Abstract
Young people who receive Medicaid-funded mental health services during the transition to adulthood often face disenrollment from Medicaid without continuity into publicly-funded services. This paper investigates the longitudinal predictors of these coverage gaps and disenrollment from age 16 to 23. Cox regression analyses estimated predictors of time until the first loss of coverage for 180 days or more, and time until final disenrollment with no subsequent reenrollment. Females were much more likely to regain and retain coverage after initial loss. Funding source and diagnoses predicted Medicaid retention differentially by gender. For both genders, funding through SSI or a diagnosis of MR/DD was related to Medicaid retention. Disenrollment especially impacted males precisely at their 18th and 19th birthdays. Nearly one-third of females qualified for Medicaid due to pregnancy. Eligibility guidelines relate to retention and loss during the transition to adulthood and may need reevaluation to ensure continuity of care.
Keywords: Medicaid, mental health, disability, gender/sex differences, transition to adulthood
Introduction
Insurance coverage, and specifically Medicaid, plays a critical role for adolescents to access both the mental and physical health care systems. More than one in four youth are insured through Medicaid or the related State Children’s Health Insurance Programs (SCHIP) (Kaiser Commission on Medicaid and the Uninsured, 2003). Medicaid pays for services and supports that are a crucial part of the social safety net for those with special needs, including adolescents with mental health problems. In 2003, public spending on mental health and substance abuse direct treatment totaled $100 billion, and Medicaid accounted for 26% of all mental health funding (Mark et al., 2007). However, eligibility criteria are inconsistent among the various sources of access to Medicaid, and this may result in the loss of Medicaid funding during late adolescence and young adulthood due to age-specific eligibility criteria. As a result, youth who receive mental health services during the transition to adulthood often face disenrollment from Medicaid without continuity into publicly-funded adult services. The difficulties of transitioning to adulthood for youth with mental health problems have been well documented (Clark & Davis, 2000). They must navigate the transition from child to adult systems while struggling with serious mental or behavioral health issues (Davis, 2003; Diaz et al., 2004), often facing the end of publicly-funded supportive services before they are developmentally prepared to function as adults (Mallory, 1995).
Lack of Insurance and Gaps in Medicaid Enrollment
Insurance coverage – or lack thereof – is not distributed equally. Hispanic and African-American children are more likely to be uninsured, and are more likely to use Medicaid or SCHIP, when compared to whites (Kaiser Commission on Medicaid and the Uninsured, 2008). More than twice the number of young adults as adolescents are without insurance coverage of any kind—eight million young adults (aged 19 to 25) lack coverage compared to four million adolescents (aged 10 to 18). The deficit of insurance coverage among this age group may be explained by their inability to maintain eligibility for public insurance, combined with a lack of employment opportunities that provide private insurance (Lawrence, Gootman, & Sim, 2008).
Insurance disruption is associated with less access to care, less care utilization, and greater unmet medical need (Federico, Steiner, Beaty, Crane, & Kempe, 2007). Youth disenroll from public insurance in four ways: they become ineligible for coverage, they are administratively disenrolled due to ending coverage periods (though they remain eligible), they obtain private coverage, or they withdraw despite continued eligibility (Sommers, 2005). Around 45% of children lose Medicaid or SCHIP coverage despite continued eligibility and lack of alternative coverage (Sommers, 2005). Many who lose coverage are likely to reenroll; Medicaid coverage patterns for children in five states reveal that, over a two-year period, 16–41% had multiple periods of disenrollment (Fairbrother, Emerson, & Partridge, 2007). Gaps in Medicaid enrollment over time occur for various reasons, such as caseworker or caregiver neglect.
There are several demographic characteristics of children and their families that may contribute to increased risk of disenrollment. For example, even though one study found that African-Americans are the least likely to lose eligibility for Medicaid (Sommers, 2005), another study found that African-American children have higher than average rates of disenrollment from SCHIP, a form of public health insurance for needy children (Philips, Miller, Cantro, & Gaboda, 2004). Gender also plays a role in Medicaid enrollment, particularly for older youths. At younger ages, differences between males and females in enrollment have been small (Philips et al., 2004). At the age of transition out of child public assistance, females are more likely to meet income requirements, and clearly more likely to meet pregnancy or motherhood requirements than males (Kaiser Commission on Medicaid and the Uninsured, 2007). Thus, there is a widening in the gender gap in Medicaid at transition ages.
Rural communities are of special concern. Rural children are more likely to be uninsured when compared to urban children at any single point in time, and are more likely to be uninsured for longer periods of time (Coburn, McBride, & Ziller, 2002). Rural youth are affected by multiple factors, such as poverty, transportation problems, stigma of seeking service, lack of available services, and inadequate access to physicians (Hartley, 2004; McCabe et al., 1999; Ricketts, 1999) that serve as barriers to the use of behavioral health services (Starr, Campbell, & Herrick, 2002) and to enrollment in Medicaid programs (Coburn et al., 2002). Medicaid rules are also primarily implemented at the community level as youth and their families enroll through and interact with local child welfare personnel.
New Contribution
Medicaid coverage serves a vital function in providing services to populations who lack health insurance or to populations with unique needs. The studies above indicate that lack of enrollment and gaps in enrollment can have detrimental effects on access to health care and service utilization. Gaps in enrollment may be related to demographic and systemic variables, including gender, race, age, and rurality. Additionally, certain subpopulations, such as youth with mental health problems transitioning to adulthood, seem to be at a heightened risk of Medicaid loss. However, research on Medicaid retention is lacking specifically in regards to youth who received mental health services during the transition to adulthood. Little is known about the variables related to disenrollment in this population.
