Abstract
Constancy of hepatic blood flow (HBF) is crucial for several homeostatic roles. The present conceptual review focuses on interrelated mechanisms that act to maintain a constant HBF per liver mass. The liver cannot directly control portal blood flow (PF); therefore, these mechanisms largely operate to compensate for PF changes. A reduction in PF leads to reduced intrahepatic distending pressure, resulting in the highly compliant hepatic vasculature passively expelling up to 50% of its blood volume, thus adding to venous return, cardiac output and HBF. Also activated immediately upon reduction of PF are the hepatic arterial buffer response and an HBF-dependent hepatorenal reflex. Adenosine is secreted at a constant rate into the small fluid space of Mall which surrounds the terminal branches of the hepatic arterioles, portal venules and sensory nerves. The concentration of adenosine is regulated by washout into the portal venules. Reduced PF reduces the washout and the accumulated adenosine causes dilation of the hepatic artery, thus buffering the PF change. Adenosine also activates hepatic sensory nerves to cause reflex renal fluid retention, thus increasing circulating blood volume and maintaining cardiac output and PF. If these mechanisms are not able to maintain total HBF, the hemodynamic imbalance results in hepatocyte proliferation, or apoptosis, by a shear stress/nitric oxide-dependent mechanism, to adjust total liver mass to match the blood supply. These mechanisms are specific to this unique vascular bed and provide an excellent example of multiple integrative regulation of a major homeostatic organ.
Keywords: adenosine, hepatic arterial buffer response, hepatic vascular bed, kidney, pharmacodynamics
INTRODUCTION
Constancy of hepatic blood flow is crucial for the homeostatic integration of nutrient and hormone fluxes and cardiovascular stability. The hepatic clearance of many drugs and hormones is blood flow dependent and a relatively constant rate of removal of hormones from the plasma is necessary to allow fine control of blood levels by the endocrine glands.
There are multiple interrelated mechanisms that act acutely and chronically to maintain a constant hepatic blood flow-to-liver mass ratio. Maintenance of hepatic blood flow is made more complex by the unique characteristics of the hepatic vascular bed. The liver receives approximately 25% of the entire cardiac output and three-quarters of that blood flow is provided to the liver through the portal venous drainage from the stomach, intestines, spleen, pancreas, and visceral fat. The liver is not capable of directly controlling portal blood flow. Yet, as will be discussed, the liver can have very significant indirect effects to regulate portal blood flow via mechanisms impacting on blood flow to the splanchnic organs that drain into the portal vein. The first mechanism is a simple physical consequence of the very high vascular capacitance (blood volume) and compliance (change in hepatic blood volume per unit change in intrahepatic pressure). A decrease in portal blood flow leads to a passive decrease in intrahepatic pressure and a passive expulsion of blood from the large hepatic reservoir into the central venous system. This increase in venous return leads to increased cardiac output which, in turn, leads to elevated blood flow in the splanchnic arteries that feed the portal venous bed, thus at least partially correcting the initial flow deficit.
At the same time, the reduced portal flow activates the hepatic arterial buffer response (HABR) secondary to reduced washout of adenosine from the space of Mall which surrounds the terminal branches of the portal vein and hepatic artery before they drain into the hepatic sinusoidal syncytium. Adenosine appears to be secreted at a constant rate into the space of Mall, with the local concentration of the potent vasodilator being regulated by the rate of washout into the portal blood. By this mechanism, reduced portal flow leads to accumulation of adenosine and hepatic arterial dilation, thereby serving to buffer the impact that changes in portal flow have on total hepatic blood flow. This is the mechanism of the HABR.
The accumulated adenosine also activates sensory nerves in the liver, which results in activation of a hepatorenal reflex. This reflex leads to reduced renal output and fluid retention, thereby elevating blood volume, venous return, cardiac output, and splanchnic blood flow. The elevated adenosine level that occurs in response to reduced portal flow leads to rapid responses. The hepatic artery is dilated within seconds and the response is well maintained. The hepatorenal reflex is also activated immediately but the renal fluid retention has cardiovascular consequences only after a much longer time scale, until fluid retention becomes significant.
Hepatocyte proliferation is also rapidly activated but is modulated over a longer period of time by a hemodynamic mechanism related to vascular shear stress. Hepatic vascular shear stress regulates nitric oxide and prostaglandin release to trigger a cascade leading to hepatocyte proliferation or apoptosis. By this mechanism, hepatic cell mass is adjusted to maintain a constant ratio to the mean chronic hepatic blood supply.
Nitric oxide and adenosine play distinct roles to inhibit vasoconstrictors: nitric oxide acts if constriction raises shear stress; adenosine acts if hepatic blood flow is reduced.
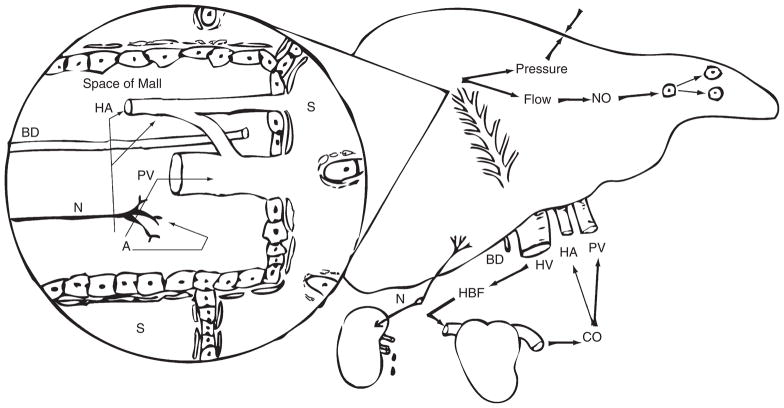
The focus in the present review will be on concepts. Detailed references are available in the original articles and reviews. Figure 1 presents a conceptual summary.
Figure 1.
The space of Mall is a minute fluid space surrounding the hepatic arterioles (HA), bile ductules (BD), portal venules (PV), and sensory nerves (N) receptive to adenosine. Adenosine (A) is secreted into the space of Mall and its concentration is regulated by the rate of washout from the space of Mall into the blood vessels. A reduction in blood flow leads to immediate increase in adenosine levels which acts on the HA causing vasodilation and inhibition of vasoconstrictors. Adenosine does not modulate the PV. Portal and arterial blood flow wash adenosine from the space of Mall thus controlling HA vascular tone and blood flow. Adenosine also acts on hepatic sensory nerves that serve to reflexly regulate renal fluid retention and therefore, indirectly, cardiac output (CO) and hepatic blood flow (HBF). Outside the space of Mall, a highly vascular and distensible liver responds to changes in intrahepatic distending blood pressure to regulate the large hepatic blood reservoir. The hepatic cells (probably endothelial) respond to blood flow that is sensed via shear stress. Vascular shear stress results in the release of nitric oxide (NO). NO dilates the resistance vessels in the HA and PV and blocks vasoconstrictors. NO causes vascular escape from vasoconstriction in the HA. NO also activates the machinery of hepatic proliferation serving as the trigger to adjust the functional cell mass of the liver. HV, hepatic vein; S, sinusoid.
HEPATIC COMPLIANCE
The liver is an exceptionally vascular organ. Although it constitutes only 2.5% of bodyweight, it receives about 25% of the cardiac output. The liver accounts for 12% of the total blood volume and half of that blood can be rapidly expelled from the liver in response to both active and passive influences, thus giving the liver a dramatic role as a blood volume reservoir.1
The determinants of the volume of blood in an organ are the distending transmural pressure, the compliance of the vessels, and the unstressed volume. Compliance is the extent to which the volume of the vessel changes in response to a change in transmural pressure. The concept of stressed and unstressed capacitance with specific reference to the role of the splanchnic circulation has previously been reviewed.2 Unstressed volume is a hypothetical volume of blood that would remain within the organ at a vascular pressure of zero. This measurement is obtainable only through extrapolation of pressure-volume curves through the zero pressure axis. All known active constrictors of hepatic blood volume do so through changes in the unstressed volume. Stressed volume is the volume of blood in the organ due to distension by the intravascular transmural pressure acting against the compliant vascular bed. The relationship between distending pressure and hepatic blood volume is linear over the physiological range of portal venous pressure.3 Portal venous pressure provides a good estimate of the intrahepatic distending pressure that acts upon the compliant hepatic vascular bed.
