Abstract
Objective
This study examined the effects of multichannel wide-dynamic range compression (WDRC) amplification and stimulus audibility on consonant recognition and error patterns.
Design
Listeners had either severe or mild-to-moderate sensorineural hearing loss. Each listener was monaurally fit with a wearable hearing aid using typical clinical procedures, frequency-gain parameters and a hybrid of clinically prescribed compression ratios for DSL (Scollie et al., 2005) and NAL-NL (Dillon, 1999). Consonant-vowel nonsense syllables were presented in soundfield at multiple input levels (50, 65, 80 dB SPL). Test conditions were four-channel fast-acting WDRC amplification and a control compression limiting (CL) amplification condition. Listeners identified the stimulus heard from choices presented on an on-screen display. A between-subject repeated measures design was used to evaluate consonant recognition and consonant confusion patterns.
Results
Fast-acting WDRC provided a considerable audibility advantage at 50 dB SPL, especially for listeners with severe hearing loss. Listeners with mild-to-moderate hearing loss received less audibility improvement from the fast-acting WDRC amplification, for conversational and high level speech, compared to listeners with severe hearing loss. Analysis of WDRC benefit scores revealed that listeners had slightly lower scores with fast-acting WDRC amplification (relative to CL) when WDRC provided minimal improvement in audibility. The negative effect was greater for listeners with mild-to-moderate hearing loss compared to their counterparts with severe hearing loss.
Conclusions
All listeners, but particularly the severe loss group, benefited from fast-acting WDRC amplification for low-level speech. For conversational and higher speech levels (i.e., when WDRC does not confer a significant audibility advantage), fast-acting WDRC amplification appears to slightly degrade performance. Listeners’ consonant confusion patterns suggest that this negative effect may be partly due to fast-acting WDRC-induced distortions which alter specific consonant features. In support of this view, audibility accounted for a greater percentage of the variance in listeners’ performance with CL amplification compared to fast-acting WDRC amplification.
Keywords: severe hearing loss, wide dynamic range compression, audibility, hearing aids, consonant confusions, feature analysis
Introduction
At present, at least 83% of clinically dispensed hearing aids are digital, with some form of non-linear algorithm (Strom, 2006). The benefit of non-linear wide dynamic range compression (WDRC) amplification is well documented in listeners with mild-to-moderate hearing loss. Common advantages for these listeners include improved audibility of low-level speech (e.g., Kam & Wong, 1999; Moore & Glasberg, 1986; Souza, 2002; Souza & Turner, 1998), improved recognition for speech in quiet (e.g., Moore, Johnson, Clark & Pluvinage, 1992), and under some circumstances, for speech in noise (Moore, Peters & Stone, 1999). Subjective benefits of wide dynamic range compression include listening comfort for loud speech (Boike & Souza, 2000; Davies-Venn, Souza & Fabry, 2007; Jenstad, Seewald, Cornelisse & Shantz, 1999; Kam & Wong, 1999; Larson, Williams, Henderson, Luethke, Beck,. et al., 2002; Lunner, Hellgren, Arlinger & Elberling, 1997; Souza, 2002), and pleasantness (Davies-Venn, Souza & Fabry, 2007; Kam & Wong, 1999).
The effects of fast-acting WDRC amplification have been studied extensively in listeners with mild-to-moderate hearing loss, but listeners with severe hearing loss have not received a similar scope of evaluation. There is also a lack of consensus among studies that have evaluated listeners with severe hearing loss regarding whether these listeners can attain all the potential benefits of wide dynamic range compression. Some studies have noted that listeners with severe hearing loss can achieve these benefits (Barker, Dillon & Newall, 2001; Kam & Wong, 1999; Marriage & Moore, 2003; Marriage, Moore, Stone & Baer, 2005), while others have suggested that the listeners with severe hearing loss may show detrimental effects of fast-acting WDRC processing (Byrne & Dillon, 1986; Plomp, 1994; Souza & Bishop, 1999; Souza et al., 2005; Verschuure, Prinsen & Dreschler, 1994; Verschuure, Benning, Van Cappellen, Dreschler & Boeremans, 1998).