This study goes beyond previous studies which had focused on physical health, by exploring and describing the course of Medicaid retention and gaps in coverage for people who received a Medicaid-funded mental health service in adolescence. Additionally, this paper examines the predictors of gaps in Medicaid enrollment and disenrollment for adolescents with mental health problems. Within this framework, we focused in particular on: 1) exploring gender differences in interruptions in enrollment and ultimate disenrollment, 2) discovering the proportion of youth who retained coverage into adulthood, 3) uncovering periods during which youth are at a higher risk of disenrollment, and 4) documenting individual and community factors associated with disenrollment.
Conceptual Framework
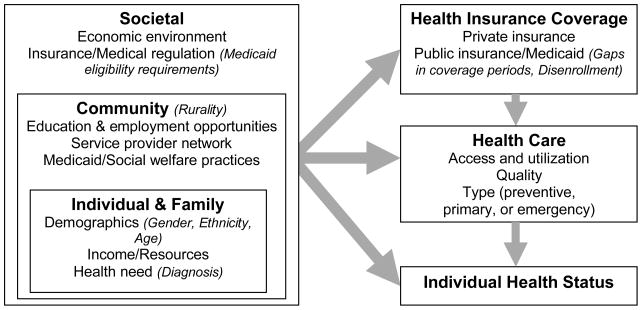
Figure 1 depicts our overall conceptual framework for factors related to insurance coverage, and the relationship of health care utilization and health status with health insurance coverage, including gaps and discontinuity in coverage. Our paper addresses a subset of this more comprehensive framework—italicized items in Figure 1 are variables we used in our analyses. Factors associated with lack of health insurance coverage span individual, family, community, and societal levels, from insurance eligibility requirements to availability of services to individual resources and need. Our paper addresses variables related to several of these, although we recognize that a comprehensive examination of this topic reaches far beyond the factors depicted in Figure 1 or the variables available to us.
Figure 1.
Conceptual Framework for Factors Related to Insurance Coverage
Societal factors are believed to impact health insurance, access, and individual health status through the economic environment and insurance regulation. We include in our analyses one variable representing a primary factor, Medicaid eligibility requirements, because this is a major factor determining which societal subpopulations receive publicly-funded medical care. Community factors relating to health insurance, access, and health status include economic opportunities, service provider networks, and local health practices. Our analyses use rurality as an indicator of these factors, based on its empirically established relationships to them, as described above. Family and individual factors such as income, need, and demographics are clearly related to health insurance, health care, and health status, as discussed above. At this level, our analyses include demographics (race/ethnicity, gender, and age) and need for mental health care as indicated by psychiatric diagnosis.
These societal, community, and individual level factors are hypothesized to impact health status, health care receipt, and health insurance coverage, measured in our study as gaps in Medicaid and final loss of Medicaid. Ultimately, this is important because of what is detailed in the rest of the Conceptual Framework. As has been the center of recent and ongoing health care reform discussion, the lack of health insurance coverage poses a critical barrier to accessing appropriate care in a timely manner. The research we describe above indicates that this often results in lack of preventive care, overreliance on emergency services, high levels of unmet medical need, and a negative impact on health status. Hence, this framework reveals the importance of investigating the individual and community factors related to disenrollment from Medicaid.
Methods
Context of the Study
This secondary analysis used data from Mississippi. Mississippi is one of a few states with more than 15% of children uninsured (Kaiser Commission on Medicaid and the Uninsured, 2008), and this state covers more than 12% of its children through Medicaid (Kaiser Commission on Medicaid and the Uninsured, 2003). Mississippi’s insurance statistics reflect the racial disparities in Medicaid coverage. While 44% of the children in Mississippi are African-American, 76% of the children on Medicaid are African-American (Saunders & Heflinger, 2004). About 30% of the children in Mississippi live in poverty, and 45% of Mississippi children live in single-parent households. Approximately eight percent of Mississippi Medicaid children and adolescents use mental or behavioral health services (Saunders & Heflinger, 2004).
Datasets
The data for the current study are drawn from the Mississippi Division of Medicaid from 1993 to 2005. Enrollment files supplied information on youth demographic characteristics, Medicaid eligibility categories and periods of eligibility, and county of residence. Claims data were used to extract information on date and type of service, with mental health service use determined by a combination of diagnosis and service type. These data have been used in previously published research (e.g. Saunders & Heflinger, 2004, 2005).
Sample
This longitudinal study examines the Medicaid enrollment periods for a total sample of 6,471 people, consisting of 3,105 females (48%) and 3,366 males (52%). This sample represents all youth who: a) were born from July of 1977 through December of 1982, b) were currently enrolled in Medicaid at their 16th birthday, c) received a Medicaid-funded mental-health related service when 15 or 16 years old, d) received a mental health diagnosis at some point during their Medicaid coverage period, and e) had not solely been diagnosed with mental retardation, developmental disabilities, or a substance use disorder. The last group was excluded primarily because the authors were most interested in examining the population of those diagnosed with mental health related problems, however youth with mental retardation or developmental disabilities in addition to mental health related problems are included. People with developmental disorders and mental retardation are a unique group and exploratory analyses revealed they rarely lost coverage. Individuals had to be enrolled at their 16th birthday because we were interested in the timeframe of transition to adulthood, often considered to start at age 16 (Davis, 2003), and our approach to analyses, described below, required a single starting age-point. This is because we were interested in age- and time- related effects rather than simply time-related effects. All cases were restricted to a study period of 7.5 years after their 16th birthday, placing the last data point when individuals were 23.5 years old. This maximized the possible timeframe based on when we obtained the data, while ensuring all cases had an equal observation period. Table 1 presents descriptive information for this sample, stratified by gender. Pearson chi-square tests emphasize variables on which the genders differed.