The impact of changes in portal flow on portal pressure are made more complex by the fact that the venous resistance sites within the liver are passively distensible, with the intrahepatic vascular resistance being related to 1/distending pressure cubed. Thus a large change in portal blood flow can be partially compensated for by what we have referred to as portal pressure autoregulation4 so that doubling portal flow or reducing it by 50% results in changes of only a few mmHg in portal pressure. Nevertheless, the extremely compliant vascular bed of the liver responds rapidly and dramatically to small changes in distending pressure, with an increase in distending pressure of 8 mmHg resulting in doubling of the hepatic blood volume.5
The impact of the passive consequences of portal pressure on hepatic blood volume are dramatically demonstrated in experiments using an in vivo hepatic plethysmograph in cats where the active regulators of hepatic blood volume have been largely eliminated by removal of the pituitary gland, the adrenal glands, the kidneys, and hepatic denervation. In this model, hemorrhage results in a decrease in splanchnic blood flow and portal venous pressure with hepatic blood volume rapidly decreasing to compensate for 25% of the hemorrhaged blood volume. Through the use of vascular snares on the arteries supplying the splanchnic beds, an equal reduction in portal blood flow to that produced by the hemorrhage lead to an equal decrease in hepatic blood volume, which is presumed to result entirely in response to the reduction in intrahepatic blood pressure.6 Partial occlusion of the superior mesenteric artery in dogs led to a reduction of portal venous pressure of 2.8 mmHg and a rise in cardiac output of 19%.7
Thus, a decrease in portal blood flow results in a decrease in portal pressure and a passive expulsion of blood from the liver into the central venous compartment. Depending upon the mechanism that caused the reduction in portal flow, the hepatic blood volume response serves either to maintain the venous return (preload to the heart) or to actually increase it, thus maintaining or elevating the cardiac output which, in turn, results in increased flow to the splanchnic arteries and a partial correction of the portal flow.
The role of hepatic compliance in diseased livers is not clear. The hepatic blood volume response to hemorrhage was dramatically decreased in a 14 day chronic bile duct ligation model of liver disease in cats. However, hepatic compliance was, unexpectedly, not affected despite the presence of severe biliary hyperplasia, portal tract distortion, and fibrosis. The reduction in hepatic vascular response to hemorrhage appeared to be accounted for by dysfunction of hepatic sympathetic nerves, as the direct response to nerve stimulation was severely impaired whereas the response to infused norepinephrine was well maintained8 (stressed volume was not altered, unstressed volume was impaired).
Although research has not been specifically carried out to examine the stressed and unstressed liver volume responses in the more severely diseased liver, it seems reasonable to anticipate that a cirrhotic liver is less distensible and therefore plays a reduced role in this disease state. Similarly, when cirrhosis results in extensive portacaval shunting, any change in portal inflow is reflected as changes in the outflow via the portacaval shunt. The liver would not be exposed to the changed flow or pressure and portal inflow would not impact on hepatic capacitance thus eliminating this mechanism as a regulator of hepatic blood flow.
THE HEPATIC ARTERIAL BUFFER RESPONSE
The historical perspective of the development of the modern hepatic arterial buffer response (HABR) concept has previously been reviewed.9 Prior to 197710 it was the consensus, strongly and commonly stated in textbooks and reviews, that hepatic metabolic supply and demand regulated hepatic arterial blood flow in the same manner as arterial blood flow was regulated in other organs. A survey of the literature indicates that there does not appear to ever have existed experimental evidence to support this contention. Although many extrinsic factors such as hepatic sympathetic nerves, circulating hormones and nutrients may dramatically affect hepatic arterial blood flow, the primary intrinsic regulator of the arterial flow appears to be the inverse reaction of the hepatic artery to changes in portal blood flow. Child,11 in his classical treatise on the portal vascular circulation, attributed the first observation of the effect of changes in portal perfusion on hepatic arterial blood flow to Betz in 186312 and Gad in 1873.13
The discovery of the mechanism of the HABR is an example of pure serendipity where it was observed that hemodilution, resulting in a dramatic decrease in hepatic oxygen delivery, did not result in the anticipated dilation of the hepatic artery. Subsequent studies showed that both increases and decreases in hepatic metabolic activity were without the anticipated effects on hepatic arterial blood flow and that the only parameter that appeared to correlate with changes in hepatic arterial blood flow was the opposite changes in portal flow.10 A number of alternative hypotheses were tested and rejected prior to demonstration of the adenosine washout theory.14
The hepatic vascular bed is unique in many ways including the fact that it receives blood flow from the portal vein as well as a separate hepatic arterial supply. These blood vessels undergo progressive parallel divisions that eventually travel as their terminal branches through a small space referred to as the space of Mall, which is surrounded by a limiting plate of hepatocytes. The space of Mall is seen in the portal triad, which is most typically identified as an enclosed space arranged in a hexagonal pattern around a central hepatic venule. In the space of Mall, the hepatic artery is intimately intertwined with the portal venule. The two vessels eventually drain into the hepatic sinusoids. Adenosine appears to be produced at a constant rate, independent of oxygen supply or demand, and is secreted into the space of Mall where it serves as a powerful dilator of the hepatic artery. The concentration of adenosine is regulated by the rate of washout into the blood vessels that pass through the space of Mall. According to this theory, a decrease in portal blood flow results in a reduced washout of adenosine and the accumulated adenosine concentration results in dilation of the hepatic artery thus partially compensating for the decrease in portal blood flow. A similar mechanism accounts for autoregulation of the hepatic artery whereby an increase in hepatic arterial flow leads to an increased washout of adenosine and a subsequent constriction of the artery.15 Thus, adenosine was the first blood flow-dependent blood flow regulator to be identified. Although the buffer capacity of this mechanism results only in a partial compensation for changes in portal flow, it often results in a full compensation for the decrease in oxygen delivery9 even in cirrhotic livers.16
The role of adenosine as the regulator of the HABR initially appears inconsistent with the statement that the hepatic artery is not controlled by the oxygen supply or demand to the liver, especially considering that the known primary sources of adenosine are breakdown products of the adenine nucleotides and cyclic AMP. However, adenosine production by oxygen-independent demethylation of S-adenosyl-homocysteine accounts for basal adenosine production in the heart17 and could also account for its production in the liver.
Evidence consistent with the HABR hypothesis9 includes the observation that adenosine is an extremely potent dilator of the hepatic artery. In addition, the hypothesis requires that portal blood must have access to the arterial resistance vessels so that portal flow can wash adenosine away from the area of the resistance vessels. This is shown by the observation that adenosine given into the portal blood has ready access to the arterial resistance vessel sites and results in dose-dependent arterial vasodilation. Potentiators of the effects of exogenous adenosine also potentiate the buffer response and blockers of the effects of exogenous adenosine also inhibit the buffer response. Consistent with classical pharmacological theory, adenosine receptor antagonists are more effective at blocking exogenously given adenosine than adenosine released endogenously. Nevertheless, full dose–response studies indicate that a complete and selective blockade of the dilator effect of adenosine and the HABR can be achieved using 8-phenyltheophylline, which leaves the response to other dilators, including isoproterenol, intact.18,19
One area that continues to cause confusion related to the adenosine hypothesis is based upon the unusual anatomy of the hepatic microcirculation. Hepatic microvascular terminology remains controversial. The ‘lobular’ concept has the microvascular unit of the liver as a tissue mass supplied by six sets of inlet vessels (terminal hepatic arteriole and portal venule) and one outlet vessel (the central venule). The ‘acinar’ concept has one set of inlet vessels and six outlet venous drainage channels. The regulatory processes related to the hepatic arterial buffer response and to a hepatorenal reflex are clearly related to the inlet side of the hepatic vasculature. Moreover, other vascular beds typically show tissue perfusion via one arterial inlet with several alternate venous pathways. The HABR hypothesis is most easily interpreted from the acinar perspective where the microvascular unit is the tissue mass supplied by the paired terminal branches of the hepatic artery and portal vein. The concepts reviewed in this manuscript are explained using the acinus; however, they could as easily be explained using the lobular terminology.
