. [DOI] [PubMed] [Google Scholar]
- 56.Chermack ST, Singer K, Beresford TP. Screening for alcoholism among medical inpatients: how important is corroboration of patient self-report? Alcoholism, clinical and experimental research. 1998 Oct;22(7):1393–1398. doi: 10.1111/j.1530-0277.1998.tb03925.x. [DOI] [PubMed] [Google Scholar]
- 57.Straus MA, Hamby SL, Boney-McCoy S, et al. The Revised Conflict Tactics Scales (CTS2) J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 58.Forjuoh SN, Kinnane JM, Coben JH, et al. Victimization from physical violence in Pennsylvania: prevalence and health care use. Acad Emerg Med. 1997 Nov;4(11):1052– 1058. doi: 10.1111/j.1553-2712.1997.tb03679.x. [DOI] [PubMed] [Google Scholar]
- 59.Dearwater SR, Coben JH, Campbell JC, et al. Prevalence of intimate partner abuse in women treated at community hospital emergency departments. Jama. 1998 Aug 5;280(5):433–438. doi: 10.1001/jama.280.5.433. [DOI] [PubMed] [Google Scholar]
- 60.McCloskey LA, Lichter E, Ganz ML, et al. Intimate partner violence and patient screening across medical specialties. Acad Emerg Med. 2005 Aug;12(8):712–722. doi: 10.1197/j.aem.2005.03.529. [DOI] [PubMed] [Google Scholar]
- 61.Straus MA. Conflict Tactics Scales. In: Jackson NA, editor. Encyclopedia of Domestic Violence. New York, Routledge: Taylor & Francis Group; 2007. p. 824. [Google Scholar]
- 62.Chermack ST, Fuller BE, Blow FC. Predictors of perpetrator of partner violence and non-partner violence among patients in substance abuse treatment. Drug and alcohol dependence. 2000;58(1–2):43–54. doi: 10.1016/s0376-8716(99)00067-8. [DOI] [PubMed] [Google Scholar]
- 63.Fagan JA, Browne A. Violence between partners and intimates. In: Reiss A, Roth J, editors. Understanding and preventing violence: Vol. 3. Social Influences. Vol. 3. Washington, DC: National Academy Press; 1994. pp. 115–292. [Google Scholar]
- 64.Chermack ST, Walton MA. The relationship between family aggression history and expressed aggression among college males. Aggressive Behav. 1999;25:255–267. [Google Scholar]
- 65.Wells S, Graham K. Aggression involving alcohol: relationship to drinking patterns and social context. Addiction. 2003 Jan;98(1):33–42. doi: 10.1046/j.1360-0443.2003.00253.x. [DOI] [PubMed] [Google Scholar]
- 66.Isner JM, Estes NA, 3rd, Thompson PD, et al. Acute cardiac events temporally related to cocaine abuse. N Engl J Med. 1986 Dec 4;315(23):1438–1443. doi: 10.1056/NEJM198612043152302. [DOI] [PubMed] [Google Scholar]
- 67.Licata A, Taylor S, Berman M, et al. Effects of cocaine on human aggression. Pharmacol Biochem Behav. 1993;45(3):549–552. doi: 10.1016/0091-3057(93)90504-m. [DOI] [PubMed] [Google Scholar]
- 68.Macdonald S, Anglin-Bodrug K, Mann RE, et al. Injury risk associated with cannabis and cocaine use. Drug and alcohol dependence. 2003 Nov 24;72(2):99–115. doi: 10.1016/s0376-8716(03)00202-3. [DOI] [PubMed] [Google Scholar]
- 69.Conway T, Hu TC, Kim P, et al. Prevalence of violence victimization among patients seen in an urban public hospital walk-in clinic. J Gen Intern Med. 1994 Aug;9(8):430–435. doi: 10.1007/BF02599057. [DOI] [PubMed] [Google Scholar]
- 70.Eronen M, Hakola P, Tiihonen J. Factors associated with homicide recidivism in a 13-year sample of homicide offenders in Finland. Psychiatr Serv. 1996 Apr;47(4):403–406. doi: 10.1176/ps.47.4.403. [DOI] [PubMed] [Google Scholar]
- 71.Falck RS, Wang J, Carlson RG, et al. The epidemiology of physical attack and rape among crack-using women. Violence Vict. 2001 Feb;16(1):79–89. [PubMed] [Google Scholar]
- 72.Harrison LD. Trends in illicit drug use in the United States: conflicting results from national surveys. Int J Addict. 1992;27(7):817–847. doi: 10.3109/10826089209068769. [DOI] [PubMed] [Google Scholar]
- 73.Murdoch D, Pihl RO, Ross D. Alcohol and crimes of violence: present issues. Int J Addict. 1990 Sep;25(9):1065–1081. doi: 10.3109/10826089009058873. [DOI] [PubMed] [Google Scholar]
