Abstract
Background
ICD-10 includes a craving criterion for alcohol dependence while DSM-IV does not. Little is known about whether craving fits with or improves the DSM-IV criteria set for alcohol use disorders.
Methods
Data were derived from current drinkers (N=18,352) in the 1991–92 National Longitudinal Alcohol Epidemiologic Survey (NLAES), a nationally representative survey of US adults >17 years of age. The AUDADIS was used to assess the eleven DSM-IV dependence and abuse criteria, and alcohol craving. Exploratory factor, Item Response Theory, and regression analyses were used to evaluate the psychometric properties and concurrent validity of DSM-based alcohol disorder criteria with the addition of alcohol craving.
Results
The past-12 month prevalence of craving was 1.3%. Craving formed part of a unideminsional latent variable that included existing DSM-IV criteria. Craving demonstrated high severity on the alcohol use disorder continuum, resulting in an improved dimensional model with greater discriminatory ability compared to current DSM-IV criteria. Correlates of the diagnosis did not change with the addition of craving, and past-12 month craving was associated with prior alcohol dependence, depression, and earlier age of alcohol disorder onset among those with current DSM-IV alcohol dependence.
Conclusions
The addition of craving to the existing DSM-IV criteria yields a continuous measure that better differentiates individuals with and without alcohol problems along the alcohol use disorder continuum. Few individuals are newly diagnosed with alcohol dependence given the addition of craving, indicating construct validity but redundancy with existing criteria.
Introduction
A critical appraisal of the current criteria for a diagnosis of substance abuse and dependence is underway in preparation for the publication of a fifth revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM-V). Some proposed changes include combining abuse and dependence criteria into a single diagnosis, for which considerable evidence exists as these criteria form a single latent variable with criteria arrayed across the severity spectrum (Martin et al., 2008, Saha et al., 2006). Other issues under consideration include adding a criterion indicating quantity/frequency (Keyes et al., in press, Li et al., 2007b, Saha et al., 2007) and creating a dimensional, scalable form of diagnosis that would include diagnostic criteria and correlates of substance use (Helzer et al., 2007, Li et al., 2007a). Another area under discussion is whether the diagnosis would benefit from the addition of a new criterion indicating craving for alcohol and/or other illicit drugs.
Support for the validity of craving as a component of addiction comes from many lines of evidence, including behavioral research (Heinz et al., 2008, Miller and Goldsmith, 2001, O’Brien et al., 1998, Weiss, 2005), imaging (Bencherif et al., 2004, Kalivas and O’Brien, 2008, Oslin et al., 2009, Weiss, 2005), pharmacology (O’Brien, 2005), and genetic epidemiology (Foroud et al., 2007). In fact, some have suggested that reduction of craving is central to the treatment of addiction (O’Brien et al., 2005). If so, then craving might be useful to add to the alcohol and drug disorder criteria in DSM-V, an option that is currently under consideration by the DSM-V Substance Disorders Workgroup. Further, craving is one of the substance dependence criteria in the International Classification of Disease, tenth edition (ICD-10) of the World Health Organization (World Health Organization, 1993), thus inclusion of craving in DSM-V would increase the comparability of these two diagnostic systems. However, in considering the addition of a new criterion to the DSM-V, several issues must simultaneously be balanced. A new criterion should be an observable indicator of the underlying latent construct of the disorder, and its addition should improve the diagnosis, in terms of reliability, validity, and/or case finding. Further, changes to the epidemiology of alcohol disorders based on the new addition (e.g., prevalence, correlates) need to be identified and their implications considered carefully in weighing the pros and cons of a new criterion.
Empirical assessment of the advisability of adding a new criterion can proceed using multiple analytic strategies. First, craving should be subjected to latent variable analysis (factor and item response theory [IRT] analysis) with the existing criteria. Previous studies of the alcohol abuse and dependence criteria indicate that they are arrayed across a single underlying continuum of severity (Gelhorn et al., 2008, Harford et al., 2009, Kahler and Strong, 2006, Krueger et al., 2004, Langenbucher et al., 2004, Martin et al., 2006, Proudfoot et al., 2006, Saha et al., 2006, Wu et al., 2009). Given such a structure, craving should form part of this single underlying latent variable to be a viable candidate for addition to DSM-V. Further, craving would demonstrate diagnostic improvement if the ability of the diagnosis as a whole to discriminate those with and without an alcohol disorder is improved with the addition of a craving criterion.
If craving demonstrates utility in latent variable analyses, then demonstrating concurrent validity is an additional step towards demonstrating benefit from adding craving to the alcohol disorder criteria. One way to demonstrate concurrent validity is to examine the correlates of craving among those with a DSM-IV alcohol disorder. If craving validly represents the construct of interest (having an alcohol disorder), it should be correlated with known risk factors for alcohol disorder. Another way to demonstrate concurrent validity is to construct alternative versions of the diagnosis, with and without craving, and test the associations of these two versions with known risk factors. If craving is a valid indicator of an alcohol disorder, known risk factors should remain associated with the diagnosis once craving is included; further, craving should demonstrate improvement by strengthening the associations.
The present analysis evaluates the empirical evidence for the addition of craving using these analytic methods. We had four aims. (1) To conduct a factor analysis of the existing DSM-IV criteria with and without craving. (2) To conduct IRT analyses to examine the severity and discrimination of alcohol abuse/dependence criteria and a craving criterion and evaluate the changes to the total discriminatory ability and severity of the set of total set criteria regarding the latent trait of alcohol problems once craving is included as an additional criterion. (3) To evaluate the concurrent validity of craving by assessing the clinical characteristics of DSM-IV alcohol dependent individuals with and without alcohol craving. (4) To evaluate the concurrent validity of craving by constructing alternative versions of AUD diagnoses with and without craving and assess the associations between these alternatives and known risk factors for alcohol use disorders.
Methods
Sample
The 1991–1992 National Longitudinal Alcohol Epidemiologic Survey (NLAES) is a nationally representative survey of non-institutionalized adults (18+) in the United States. The survey was sponsored by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), with fieldwork conducted by the U.S. Census Bureau. Face-to-face interviews by experienced lay interviewers were completed on 42,862 individuals. The NLAES featured a complex multistage design, described in detail elsewhere (Grant, 1997, Grant et al., 2004). NLAES design elements are similar to the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (Grant et al.). While recent psychometric studies have used the NESARC survey (conducted in 2001–2002) to evaluate diagnostic properties of various DSM algorithms (Kahler and Strong, 2006, Saha et al., 2006, Saha et al., 2007), this data set did not include a craving measure and thus could not be used for the present purpose. Analyses were restricted to NLAES respondents who drank at least 12 drinks in the past year (N=18,352), the NLAES definition of current drinkers.