The terminal branches of the hepatic portal venules and arterioles drain into the center of the hepatic acinus, which represents a sphere of hepatic tissue of approximately 2 mm in diameter. Blood flows concurrently in adjacent sinusoids and passes approximately 16 hepatocytes prior to draining into the terminal hepatic venules. The microvascular anatomy is such that this unique separation of inlet and outlet vessels precludes diffusion of products produced by the hepatocytes from moving upstream to act on the arterial resistance vessels. Thus, although the liver is capable of producing huge amounts of adenosine in response to hypoxia, this adenosine is produced by hepatocytes that export the adenosine into the sinusoidal blood. The blood flows away from the resistance vessels so that the resistance vessels are not affected by hepatic parenchymal cell adenosine production or by other dilator substances released from these parenchymal or sinusoidal cells. Although the role for adenosine in regulating the hepatic arterial buffer response has been clearly demonstrated, the site of adenosine production, the cell type, and the specific biochemical pathway of production have not been identified, primarily due to the inaccessibility of the very small fluid space of Mall and the inability to sample directly from that space.
The hepatic arterial buffer capacity is difficult to quantitate. To accurately quantitate the buffer capacity, changes in portal flow must be induced in the absence of reflex, hormonal, or arterial pressure changes. These conditions are virtually impossible to attain except in very invasive surgical protocols. Simple occlusion of the portal vein will result in splanchnic pooling and reduced arterial pressure, and occlusion of the superior mesenteric artery will result in reduced portal flow but increased arterial pressure. Nevertheless, these simple procedures are a useful means by which to demonstrate the presence but not the quantification of the buffer response.
The HABR is fully maintained in transplanted human livers20,21 and appears to be maintained in liver diseases of considerable severity.16,22–26 Portal flow remains high as long as 2 years after liver transplantation, mainly as a result of elevated splenic blood flow, and is associated with reduced hepatic arterial flow.20
Elevated intra-abdominal pressure that occurs as a result of the inflation of peritoneal spaces using CO2 during laparoscopic surgery results in decreased blood flow to the splanchnic organs but the HABR results in preservation of the hepatic arterial flow, thus providing protection for liver function during sustained elevations in intra-abdominal pressure.27–29 However, it has been reported that a CO2 pneumoperitoneum resulted in a decrease in portal flow without compensatory HABR and resulted in evidence of hepatic tissue damage after 2 h of pneumoperitoneum in rats.30
The HABR is activated during an acute hemorrhage response, thereby offering protection to the liver.31 The HABR also tends to maintain hepatic blood flow constant in the face of systemically administered vasoactive compounds, leading some to incorrect conclusions as to the effect of pharmacological agents on the hepatic artery. For example, adenosine, isoproterenol, and glucagon all produce vasodilation of the hepatic artery when infused directly into the hepatic artery. However when given systemically they lead to an increased portal blood flow with resultant activation of the HABR, leading to constriction of the hepatic artery, depending upon the dose, and can actually lead to a decrease in hepatic arterial blood flow.32
Although the exact site of interaction of the hepatic artery and portal vein has not been identified, it is clearly occurring at a very localized level. Selective ligation of the portal inflow into a lobar vein leads to an increase in portal flow in the unligated lobes associated with activation of the HABR and a decrease in arterial flow; the lobes with ligated portal flow had an increase in the hepatic arterial flow.33 Richter et al. have suggested that the merging of increased hepatic arterial flow, induced by occlusion of the portal vein, occurs well upstream from the sinusoids and results in maintenance of homogeneity of sinusoidal perfusion.19
If a HABR response to brief portal occlusion does not occur prior to establishment of a portacaval shunt to reduce portal hypertension, those patients will show the greatest reduction in portal pressure.34 Unfortunately, those are the same patients with the poorest prognosis for survival.35 The demonstration of an intact HABR, by observing an elevated portal and decreased arterial flow after a balanced liquid meal,36 has been suggested as a tool to assess the severity of liver disease.37
In the presence of significant portacaval shunts, the HABR may become totally dysfunctional in that changes in portal flow will be reflected in changes through the portacaval shunts rather than through the liver, thereby having no impact on local adenosine concentrations. Changes in portal blood flow can normally result in the full range of arterial vascular responses from full constriction to full dilation. Therefore, it would be anticipated that the hepatic artery, in instances of complete portacaval shunting, would be fully dilated, thus benefiting oxygen supply. However, it has been suggested that the buffer capacity may be insufficient to maintain a normal oxygen supply in cirrhotic livers.38 A complete portacaval shunt leads to arterial flow effluxing retrograde through the portal vein and is associated with long-term microvascular reorganization.39
HEPATORENAL REFLEX
Patients who die from liver disease die in renal failure. Renal dysfunction is demonstrable at the early stages of liver disease. As liver injury progresses, functional renal failure develops with sodium and water retention, decreased renal blood flow and glomerular filtration rate in the absence of significant morphological changes in the kidney. Various mechanisms have been suggested for the pathogenesis of renal insufficiency secondary to acute and chronic liver injury including: peripheral arterial vasodilation secondary to overproduction of vasodilator substances in the splanchnic circulation leading to splanchnic pooling and decreased effective systemic arterial plasma volume;40–43 overproduction of endothelin due to endotoxemia leading to renal vasoconstriction;40–43 and activation of a hepatorenal baroreflex that stimulates renal sympathetic nerves leading to sodium retention.42,44–47 We have recently suggested that a hepatic blood flow-dependent hepatorenal reflex is the primary pathophysiological mechanism for renal dysfunction in liver disease. This reflex is activated by adenosine in the space of Mall that is regulated by hepatic blood flow.48–51
It has long been recognized that in hepatic cirrhosis, the disturbance in hepatic portal circulation relates to the pathogenesis of sodium and water retention through the activation of a hepatorenal reflex.52 Liver cirrhosis is characterized by increases in renal sympathetic nerve activity.44 Selective bilateral renal denervation produced by lumbar sympathetic anesthetic block promotes renal water and sodium excretion in these patients.53 Animal models of cirrhosis show an increase in renal efferent sympathetic nerve activity that contributes significantly to the pathophysiological renal retention of sodium and water resulting from activation of a hepatic afferent limb.54–56 Although the efferent limb of the renal disturbance is reasonably defined, the afferent limb has, until recently, remained unclear.
A consensus appears to have arisen that the intrahepatic vascular resistance that occurs in chronic liver disease results in portal hypertension with the elevated portal pressure activating the afferent limb of the hepatorenal reflex. However, such a reflex implies a positive feedback situation whereby the normal physiology would result in an increase in portal blood flow causing an increase in portal pressure and activation of the hepatorenal reflex. This would result in salt and water retention and an expanded blood volume, leading to increased cardiac output and increased portal flow with a further increase in portal pressure. The alternative hypothesis of portal flow being the sensed parameter regulating the hepatorenal reflex had not been previously suggested, in fact there had never been a suggestion of regional blood flow being monitored by sensory nerves in any organ. Nevertheless, a number of earlier studies had suggested that the hepatorenal reflex is unlikely to be activated in response to baroreceptors. Using anesthetized dogs, Koyoma et al. observed that the partial occlusion of the portal vein resulted in activation of renal sympathetic nerves that was not related to increases in either extrahepatic portal pressure or intrahepatic sinusoidal pressure because intrahepatic sinusoidal pressure was decreased in these studies.46 Levy and Wexler found that sodium retention persisted in cirrhotic dogs after end-to-side portacaval anastomoses, a maneuver that normalized intrahepatic hypertension but was still associated with a dramatic decrease in intrahepatic portal blood flow.57 Liang reported a lack of correlation of increased portal pressure with the rate of urine flow at portal pressure elevations up to 15 cm of water; only at pressures above this level, when portal blood flow would have been reduced, did the urine flow rate begin to decrease.58 Most of the studies purporting to show evidence for portal pressure regulation of the hepatorenal reflex have also resulted in reduction of intrahepatic portal flow. Cirrhosis is characterized by a hyperdynamic splanchnic circulation and portal hypertension42,59 but, because of the presence of portacaval shunts directing flow around the liver, the blood flow that directly perfuses functional sinusoidal and parenchymal hepatocytes is actually decreased.60
The hypothesis relating intrahepatic blood flow to the hepatorenal reflex is supported by a recent series of publications and ongoing studies reported by us. The hypothesis is that functional portal blood flow through the liver results in reduced washout of adenosine from the space of Mall, as described in the previous section related to the hepatic arterial buffer response. Adenosine acts on sensory nerves arising in the space of Mall and activates the hepatorenal reflex.