Table 1.
Descriptive Information Cross-Tabulated by Gender (N = 6,471)
| Variable | Female Percentage (n=3,105) | Male Percentage (n=3,366) | Total Percentage (n=6,471) |
|---|---|---|---|
| Total percentage of sample | 48 | 52 | 100 |
| Race** | |||
| African American | 65.5 | 67.4 | 66.5 |
| White | 28.9 | 29.9 | 29.4 |
| Other or missing | 5.5 | 2.6 | 4.0 |
| Rural residence | 71.2 | 69.2 | 70.2 |
| Diagnosis any time, 15+ | |||
| Major depressive disorder** | 23.9 | 17.1 | 20.4 |
| Bipolar | 5.2 | 6.0 | 5.6 |
| Schizophrenia | 5.9 | 6.9 | 6.4 |
| Borderline** | 2.2 | 0.4 | 1.3 |
| Attention deficit/hyperactivity disorder** | 7.4 | 23.0 | 15.5 |
| Conduct disorder/oppositional defiant disorder** | 28.3 | 38.1 | 33.4 |
| Substance abuse disorders** | 9.0 | 16.9 | 13.1 |
| Mental retardation/developmental disability** | 7.7 | 11.6 | 13.1 |
| Other only (none of the above)** | 43.1 | 26.5 | 34.5 |
| Ever eligible for Medicaid, 15+ through | |||
| Foster care** | 8.8 | 5.5 | 7.1 |
| Supplemental security income** | 35.8 | 59.0 | 47.9 |
| Aid to families with dependent children/temporary assistance for needy families** | 63.6 | 43.1 | 52.9 |
| Medical assistance to families** | 21.5 | 7.4 | 14.2 |
| Pregnant women, 133% or 185% of poverty | 32.1 | -- | 15.4 |
| Children under 19 years* | 12.0 | 9.6 | 10.6 |
Note: Total for diagnosis and eligibility adds to more than 100% because multiple categories are possible.
p < .01;
p < .001 (Pearson chi-square analyses between genders).
Measures
Dependent variables
The primary dependent variable was time from age 16 until final disenrollment from Medicaid with no subsequent reenrollment. The secondary dependent variable was time until disenrollment from Medicaid for at least 180 days before a subsequent reenrollment, if any. We chose this 180-day-or-more gap in coverage rather than some other number of days for theoretical and empirical reasons. Small gaps of coverage of a few months are often related to changing eligibility categories, with little or no practical loss of services. Hence, we considered these gaps to be of less interest. Empirically, there was a steep decline in the proportion of people who lost coverage and then reenrolled at 180 days or more. Overall, 47% of people lost coverage for 31 days or more and then regained it, compared to 32.4% for 180 days or more and 32.1% for 365 days or more.
Independent variables
Independent variables included gender, race (African-American, White, Other/Missing), rural residence, several Medicaid eligibility categories, and several psychiatric diagnosis categories. Age is an indirect variable, treated as a function of time in our approach to analysis. Rurality was defined by the county in which the person was recorded as living at the time nearest their last eligibility period. The Rural-Urban Commuting Area (RUCA) Codes (Version 2.0) were used to classify counties in Mississippi (WWAMI Rural Health Research Center, 2006). The RUCAs combine the Bureau of Census Urbanized Area and Urban Cluster definitions with information on work commuting (United States Department of Agriculture Economic Research Service, 2004). Since this study used county as the level of analysis, the county conversion was used (Washington State Department of Health, 2006) and then dichotomized (1 = rural, 0 = not rural), corresponding with RUCA Categorization C (WWAMI Rural Health Research Center, 2006).
The Medicaid eligibility categories included being enrolled through foster care, Social Security Income (SSI), Aid to Families with Dependent Children (AFDC), Temporary Assistance for Needy Families (TANF), Medical Assistance for Families, and children under 19 years. Combined into one category were “pregnant women at less than 133% of the poverty level” and “pregnant women at less than 185% of the poverty level.” It should be emphasized that the “pregnant women” category is a conservative estimate of the number of females in the study who became pregnant, as pregnant women could also qualify for Medicaid under one of three other categories. Other eligibility categories made up a total of less than 5% of the overall eligibility periods for less than 3% of the population, so these were not included in this analysis.
Eligibility requirements were hypothesized to have a relationship to loss of coverage. The most salient requirements for this study are as follows. For all categories except foster care, families or young adults were required to be categorized as having “limited income” (as determined by the state) or to be some proportion of the “need” or poverty standard. For AFDC in Mississippi in 1996, a family of three could have an income no greater than 185% of the need standard, which was $681 a month. Other income limitations also applied, depending on the eligibility category. Age requirements also applied to several categories. AFDC and TANF covered families with children under 18 years of age, or 19 with an optional state extension. Since SSI required that the person be disabled, the age requirement was directly related to the definition of disability. For SSI, people under 18 were to have marked and severe functional limitations, while people over 18 were to have functional limitations that resulted in the inability to do any substantial gainful activity. Being qualified under “Child under 19 years” was a poverty-eligible program with a clear age requirement of being under 19. Being eligible under foster care required being in the custody of child welfare, without any specified age standard. Medical assistance for families was a large subcategory of AFDC and TANF, with the same eligibility requirements but focused on providing medically related assistance.
Individuals’ eligibility categories changed with relative frequency, often seamlessly month to month. Due to the difficulty of modeling time-dependent categorical variables through this extended dataset, eligibility category was included in the analysis as static variables indicating whether the individual ever qualified through that category from age 15 through the end of the study (e.g. “ever qualified through SSI”). This resulted in each eligibility category being treated as its own dichotomous variable, and the proportion of people qualifying through the total collection of categories add to more than 100%.