Measures
DSM-IV alcohol diagnoses
DSM-IV alcohol abuse/dependence criteria experienced in the last 12 months were generated from 34 symptom question in the Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS). Although the DSM-IV classification was not published until 1994, all the specific diagnostic criteria for DSM-IV alcohol abuse and dependence were known prior to the fieldwork for NLAES and were incorporated into the AUDADIS. The reliability of AUDADIS diagnosis has been shown to be good to excellent (Canino et al., 1999, Chatterji et al., 1997, Grant et al., 2003, Grant et al., 1995, Hasin et al., 1997a, Hasin et al., 2006) and validity has been extensively documented (Canino et al., 1999, Cottler et al., 1997, Hasin, 2003, Hasin et al., 1997b, Hasin and Paykin, 1999, Hasin et al., 1999, Hasin et al., 1997c, Pull et al., 1997, Ustun et al., 1997, Vrasti et al., 1998).
The abuse criteria included: 1) use in hazardous situations (Hazardous Use); 2) failure to fulfill major role obligations (Neglect Roles); 3) legal problems related to drinking (Legal Problems); and 4) social or interpersonal problems (Social/Interpersonal Problems). Dependence criteria included: 1) tolerance (Tolerance); 2) withdrawal or withdrawal relief avoidance (Withdrawal); 3) drinking larger amounts or for longer periods than intended (Larger/Longer); 4) persistent desire or unsuccessful efforts to cut down (Quit/Control); 5) time spent in activities to obtain alcohol or to recover from its effects (Time Spent); 6) giving up or reducing important activities in favor of drinking (Activities Given Up); and 7) continued drinking despite knowledge of a physical or psychological problem caused or exacerbated by drinking (Phys/Psych Problems).
Craving
The following item was used to address craving: “In your entire life, did you ever want a drink so badly that you couldn’t think of anything else?” Respondents who responded positively were then asked for more information regarding the time frame(s) in which the experience occurred. We considered the individual positive for the item if they responded that the experience occurred in the past 12-months.
All measures described above were also assessed in the prior to past-year timeframe (i.e., whether each criterion was experienced in the time frame prior to the past year). Included as an online supplement, we repeated IRT analysis of the craving criterion assessed on a lifetime timeframe (past year or prior to the past year) to demonstrate similarities in structure.
Statistical analysis
All analyses incorporate sampling weights to adjust for oversampling of some demographic groups, and all standard errors are adjusted to correct for dependencies in the data caused by the complex survey design (that is, unequal probability of selection into the sample through clustering by geographically-defined stratum and primary sampling unit).
Criterion prevalence, demographic and clinical covariate
Prevalences of abuse and dependence criteria as well as craving among current drinkers were estimated using SUDAAN software (Research Triangle Institute, 2004). In addition, within the portion of the sample diagnosed with DSM-IV alcohol dependence, we examined the clinical correlates of endorsing craving. Odds ratios were estimated using logistic regression. Finally, we constructed two diagnoses, one that corresponds to current DSM-IV criteria, and one that includes craving but leaves the threshold for diagnosis at ≥3 criteria. Prevalence and clinical covariates of these two diagnoses were estimated to determine the concurrent validity of a diagnosis that includes craving.
Exploratory Factor Analysis (EFA)
We began psychometric analysis by estimating one and two-factor models for existing DSM-IV criteria with and without craving. We did this to determine unidimensionality of the criteria (i.e., representing a single underlying factor), which is required to accurately estimate the parameters of the most widely used IRT models. EFA of tetrachoric correlations using quartimin rotation (Jennrich and Sampson, 1966) was used, maximizing the sum of row variance of the structure matrix. This rotation was chosen over other possible rotations (e.g., Promax) because it is less likely to produce multiple spurious factors (favoring parsimonious factor structures) while still allowing for correlated factors (Lubke & Muthen, 2007). All latent variable analyses were conducted using MPLUS Version 5.21 (Muthén & Muthén, 2009), which adjusted standard errors for the complex sampling design and uses a weighted least squares mean and variance adjusted (WLSMV) estimator.
Four fit measures were used to determine the best fitting model: Comparative Fit Index (CFI), Tucker Lewis Index (TLI), Root Mean Square Error of Approximation (RMSEA), and examination of the eigenvalues of factors. The generally accepted interpretation of CFI and TLI is that values over 0.95 indicate good fit, while RMSEA less than 0.05 indicates good model fit (Kline, 1998). We stopped evaluating factor solutions once eigenvalues were <1.0, as factors with eigenvalues less than 1.0 do not explain a sufficient amount of variance in the criteria to be retained (Kaiser-Guttman rule).
Item Response Theory analysis
Once unidimensionality of criteria is established through EFA, we can fit IRT models to estimate parameters (severity and discrimination) for the craving criterion in the context of existing abuse/dependence criteria, and evaluate the total information provided by the set of criteria in reference to the alcohol use disorder continuum. We fit a 2-parameter logistic IRT model (Birnbaum, 1968) using a maximum likelihood estimator once unidimensionality of the underlying factor structure was established. In MPLUS, 2-parameter IRT models are fit as Confirmatory Factor Analysis (CFA) models, where the CFA model parameters are rescaled to an IRT metric (Bock et al., 1988).
Our IRT analysis began by hypothesizing a continuous latent variable representing the alcohol use disorder continuum, referred to as θ, which is normally distributed with mean 0 and standard deviation 1. The 2-parameter logistic IRT provides estimates of the discrimination (parameter a) and severity (parameter b) of each item indexing this continuum. Discrimination is defined as the ability of the criterion to distinguish between those who are higher on the alcohol use disorder continuum versus those who are lower. Severity is defined as the point along the continuum when there is a 50% chance of the item being present. Note that severity is directly related to the prevalence of the criterion in the data; in most cases criteria that are rare are more clinically severe, but higher severity in the IRT model does not necessarily indicate higher clinical severity. The formula for calculating the probability of item endorsement in MPLUS (Muthén & Asparouhov, 2002) is:
Where u is the evaluated criterion, D is a constant approximately equal to (√(π2/3) = 1.7).
Goodness of model fit was assessed using four criteria: Bayesian Information Criteria (BIC), sample-size adjusted BIC, Akaike Information Criteria (AIC), and −2 Log Likelihood. The BIC is a fit statistic that extends the traditional maximum-likelihood-based model fit statistics in several ways including penalization for complexity of the model (i.e., number of parameters) (Etzioni and Kadane, 1995). The AIC is closely related but imposes a relatively lighter penalty for model complexity, when compared with BIC (Akaike, 1978). The −2 Log Likelihood is a standard maximum likelihood statistic for evaluating model fit. Note that absolute goodness-of-fit measures used in EFA analyses described earlier (e.g., CFI, TLI) are not available for maximum likelihood estimated IRT models fit to response patterns; thus relative measures BIC, sample size adjusted BIC, and AIC are estimated. Model fits were examined by comparing fit indices with all existing DSM-IV criteria plus craving to a model in which the craving parameter was constrained to be zero.