We established a vascular shunt connecting the portal vein and vena cava in rats to allow for control of the portal venous blood flow.49 Partial occlusion of the portal vein close to the hilum of the liver decreased intrahepatic portal flow and the extra portal flow was allowed to bypass the liver through the shunt to prevent splanchnic congestion. A 50% decrease in intrahepatic portal flow through this mechanism did not cause significant changes in systemic arterial blood pressure but decreased urine flow by 38% and sodium excretion by 44%. The renal effect of reduced portal blood flow was prevented by hepatic denervation or intraportal administration of the adenosine receptor antagonist, 8-phenyltheophylline. Involvement of intrahepatic baroreceptors was eliminated because intrahepatic sinusoidal pressure was decreased following partial portal vein occlusion. These studies provided the first evidence that intrahepatic portal flow could activate a hepatorenal reflex.
Our prior studies related to the HABR indicated that adenosine in the space of Mall was regulated by intrahepatic blood flow. The observation that the hepatic perivascular region is also rich in sensory nerves61 supported the feasibility of an adenosine-mediated afferent limb in the hepatorenal reflex. Adenosine has previously been shown to activate sensory nerves in the carotid body62 and in the heart.63 Stimulation of myocardial adenosine A1 receptors increased the discharge of cardiac afferent fibers and resulted in an increase in neural discharge of the renal sympathetic efferent fibers in anesthetized dogs.63,64 To test if adenosine could activate a hepatic afferent reflex, adenosine was infused directly into the portal vein and resulted in a significant decrease in urine flow and sodium excretion. In contrast, intravenous adenosine at the same dose was without any effect on renal function, thereby indicating that the effect of the infused adenosine was through the liver and not a direct action on the kidney. Intraportal infusion of the adenosine receptor antagonist, 8-phenyltheophylline, abolished the renal response to intraportal adenosine. Further, both hepatic and renal denervation abolished the renal response to adenosine, thereby proving the reflex connection.48 Thus, these data taken together are consistent with the hypothesis that reduction in intraportal blood flow leads to an adenosine-mediated activation of hepatic afferent nerves which results in a sympathetic reflex to the kidneys leading to fluid retention.
This response would serve a useful function in normal physiological conditions where the reduced portal flow would cause fluid retention, thereby increasing the circulating blood volume and cardiac output. The elevated cardiac output would result in elevated portal flow, thus correcting the flow imbalance to the liver. The hypothesis also proposes that, in the diseased state, with portacaval shunts existing, the signal would be anticipated to occur as a result of the decreased intrahepatic portal flow. However, in this state, the salt and water retention would not lead to a correction of the intrahepatic flow but, rather, would lead to elevated cardiac output and elevated portal inflow which would simply bypass the liver through the shunts and lead to a progressive, inappropriate reflex accumulation of fluid.
We have recently demonstrated that renal dysfunction is mediated through this adenosine-dependent hepatorenal reflex in both acute and chronic liver disease models in rats. Chronic administration of the hepatotoxin, thioacetamide, resulted in severe fibrosis consistent with advanced liver disease. Reduced basal urine flow and a reduced ability to excrete a saline load were demonstrated. The renal dysfunction was partially corrected by intrahepatic administration of the adenosine receptor antagonist, 8-phenyltheophylline.50 The acute model of liver injury involved intraperitoneal injection of thioacetamide (500 mg/kg) in rats. Severe liver injury was demonstrated 24 h after the insult and was associated with reduced renal arterial blood flow and glomerular filtration rate and sodium retention. The response to a saline volume expansion challenge was inhibited. As with the other models, 8-phenylpheophylline improved urine production. To specify the adenosine receptor subtype, selective adenosine A1 and A2 receptor antagonists were compared. The selective A1 antagonist, 8-cyclopentyl-1,3-dipropylxanthine, greatly improved the impaired renal function induced by acute liver injury and this beneficial effect was blunted in rats with liver denervation. In contrast, intravenous administration of the antagonist was only effective at higher doses, thereby confirming that the adenosine receptor antagonist was acting on the liver and not directly on the kidney. The adenosine A2 agonist was without impact on the renal function.51
Although both the chronic and acute liver disease models clearly demonstrated an adenosine-dependent hepatorenal reflex impairment of renal function, the relationship to intrahepatic portal flow in diseased livers cannot be assumed. Adenosine concentrations in the space of Mall can be elevated by reduced portal flow or intrahepatic vascular shunting but it is equally possible that adenosine levels could be elevated independent of blood flow secondary to hepatic inflammation65–67 or by a decrease in the recycling of adenosine through the adenosine kinase pathway.68 Regardless of the source of increased adenosine in the diseased state, the normal physiology is strongly supportive of a hepatic reflex mechanism by which the liver indirectly affects its own blood flow. The involvement of this reflex in liver disease suggests a therapeutic approach treating the early renal dysfunction and, perhaps, even the late-stage hepatorenal syndrome through the blockade of intrahepatic adenosine A1 receptors.
MODULATION OF VASOCONSTRICTORS BY ADENOSINE AND NITRIC OXIDE
Vasoconstriction of the hepatic artery, whether produced by sympathetic nerve activation or delivery of vasoconstrictors to the resistance vessels through the circulation, leads to reductions in hepatic arterial flow. The portal circulation, however, responds to constrictors by an elevation in portal pressure with portal flow remaining constant, as portal flow is regulated by the outflow of the extrahepatic splanchnic organs. Nitric oxide and adenosine play an additional protective role tending to minimize the impact of vasoconstrictors on hepatic blood flow.
The role of nitric oxide in modulating vasoconstrictors in the liver appears to be dependent upon shear stress.69 If vasoconstriction leads to increased shear stress (flow held steady, pressure increasing), nitric oxide release suppresses the constriction thus protecting the hepatic endothelial cells from shear stress-induced disruption. Blockade of nitric oxide synthase potentiates the response of both the hepatic artery and portal vein to sympathetic nerve stimulation and norepinephrine infusion. However, if shear stress is not increased during the constriction (flow allowed to decrease, pressure held steady), nitric oxide is not released and blockade of nitric oxide synthase is without impact.70 The hepatic artery responds to vasoconstriction by an initial reduction in blood flow but, in the face of continued stimulation, the flow returns toward baseline by a process referred to as vascular escape. Vascular escape in the hepatic artery is mediated by nitric oxide70 probably secondary to shear stress induced in the portal vein, as vascular constriction in the portal venules does not reduce portal flow but does increase portal pressure and therefore shear stress.
Adenosine has been shown to antagonize the vasoconstriction of the hepatic artery induced by a range of endogenous constrictors including sympathetic nerves, norepinephrine, angiotensin, and vasopressin.71 In contrast, adenosine has insignificant effects on either the basal portal vascular tone or on the action of vasoconstrictors on the portal vein or capacitance vessels in cats at doses that significantly modulated the arterial responses.72 Adenosine may therefore play a modest role in suppressing vasoconstriction and reduced blood flow via the hepatic artery.
Thus, the combination of adenosine and nitric oxide provide the liver with a unique ability to escape from severe vasoconstrictor influences. The role of adenosine is likely only activated if total hepatic blood flow is reduced and results in local accumulation of adenosine at the vascular resistance site. In contrast, local constriction restricted to the liver is antagonized by shear stress/nitric oxide-induced vasodilation. By this mechanism, shear stress is minimized in the portal circulation and the rise in portal pressure is attenuated and the reduction in blood flow in the hepatic artery is antagonized. By these mechanisms, the liver can protect itself from excess vasoconstriction whether blood flow is reduced or shear stress is increased and whether generalized or regional hepatic vasoconstriction occurs. This is important in the liver in contrast to other vascular beds where vasoconstriction results in regional hypoxia and release of vasodilator substances that inhibit the constriction. This mechanism is not tenable in the liver because vasodilator substances released from hypoxic hepatocytes enter the sinusoidal blood and are swept downstream to the hepatic veins without the opportunity for contact with the resistance vessels upstream.