Individuals had been diagnosed by credentialed staff during the course of treatment from age 15 through the end of the study, and the diagnosis was submitted in Medicaid billings. Diagnostic categories included Major Depressive Disorders, Bipolar Disorder, Schizophrenia, Borderline Personality Disorder, Attention Deficit Disorder/Attention Deficit Hyperactivity Disorder (ADD/ADHD), Conduct Disorder/Oppositional Defiant Disorder (CD/ODD), Substance Abuse Disorders, and Mental Retardation/Developmental Disabilities (MR/DD). Individuals could receive multiple diagnoses over the course of the study. A category of “Other” was created for those who were not diagnosed with any of the categories above but who did receive a mental health diagnosis.
Analysis
Crosstabulations with chi-square tests were used to test for gender differences in the proportion of those who were reenrolled in Medicaid within 180 days after the first disenrollment, compared to those who were not reenrolled. Next, two Kaplan-Meier time-to-event analyses were run testing for gender differences in 1) the time from 16th birthday until the first 180-day gap in coverage and 2) the time from 16th birthday and final disenrollment with no subsequent reenrollment. The Kaplan-Meier survival analysis technique is analogous to an ANOVA for comparing groups on a dependent variable, (in this case, time until disenrollment), except it can account for right-censored data, or data partially missing due to an event that had not occurred or the loss of the participant from the dataset (Hosmer & Lemeshow, 2000; Singer & Willett, 2003). This allows the participant’s data to be included in the analysis for calculating the proportional chance of the event occurring up to the day censored. In our dataset, participants were censored when they died or when the study window ended without disenrollment. The dataset did not indicate those who moved out of state.
Third, after the analysis above established that there were strikingly different trends for the genders on time until disenrollment, we chose to explore possible predictors of these trends stratified by gender. Hence, two Cox Regression time-to-event analyses were run examining the time until first disenrollment of 180 days or more, one for females and one for males. Two additional analyses were run predicting time until final disenrollment for females and males. Cox Regression time-to-event analysis is analogous to multiple regression in that it can account for the predictive value of several covariates on a dependent variable (in this case, time until disenrollment), however, it allows for right-censored data (Hosmer & Lemeshow, 2000; Singer & Willett, 2003). Race was included as a categorical variable with a deviation contrast so Whites and African-Americans were compared to the overall effect of all racial categories and “Other/missing” was excluded from testing. All other categorical variables were included in the model with an indicator contrast, meaning their respective absence was the referent category (e.g. Bipolar vs. Not-Bipolar). Since the goal of this study was an exploratory examination of the possible predictors of disenrollment, as opposed to building the most parsimonious model for the data, all variables were left in the final model regardless of statistical significance.
Results
Comparison of Females and Males
The first analysis addressed gender differences in reenrollment in Medicaid after 180-day gaps in coverage. Six times as many women as men were reenrolled after a loss of coverage lasting 180 days or more. Only 8.5% of males were reenrolled after loss, whereas 52.6% of females were reenrolled at least once, and some women were reenrolled up to four times, χ2(4, N = 6471) = 1,550, p < .001.
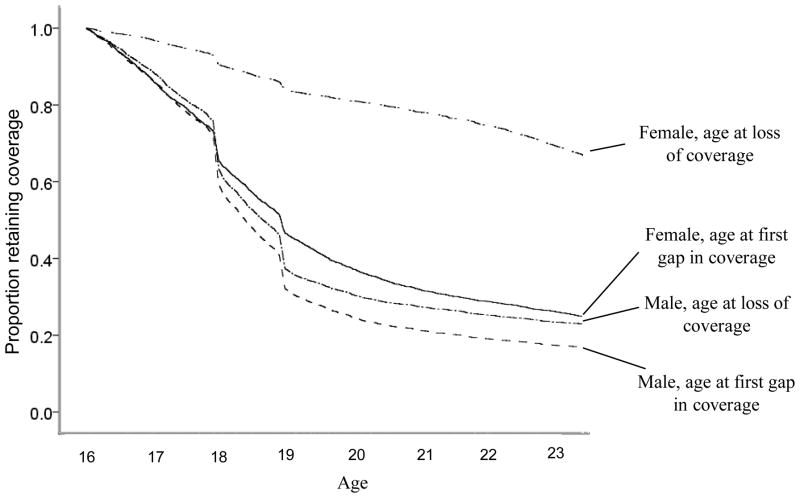
Two Kaplan-Meier time-to-event analyses were run comparing males to females, one for the time until the first disenrollment for 180 days or more, and the second for time until final disenrollment with no subsequent reenrollment. For ease of interpretation, Figure 2 combines the four time-to-event empirical curves for these two analyses. By the end of the 7.5 year study period, 75% of females had lost coverage for 180 days or more, compared to 83% of the males (Log Rank χ2(1, N = 6471) = 88.2, p < .001). Females took longer to be disenrolled, on average; the median number of days of coverage between age 16 and the first disenrollment was 1,074 for females, compared to 877 days for males.
Figure 2.
Years from 16th Birthday until 180-day Gap in Coverage or End of Coverage for Males and Females
The results for the second set of Kaplan-Meier analyses, which compared time until final disenrollment, were dramatic. Males lost coverage earlier and were less likely to regain coverage than females (Log Rank χ2(1, N = 6471) = 1,595, p < .001). By the end of the study, 33% of females had been disenrolled without subsequent reenrollment, compared to 77% of males. The median number of days until final disenrollment for females was greater than 2,734 (the precise median could not be calculated because at least half of the females did not lose coverage), compared to 974 days for males.