The aggregate information function (AIF) graph was generated to visually represent the total amount of information provided by the model of all criteria. The height of the information function reflects the collective discriminatory ability of the model and represents the extent of the information provided by the set of criteria under assessment. Thus, the higher the peak of the information curve, the greater the ability of the criteria to distinguish between those with and without alcohol problems. The placement of the curve along the latent continuum reflects the severity of the overall test.
Finally, measurement non-invariance of the craving criterion was tested across gender, race/ethnicity, and age. Race/ethnicity was operationalized as a five-level nominal variable (non-Hispanic White, non-Hispanic Black, Native American/Alaska Native, Asian/Pacific Islander, and Hispanic), and age was operationalized as a four-level ordinal variable (18–29, 30–44, 45–64, 65+). MPLUS uses CFA with covariates (Multiple Indicators Multiple Causes [MIMIC] model) to test item measurement non-invariance due to differential item functioning. We tested the direct effect of the covariate on the craving item that is unmediated through the underlying latent trait. An alpha of 0.05 was selected a priori. A significant direct effect means that for the same severity level, members of different covariate groups have different probabilities of endorsing the item; this is indicative of measurement non-invariance, as group membership should not be a determinant of criterion endorsement probability at equal levels of severity if the criterion is completely unbiased. The final MIMIC model included all significant indirect (latent trait regressed on covariate) and direct (item regressed on covariate) effects. A similar approach has been taken previously in IRT analyses of alcohol criteria (Harford et al., 2009). Because measurement non-invariance analyses of DSM-IV alcohol abuse/dependence criteria have been previously pursued (e.g., previous analyses in data with similar design and population as these indicating non-invariance for Quit/Control, Withdrawal, Neglect Roles, and Larger/Longer by sex and almost all criteria by age; Saha et al., 2006, 2007), we focused our measurement non-invariance analysis on the craving criterion only.
Results
Exploratory Factor analysis
Table 1 shows one and two factor solutions for four EFAs. A three-factor solution was not estimated as the eigenvalue for the second factor in a two-factor solution was less than one. Comparing the one- and two-factor solutions, a one-factor solution is the most parsimonious model for existing DSM-IV criteria, based on excellent fit statistics (CFI=0.995, TLI=0.993, and RMSEA=0.023) and only marginal increases in fit moving from a one-factor to a two-factor solution. The eigenvalue for the second factor in the two-factor model was less than 1.0, indicating the second factor does not explain sufficient additional variance in the criteria to be considered a useful addition to the model. The addition of a craving criterion does not materially change the factor structure of the diagnosis. Craving loads on the single factor in the one factor model (0.870), and one factor remains the most parsimonious representation of the data structure with excellent model fit (CFI=0.994, TLI= 0.993, RMSEA=0.022).
Table 1.
Among current drinkers (N=18,352), prevalence of DSM-IV abuse and dependence criteria as well as craving criterion, and exploratory factor analysis (EFA) of four models of DSM-IV abuse and dependence criteria as well as craving criterion.
| Model 1: existing DSM-IV criteria | Model 2: addition of Craving | ||||||
|---|---|---|---|---|---|---|---|
| Prevalence (N=18,352) | One factor | Two factors* | One factor | Two factors* | |||
| % | Loading (SE) | Loading (SE) | Loading (SE) | Loading (SE) | |||
| Neglect roles (A) | 5.85 | 0.85 (0.01) | 0.65 (0.04) | −0.24 (0.04) | 0.81 (0.01) | 0.60 (0.04) | −0.30 (0.04) |
| Hazardous use (A) | 14.59 | 0.80 (0.01) | 0.04 (0.01) | −0.94 (0.04) | 0.75 (0.01) | 0.04 (0.02) | −0.92 (0.03) |
| Legal problems (A) | 1.67 | 0.64 (0.02) | 0.16 (0.08) | −0.55 (0.08) | 0.83 (0.02) | 0.14 (0.08) | −0.58 (0.07) |
| Social/Interpersonal problems (A) | 7.47 | 0.82 (0.01) | 0.62 (0.04) | −0.24 (0.04) | 0.83 (0.01) | 0.58 (0.04) | −0.29 (0.04) |
| Tolerance (D) | 15.69 | 0.75 (0.01) | 0.73 (0.03) | −0.04 (0.03) | 0.71 (0.01) | 0.70 (0.03) | −0.08 (0.04) |
| Withdrawal (D) | 12.60 | 0.83 (0.01) | 0.70 (0.03) | −0.17 (0.04) | 0.86 (0.01) | 0.67 (0.03) | −0.21 (0.04) |
| Larger/Longer (D) | 25.48 | 0.84 (0.01) | 0.65 (0.04) | −0.23 (0.04) | 0.91 (0.01) | 0.59 (0.04) | −0.30 (0.05) |
| Quit/Control (D) | 17.52 | 0.71 (0.01) | 0.84 (0.03) | 0.13 (0.03) | 0.82 (0.01) | 0.75 (0.03) | 0.03 (0.04) |
| Time Spent (D) | 3.31 | 0.85 (0.01) | 0.91 (0.03) | 0.06 (0.03) | 0.85 (0.01) | 0.91 (0.03) | 0.05 (0.03 |
| Activities Given Up (D) | 1.61 | 0.91 (0.01) | 0.92 (0.03) | 0.01 (0.04) | 0.80 (0.01) | 0.86 (0.04) | −0.07 (0.04) |
| Phys/Psych Problems (D) | 5.22 | 0.82 | 0.89 (0.02) | 0.07 (0.03) | 0.64 (0.01) | 0.87 (0.03) | 0.04 (0.03) |
| Craving | 1.26 | -- | -- | 0.87 (0.01) | 0.99 (0.03) | 0.11 (0.04) | |
| Eigenvalue | 7.371 | 0.744 | 8.099 | 0.773 | |||
| CFI | 0.995 | 0.997 | 0.994 | 0.997 | |||
| TLI | 0.993 | 0.996 | 0.993 | 0.996 | |||
| RMSEA | 0.023 | 0.018 | 0.022 | 0.017 | |||
| Factor correlation | -- | 0.746 | -- | 0.747 | |||
Bolded text indicates factor loadings greater than an absolute value for 0.4
Item Response Theory analysis
Discrimination and severity estimates
Two models were tested: both have twelve variables in the model (the eleven existing criteria and the craving criterion). In Model 1, the craving criterion was constrained to have no relationship with the latent trait. In Model 2, the craving criterion was unconstrained. Results are shown in Table 2.
Table 2.