BLOOD FLOW REGULATION OF HEPATOCYTE PROLIFERATION
We now discuss the hypothesis, first proposed in 1997,73 that changes in portal blood flow lead to shear stress-dependent changes in hepatic nitric oxide production which serves as the initial trigger for the activation of a complex cascade of events leading to cellular proliferation in the case of elevated portal flow or apoptosis in the case of reduced portal flow.
Prior to 1954, there were a number of studies that were compatible with the hypothesis that hepatic blood flow regulated liver cell mass, but a few poorly conducted and improperly interpreted studies led to a rapid consensus that hepatic blood flow was not a significant regulator of liver mass. However, in a review on hepatic circulation, Greenway and Lautt suggested that the coincidence of enzyme induction and elevated portal flow that had been interpreted to suggest that an increase in hepatic metabolism and liver volume led to an increase in portal flow was inconsistent with several clearly defined studies demonstrating that the liver cannot directly control portal blood flow.1 We suggested that the data were better accounted for by blood flow controlling liver cell mass rather than liver cell mass controlling blood flow.
The liver is well recognized to have a unique ability to rapidly regenerate. Perhaps even the ancient Greeks knew of this remarkable ability because the legend of Prometheus describes the wrathful punishment by Zeus for the sin of revealing the secret of fire to mankind by the unique torture of the chained Prometheus having his liver plucked out by an eagle by day only to have it regenerated by night, thus perpetuating his torment indefinitely. Although the extent of hepatic liver regeneration is exaggerated by this legend, it remains a striking observation that following a two-thirds partial hepatectomy in rats, full restoration of liver volume can be obtained within approximately 1 week and 50% of the recovery occurs within 48 h. In a review of hepatic regeneration, Michalopolous and DeFrances indicated that, despite over 100 years of research, the trigger of liver regeneration remained unknown and that the discovery of this trigger would be akin to the big bang theory of evolution of the universe.74
For a finite event to be proposed as a trigger for the regeneration cascade, the event must occur immediately after the partial hepatectomy and serve as a trigger for the entire cascade. A dramatic hemodynamic stimulus occurs at the time of surgical removal of liver lobes or selective ligation of portal lobar veins. With the classical model of a two-thirds partial hepatectomy, all of the portal blood flow is forced to pass through the remaining liver mass thereby increasing the flow-to-mass ratio to three times normal levels. Vascular shear stress in the liver can be assessed from changes in portal pressure and results in the release of nitric oxide which has a significant impact on vascular and metabolic responses to sympathetic nerve stimulation.75 The first studies to test this shear stress/nitric oxide hypothesis73,76 were based on previous observations that a wide range of hepatic proliferating factors appeared in the plasma of animals that had been subjected to a partial hepatectomy. We developed a bioassay to detect the presence of proliferating factors utilizing the ability of plasma from a rat with partial hepatectomy to stimulate hepatocyte proliferation in vitro. Blood removed from animals that had been subjected to a two-thirds partial hepatectomy showed maximal proliferative stimulation from samples drawn 4 h after the partial hepatectomy. The nitric oxide synthase antagonist, L-NAME, was given to prevent shear stress-induced stimulation of nitric oxide production. Blood from these animals showed no proliferative activity.73 The response was restored by provision of a nitric oxide donor to the liver.77
Subsequent studies evaluated the earliest and latest stages of the regeneration cascade. At the early stage, we utilized the expression of an immediate early gene that had previously been shown to reach a peak activation 15 min after partial hepatectomy and was dependent on the degree of partial hepatectomy performed.78 C-fos activation was shown to occur in the remnant liver following partial hepatectomy and not in sham-operated animals.79 C-fos mRNA expression was prevented by blocking hepatic nitric oxide synthase activation and by blocking prostaglandin production, both of which are regulated by shear stress. Activation of c-fos was inhibited by blockade of nitric oxide synthase or cyclooxygenase and could be reversed in both cases by giving nitric oxide donors and the prostaglandins, PGE2 and PGI2, suggesting that there is an interaction between nitric oxide and prostaglandins in triggering the liver regeneration cascade.80 The late response was quantified from liver mass restoration determined 48 h after the partial hepatectomy. The phosphodiesterase V antagonist, zaprinast, the nitric oxide donor, SNAP, and PGI2 potentiated early c-fos mRNA expression and 48 h hepatocyte mass restoration.
The relationship between hepatic blood flow and regulation of hepatocyte proliferation was strongly supported by the demonstration that prevention of shear stress following partial hepatectomy blocked the activation of the regeneration cascade. Occlusion of the superior mesenteric artery decreases hepatic blood flow by approximately two-thirds; a two-thirds partial hepatectomy delivers the entire portal flow to one-third of the normal liver mass thereby increasing hepatic blood flow per remaining liver mass by three times. Therefore, occlusion of the superior mesenteric artery following a two-thirds partial hepatectomy should prevent the development of shear stress in the remnant liver. This was shown by a lack of activation of c-fos in this model.79 Selective ligation of portal lobar veins leads to decreased portal flow in the ligated lobes with elevated flow to the unligated lobes. Liver volume adjusts so that flow per unit liver weight is restored after 1 week by hypertrophy of the unligated lobes and atrophy of the ligated lobes.33 The selective ligation of the left branch of the portal vein resulted in increased portal flow to the unligated two-thirds of the liver and led to similar elevation in portal pressure as was achieved by two-thirds partial hepatectomy of the same lobes thus indicating similar elevations of shear stress. The resultant elevations in c-fos in the unligated lobes and the appearance of proliferating factors in plasma were similar to what was seen after surgical removal of the ligated lobes and could be blocked by nitric oxide synthase antagonists.79 This study confirmed that the trigger for regeneration was hemodynamic in nature and regulated by nitric oxide and was not dependent upon reduction of liver parenchymal cell mass.
The relationship of portal pressure (shear stress) to the triggering of regeneration was also shown by Sato et al. who suggested that there was an upper limit to a beneficial effect of elevated portal pressure.81 A 90% partial hepatectomy raised portal pressure to an extent that was suggested to account for a lesser degree of effective regeneration. C-fos activation 15 min after partial hepatectomy also increased in proportion to the degree of ablation but the 90% hepatectomy was less effective.78 Maintained hyperdynamic portal circulation, seen after human liver transplant, was also associated with more rapid liver regeneration.82
These hemodynamic relationships to shear stress and liver volume do not appear to have been studied in liver disease but the presence of portacaval shunts and altered intrahepatic hemodynamics could be a major cause of reduced hepatic regenerative capacity in diseased states.
CONCLUSIONS
The hepatic vascular bed plays several major roles in homeostasis. Liver blood volume is rapidly expanded or contracted in response to both active and passive stimuli to regulate venous return and therefore cardiac preload and cardiac output. Changes in portal blood flow are determined entirely by the splanchnic organs that drain into the portal vein and the liver has no direct means by which to control its portal inflow. Changes in portal flow lead to changes in portal and intrahepatic pressure which result in passive action against the compliant vascular bed so that the liver serves as a volume buffer to regulate cardiac output. By this mechanism, a decrease in portal blood flow leads to a passive expulsion of blood from the liver thereby leading to an elevation in cardiac output and at least partial restoration of portal blood flow.
A reduction in portal blood flow also simultaneously activates the hepatic arterial buffer response by virtue of the reduced portal flow washing away less adenosine from the space of Mall surrounding the hepatic arteriole resistance vessels. Adenosine results in vasodilation of the hepatic artery, thereby accounting for the mechanism of the hepatic arterial buffer response. The impact of the buffer response is immediate. At the same time, the elevated adenosine concentration acts on hepatic afferent nerves to stimulate a hepatorenal reflex resulting in decreased urine output and sodium retention, thereby leading to a prolonged fluid retention and resultant increase in cardiac output. This mechanism, while serving the normal physiological role of tending to maintain hepatic blood flow, is proposed to be the mechanism of renal dysfunction in liver disease where portal flow is directed around the liver through portacaval shunts or where adenosine production supplying the space of Mall is elevated secondary to the metabolic dysfunctions occurring in the diseased liver.