Of studies that evaluated speech recognition with fast-acting WDRC amplification on listeners with severe hearing loss, Kam and Wong (1999) revealed that these listeners performed better with fast-acting WDRC amplification than with linear amplification for recognition of low-level speech in quiet. A non-significant difference was found between fast-acting WDRC amplification and CL amplification for perceived clarity across all input levels (50, 65, and 80 dB SPL). Listeners were given individualized compression ratios averaging 2.35 across all subjects. They were tested using Cantonese monosyllabic words and sentences in noise. Although this study made a direct comparison between these two amplifications using different input levels, it is difficult to generalize results because the test materials were made using a tonal language with different intonation patterns compared to English syllables. For listeners with mild-to-moderate hearing loss, the perceptual weight of temporal cues is different between English and a tonal language (Fu, Zeng, Shannon & Soli, 1998). In addition, single-channel compression is now rarely used in the clinic and multichannel compression causes other acoustic distortions (Bor, Souza & Wright, 2008) that may not have occurred in the single channel device used by Kam and Wong (1999).
Marriage et al. (2005) compared multichannel WDRC amplification to peak clipping and compression limiting amplification in children. Their listeners were clinically fit with BTE hearing aids and tested using word, sentence and phrase rating and recognition tasks. The results from their small set of listeners with severe hearing loss (N=6) revealed better performance with the multichannel WDRC amplification when compared to linear amplification. An earlier study conducted by Marriage and Moore (2003) revealed similar results on a speech perception task using WDRC amplification on three children with severe hearing loss.
Some studies have shown better performance for linear amplification. DeGennaro, Braida, and Durlach (1986) evaluated listeners with severe hearing loss and their results showed that although WDRC amplification improved audibility, it did not provide measurable benefit over linear amplification. Albeit their use of a small subject sample and extremely fast time constants, their protocol which used 16-channel compression with fast time constants, may have introduced a type of temporal distortion similar to today’s advanced-technology hearing aids. Boothroyd, Springer, Smith and Schulman (1988) evaluated eight listeners with severe to profound hearing loss and their results also showed reduced performance with compression compared to linear amplification for seven of the eight subjects. A recent study by Souza, Jenstad and Folino (2005) compared scores of 13 listeners with severe hearing loss on an identification task using consonant-vowel nonsense syllables. Speech stimuli were processed using peak clipping (PC), CL, two-channel WDRC and three-channel WDRC amplification. This study used a simulated hearing aid with a 3:1 compression ratio and short attack (3 msec) and release (25 msec) time constants. Overall, scores for the listeners with severe hearing loss revealed better performance with CL amplification compared to three-channel WDRC amplification.
One shortcoming of the Souza et al. (2005) study was use of the same frequency-gain response for all listeners, which might not have set audibility to an optimal level for each individual. Even though this was a well-controlled test of compression, the usage of a laboratory-based hearing aid did not allow for consideration of the interrelationships between fast-acting WDRC and other processing, as would occur in a commercial aid where fast-acting WDRC would normally be combined with compression limiting and the net effect would dictate performance. Finally, that study used only a single (conversational) input level and audibility was not quantified or used to evaluate improvement in scores or lack thereof with fast-acting WDRC compared to CL.
A recurring discrepancy between recent studies that do and those that do not provide support for using fast-acting WDRC amplification in listeners with severe hearing loss is the use of clinically-fit hearing aids (e.g. Kam & Wong, 1999; Marriage & Moore, 2003; Marriage et al., 2005) versus laboratory-based hearing aid simulations (e.g. DeGennaro et al., 1986; Souza & Bishop, 1999, Souza et al., 2005). Studies which have used clinically-fit hearing instruments used individualized frequency gain responses and in some cases individualized compression parameters. Most laboratory-based studies which used simulated hearing aid responses employed an average frequency-gain response with common compression parameters. This type of protocol may limit generalization of results to clinical settings.
Accordingly, in the present study clinically fit hearing instruments with fast-acting multichannel fast-acting WDRC amplification as well as CL amplification were used to process speech stimuli presented at multiple input levels. It was hypothesized that the listeners with severe hearing loss would receive less improvement in performance from fast-acting WDRC (relative to CL) with increase in audibility compared to listeners with mild-to-moderate hearing loss.