Criterion response model parameters for 1) existing DSM-IV abuse and dependence criteria and 2) the addition of craving among current drinkers in the general population (N=18,352)
| Model 1: existing DSM-IV criteria | Model 2: addition of Craving | |||
|---|---|---|---|---|
| Discrimination (SE) | Severity (SE) | Discrimination (SE) | Severity (SE) | |
| Neglect roles (A) | 1.75 (0.06) | 1.92 (0.03) | 1.75 (0.06) | 1.92 (0.03) |
| Hazardous use (A) | 1.31 (0.03) | 1.42 (0.02) | 1.30 (0.03) | 1.43 (0.02) |
| Legal problems (A) | 1.05 (0.05) | 3.16 (0.09) | 1.05 (0.05) | 3.16 (0.09) |
| Social/Interpersonal problems (A) | 1.55 (0.05) | 1.83 (0.03) | 1.54 (0.05) | 1.83 (0.03) |
| Tolerance (D) | 0.59 (0.00) | 2.08 (0.02) | 0.59 (0.00) | 2.08 (0.02) |
| Withdrawal (D) | 1.63 (0.04) | 1.41 (0.02) | 1.63 (0.04) | 1.41 (0.02) |
| Larger/Longer (D) | 1.68 (0.05) | 0.82 (0.01) | 1.67 (0.04) | 0.82 (0.01) |
| Quit/Control (D) | 1.03 (0.03) | 1.36 (0.02) | 1.02 (0.03) | 1.36 (0.02) |
| Time Spent (D) | 1.82 (0.07) | 2.20 (0.03) | 1.87 (0.07) | 2.18 (0.03) |
| Activities Given Up (D) | 2.54 (0.15) | 2.39 (0.04) | 2.52 (0.15) | 2.39 (0.04) |
| Phys/Psych Problems (D) | 1.51 (0.05) | 2.02 (0.03) | 1.54 (0.05) | 2.01 (0.03) |
| Craving | -- | -- | 1.98 (0.11) | 2.59 (0.05) |
| Bayesian (BIC) | 52571.086 | 50976.329 | ||
| Sample-Size Adjusted BIC | 52727.821 | 50903.238 | ||
| Akaike (AIC) | 52657.909 | 50812.469 | ||
| −2 Log Likelihood | −46854.376 | −46272.643 | ||
In the 2-parameter model including the eleven existing DSM-IV criteria (Model 1), the criteria indicating the highest severity include Legal Problems (3.16, SE=0.1), Activities Given Up (2.39 SE=0.1), and Time Spent (2.20, SE=0.0) while the criteria with the lowest severity were Larger/Longer (0.82, SE=0.0), Quit/Control (1.36, SE=0.0), and Hazardous Use (1.42, SE=0.0). Activities Given Up ranked the highest in discriminatory ability, indicating it was comparatively the best in discriminating the individuals along the underlying alcohol use disorder continuum. Tolerance and Quit/Control exhibited the lowest level of discrimination.
Table 2 also includes the discrimination and severity parameter estimates for a model with the addition of the craving criterion (Model 2). Neither the magnitude of parameter estimates nor the rank order of DSM-IV criteria in terms of discrimination and severity substantially changed when craving was added to the model. Craving fell along a mid- to high-end of severity and discrimination (severity: 2.59 [SE=0.0]; discrimination: 1.98 [SE=0.1]). The BIC, sample size-adjusted BIC, and AIC indicated that a model including craving had substantially better fit to the data, compared to the model including DSM-IV criteria only (See Table 4).
Table 4.
Concurrent validity of two diagnostic formulations (Diagnosis 1: current DSM-IV alcohol dependence; Diagnosis 2: current DSM-IV criteria plus craving, threshold remains at three or more criteria)
| Diagnosis 1 Present | Diagnosis 1 Absent | p-value for difference* | Diagnosis 2 Present | Diagnosis 2 Absent | p-value for difference* | |
|---|---|---|---|---|---|---|
| 2,002 | 16,350 | 2,022 | 16,330 | |||
| Age of alcohol use onset (Mean, SD) | 17.03 (0.09) | 19.13 (0.05) | <0.001 | 17.03 (0.09) | 19.13 (0.05) | <0.001 |
| Family history of alcohol problems (%, SE) | 42.89 (1.38) | 25.79 (0.42) | <0.001 | 43.12 (1.37) | 25.73 (0.41) | <0.001 |
| Used treatment services for alcohol problems in the past year (%, SE) | 12.40 (0.92) | 0.84 (0.09) | <0.001 | 12.38 (0.91) | 0.82 (0.09) | <0.001 |
| Alcohol dependence prior to the past year (%,SE) | 51.29 (1.26) | 11.98 (0.31) | <0.001 | 51.05 (1.26) | 11.96 (0.32) | <0.001 |
| Meets criteria for alcohol abuse (%, SE) | 59.33 (1.30) | 6.99 (0.26) | <0.001 | 59.20 (1.29) | 6.94 (0.26) | <0.001 |
| Current depression diagnosis (%, SE) | 19.374 (1.07) | 6.31 (0.21) | <0.001 | 19.35 (1.06) | 6.29 (0.21) | <0.001 |
| Current drug abuse/dependence diagnosis (%,SE) | 15.09 (0.97) | 1.52 (0.13) | <0.001 | 14.95 (0.96) | 1.52 (0.13) | <0.001 |
derived for linear regression (age of onset as outcome) or logistic regression (all other outcomes) controlling for age, sex, race/ethnicity, education, employment, urbanicity, and region
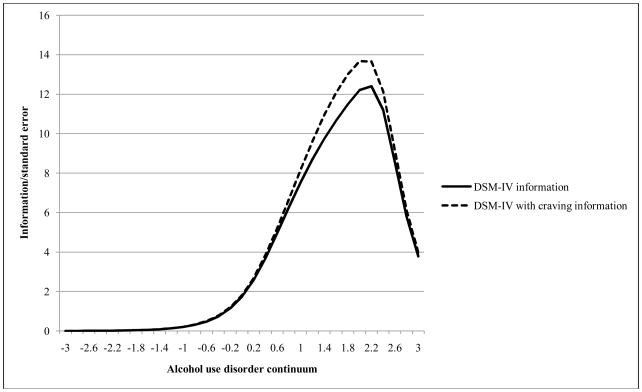
Aggregate Information Function (AIF)
Figure 1 plots the AIF for the eleven existing DSM-IV criteria as well as the AIF for the existing DSM-IV criteria with craving included. The model with craving creates a more discriminating overall set of criteria (reflected in the increase peak of the curve) but reflects little change in the ability of the model to capture a greater or different range of severity of the underlying continuum of disorder.
Figure 1.
Aggregate information curves for 1) the existing DSM-IV criteria and 2) the addition of craving among current drinkers in the general population (N=18,352)
Measurement non-invariance
We tested whether craving evidences measurement non-invariance by gender, age, and race/ethnicity. Controlling for the indirect effect of race/ethnicity on craving that is mediated through the latent alcohol use disorder continuum, blacks are less likely to endorse craving compared to Whites (Z=−1.35, SE=0.52, p=0.009); no indirect effects were significant comparing other racial/ethnic groups to Whites. Compared to those 65+, individuals 45–64 are more likely to endorse craving (Z=0.91, SE=0.39, p=0.02); no indirect effects were significant comparing other age groups to those 65+. There were no significant indirect effects of gender (p=0.23).