The liver also has a unique response to severe vasoconstriction. Under normal physiological situations, regional intrahepatic vasoconstriction results in a lack of impact on portal flow but the intrahepatic portal resistance increases portal pressure and shear stress and causes release of nitric oxide which inhibits the constriction and accounts for vascular escape from the constrictors. If vasoconstriction is more systemic and results in reduced portal flow, the accumulated adenosine counteracts the constriction of the hepatic artery but not the portal or capacitance vessels.
Finally, if these mechanisms do not correct an imbalance in the blood flow-to-liver mass ratio, the liver responds by adjusting the hepatocyte total mass through a hemodynamic mechanism whereby hepatic blood flow results in shear stress-induced regulation of hepatic nitric oxide and prostaglandins which, in turn, serves as a trigger for a complex cascade of events regulating hepatocyte proliferation. Thus, if the ratio of total hepatic blood flow-to-liver mass cannot be maintained by adjustments to blood flow, the liver adjusts the hepatocyte mass.
Acknowledgments
The experimental work of the author, upon which this review is primarily based, was contributed to by numerous colleagues, trainees, and technologists over several decades. Clive Greenway was the major collaborator for the hepatic compliance work, Dallas Legare for the hepatic arterial buffer response, Zhi Ming for the hepatorenal studies, Helen Wang and Jodi Smith Schoen for the hepatic regeneration studies. Manuscript preparation was by Karen Sanders.
Funding of the studies was provided primarily by the Heart and Stroke Foundations of Saskatchewan and Manitoba, the Canadian Institutes of Health Research, the Kidney Foundation of Manitoba, and the Canadian Liver Foundation.
References
- 1.Greenway CV, Lautt WW. Hepatic circulation. In: Schultz SG, Wood JD, Rauner BB, editors. Handbook of Physiology. The Gastrointestinal System I. Part 2, Chapter 41. Vol. 1. American Physiological Society; New York: Oxford University Press; 1989. pp. 1519–64. [Google Scholar]
- 2.Greenway CV, Lautt WW. Blood volume, the venous system, preload, and cardiac output. Can J Physiol Pharmacol. 1986;64:383–7. doi: 10.1139/y86-062. [DOI] [PubMed] [Google Scholar]
- 3.Greenway CV, Seaman KL, Innes IR. Norepinephrine on venous compliance and unstressed volume in cat liver. Am J Physiol. 1985;248:H468–76. doi: 10.1152/ajpheart.1985.248.4.H468. [DOI] [PubMed] [Google Scholar]
- 4.Lautt WW, Legare DJ. Passive autoregulation of portal venous pressure: distensible hepatic resistance. Am J Physiol. 1992;263:G702–8. doi: 10.1152/ajpgi.1992.263.5.G702. [DOI] [PubMed] [Google Scholar]
- 5.Lautt WW, Greenway CV. Hepatic venous compliance and role of liver as a blood reservoir. Am J Physiol. 1976;231:292–5. doi: 10.1152/ajplegacy.1976.231.2.292. [DOI] [PubMed] [Google Scholar]
- 6.Lautt WW, Brown LC, Durham JS. Active and passive control of hepatic blood volume responses to hemorrhage at normal and raised hepatic venous pressure in cats. Can J Physiol Pharmacol. 1980;58:1049–57. doi: 10.1139/y80-158. [DOI] [PubMed] [Google Scholar]
- 7.Groszmann RJ, Blei AT, Kniaz JL, Storer EH, Conn HO. Portal pressure reduction induced by partial mechanical obstruction of the superior mesenteric artery in the anesthetized dog. Gastroenterology. 1978;75:187–92. [PubMed] [Google Scholar]
- 8.Schafer J, d’Almeida MS, Weisman H, Lautt WW. Hepatic blood volume responses and compliance in cats with long-term bile duct ligation. Hepatology. 1993;18:969–77. doi: 10.1002/hep.1840180431. [DOI] [PubMed] [Google Scholar]
- 9.Lautt WW. The 1995 Ciba-Geigy Award Lecture. Intrinsic regulation of hepatic blood flow. Can J Physiol Pharmacol. 1996;74:223–33. [PubMed] [Google Scholar]
- 10.Lautt WW. The hepatic artery: subservient to hepatic metabolism or guardian of normal hepatic clearance rates of humoral substances. Gen Pharmacol. 1977;8:73–8. doi: 10.1016/0306-3623(77)90030-1. [DOI] [PubMed] [Google Scholar]
- 11.Child CG. The Hepatic Circulation and Portal Hypertension. Philadelphia: W.B. Saunders Company; 1954. [Google Scholar]
- 12.Betz W. The circulation within the liver, especially that of the hepatic artery. Zeitschrift fuer rat Med. 1863;18:44–60. [Google Scholar]
- 13.Gad J. Studies on the relations of the blood stream of the portal vein to the blood stream in the hepatic artery (Dissertation) Berlin: G. Schade; 1873. [Google Scholar]
- 14.Lautt WW. Role and control of the hepatic artery. In: Lautt WW, editor. Hepatic Circulation in Health and Disease. New York: Raven Press; 1981. pp. 203–26. [Google Scholar]
- 15.Ezzat WR, Lautt WW. Hepatic arterial pressure-flow auto-regulation is adenosine mediated. Am J Physiol. 1987;252:H836–45. doi: 10.1152/ajpheart.1987.252.4.H836. [DOI] [PubMed] [Google Scholar]
- 16.Mucke I, Richter S, Menger MD, Vollmar B. Significance of hepatic arterial responsiveness for adequate tissue oxygenation upon portal vein occlusion in cirrhotic livers. Int J Colorectal Dis. 2000;15:335–41. doi: 10.1007/s003840000247. [DOI] [PubMed] [Google Scholar]
- 17.Lloyd HGE, Schrader J. The importance of the transmethylation pathway for adenosine metabolism in the heart. In: Gerlach E, Becker BF, editors. Topics and Perspectives in Adenosine Research. Berlin: Springer-Verlag; 1987. pp. 199–208. [Google Scholar]
- 18.Lautt WW, Legare DJ. The use of 8-phenyltheophylline as a competitive antagonist of adenosine and an inhibitor of the intrinsic regulatory mechanism of the hepatic artery. Can J Physiol Pharmacol. 1985;63:717–22. doi: 10.1139/y85-117. [DOI] [PubMed] [Google Scholar]
- 19.Richter S, Vollmar B, Mucke I, Post S, Menger MD. Hepatic arteriolo-portal venular shunting guarantees maintenance of nutritional microvascular supply in hepatic arterial buffer response of rat livers. J Physiol. 2001;531:193–201. doi: 10.1111/j.1469-7793.2001.0193j.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bolognesi M, Sacerdoti D, Bombonato G, et al. Change in portal flow after liver transplantation: effect on hepatic arterial resistance indices and role of spleen size. Hepatology. 2002;35:601–8. doi: 10.1053/jhep.2002.31352. [DOI] [PubMed] [Google Scholar]
- 21.Henderson JM, Gilmore GT, Mackay GJ, Galloway JR, Dodson TF, Kutner MH. Hemodynamics during liver transplantation: the interactions between cardiac output and portal venous and hepatic arterial flows. Hepatology. 1992;16:715–18. doi: 10.1002/hep.1840160316. [DOI] [PubMed] [Google Scholar]
- 22.Aoki T, Imamura H, Kaneko J, et al. Intraoperative direct measurement of hepatic arterial buffer response in patients with or without cirrhosis. Liver Transpl. 2005;11:684–91. doi: 10.1002/lt.20380. [DOI] [PubMed] [Google Scholar]
- 23.Gulberg V, Haag K, Rossle M, Gerbes AL. Hepatic arterial buffer response in patients with advanced cirrhosis. Hepatology. 2002;35:630–4. doi: 10.1053/jhep.2002.31722. [DOI] [PubMed] [Google Scholar]