The lines in Figure 2 illustrate more than the simple comparisons described above. Large numbers of disenrollments occurred approximately on the participants’ 18th and 19th birthday. Males were disproportionately disenrolled at these ages. When only including in the analysis those people who were disenrolled without subsequent reenrollment, 28% of males were permanently disenrolled on their 18th or 19th birthday, compared to 14% of females, χ2(1, n = 3609) = 82.2, p < .001.
Cox Regression for Females
The final model for the Cox regression predicting the number of days until first disenrollment for 180 days or more is depicted in Table 2. This table illustrates the hazard ratio, which is an estimate of the effect size of the predictor and can be interpreted similar to relative risk. The hazard ratio can be thought of as the odds that an individual with that characteristic will be disenrolled compared to individuals without that characteristic, when controlling for other factors in the model. Hence, hazard ratios above 1.0 represent increased risk of disenrollment, hazard ratios below 1.0 represent decreased risk of disenrollment. As with odds ratios, the magnitude of the HR becomes increasingly strong as the HR falls below zero, so that an HR of .5 (i.e. 0.5:1) is equivalent to an HR of 2.0 (i.e. 2:1), but an HR of .25 (i.e. 0.25:1) is equivalent to an HR of 4.0 (i.e. 4:1).
Table 2.
Cox Regressions Predicting Time until First Loss of Coverage for 180 or More Days for Males and Females
| Females | Males | |||
|---|---|---|---|---|
| Hazard Ratio | p | Hazard Ratio | p | |
| Racea | ||||
| White | 1.098 | .019 | 1.154 | .004 |
| African-American | .785 | <.001 | 1.024 | .614 |
| Rural Countyb | .923 | .088 | .951 | .232 |
| Diagnosisb | ||||
| Major Depressive | 1.042 | .543 | .978 | .694 |
| Bipolar | .962 | .742 | .946 | .531 |
| Schizophrenia | .749 | .024 | .596 | <.001 |
| Attention Deficit/Hyperactivity Disorder | .977 | .810 | 1.121 | .040 |
| Conduct Disorder/Oppositional Defiant Disorder | .985 | .823 | 1.067 | .209 |
| Substance Use | 1.138 | .106 | 1.102 | .079 |
| Mental Retardation/Dev. Disability | .495 | <.001 | .396 | <.001 |
| Other only | 1.110 | .174 | 1.029 | .659 |
| Eligibility categoryb | ||||
| Foster care | .890 | .133 | .597 | <.001 |
| Supplemental Security Income | .338 | <.001 | .191 | <.001 |
| Pregnancy, <185% of poverty | 1.362 | <.001 | - | - |
| Med. Assistance to Families | .933 | .160 | .951 | .485 |
| Aid to Families with Dependent Children/Temporary Assistance for Needy Families | .910 | .128 | 1.406 | <.001 |
| Child under 19 | 1.093 | .142 | .341 | <.001 |
| Model Statistics | ||||
| χ2 statistic | 932 | 424 | ||
| df | 17 | 16 | ||
| Model significance | <.001 | <.001 | ||
| −2 Log Likelihood | 33684 | 41290 | ||
Race included as a deviation contrast, with each category compared to the overall effect of race including “other” and “missing” race
Included as indicator contrast, with their respective absence as indicator category
The significant predictors with the largest effect size were SSI (HR = .338, p < .001) and MR/DD (HR = .495, p < .001), both of which were associated with a lengthened time until first disenrollment. Also associated with a lengthened time were being diagnosed with Schizophrenia (HR = .749, p =.024) and being African-American (HR = .785, p < .001). Being eligible through pregnancy at less than 185% of poverty (HR = 1.362, p <.001) and being White (HR = 1.098, p = .019) were associated with a shortened time until first disenrollment. When controlling for all variables in the model, rurality was not statistically significant.
The final model for the Cox regression predicting the number of days until final disenrollment for females is depicted in Table 3. Again, the most important predictors of time to disenrollment were SSI (HR =.372, p < .001) and MR/DD (HR = .511, p <.001), both of which were associated with a lengthened time until disenrollment. Being White was the next strongest factor (HR 1.771, p =.004), and it was associated with a shortened time until disenrollment. Being eligible through pregnancy at less than 185% of poverty (HR = .634, p = .634) or through AFDC/TANF (HR =.641, p <.001) were both associated with a lengthened time until disenrollment. The final significant variable was being diagnosed with ADD/ADHD (HR = 1.363, p = .015), which was associated with a shortened time until disenrollment. When controlling for all variables in the model, rurality was not statistically significant.
Table 3.