Methods
Subjects
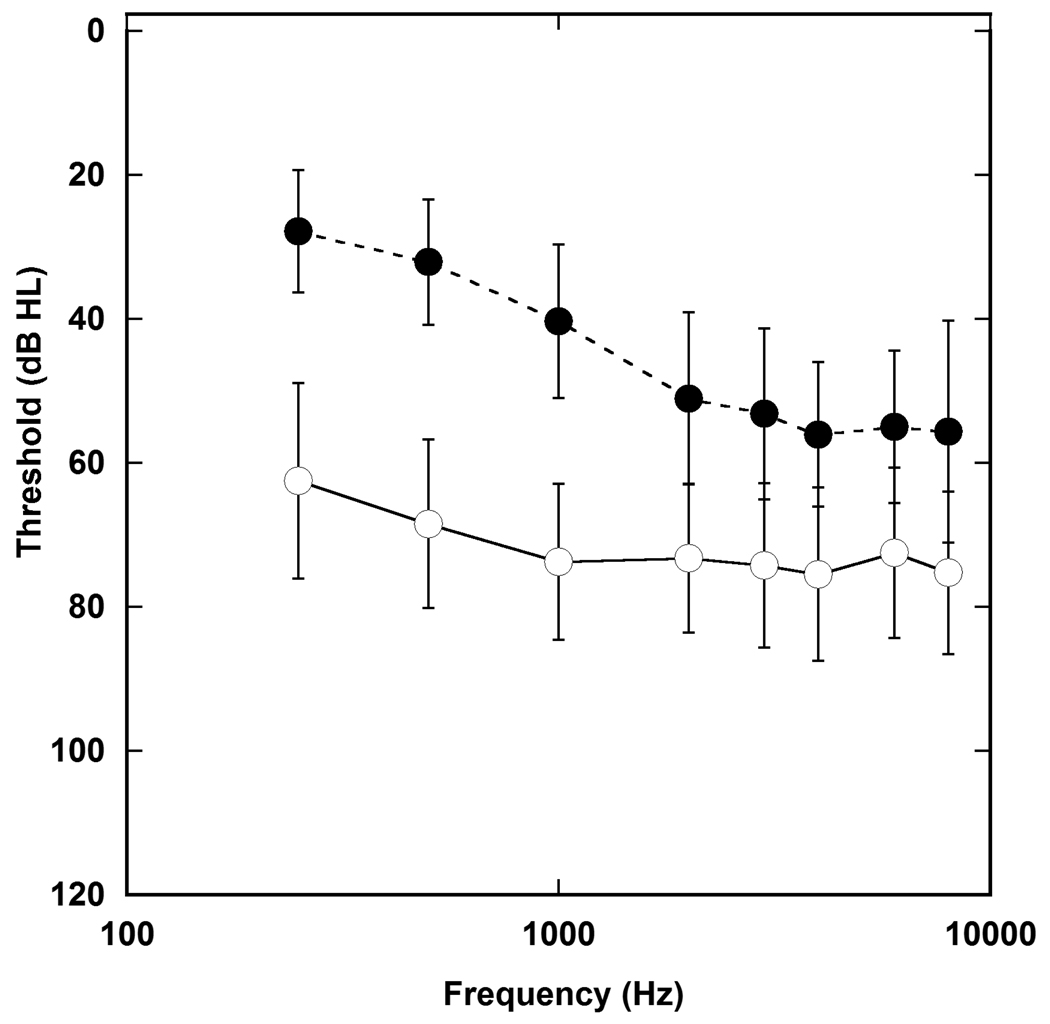
Two age-matched groups of listeners were recruited to participate in this study. Twenty-two of the participants (mean age of 60 years, range 22 to 89 years) were classified as listeners with severe hearing loss. Severe hearing loss was defined as pure tone average (0.5, 1 and 2 kHz) thresholds from 65 to 90 dB HL. Fifteen of the participants were classified as listeners with mild-to-moderate hearing loss (mean age of 66 years, range 30 to 90 years). Mild-to-moderate hearing loss was defined as pure tone average (PTA) thresholds from 25 to 55 dB HL. One subject with mild-to-moderate hearing loss had an asymmetrical loss and data were also collected using the other ear for inclusion in the severe group. The groups were not statistically different in age t (32) = −1.06, p = 0.30. Each listener’s loudness discomfort levels (LDLs) were obtained for .5 and 3 kHz warble tones (see Table 1), using standard instructions as recommended by Hawkins, Walden, Montgomery and Prosek (1987). All listeners had sensorineural hearing loss which was defined as the absence of an air-bone gap greater than 10 dB HL from 500 Hz to 4000 Hz and normal (Type A) tympanograms (Jerger, 1970). Acoustic reflex thresholds and acoustic reflex decay were obtained to rule out retrocochlear pathology for subjects with asymmetrical hearing loss. Test ear was determined based on the ear which best fit the inclusion criteria. When both ears met the study criteria, the ear with better word recognition score was chosen. Figure 1 illustrates the mean thresholds and standard deviations for the test ear of both groups.