- 24.Iwao T, Toyonaga A, Shigemori H, et al. Hepatic artery hemodynamic responsiveness to altered portal blood flow in normal and cirrhotic livers. Radiology. 1996;200:793–8. doi: 10.1148/radiology.200.3.8756933. [DOI] [PubMed] [Google Scholar]
- 25.Richter S, Mucke I, Menger MD, Vollmar B. Impact of intrinsic blood flow regulation in cirrhosis: maintenance of hepatic arterial buffer response. Am J Physiol Gastrointest Liver Physiol. 2000;279:G454–62. doi: 10.1152/ajpgi.2000.279.2.G454. [DOI] [PubMed] [Google Scholar]
- 26.Saftoiu A, Ciurea T, Gorunescu F. Hepatic arterial blood flow in large hepatocellular carcinoma with or without portal vein thrombosis: assessment by transcutaneous duplex Doppler sonography. Eur J Gastroenterol Hepatol. 2002;14:167–76. doi: 10.1097/00042737-200202000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Putensen C, Wrigge H, Hering R. The effects of mechanical ventilation on the gut and abdomen. Curr Opin Crit Care. 2006;12:160–5. doi: 10.1097/01.ccx.0000216585.54502.eb. [DOI] [PubMed] [Google Scholar]
- 28.Tsuboi S, Kitano S, Yoshida T, Bandoh T, Ninomiya K, Baatar D. Effects of carbon dioxide pneumoperitoneum on hemodynamics in cirrhotic rats. Surg Endosc. 2002;16:1220–5. doi: 10.1007/s00464-001-9163-x. [DOI] [PubMed] [Google Scholar]
- 29.Yokoyama Y, Alterman DM, Sarmadi AH, et al. Hepatic vascular response to elevated intraperitoneal pressure in the rat. J Surg Res. 2002;105:86–94. doi: 10.1006/jsre.2001.6260. [DOI] [PubMed] [Google Scholar]
- 30.Richter S, Olinger A, Hildebrandt U, Menger MD, Vollmar B. Loss of physiologic hepatic blood flow control (‘hepatic arterial buffer response’) during CO2-pneumoperitoneum in the rat. Anesth Analg. 2001;93:872–7. doi: 10.1097/00000539-200110000-00014. [DOI] [PubMed] [Google Scholar]
- 31.Lautt WW, McQuaker JE. Maintenance of hepatic arterial blood flow during hemorrhage is mediated by adenosine. Can J Physiol Pharmacol. 1989;67:1023–8. doi: 10.1139/y89-161. [DOI] [PubMed] [Google Scholar]
- 32.Lautt WW, Lockhart LK, Legare DJ. Adenosine modulation of vasoconstrictor responses to sympathetic nerves and norepinephrine infusion in the superior mesenteric artery of the cat. Can J Physiol Pharmacol. 1988;66:937–41. doi: 10.1139/y88-152. [DOI] [PubMed] [Google Scholar]
- 33.Rocheleau B, Ethier C, Houle R, Huet PM, Bilodeau M. Hepatic artery buffer response following left portal vein ligation: its role in liver tissue homeostasis. Am J Physiol. 1999;277:G1000–7. doi: 10.1152/ajpgi.1999.277.5.G1000. [DOI] [PubMed] [Google Scholar]
- 34.Zimmon DS, Kessler RE. Effect of portal venous blood flow diversion on portal pressure. J Clin Invest. 1980;65:1388–97. doi: 10.1172/JCI109803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burchell AR, Moreno AH, Panke WF, Nealon TJ., Jr Hepatic artery flow improvement after portacaval shunt: a single hemodynamic clinical correlate. Ann Surg. 1976;184:289–302. doi: 10.1097/00000658-197609000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dauzat M, Lafortune M, Patriquin H, Pomier-Layrargues G. Meal induced changes in hepatic and splanchnic circulation: a noninvasive Doppler study in normal humans. Eur J Appl Physiol. 1994;68:373–80. doi: 10.1007/BF00843732. [DOI] [PubMed] [Google Scholar]
- 37.Lafortune M, Dauzat M, Pomier-Layrargues G, et al. Hepatic artery: effect of a meal in healthy persons and transplant recipients. Radiology. 1993;187:391–4. doi: 10.1148/radiology.187.2.8475279. [DOI] [PubMed] [Google Scholar]
- 38.Sato N, Hayashi N, Kawano S, Kamada T, Abe H. Hepatic hemodynamics in patients with chronic hepatitis or cirrhosis as assessed by organ-reflectance spectrophotometry. Gastroenterology. 1983;84:611–16. [PubMed] [Google Scholar]
- 39.McCuskey RS, Vonnahme FJ, Grun M. In vivo and electron microscopic observations of the hepatic microvasculature in the rat following portacaval anastomosis. Hepatology. 1983;3:96–104. doi: 10.1002/hep.1840030116. [DOI] [PubMed] [Google Scholar]
- 40.Ellis AJ, O’Grady JG. Clinical disorders of renal function in acute liver failure. In: Arroyo V, Ginès P, Rodés J, Schrier RW, editors. Ascites and Renal Dysfunction in Liver Disease: Pathogenesis, Diagnosis, and Treatment. Malden: Blackwell Science; 1999. pp. 36–62. [Google Scholar]
- 41.Gentilini P, Laffi G, Villa GL, Romanelli RG, Blendis LM. Ascites and hepatorenal syndrome during cirrhosis: two entities or the continuation of the same complication? J Hepatol. 1999;31:1088–97. doi: 10.1016/s0168-8278(99)80324-9. [DOI] [PubMed] [Google Scholar]
- 42.Gines P, Arroyo V. Hepatorenal syndrome. J Am Soc Nephrol. 1999;10:1833–9. doi: 10.1681/ASN.V1081833. [DOI] [PubMed] [Google Scholar]
- 43.Gines P, Guevara M, Arroyo V, Rodes J. Hepatorenal syndrome. Lancet. 2003;362:1819–27. doi: 10.1016/S0140-6736(03)14903-3. [DOI] [PubMed] [Google Scholar]
- 44.DiBona GF. Reflex regulation of renal sympathetic nerve activity in cirrhosis. In: Häussinger D, Jungermann K, editors. Liver and Nervous System. Falk Symposium No. 103. London: Kluwer Academic Publishers; 1998. pp. 315–19. [Google Scholar]
- 45.Jalan R, Forrest EH, Redhead DN, Dillon JF, Hayes PC. Reduction in renal blood flow following acute increases in the portal pressure: evidence for the existence of a hepatorenal reflex in man? Gut. 1997;40:664–70. doi: 10.1136/gut.40.5.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Koyoma S, Kanai K, Aibiki M, Fujita T. Reflex increase in renal nerve activity during acutely altered portal venous pressure. J Auton Nerv Syst. 1988;23:55–62. doi: 10.1016/0165-1838(88)90166-x. [DOI] [PubMed] [Google Scholar]
- 47.Lang F, Tschernko E, Schulze E, et al. Hepatorenal reflex regulating kidney function. Hepatology. 1991;14:590–4. doi: 10.1016/0270-9139(91)90043-u. [DOI] [PubMed] [Google Scholar]
- 48.Ming Z, Smyth DD, Lautt WW. Intrahepatic adenosine triggers a hepatorenal reflex to regulate sodium and water excretion. Auton Neurosci. 2001;93:1–7. doi: 10.1016/S1566-0702(01)00315-0. [DOI] [PubMed] [Google Scholar]
- 49.Ming Z, Smyth DD, Lautt WW. Decreases in portal flow trigger a hepatorenal reflex to inhibit renal sodium and water excretion in rats: role of adenosine. Hepatology. 2002;35:167–75. doi: 10.1053/jhep.2002.30425. [DOI] [PubMed] [Google Scholar]
- 50.Ming Z, Fan YJ, Yang X, Lautt WW. Blockade of intrahepatic adenosine receptors improves urine excretion in cirrhotic rats induced by thioacetamide. J Hepatol. 2005;42:680–6. doi: 10.1016/j.jhep.2004.12.023. [DOI] [PubMed] [Google Scholar]
- 51.Ming Z, Fan YJ, Yang X, Lautt WW. Contribution of hepatic adenosine A1 receptors to renal dysfunction associated with acute liver injury in rats. Hepatology. 2006;44:813–22. doi: 10.1002/hep.21336. [DOI] [PubMed] [Google Scholar]