Cox Regressions Predicting Time until Final Loss of Coverage for Males and Females
| Females | Males | |||
|---|---|---|---|---|
| Hazard Ratio | p | Hazard Ratio | p | |
| Racea | ||||
| White | 1.771 | <.001 | 1.048 | .356 |
| African American | 1.066 | .373 | 1.031 | .540 |
| Rural Countyb | .949 | .448 | .998 | .964 |
| Diagnosisb | ||||
| Major Depressive | 1.049 | .617 | 1.046 | .448 |
| Bipolar | 1.143 | .392 | .884 | .190 |
| Schizophrenia | .729 | .093 | .524 | <.001 |
| Attention Deficit/Hyperactivity Disorder | 1.363 | .015 | 1.236 | <.001 |
| Conduct Disorder/Oppositional Defiant Disorder | 1.093 | .356 | 1.095 | .093 |
| Substance Use | 1.224 | .072 | 1.060 | .323 |
| Mental Retardation/Dev. Disability | .511 | <.001 | .377 | <.001 |
| Other only | 1.024 | .830 | 1.031 | .649 |
| Eligibility categoryb | ||||
| Foster care | .894 | .314 | .583 | <.001 |
| Supplemental Security Income | .372 | <.001 | .152 | <.001 |
| Pregnancy, <185% of poverty | .634 | <.001 | - | - |
| Med. Assistance to Families | 1.101 | .189 | .803 | .003 |
| Aid to Families with Dependent Children/Temporary Assistance for Needy Families | .641 | <.001 | 1.032 | .658 |
| Child under 19 | .971 | .750 | .359 | <.001 |
| Model Statistics | ||||
| χ2 statistic | 250 | 2168 | ||
| df | 17 | 16 | ||
| Model significance | <.001 | <.001 | ||
| −2 Log Likelihood | 15668 | 36839 | ||
Race included as a deviation contrast, with each category compared to the overall effect of race including “other” and “missing” race
Included as indicator contrast, with their respective absence as indicator category
Comparing the model for the time until first disenrollment for 180 days or more to the model for the time until the final enrollment, we see a few similarities and differences. SSI and MR/DD are the major predictors in both models, associated with a lengthened time until loss of eligibility. Being White was associated with a shortened time until disenrollment in both models, but it had a much weaker effect for first disenrollment. Schizophrenia had a strong relationship to retention of enrollment in both models. ADD/ADHD was a significant predictor of disenrollment only for the final loss of services. Interestingly, being eligible through pregnancy at less than 185% of poverty level was associated with a shortened time until first disenrollment, but a lengthened time until final loss of eligibility.
Cox Regression for Males
The regression models for males predicting the number of days until first disenrollment for 180 days or more are also depicted in Table 2. In order of effect size, the variables that were significantly related to a lengthened time until first disenrollment were being eligible through SSI (HR = .191, p <.001) or as a child under 19 years (HR = .341, p < .001), being diagnosed with MR/DD (HR = .396, p < .001) or Schizophrenia (HR =.596, p < .001), and being eligible through foster care (HR = .597, p < .001). Variables associated with a shortened time until first disenrollment included being eligible through AFDC/TANF (HR = 1.406, p < .001), being White (HR = 1.154, p = .004), and being diagnosed with ADD/ADHD (HR = 1.121, p = .04). When controlling for all variables in the model, rurality was not statistically significant.
Variables associated with a lengthened time until final disenrollment, in order of effect size, included being eligible for services through SSI (HR = .152, p <.001) or as a child under 19 years (HR = .359, p < .001), being diagnosed with MR/DD (HR = .377, p <.001) or Schizophrenia (HR = .524, p < .001), and being eligible for services through foster care (HR = .583, p < .001) or Medical Assistance to Families (HR = .803, p = .003). Being diagnosed with ADD/ADHD was associated with a shortened time until disenrollment (HR = 1.236, p < .001). Being eligible through SSI had an extremely strong effect size, indicating that those who were eligible through SSI had an odds of coverage loss that were 85% less than those who were not eligible through SSI. The variables of eligibility as a child under 19 years, a mental retardation or developmental disability diagnosis, a Schizophrenia diagnosis, and being eligible through foster care were also all very strong predictors related to decreased odds of disenrollment. When controlling for all variables in the model, rurality was not statistically significant.
Since most males did not regain coverage after initial loss, the two models above were very similar. Being White was predictive of a shortened time until first disenrollment, but not final disenrollment. Being eligible through SSI and being diagnosed with MR/DD were the two strongest predictors of enrollment loss.
Discussion and Implications
Our study aimed to explore gender differences in interruptions in enrollment and ultimate disenrollment, discover the proportion of youth retaining coverage from 16 years of age into adulthood, uncover periods of heightened risk of disenrollment, and document individual and community factors related to disenrollment. We found that gender was a major predictor of loss of Medicaid coverage into adulthood among young adults with mental health problems. Although males were only slightly more likely to be disenrolled than females, females were much more likely to regain and retain coverage through the end of the study—six times as many women as men were reenrolled after a loss of coverage lasting 180 days or more. Women were also more likely to retain coverage into adulthood; by the end of the study, 33% of females were not enrolled, compared to 77% of males. There was some evidence that these findings were due to pregnancy and motherhood (discussed below), and it is possible that males were more likely to lose coverage in part due to incarceration, though this dataset did not allow this to be examined.
Other individual factors were also related to retention, including eligibility source and diagnoses. Ultimately, being eligible through SSI was the strongest predictor of retention for both males and females. Unsurprisingly, more severe diagnoses such as Schizophrenia, mental retardation, or developmental disabilities were also strongly related to retention of Medicaid coverage. In regards to race/ethnicity, our findings did not necessarily help clarify the contradictory existing literature regarding racial effects discussed above. White females were consistently more likely to be disenrolled when compared to African-Americans and other racial categories. White males were more likely to lose initial coverage. African-American females were less likely to experience first disenrollment. African-American males and females were not significantly different than other racial categories on time until final disenrollment.
We also found that there were heightened period of disenrollment. Aging-out of Medicaid coverage also appeared to be strongly related to disenrollment as there were significant periods of disenrollment near people’s 18th and 19th birthdays. Aging-out disproportionately impacted males, and because aging-out is directly tied to eligibility requirements, this is likely due to unequal rates of eligibility sources between the genders. Two sources stand out here, both related to motherhood. First, one-third of females were eligible through “pregnancy at less than 185% of poverty” at some point, which does not have an age requirement. Second, gender moderated the effect of AFDC/TANF coverage on retention. AFDC/TANF was significantly related to a decreased time until first disenrollment for males, and an increased time until last disenrollment for females. Again, it seems likely that this is related to motherhood. It may be that males are likely cut from Medicaid when they turn 18 or 19, because they may be more likely to be covered as the child in an AFDC/TANF-eligible family. (To be eligible for AFDC/TANF, the child in a family must be under the age of 18 or 19, depending on the state’s requirements.) Females, on the other hand, may be more likely to be eligible through 18 and 19 years of age because they may be covered as the parent of an AFDC/TANF-eligible family—females outnumber males as single parents more than five-to-one (U.S. Census Bureau, 2000), and female-headed households are more likely to be in poverty than male-headed households (Bangs, Lichtenwalter, Hughes, Anthou, & Shorter, 2004). SSI, with its looser rules on age requirements, may actually act to reduce the gender disparities in enrollment during the transition to adulthood, because males were more likely to be covered under SSI.