- 74.Fals-Stewart W. The occurrence of partner physical aggression on days of alcohol consumption: A longitudinal diary study. Journal of consulting and clinical psychology. 2003;71(1):42–52. doi: 10.1037//0022-006x.71.1.41. [DOI] [PubMed] [Google Scholar]
- 75.Hoaken PN, Stewart SH. Drugs of abuse and the elicitation of human aggressive behavior. Addictive behaviors. 2003 Dec;28(9):1533–1554. doi: 10.1016/j.addbeh.2003.08.033. [DOI] [PubMed] [Google Scholar]
- 76.Moore TM, Stuart GL. A review of the literature on marijuana and interpersonal violence. Aggression and Violent Behavior. 2005;10(2):171–192. [Google Scholar]
- 77.Goldstein PJ. The Drugs/Violence Nexus: A Tripartite Conceptual Framework. J Drug Issues. 1985;15:493–506. [Google Scholar]
- 78.Siegal HA, Falck RS, Wang J, et al. Crack-cocaine users as victims of physical attack. J Natl Med Assoc. 2000;92(2):76–82. [PMC free article] [PubMed] [Google Scholar]
- 79.Baskin-Sommers A, Sommers I. Methamphetamine use and violence among young adults. Journal of Criminal Justice. 2006;34(6):661–674. [Google Scholar]
- 80.Abbott J, Johnson R, Koziol-McLain J, et al. Domestic violence against women. Incidence and prevalence in an emergency department population. JAMA. 1995 Jun 14;273(22):1763–1767. doi: 10.1001/jama.273.22.1763. [DOI] [PubMed] [Google Scholar]
- 81.Thompson MP, Kaslow NJ, Kingree JB, et al. Partner violence, social support, and distress among inner-city African American women. Am J Community Psychol. 2000 Feb;28(1):127–143. doi: 10.1023/A:1005198514704. [DOI] [PubMed] [Google Scholar]
- 82.Rich JA, Sullivan LM. Correlates of violent assault among young male primary care patients. J Health Care Poor Underserved. 2001 Feb;12(1):103–112. doi: 10.1353/hpu.2010.0538. [DOI] [PubMed] [Google Scholar]
- 83.Mechem CC, Shofer FS, Reinhard SS, et al. Violence between women in an urban emergency department patient population. Acad Emerg Med. 2001 Jan;8(1):30–35. doi: 10.1111/j.1553-2712.2001.tb00544.x. [DOI] [PubMed] [Google Scholar]
- 84.O'Farrell TJ, Fals-Stewart W. Behavioral couples therapy for alcoholism and drug abuse. Journal of substance abuse treatment. 2000 Jan;18(1):51–54. doi: 10.1016/s0740-5472(99)00026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.O'Farrell TJ, Murphy CM. Marital violence before and after alcoholism treatment. J Cons Clin Psych. 1995;63(2):256–262. doi: 10.1037//0022-006x.63.2.256. [DOI] [PubMed] [Google Scholar]
- 86.Fava GA, Rafanelli C, Grandi S, et al. Prevention of recurrent depression with cognitive behavioral therapy: preliminary findings. Archives of general psychiatry. 1998 Sep;55(9):816–820. doi: 10.1001/archpsyc.55.9.816. [DOI] [PubMed] [Google Scholar]
- 87.Swartz MS, Swanson JW, Hiday VA, et al. Taking the wrong drugs: the role of substance abuse and medication noncompliance in violence among severely mentally ill individuals. Social psychiatry and psychiatric epidemiology. 1998a Dec;33 (Suppl 1):S75–80. doi: 10.1007/s001270050213. [DOI] [PubMed] [Google Scholar]
- 88.Swartz MS, Swanson JW, Hiday VA, et al. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. The American journal of psychiatry. 1998b Feb;155(2):226–231. doi: 10.1176/ajp.155.2.226. [DOI] [PubMed] [Google Scholar]
- 89.Swanson J, Estroff S, Swartz M, et al. Violence and severe mental disorder in clinical and community populations: the effects of psychotic symptoms, comorbidity, and lack of treatment. Psychiatry. 1997 Spring;60(1):1–22. doi: 10.1080/00332747.1997.11024781. [DOI] [PubMed] [Google Scholar]
- 90.Havard A, Shakeshaft A, Sanson-Fisher R. Systematic review and meta-analyses of strategies targeting alcohol problems in emergency departments: interventions reduce alcohol-related injuries. Addiction. 2008 Mar;103(3):368–376. doi: 10.1111/j.1360-0443.2007.02072.x. [DOI] [PubMed] [Google Scholar]
- 91.Cooper C, Eslinger DM, Stolley PD. Hospital-based violence intervention programs work. J Trauma. 2006 Sep;61(3):534–540. doi: 10.1097/01.ta.0000236576.81860.8c. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.