- 52.Lautt WW. Hepatic nerves – a review of their functions and effects. Can J Physiol Pharmacol. 1980;58:105–23. doi: 10.1139/y80-019. [DOI] [PubMed] [Google Scholar]
- 53.Solis-Herruzo JA, Duran A, Favela V. Effect of lumbar sympathetic block on kidney function in cirrhotic patients with hepatorenal syndrome. J Hepatol. 1987;5:167–73. doi: 10.1016/s0168-8278(87)80569-x. [DOI] [PubMed] [Google Scholar]
- 54.Abraham WT, Lauwaars ME, Kim JK, Pena RL, Schrier RW. Reversal of atrial natriuretic peptide resistance by increasing distal tubular sodium delivery in patients with decompensated cirrhosis. Hepatology. 1995;22:737–43. [PubMed] [Google Scholar]
- 55.Koepke JP, Jones S, DiBona GF. Renal nerves mediate blunted natriuresis to atrial natriuretic peptide in cirrhotic rats. Am J Physiol. 1987;252:R1019–23. doi: 10.1152/ajpregu.1987.252.5.R1019. [DOI] [PubMed] [Google Scholar]
- 56.Rodriguez-Martinez M, Sawin LL, DiBona GF. Arterial and cardiopulmonary baroreflex control of renal nerve activity in cirrhosis. Am J Physiol. 1995;268:R117–29. doi: 10.1152/ajpregu.1995.268.1.R117. [DOI] [PubMed] [Google Scholar]
- 57.Levy M, Wexler MJ. Renal sodium retention and ascites formation in dogs with experimental cirrhosis but without portal hypertension or increased splanchnic vascular capacity. Lab Clin Med. 1978;91:520–36. [PubMed] [Google Scholar]
- 58.Liang CC. The influence of hepatic portal circulation on urine flow. J Physiol. 1977;214:571–81. doi: 10.1113/jphysiol.1971.sp009449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bosch B, Garcia-Pagan CG. Complication of cirrhosis. I. Portal hypertension. J Hepatol. 2000;32 (Suppl 1):141–56. doi: 10.1016/s0168-8278(00)80422-5. [DOI] [PubMed] [Google Scholar]
- 60.Kawasaki T, Moriyasu F, Kimura T, et al. Hepatic function and portal hemodynamics in patients with liver cirrhosis. Am J Gastroenterol. 1990;85:1160–4. [PubMed] [Google Scholar]
- 61.Niijima A. An electrophysiological study on hepatovisceral reflex: the role played by vagal hepatic afferents from chemosensors in the hepatoportal region. In: Haussinger D, Jungermann K, editors. Liver and Nervous System. London: Kluwer Academic Publishers; 1998. pp. 159–72. [Google Scholar]
- 62.Vandier C, Conway AF, Landauer RC, Kumar P. Presynaptic action of adenosine on a 4-aminopyridine-sensitive current in the rat carotid body. J Physiol. 1999;515:419–29. doi: 10.1111/j.1469-7793.1999.419ac.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thames MC, Kinugawa T, Dibner-Dunlap ME. Reflex sympathoexcitation by cardiac sympathetic afferents during myocardial ischemia: role of adenosine. Circulation. 1993;87:1698–704. doi: 10.1161/01.cir.87.5.1698. [DOI] [PubMed] [Google Scholar]
- 64.Montano N, Lombardi F, Ruscone TG, Contini M, Guazzi M, Malliani A. The excitatory effect of adenosine on the discharge activity of the afferent cardiac sympathetic fibers. Cardiologia. 1991;36:953–9. [PubMed] [Google Scholar]
- 65.O’Beirne JP, Chouhan M, Hughes RD. The role of infection and inflammation in the pathogenesis of hepatic encephalopathy and cerebral edema in acute liver failure. Nat Clin Pract Gastroenterol Hepatol. 2006;3:118–19. doi: 10.1038/ncpgasthep0417. [DOI] [PubMed] [Google Scholar]
- 66.O’Grady JG. Acute liver failure. Postgrad Med J. 2005;81:148–54. doi: 10.1136/pgmj.2004.026005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rolando N, Wade J, Davalos M, Wendon J, Philpott-Howard J, Williams R. The systemic inflammatory response syndrome in acute liver failure. Hepatology. 2000;32:734–9. doi: 10.1053/jhep.2000.17687. [DOI] [PubMed] [Google Scholar]
- 68.Bontemps F, Vincent MF, Van-den-Berghe G. Mechanisms of elevation of adenosine levels in anoxic hepatocytes. Biochem J. 1993;290:671–7. doi: 10.1042/bj2900671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lautt WW, Macedo MP. Nitric oxide and hepatic circulation. In: Kadowitz PJ, McNamara DB, editors. Nitric Oxide and the Regulation of the Peripheral Circulation. Boston: Birkhauser; 2000. pp. 243–58. [Google Scholar]
- 70.Ming Z, Han C, Lautt WW. Nitric oxide mediates hepatic arterial vascular escape from norepinephrine-induced constriction. Am J Physiol. 1999;277:G1200–6. doi: 10.1152/ajpgi.1999.277.6.G1200. [DOI] [PubMed] [Google Scholar]
- 71.Lautt WW, Legare DJ. Adenosine modulation of hepatic arterial but not portal venous constriction induced by sympathetic nerves, norepinephrine, angiotensin, and vasopressin in the cat. Can J Physiol Pharmacol. 1986;64:449–54. doi: 10.1139/y86-072. [DOI] [PubMed] [Google Scholar]
- 72.Lautt WW, Schafer J, Legare DJ. Effect of adenosine and glucagon on hepatic blood volume responses to sympathetic nerves. Can J Physiol Pharmacol. 1991;69:43–8. doi: 10.1139/y91-007. [DOI] [PubMed] [Google Scholar]
- 73.Wang H, Lautt WW. Does nitric oxide (NO) trigger liver regeneration? Proc West Pharmacol Soc. 1997;40:17–18. [PubMed] [Google Scholar]
- 74.Michalopolous GK, DeFrances MC. Liver regeneration. Science. 1997;276:60–6. doi: 10.1126/science.276.5309.60. [DOI] [PubMed] [Google Scholar]
- 75.Macedo MP, Lautt WW. Shear-induced modulation of vasoconstriction in the hepatic artery and portal vein by nitric oxide. Am J Physiol. 1998;274:G253–60. doi: 10.1152/ajpgi.1998.274.2.G253. [DOI] [PubMed] [Google Scholar]
- 76.Wang H, Lautt WW. Hepatocyte primary culture bioassay –a simplified tool to assess the initiation of the liver regeneration cascade. J Pharmacol Toxicol Methods. 1997;38:141–50. doi: 10.1016/s1056-8719(97)00079-8. [DOI] [PubMed] [Google Scholar]
- 77.Wang H, Lautt WW. Evidence of nitric oxide, a flow-dependent factor, being a trigger of liver regeneration in rats. Can J Physiol Pharmacol. 1998;76:1072–9. doi: 10.1139/cjpp-76-12-1072. [DOI] [PubMed] [Google Scholar]
- 78.Moser MJ, Gong Y, Zhang MN, et al. Immediate-early oncogene expression and liver function following varying extents of partial hepatectomy in the rat. Dig Dis Sci. 2001;46:907–14. doi: 10.1023/a:1010791915733. [DOI] [PubMed] [Google Scholar]
- 79.Schoen JM, Wang HH, Minuk GY, Lautt WW. Shear stress-induced nitric oxide release triggers the liver regeneration cascade. Nitric Oxide. 2001;5:453–64. doi: 10.1006/niox.2001.0373. [DOI] [PubMed] [Google Scholar]
- 80.Schoen Smith JM, Lautt WW. The role of prostaglandins in triggering the liver regeneration cascade. Nitric Oxide. 2005;13:111–17. doi: 10.1016/j.niox.2005.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sato Y, Koyama S, Tsukada K, Hatakeyama K. Acute portal hypertension reflecting shear stress as a trigger of liver regeneration following partial hepatectomy. Surg Today. 1997;27:518–26. doi: 10.1007/BF02385805. [DOI] [PubMed] [Google Scholar]
- 82.Eguchi S, Yanaga K, Sugiyama N, Okudaira S, Furui J, Kanematsu T. Relationship between portal venous flow and liver regeneration in patients after living donor right-lobe liver transplantation. Liver Transpl. 2003;9:547–51. doi: 10.1053/jlts.2003.50128. [DOI] [PubMed] [Google Scholar]