In terms of community factors and contrary to our expectations, rurality was unrelated to time until first or last disenrollment, implying that Medicaid is not implemented differently across rural and urban areas in terms of disenrollment in Mississippi’s system.
Policy implications
Many youth with mental health problems were disenrolled from Medicaid precisely on their 18th or 19th birthday. It is unlikely that this large group of youth simultaneously lose their need for these services on their birthday. Hence, the sweeping loss of coverage on these dates appears arbitrary, as it seems based on age-related eligibility requirements. Males were particularly vulnerable to disenrollment at these times, which is consistent with the fact that females are more likely to retain coverage due to eligibility sources without age requirements. This study reveals a need to rethink automatic ineligibility and disenrollment from Medicaid as a function of age (Ketsche et al., 2007). Davis and Koyanagi (2005) suggested that this population of youth with mental health problems needs continuity of care – not disrupted by disenrollment—from ages 14 to 30. Federal eligibility guidelines need re-evaluation, and states should consider their options to extend eligibility beyond the age criteria set by the federal Medicaid program.
Practice implications
For clinicians, social workers, case workers, and other mental health professionals, this study emphasizes the need to address the transition to adulthood and ensure continuity of care past the age of 18 and 19 for those young adults who need it. Treatment planning and case management needs to identify, track, and coordinate needs and resources as these youth move through this transition to adulthood (Hoffman, Heflinger, Athay, & Davis, 2009). An eighteenth birthday does not signify a change in mental health needs, as the currently bifurcated mental health system suggests. Further, we have shown that youth may already be parents well before their eighteenth birthday. Practitioners need to respond to these realities to serve this overlooked population.
Limitations and future research
The use of large existing databases provides an excellent opportunity for examining existing patterns of service use and, as in this study, issues regarding eligibility and enrollment. Changes in eligibility criteria and enrollment patterns should play an important role in evaluating health care reform efforts. Future research should aim for a more complete picture of the development of these individuals by incorporating additional data sources, specifically juvenile and adult justice, child welfare, employment, and physical and mental health records, to examine the relationship between Medicaid disenrollment and multi-system involvement. Also, it is important for future analyses to compare disenrollment patterns in the general Medicaid population with youth who have mental health problems to understand how mental illness affects Medicaid disenrollment during the age of transition. Finally, the somewhat inconsistent findings from existing research and our own data in regards to racial/ethnic differences should be clarified with additional research.
This research is limited in a few ways that warrant discussion. Since this research was conducted in one state, Mississippi, generalizability to other states is unsupported. Mississippi may have a unique system of Medicaid disenrollment and re-enrollment. These patterns can be influenced by systemic factors such as the number of caseworkers and the organization of paperwork or electronic records that may vary by state (Sommers, 2005). Additionally Mississippi is a relatively resource-poor state with relatively high proportions of uninsured children, high levels of racial disparities, high levels of teen pregnancy, and high levels of other health needs. However, while certain patterns of disenrollment are likely particular to state of residence and specific physical/mental disabilities, the federal eligibility guidelines in terms of age, disability, and type of need (specifically, pregnancy) are consistent enough across states that age- and gender-related disenrollment patterns could be expected to follow similar trends.
Another limitation is that the dataset did not follow youth as they moved outside of Mississippi. However, Mississippi’s rate of outmigration from 1995 to 2000, when the sample was reaching age of transition, was relatively low—Mississippi ranked 40th out of 51 in percentage of population outmigration (Franklin, 2003). Thus, while we expect that some disenrollment was due to outmigration, it is unlikely that enough youth left the state to significantly bias the results.
Additionally, most large administrative databases are limited by imprecise measures which may miss some of the most important factors in this work, including individual reasons why a youth lost coverage, and the experiences that families and youths had with the service system. Hence, the explanations for the existing patterns need a more grounded and qualitative approach to help identify additional areas of concern and opportunities for intervention. Longitudinal studies of health and other life events for youth at high risk of problems during the transition to adulthood are needed to understand the personal, family, and community factors that influence their enrollment.
Acknowledgments
The authors would like to acknowledge the support of the Mississippi Division of Medicaid in accessing the data used in this study. This research was supported by grants from the National Institute of Mental Health (R01 MH-70680); and National Institute on Drug Abuse (R21 DA017682). The opinions and conclusions presented are those of the authors and do not necessarily represent those of the funders or of the Mississippi Division of Medicaid.
Contributor Information
Michael D. Pullmann, Email: pullmann@u.washington.edu.
Craig Anne Heflinger, Email: c.heflinger@vanderbilt.edu.
Lindsay S. Mayberry, Email: lindsay.f.satterwhite@vanderbilt.edu.