Supplementary analysis: lifetime estimates
As supplementary analyses, we conducted exploratory factor and IRT analysis on lifetime criteria among lifetime drinkers (N=27,616) (see Supplementary Analysis). Similarly to past 12-month estimates, craving exhibited low prevalence compared to existing DSM-IV criteria (3.5% SE=0.1). Craving was unidimensional with existing criteria, with a one-factor model fitting the seven DSM-IV dependence, four DSM-IV abuse, and craving criteria (CFI=0.995, TLI=0.994, RMSEA=0.031, SRMR=0.041). IRT analysis indicated relatively high severity (craving was the second most severe item after ‘neglect roles’) and discrimination (craving was the third most discriminating item of the twelve). Model fit estimates indicated improved fit with the addition of craving. While the rank order of discrimination and severity estimates are slightly different comparing lifetime to past-12 month criteria, Neglect Roles, Legal Problems, and Activities Given Up, remained the highest severity criteria, while Larger/Longer, Hazardous Use, and Quit/Control remained the low severity criteria.
Concurrent validity: clinical correlates
Table 3 presents the concurrent validity analysis, assessing clinical correlates of craving among those with DSM-IV alcohol dependence. Controlling for age, sex, race/ethnicity, education, urbanicity, region, and number of alcohol dependence symptoms, individuals with craving had a younger age of alcohol dependence onset (OR=0.96, 95% C.I. 0.92–0.99), were more likely to have had alcohol dependence prior to the past year (OR=2.10, 95% C.I. 1.17–3.77), and were more likely to have a current depression diagnosis (OR=2.29, 95% C.I. 1.37–3.84).
Table 3.
Clinical characteristics of DSM-IV alcohol dependent individuals (N=2,002) with and without craving experiences.
| With craving | Without craving | |||
|---|---|---|---|---|
| N=203 | N=1799 | |||
| % (SE) | % (SE) | OR1 (95% C.I.)* | OR2 (95% C.I.)** | |
| Age of alcohol use onset (Mean, SD) | 16.14 (0.40) | 17.14 (0.09) | 0.93 (0.87–0.99) | 0.96 (0.90–1.01) |
| Age of alcohol dependence onset (Mean, SD) | 21.13 (0.52) | 22.44 (0.29) | 0.96 (0.93–0.99) | 0.96 (0.92–0.99) |
| Family history of alcohol problems (%, SE) | 55.4 (4.12) | 41.5 (1.44) | 1.30 (0.87–1.95) | 1.03 (0.67–1.59) |
| Used treatment services for alcohol problems in the past year (%, SE) | 31.2 (3.79) | 10.2 (0.90) | 3.25 (2.09–5.04) | 1.01 (0.59–1.73) |
| Alcohol dependence prior to the past year (%, SE) | 76.9 (3.46) | 23.1 (3.52) | 4.07 (2.42–6.84) | 2.10 (1.17–3.77) |
| Meets criteria for alcohol abuse (%, SE) | 86.8 (2.89) | 56.2 (1.40) | 5.63 (3.00–10.56) | 1.83 (0.95–3.50) |
| Current depression diagnosis (%, SE) | 41.0 (4.07) | 16.9 (1.06) | 3.93 (2.51–6.15) | 2.29 (1.37–3.84) |
| Current drug abuse/dependence diagnosis (%, SE) | 26.0 (3.51) | 13.8 (0.97) | 2.00 (1.33–3.01) | 0.94 (0.53–1.68) |
controlling for age, sex, race/ethnicity, education, urbanicity, region
controlling for age, sex, race/ethnicity, education, urbanicity, region, and number of alcohol dependence symptoms Bolded text indicates statistical significance at the p<0.05 level
In Table 4 we present the concurrent validity analysis assessing the association between clinical covariates and two alcohol dependence diagnoses: first, the existing DSM-IV diagnosis, and second, a diagnosis with craving as an indicator. The threshold for diagnosis was kept at ≥3 criteria. No differences were found.
Based on the present DSM-IV definition, the prevalence of alcohol dependence among current drinkers was 11.4%. When craving was added as an eighth criterion and the threshold kept at ≥3 criteria for diagnosis, the prevalence of alcohol dependence increased very slightly (to 11.5%) with 20 additional cases identified.
Discussion
Taken together, these analyses indicate advantages as well as disadvantages related to including craving as an additional criterion in the DSM. Advantages of craving are four-fold. First, craving forms part of a unidemensional construct with the other DSM-IV criteria, indicating that craving taps into the same underlying latent construct (conceptualized here as an alcohol use disorder continuum) as existing criteria. Second, the addition of craving improves the overall fit of the criteria to a general population sample, indicating that a diagnostic set with craving better captures the full range of alcohol problems in the general population compared to a diagnosis without craving. Third, the addition of craving increases the total discriminatory ability of the set of criteria as a whole. This indicates that craving is highly related to the alcohol use disorder continuum, and that a diagnosis with craving can better distinguish individuals with and without alcohol problems. Finally, craving is associated with several risk factors among individuals with DSM-IV diagnosed alcohol dependence, including younger age of dependence onset, prior to past year alcohol dependence (suggesting a chronic course), and major depressive disorder. This indicates concurrent validity; craving is correlated with alcohol-associated risk factors with which we would expect an indicator of alcohol problems to be correlated. Note that these analyses are not intended to reveal anything about the etiology of craving per se; we would expect that any construct that captures the alcohol use disorder continuum would be related to these risk factors among those with DSM-IV alcohol dependence.
These considerations need to be weighed against the disadvantages of adding a new criterion that is not already included in most datasets. Points of evidence against craving are three-fold. First, the indicator of craving used in these analyses exhibited some measurement non-invariance, with Blacks less likely than Whites to endorse craving at the same level of alcohol disorder severity, and individuals 45–64 more likely than individuals 65+ to endorse craving. While measurement non-invariance has been demonstrated for many of the existing criteria (Gelhorn et al., 2008, Harford et al., 2009, Langenbucher et al., 2004, Martin et al., 2006, Wu et al., 2009), including non-invariance of most existing DSM-IV criteria by age in data similar in design and analyses to the NLAES sample (Saha et al., 2006, 2007), the inclusion of a new criterion that is measurement non-invariant should be viewed with caution. Second, existing IRT analyses of DSM-IV criteria have indicated the need for new criteria that capture the less severe end of the diagnostic spectrum (Li et al., 2007a, b, Martin et al., 2006, Martin et al., 2008, Saha et al., 2006, Saha et al., 2007); craving does not serve this purpose, as it is on the high end of the severity spectrum. Finally, datasets that were expensive to assemble (e.g., epidemiologic, genetic or multi-site clinical trials) and have not assessed craving would be unable to generate strict DSM-diagnoses if craving is included. It should be noted, however, that because of the high cohesion of alcohol abuse/dependence criteria with craving, the latent variable is likely still well-represented whether or not craving is included in a particular dataset. The use of a dimensional, psychometric approach to the assessment and diagnosis of alcohol problems (e.g., equating [Embretson & Reise, 2000]) may be beneficial for research and clinical practice if craving is included in the DSM-V.