Table 1.
Mean loudness discomfort levels (LDL) and real ear saturation response (RESR) for WDRC and CL.
| Frequency(Hz) | LDL(dB SPL) | WDRC (dB SPL) | CL(dB SPL) |
|---|---|---|---|
| Mild-to-moderate | |||
| 500 | 105 | 92 | 99 |
| 3000 | 107 | 105 | 112 |
| Severe | |||
| 500 | 107 | 101 | 107 |
| 3000 | 112 | 110 | 111 |
Figure 1.
Mean threshold and ±2 standard deviations for listeners with mild-to-moderate hearing loss (filled circles) and listeners with severe hearing loss (open circles). Mean pure tone averages (PTA) were 41 dB HL for the group with mild-to-moderate loss and 71 dB HL for the group with severe hearing loss
All subjects spoke English as their first or primary language. All subjects had sensorineural hearing loss. Mean pure tone average (PTA) was 72 dB HL (SD = 9.3) for the severe group and 41 dB HL (SD = 7.6) for the mild-to-moderate group. Fourteen of the listeners with severe hearing loss wore hearing aids in both ears, three wore a hearing aid in one ear and five did not have hearing aid experience. Three of the unaided listeners with severe hearing loss had normal hearing in their non-test ear. The fourth unamplified listener had a mild hearing loss in the other ear; the fifth unaided listener had borderline severe thresholds with PTA of 63 dB HL and stated that she had not obtained amplification due to more pressing health needs. Only four of the listeners with mild-to-moderate hearing loss had amplification in one or both ears.
Unaided word recognition testing was administered at 30 to 40 dB sensation level (SL) re: PTA, using a 25 word list of the Northwestern University (NU-6) recording (Wilson, Zizz, Shanks & Causey, 1990). Mean scores for the test ear were 62% (SD = 24.1) for the severe group and 93% (SD = 6.36) for the mild-to-moderate group. Two lists of the QuickSIN test (Killion, Niquette, Gudmundsen, Revit & Banerjee, 2004) were administered at 70 dB HL for the mild-to-moderate group and most comfortable loudness level (MCL) for the severe group. Speech in noise recognition (SNR) loss was determined using the protocol recommended by the test developers. Mean SNR loss was 7.1 dB (range .5 to 18 with STD of 4.3) for the mild-to-moderate group and 12.7 dB (range 1 to 25 with STD of 6.7) for the severe group. Two subjects with severe hearing loss and one with mild-to-moderate loss (S3, S8 and MM1) were unable to complete all test sessions in the fast-acting WDRC amplification condition due to unrelated health issues. Listeners were compensated on an hourly basis for their participation in this study.
Hearing Instrument
The hearing instrument was a commercial 16-band, behind-the-ear (BTE) hearing aid. This device had a fitting range that was appropriate for listeners with mild-to-profound hearing loss. The hearing instrument employed a high-level front-end (i.e. pre-amplifier) compressor, low-level expansion, and automatic gain controls for both input (AGCi, WDRC) and output (AGCo) acoustic signals. The hearing instrument had four independent channels with cross over frequencies of .63, 1.6 and 3.2 kHz. This device also had four memories with flexible compression controls that allowed both linear (CL) and fast-acting WDRC to be programmed into individual memories.