References
- Bangs RS, Lichtenwalter S, Hughes S, Anthou C, Shorter C. Pittsburgh women’s benchmarks report. Pittsburgh, PA: University of Pittsburgh Center for Social and Urban Research; 2004. [Google Scholar]
- Clark HB, Davis M, editors. Transition to Adulthood: A Resource for Assisting Young People with Emotional or Behavioral Difficulties. Baltimore, MD: Paul H. Brookes; 2000. [Google Scholar]
- Coburn AF, McBride TD, Ziller EC. Patterns of health insurance coverage among rural and urban children. Medical Care Research and Review. 2002;59(3):272–292. doi: 10.1177/1077558702059003003. [DOI] [PubMed] [Google Scholar]
- Davis M. Addressing the needs of youth in transition to adulthood. Administration and Policy in Mental Health. 2003;30(6):495–509. doi: 10.1023/a:1025027117827. [DOI] [PubMed] [Google Scholar]
- Davis M, Koyanagi C. Summary of Center for Mental Health Services Youth Transition Policy Meeting: National experts panel. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2005. [Google Scholar]
- Diaz A, Edwards S, Neal WP, Elbirt P, Rappaport M, Kierstead R, et al. Foster children with special needs: The Children’s Aid Society experience. Mount Sinai Journal of Medicine. 2004;71(3):166–169. [PubMed] [Google Scholar]
- Fairbrother GL, Emerson HP, Partridge L. How stable is Medicaid coverage for children? Health Affairs. 2007;26(2):520–528. doi: 10.1377/hlthaff.26.2.520. [DOI] [PubMed] [Google Scholar]
- Federico SG, Steiner JF, Beaty B, Crane L, Kempe A. Disruptions in insurance coverage: Patterns and relationship to health care access, unmet need, and utilization before enrollment in the state children’s health insurance program. Pediatrics. 2007;120(4):E1009–E1016. doi: 10.1542/peds.2006-3094. [DOI] [PubMed] [Google Scholar]
- Franklin RS. Domestic migration across regions, divisions, and states: 1995 to 2000. Washington, DC: U.S. Census Bureau; 2003. [Google Scholar]
- Hartley D. Rural health disparities, population health, and rural culture. American Journal of Public Health. 2004;94(10):1675–1678. doi: 10.2105/ajph.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman C, Heflinger CA, Athay M, Davis M. Policy, funding, system, and sustainability issues and recommendations for transition-age youth with emotional/behavioral disorders. In: Clark HB, Unruh D, editors. Transition of Young People with Emotional or Behavioral Difficulties: An Evidence-Informed Handbook. Baltimore: Paul H. Brookes; 2009. [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression. 2. New York: John Wiley and Sons; 2000. [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. Medicaid: Issues and challenges. Washington, DC: Henry J. Kaiser Family Foundation; 2003. [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. Issue brief: An update on women’s health policy. Washington, DC: Henry J. Kaiser Family Foundation; 2007. [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. Health coverage of children: The role of Medicaid and SCHIP. Washington, DC: Henry J. Kaiser Family Foundation; 2008. [Google Scholar]
- Ketsche P, Adams EK, Snyder A, Zhou M, Minyard K, Kellenberg R. Discontinuity of coverage for Medicaid and S-CHIP children at a transitional birthday. Health Research and Educational Trust. 2007;42(6):2410–2423. doi: 10.1111/j.1475-6773.2007.00795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence RS, Gootman JA, Sim LJ, editors. Adolescent Health Services: Missing Opportunities. Washington D.C: The National Academies Press; 2008. [PubMed] [Google Scholar]
- Mallory BL. The role of social policy in life-cycle transitions. Exceptional Children. 1995;62(3):213–223. [Google Scholar]
- Mark TL, Levit KR, Coffey RM, McKusick DR, Harwood HJ, King EC, et al. National expenditures for mental health services and substance abuse treatment, 1993–2003. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2007. [Google Scholar]
- McCabe K, Yeh M, Hough RL, Landsverk J, Hurlburt MS, Culver SW, et al. Racial/ethnic representation across five public sectors of care for youth. Journal of Emotional and Behavioral Disorders. 1999;7(2):72–82. [Google Scholar]
- Philips JA, Miller JE, Cantro JC, Gaboda D. Context or composition: What explains variation in SCHIP disenrollment? Health Services Research. 2004;39(4):865–885. doi: 10.1111/j.1475-6773.2004.00262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ricketts TC. Rural health in the United States. New York, NY: Oxford University Press; 1999. [Google Scholar]
- Saunders RC, Heflinger CA. Effects of managed care on southern youths’ behavioral services use. Health Care Financing Review. 2004;26(1):23–41. [PMC free article] [PubMed] [Google Scholar]
- Saunders RC, Heflinger CA. Physical and behavioral health of Medicaid children in two Southern states. Southern Medical Journal. 2005;98(4):429–435. doi: 10.1097/01.SMJ.0000149398.02029.5F. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis. New York: Oxford University Press; 2003. [Google Scholar]
- Sommers BD. From Medicaid to uninsured: Drop-out among children in public insurance programs. Health Services Research. 2005;40(1):59–78. doi: 10.1111/j.1475-6773.2005.00342.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starr S, Campbell LR, Herrick CA. Factors affecting the use of the mental health system by rural children. Issues in Mental Health Nursing. 2002;23:291–304. doi: 10.1080/016128402753543027. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. American FactFinder. 2000 Retrieved October 6, 2008, from http://factfinder.census.gov.
- United States Department of Agriculture Economic Research Service (Producer) Measuring rurality: New definitions in 2003. 2004 retrieved from http://www.ers.usda.gov/Briefing/Rurality/Newdefinitions/
- Washington State Department of Health. Guidelines for using rural-urban classification systems for public health assessment. Tumwater, WA: Washington State Department of Health; 2006. [Google Scholar]
- WWAMI Rural Health Research Center. Rural Urban Commuting Codes (Version 2.0) Seattle, WA: University of Washington; 2006. [Google Scholar]