The rarity of craving (1.3%) and the lack of additional cases identified can be seen as both a benefit and a drawback. If the addition of craving resulted in substantially increased prevalence and/or changed correlates of alcohol dependence (as is the case with a quantity/frequency indicator (Keyes et al., 2009)), we might consider whether diagnostic sensitivity and specificity would be adversely affected by its inclusion. On the contrary, craving does not modify the descriptive epidemiology of alcohol dependence, indicating that a similar number of cases would be identified with a diagnosis that in its totality provides a more discriminating test, better differentiating individuals along the latent trait of alcohol disorders. Further, given associations with early onset, chronicity, and major depression, the presence of craving may indicate a more severe phenotype compared to alcohol dependent individuals without craving. Given the associations of alcohol craving with a genetic variant (Foroud et al., 2007), the inclusion of craving may be useful for progress in genetic epidemiology. More analyses with diverse, genetically-informative data would be useful to fully understand the phenotypic implications of alcohol craving. Further, research clarifying the role of depression and other psychopathology in the experience of craving would be useful. On the other hand, the lack of additional cases suggests that craving is largely redundant with existing criteria. Clinical case finding would not improve given the addition of a craving criterion, raising doubts about the added benefit of the criterion in the context of the existing symptoms. Further analyses and replications in diverse samples of clinical, adolescent, and genetically-informative individuals would aid in the elucidation of craving utility in a variety of contexts.
Most previous investigations of abuse and dependence criteria using IRT focused on psychometric properties of existing criteria without evaluating new criteria, and our IRT analyses of existing abuse/dependence criteria are generally in line with this previous research (Gelhorn et al., 2008, Harford et al., 2009, Kahler and Strong, 2006, Krueger et al., 2004, Langenbucher et al., 2004, Martin et al., 2006, Proudfoot et al., 2006, Saha et al., 2006, Wu et al., 2009); one exception is a recent study of middle-aged men in the general population that examined the structure of the alcohol use disorder continuum using 110 alcohol items, including an item capturing craving (Krueger et al., 2004). Similar the present study, craving exhibited relatively high severity and discrimination. Additionally, recent analyses suggest a quantity/frequency indicator might be a useful criteria to capture the less severe end of the alcohol disorders continuum (Saha et al., 2007), leading some to call for its inclusion in the DSM-V (Li et al., 2007b, Martin et al., 2008). However, including weekly at-risk drinking may have a large impact on the prevalence of alcohol dependence in the general population (Keyes et al., 2009). The present study provided evidence for a criterion with opposite characteristics; more severe cases of alcohol disorder would be captured, and the prevalence of the diagnosis would not be largely impacted.
Limitations of this study are noted. First, the NLAES questionnaire included only a single question tapping into the relevant construct of craving. Data sources with more indicators of craving would be preferable. However, given the limited national data sources with measures of craving included in the questionnaire, the NLAES offers a unique dataset in which to examine this issue. Second, the NLAES survey was conducted in 1991–1992. Analyses comparing the alcohol diagnoses in the NLAES and its successor, the NESARC, have identified changes in prevalence of disorder and specific symptom items (Chou et al., 2005, Grant et al., 2004). In order to understand the comparability of the NLAES and NESARC, we conducted an initial IRT analysis on the base model of DSM-IV abuse and dependence criteria. Despite small variations in the magnitude of the estimates, the conclusions drawn were the same (results not shown). Additionally, responses are based on self-report and are subject to information bias. We limited the present analysis to past-12 month criteria to mitigate recall bias. As an online supplement to this report, we also analyzed lifetime endorsement of alcohol disorder criteria. Results indicated that, similarly to the analysis of past 12-month criteria, craving is relatively rare compared to other criteria, is unidimensional with existing DSM-IV criteria, exhibits high severity and discrimination, and improves the fit of the alcohol disorder criteria to the data.
The large sample size and well-tested measurement instrument (AUDADIS) used in the NLAES serve as strengths of this study. Given the pros and cons shown for adding craving to DSM-V based on epidemiologic data, a clear conclusion cannot be drawn on the advisability of this addition. However, the results presented above constitute part of the information under consideration by the DSM-V substance disorders workgroup, and provision of this information to the larger scientific community enhances the transparency of the DSM-V process. Future research using latent variable modeling techniques should focus on generating additional items that could improve both the reliability and validity of the current alcohol diagnoses, and discussions should continue regarding the utility of modifying DSM diagnoses to more closely correspond to ICD.
Supplementary Material
Acknowledgments
This research was supported in part by grants from the National Institute on Alcoholism and Alcohol Abuse (K05AA014223, Hasin), the National Institute on Drug Abuse (RO1DA018652, Hasin), a fellowship from the National Institute of Drug Abuse (F31 DA026689, K. Keyes), and support from New York State Psychiatric Institute. The authors wish to thank Timothy Geier for assistance with manuscript preparation, and Sarah Braunstein, Matthew Lamb, and Ann Madsen for helpful comments on previous drafts of this manuscript.
Footnotes
The authors report no conflicts of interest.