The first two memories of the hearing instrument were programmed with parameters consistent with fast-acting WDRC and CL amplification. Feedback cancellation was activated when an acceptable match to prescribed target gain could not be attained without feedback. All other adaptive features including directional microphones were disabled. The volume control and memory switch were also disabled to ensure accuracy in data collection.
The memory programmed with compression limiting (CL) had a dual limiter (i.e. high level front-end compressor + AGC0). The front-end limiter had a threshold of 102 dB SPL. The threshold for the back-end limiter was driven by the maximum power output (MPO), which could be set between 111 dB SPL and 132 dB SPL. On average our listeners with severe hearing loss were fit with an adjusted MPO of 122 dB SPL for CL amplification. Listeners with mild-to-moderate loss were fit with an MPO of 121 dB SPL for CL amplification. Both front and back end limiters employed a 10:1 compression ratio, an attack time of less than 1 msec and a release time of approximately 90 msec.
The fast-acting WDRC program employed a broadband equivalent input compression kneepoint of 45 dB SPL, coupled with a wide-band output limiter. The attack and release times were approximately 5 msec and 100 msec. Compression kneepoints and time constants were identical across the four compression channels. On average our listeners with severe hearing loss were fit with a maximum output of 129 dB SPL for fast-acting WDRC amplification. Listeners with mild-to-moderate loss were fit with an adjusted MPO of 126 dB SPL for fast-acting WDRC amplification. Excluding the compression ratios, all other compression parameters were identical for both listener groups. In choosing the compression ratios, the range that would be considered clinically reasonable across various prescriptive procedures was considered. For example, for the severe group, NAL-NL1 (Dillon, 1999) prescribed compression ratios between 1.3:1 and 2.5:1 while DSL version 5.0 (Scollie et al., 2005) prescribed compression ratios between 2.8:1 and 4.3:1. For listeners with mild-to-moderate hearing loss, NAL-NL1 (Dillon, 1999) prescribed ratios between 1.2:1 and 1.9:1 and DSL version 5.0 prescribed ratios between 1.4:1 and 3.4:1.
Because audibility was a potential experimental confound especially for listeners with severe hearing loss we optimized audibility by selecting a higher prescribed compression ratio. That is, the main goal was to make clinically reasonable choices that also supported the specific aims of this study, rather than to present the compression ratio prescribed by any specific fitting protocol. The severe group was fit using a 3.2:1 compression ratio, while the mild-to-moderate group had a 2:1 compression ratio. Previous studies (e.g. Braida, Durlach, De Gennaro, Peterson, & Bustamante, 1982; Souza & Turner, 1999; Stelmachowicz, Lewis & Cruetz, 1994; Verschuure, Maas, Stikvoort, Jong, Goedegebure, & Dreschler, 1996) have also shown that the effective compression ratio for speech will be considerably lower than the nominal compression ratios specified here.
Finally, results on a similar consonant recognition task revealed no significant difference F (1, 13) = .481, p = .500 in performance when the same group of listeners with mild-to-moderate hearing loss was tested using a uniform (i.e. 2:1) compression ratio compared to NAL-NL1 individually-prescribed compression ratios (Davies-Venn & Souza, 2008). Albeit a smaller sample size, two listeners from the severe group also revealed similar speech recognition scores (56% vs. 58% correct) with individually-prescribed compression ratios versus the uniform compression ratios used in this study.