References
- Akaike H. A Bayesian analysis of the minimum AIC procedure. Annals of the Institute of Statistical Mathematics. 1978;30A:9–14. [Google Scholar]
- Bencherif B, Wand GS, McCaul ME, Kim YK, Ilgin N, Dannals RF, Frost JJ. Mu-opioid receptor binding measured by [11C]carfentanil positron emission tomography is related to craving and mood in alcohol dependence. Biological Psychiatry. 2004;55:255–62. doi: 10.1016/j.biopsych.2003.07.007. [DOI] [PubMed] [Google Scholar]
- Birnbaum A. Some latent trait models. In: Lord FM, Norvick MR, editors. Statistical Theory of Mental Test Scores. Addison-Wesley; Reading, MA: 1968. pp. 397–472. [Google Scholar]
- Bock RD, Gibbons R, Muraki E. Full-Information Item Factor Analysis. Applied Psychological Measurement. 1988;12:261–280. [Google Scholar]
- Canino G, Bravo M, Ramirez R, Febo VE, Rubio-Stipec M, Fernandez RL, Hasin D. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. Journal of Studies on Alcohol. 1999;60:790–9. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D. Reliability of the alcohol and drug modules of the Alcohol Use Disorder and Associated Disabilities Interview Schedule--Alcohol/Drug-Revised (AUDADIS-ADR): an international comparison. Drug and Alcohol Dependence. 1997;47:171–85. doi: 10.1016/s0376-8716(97)00088-4. [DOI] [PubMed] [Google Scholar]
- Chou SP, Grant BF, Dawson DA, Stinson FS, Saha T, Pickering RP. Twelvemonth prevalence and changes in driving after drinking: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2005;80:223–30. doi: 10.1016/j.drugalcdep.2005.03.013. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Grant BF, Blaine J, Mavreas V, Pull C, Hasin D, Compton WM, Rubio-Stipec M, Mager D. Concordance of DSM-IV alcohol and drug use disorder criteria and diagnoses as measured by AUDADIS-ADR, CIDI and SCAN. Drug Alcohol Depend. 1997;47:195–205. doi: 10.1016/s0376-8716(97)00090-2. [DOI] [PubMed] [Google Scholar]
- Edwards G. The Alcohol Dependence Syndrome: a concept as stimulus to enquiry. British Journal of Addiction. 1986;81:171–183. doi: 10.1111/j.1360-0443.1986.tb00313.x. [DOI] [PubMed] [Google Scholar]
- Edwards G, Gross MM. Alcohol dependence: provisional description of a clinical syndrome. British Medical Journal. 1976;1:1058–1061. doi: 10.1136/bmj.1.6017.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embretson SE, Reise SP. Item Response Theory for Psychologists. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- Etzioni RD, Kadane JB. Bayesian statistical methods in public health and medicine. Annual Review of Public Health. 1995;16:23–41. doi: 10.1146/annurev.pu.16.050195.000323. [DOI] [PubMed] [Google Scholar]
- Foroud T, Wetherill LF, Liang T, Dick DM, Hesselbrock V, Kramer J, Nurnberger J, Schuckit M, Carr L, Porjesz B, Xuei X, Edenberg HJ. Association of alcohol craving with alpha-synuclein (SNCA) Alcoholism: Clinical and Experimental Research. 2007;31:537–45. doi: 10.1111/j.1530-0277.2007.00337.x. [DOI] [PubMed] [Google Scholar]
- Gelhorn H, Hartman C, Sakai J, Stallings M, Young S, Rhee SH, Corley R, Hewitt J, Hopfer C, Crowley T. Toward DSM-V: an item response theory analysis of the diagnostic process for DSM-IV alcohol abuse and dependence in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:1329–39. doi: 10.1097/CHI.0b013e318184ff2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF. Prevalence and correlates of alcohol use and DSM-IV alcohol dependence in the United States: results of the National Longitudinal Alcohol Epidemiologic Survey. Journal of Studies on Alcohol. 1997;58:464–73. doi: 10.15288/jsa.1997.58.464. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74:223–34. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Moore TC, Shepard J, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) National Institute on Alcohol Abuse and Alcoholism Web Site; [Google Scholar]
- Harford TC, Yi HY, Faden VB, Chen CM. The dimensionality of DSM-IV alcohol use disorders among adolescent and adult drinkers and symptom patterns by age, gender, and race/ethnicity. Alcoholism: Clinical and Experimental Resesarch. 2009;33:868–78. doi: 10.1111/j.1530-0277.2009.00910.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin D. Classification of alcohol use disorders. Alcohol Research and Health. 2003;27:5–17. [PMC free article] [PubMed] [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug and Alcohol Dependence. 1997a;44:133–41. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- Hasin D, Grant BF, Cottler L, Blaine J, Towle L, Ustun B, Sartorius N. Nosological comparisons of alcohol and drug diagnoses: a multisite, multi-instrument international study. Drug and Alcohol Dependence. 1997b;47:217–26. doi: 10.1016/s0376-8716(97)00092-6. [DOI] [PubMed] [Google Scholar]
- Hasin D, Hatzenbuehler ML, Keyes K, Ogburn E. Substance use disorders: Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) and International Classification of Diseases, tenth edition (ICD-10) Addiction. 2006;101(Suppl 1):59–75. doi: 10.1111/j.1360-0443.2006.01584.x. [DOI] [PubMed] [Google Scholar]
- Hasin D, Paykin A. DSM-IV alcohol abuse: investigation in a sample of at-risk drinkers in the community. Journal of Studies on Alcohol. 1999;60:181–7. doi: 10.15288/jsa.1999.60.181. [DOI] [PubMed] [Google Scholar]
- Hasin D, Paykin A, Endicott J, Grant B. The validity of DSM-IV alcohol abuse: drunk drivers versus all others. Journal of Studies on Alcohol. 1999;60:746–55. doi: 10.15288/jsa.1999.60.746. [DOI] [PubMed] [Google Scholar]
- Hasin D, Van Rossem R, McCloud S, Endicott J. Alcohol dependence and abuse diagnoses: validity in community sample heavy drinkers. Alcoholism: Clinical and Experimental Research. 1997c;21:213–9. [PubMed] [Google Scholar]
- Hasin DS, Grant B, Endicott J. The natural history of alcohol abuse: implications for definitions of alcohol use disorders. American Journal of Psychiatry. 1990;147:1537–41. doi: 10.1176/ajp.147.11.1537. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Van Rossem R, McCloud S, Endicott J. Differentiating DSM-IV alcohol dependence and abuse by course: community heavy drinkers. Journal of Substance Abuse. 1997;9:127–35. doi: 10.1016/s0899-3289(97)90011-0. [DOI] [PubMed] [Google Scholar]
- Heinz A, Beck A, Grusser SM, Grace AA, Wrase J. Identifying the neural circuitry of alcohol craving and relapse vulnerability. Addiction Biology. 2008 doi: 10.1111/j.1369-1600.2008.00136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helzer JE, Bucholz KK, Gossop M. A dimensional option for the diagnosis of substance dependence in DSM-V. International Journal of Methods in Psychiatric Research. 2007;16(Suppl 1):S24–33. doi: 10.1002/mpr.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennrich RI, Sampson PF. Rotation for simple loadings. Psychometrika. 1966;31:313–23. doi: 10.1007/BF02289465. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Strong DR. A Rasch model analysis of DSM-IV Alcohol abuse and dependence items in the National Epidemiological Survey on Alcohol and Related Conditions. Alcoholism: Clinical and Experimental Research. 2006;30:1165–75. doi: 10.1111/j.1530-0277.2006.00140.x. [DOI] [PubMed] [Google Scholar]
- Kalivas PW, O’Brien C. Drug addiction as a pathology of staged neuroplasticity. Neuropsychopharmacology. 2008;33:166–80. doi: 10.1038/sj.npp.1301564. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Geier T, Grant B, Hasin D. Influence of a drinking quantity and frequency measure on the prevalence and demographic correlates of DSM-IV alcohol dependence. Alcoholism: Clinical and Experimental Research. 2009;33:761–771. doi: 10.1111/j.1530-0277.2009.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Geier T, Grant B, Hasin D. Influence of a drinking quantity and frequency measure on the prevalence and demographic correlates of DSM-IV alcohol dependence. Alcoholism: Clinical and Experimental Research. doi: 10.1111/j.1530-0277.2009.00894.x. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. Guilford Press; New York: 1998. [Google Scholar]
- Krueger RF, Nichol PE, Hicks BM, Markon KE, Patrick CJ, Iacono WG, McGue M. Using latent trait modeling to conceptualize an alcohol problems continuum. Psychological Assessessment. 2004;16:107–19. doi: 10.1037/1040-3590.16.2.107. [DOI] [PubMed] [Google Scholar]
- Langenbucher JW, Labouvie E, Martin CS, Sanjuan PM, Bavly L, Kirisci L, Chung T. An application of item response theory analysis to alcohol, cannabis, and cocaine criteria in DSM-IV. Journal of Abnormal Psychology. 2004;113:72–80. doi: 10.1037/0021-843X.113.1.72. [DOI] [PubMed] [Google Scholar]
- Li TK, Hewitt BG, Grant BF. The Alcohol Dependence Syndrome, 30 years later: a commentary. the 2006 H. David Archibald lecture. Addiction. 2007a;102:1522–30. doi: 10.1111/j.1360-0443.2007.01911.x. [DOI] [PubMed] [Google Scholar]
- Li TK, Hewitt BG, Grant BF. Is there a future for quantifying drinking in the diagnosis, treatment, and prevention of alcohol use disorders? Alcohol and Alcoholism. 2007b;42:57–63. doi: 10.1093/alcalc/agl125. [DOI] [PubMed] [Google Scholar]
- Lubke G, Muthen B. Performance of factor mixture models as a function of model size, covariate effects, and class-specific parameters. Structural Equation Modeling. 2007;14(1):26–47. [Google Scholar]
- Martin CS, Chung T, Kirisci L, Langenbucher JW. Item response theory analysis of diagnostic criteria for alcohol and cannabis use disorders in adolescents: implications for DSM-V. Journal of Abnormal Psychology. 2006;115:807–14. doi: 10.1037/0021-843X.115.4.807. [DOI] [PubMed] [Google Scholar]
- Martin CS, Chung T, Langenbucher JW. How should we revise diagnostic criteria for substance use disorders in the DSM-V? Journal of Abnormal Psychology. 2008;117:561–75. doi: 10.1037/0021-843X.117.3.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller NS, Goldsmith RJ. Craving for alcohol and drugs in animals and humans: biology and behavior. Journal of Addictive Disorders. 2001;20:87–104. doi: 10.1300/J069v20n03_08. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5. Los Angeles, CA: 2009. [Google Scholar]
- O’Brien CP. Anticraving medications for relapse prevention: a possible new class of psychoactive medications. American Journal of Psychiatry. 2005;162:1423–31. doi: 10.1176/appi.ajp.162.8.1423. [DOI] [PubMed] [Google Scholar]
- O’Brien CP, Childress AR, Ehrman R, Robbins SJ. Conditioning factors in drug abuse: can they explain compulsion? Journal of Psychopharmacology. 1998;12:15–22. doi: 10.1177/026988119801200103. [DOI] [PubMed] [Google Scholar]
- Oslin DW, Cary M, Slaymaker V, Colleran C, Blow FC. Daily ratings measures of alcohol craving during an inpatient stay define subtypes of alcohol addiction that predict subsequent risk for resumption of drinking. Drug and Alcohol Dependence. 2009;103:131–6. doi: 10.1016/j.drugalcdep.2009.03.009. [DOI] [PubMed] [Google Scholar]
- Proudfoot H, Baillie AJ, Teesson M. The structure of alcohol dependence in the community. Drug and Alcohol Dependence. 2006;81:21–6. doi: 10.1016/j.drugalcdep.2005.05.014. [DOI] [PubMed] [Google Scholar]
- Pull CB, Saunders JB, Mavreas V, Cottler LB, Grant BF, Hasin DS, Blaine J, Mager D, Ustun BT. Concordance between ICD-10 alcohol and drug use disorder criteria and diagnoses as measured by the AUDADIS-ADR, CIDI and SCAN: results of a cross-national study. Drug and Alcohol Dependence. 1997;47:207–16. doi: 10.1016/s0376-8716(97)00091-4. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ. Experience with ICD-10/DSM-IV substance use disorders. Psychopathology. 2002;35:82–8. doi: 10.1159/000065124. [DOI] [PubMed] [Google Scholar]
- Saha TD, Chou SP, Grant BF. Toward an alcohol use disorder continuum using item response theory: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2006;36:931–41. doi: 10.1017/S003329170600746X. [DOI] [PubMed] [Google Scholar]
- Saha TD, Stinson FS, Grant BF. The role of alcohol consumption in future classifications of alcohol use disorders. Drug and Alcohol Dependence. 2007;89:82–92. doi: 10.1016/j.drugalcdep.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ustun B, Compton W, Mager D, Babor T, Baiyewu O, Chatterji S, Cottler L, Gogus A, Mavreas V, Peters L, Pull C, Saunders J, Smeets R, Stipec MR, Vrasti R, Hasin D, Room R, Van den Brink W, Regier D, Blaine J, Grant BF, Sartorius N. WHO Study on the reliability and validity of the alcohol and drug use disorder instruments: overview of methods and results. Drug and Alcohol Dependence. 1997;47:161–9. doi: 10.1016/s0376-8716(97)00087-2. [DOI] [PubMed] [Google Scholar]
- Research Triangle Institute. Software for Survey Data Analysis (SUDAAN), Version 9.1. Research Triangle Park, NC: Research Triangle Institute; 2004. [Google Scholar]
- Schuckit MA, Smith TL, Landi NA. The 5-year clinical course of high-functioning men with DSM-IV alcohol abuse or dependence. American Journal of Psychiatry. 2000;157:2028–35. doi: 10.1176/appi.ajp.157.12.2028. [DOI] [PubMed] [Google Scholar]
- Vrasti R, Grant BF, Chatterji S, Ustun BT, Mager D, Olteanu I, Badoi M. Reliability of the Romanian version of the alcohol module of the WHO Alcohol Use Disorder and Associated Disabilities: Interview Schedule --Alcohol/Drug-Revised. European Addiction Research. 1998;4:144–9. doi: 10.1159/000018947. [DOI] [PubMed] [Google Scholar]
- Weiss F. Neurobiology of craving, conditioned reward and relapse. Current Opinion in Pharmacology. 2005;5:9–19. doi: 10.1016/j.coph.2004.11.001. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization; Geneva: 1993. [Google Scholar]
- Wu LT, Pan JJ, Blazer DG, Tai B, Stitzer ML, Brooner RK, Woody GE, Patkar AA, Blaine JD. An item response theory modeling of alcohol and marijuana dependences: a National Drug Abuse Treatment Clinical Trials Network study. Journal of Studies on Alcohol and Drugs. 2009;70:414–25. doi: 10.15288/jsad.2009.70.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.