Hearing Aid Fitting
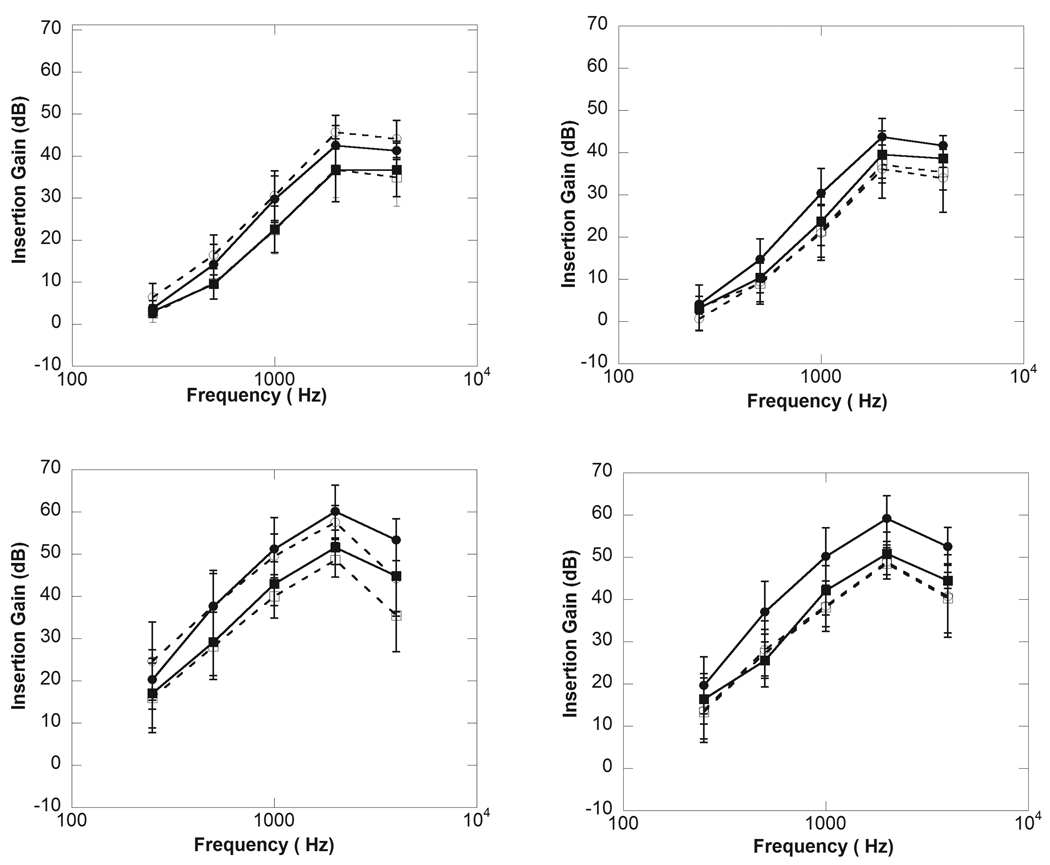
The test hearing instrument was monaurally fit on each subject using individual NAL-NL1 (Dillon, 1999) insertion gain targets for 65 dB SPL. An unvented, custom-made skeleton earmold was coupled to the BTE test instrument using standard size 13 tubing. A 65 dB SPL composite noise was presented from a speaker, positioned at 45 degrees azimuth and 12 inches from the subject’s ear. A probe tube was positioned at 5 mm beyond the medial tip of each listener’s earmold and insertion gain measures were used to adjust each listener’s frequency gain response to their prescribed NAL-NL1 gain targets. Figure 2 illustrates mean real-ear match to prescribed target gain for both listener groups at 50 and 65 dB SPL.
Figure 2.
Mean for match to prescribed target gain for listeners with mild-to-moderate hearing loss for fast-acting WDRC (top left panel) and CL amplification (top right panel) amplification. The bottom left and right panels illustrate mean match to target gain for listeners with severe hearing loss for fast-acting WDRC (bottom left) and CL (bottom right) amplification. The filled circles bars represent prescribed target gain at 50 dB SPL; the open circles represent real-ear insertion gain (REIR) at 50 dB SPL. The filled squares represent prescribed target gain at 65 dB SPL; the open squares represent real-ear insertion gain (REIR) at 65 dB SPL. The error bars represent ±1 standard deviation about the mean.
All of the testers were certified clinical audiologists and adjusted the hearing aid frequency-gain response as they would in a clinical situation. Each listener’s gain response was adjusted using the 65 dB SPL signal only. The set compression ratios in the fast-acting WDRC program were allowed to determine gain for low and high level signals. Real-ear saturation response (RESR) was measured for each program using a 90 dB SPL pure-tone sweep. The maximum power output (MPO) was adjusted if needed to ensure that the RESR was below the listener’s measured LDL at 0.5 and 3 kHz.
Upon completion of the hearing aid fitting, settings were saved onto the hearing instrument. Each listener was instructed on the behavioral task and their non-test ear was occluded with an earplug. For the three listeners with unilateral hearing loss, noise was applied at an effective masking level to the non-test ear. To ensure that the effective masking level also avoided over-masking, the amount of inter-aural crossover was determined on an individual basis using real-ear analysis. Speech noise was presented to the non-test ear at an individually pre-determined level (i.e. range 55 to 65 dB SPL) which ensured effective masking while preventing over-masking.
Procedure
A repeated-measures design was used to evaluate objective performance and consonant confusion patterns for both listener groups. The test stimuli was a set of 22 consonant-vowel /Ci/ nonsense syllable tokens from the Nonsense Syllable Test (NST) (Resnick, Dubno, Hoffnung & Levitt, 1975) spoken by a female talker. Nonsense syllables were used because they allowed evaluation of listeners’ perception of specific consonant features that were susceptible to distortions resulting from non-linear hearing aid processing. A study by Flynn, Dowell and Clark (1998) reported varied linguistic effects when listeners with severe hearing loss were evaluated with sentences compared to monosyllabic words. Thus, our choice of nonsense syllables minimized the differential effect of listeners’ metalinguistic skills, which have been shown to influence recognition of sentences (Boothroyd & Nittrouer, 1998). The vowel /i/ also provided sufficient difficulty to avoid ceiling effects in the mild-to-moderate group (Gutnick, 1982). At the completion of this study, each subject had responded to a total of 1,320 test tokens, over two 3-hour sessions. Only one vowel context was evaluated due to time constraints and the large number of response tokens measured.
All test stimuli were presented at zero degrees azimuth in sound field using a speaker (JBL LSR25P) positioned at head level, one meter from the subjects. A concatenated recording of the nonsense syllables was played through the system and its level was calibrated using a Bruel and Kjaer (B&K) 2204 sound level meter. Test stimuli were presented at 50, 65, and 80 dB SPL.
Subjects were trained to select the stimulus heard from a touch-screen display of 22 orthographically represented (e.g., “chee”, “see”) nonsense syllable tokens. Correct answer visual feedback was used during practice trials. Practice trials were presented using fast-acting WDRC amplification at 65 dB SPL. Data collection commenced after asymptotic performance was attained (± 5% for three consecutive practice trials). Each subject was tested under six conditions (i.e. 2 amplification and 3 presentation levels) and the order of conditions was randomized across subjects. Scores for each condition were averaged across 220 presentations (10 repetitions of 22 tokens) of the nonsense syllable tokens. All testing was conducted in a double-walled sound-isolating booth.
Audibility
To determine the influence of audibility, the Aided Audibility Index (AAI) was calculated for all test conditions. The AAI was calculated using the Stelmachowicz et al. (1994) method, with the modifications suggested by Souza and Turner (1998). Subject audiograms were converted from dB HL to dB SPL at the tympanic membrane using individually measured real-ear-to-dial-difference values. Octave thresholds were converted into third-octave centered frequencies from 160 Hz to 8000 Hz using the formula by Pittman and Stelmachowicz (2000). To determine the speech input level, the unamplified speech tokens were concatenated, presented, and recorded where the subject’s head would have been. Using Matlab (Mathworks) and a computer program written by Couvereur (1997) the root mean square (rms) SPL was measured for each third-octave band of the concatenated stimuli, using a non-overlapping window of 100 ms. The AAI was calculated as
where I equals the third-octave band frequency importance weighting functions for nonsense syllables from ANSI (1997), sl equals the calculated third-octave band centered sensation levels, and mcr equals the mean nominal speech compression ratio (from figure B-1 in Stelmachowicz et al. (1994):1 for CL, 1.2 for fast-acting WDRC in the mild-to-moderate group, and 2 in the severe group). sl was calculated as
where rms was the measured concatenated speech input level specified earlier, mic was the third-octave center band microphone correction factor from Bentler and Pavlovic (1989), mcr was the mean speech compression ratio specified earlier, real-ear was the measured real ear insertion gain for the appropriate test condition, and threshold was the subject’s third octave threshold in dB SPL. The variable limit was calculated using the formula specified by Stelmachowicz et al. (1994)
where SSPL 90 was the measured maximum output1.
Results
Absolute Scores
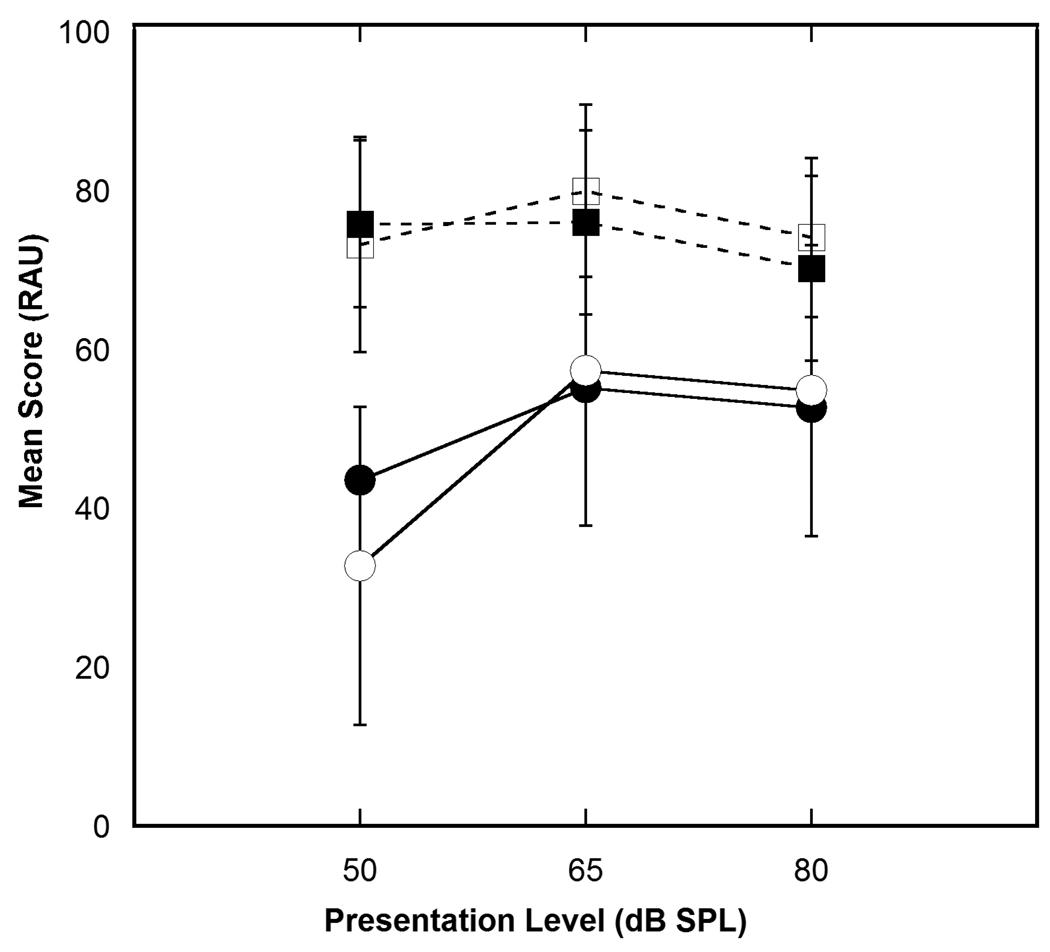
Listeners with mild-to-moderate hearing loss performed better than listeners with severe hearing loss. Absolute percent correct scores transformed to rationalized arcsine units (RAU) (Sherbecoe & Studebaker, 2004; Studebaker, 1985) are presented in Figure 3. Although the listeners with severe hearing loss had lower scores than their counterparts with mild-to-moderate hearing loss, the pattern of performance across input level was similar for both groups. Compared to CL, scores were improved with fast-acting WDRC at 50 dB SPL and either remained unchanged or decreased slightly at 65 and 80 dB SPL. The errors bars in Figure 3 indicate higher variance in performance within listeners with severe hearing loss compared to listeners with mild-to-moderate hearing loss.
Figure 3.
Mean scores in RAU for fast-acting WDRC (filled circles) and CL (open circles) for listeners with severe hearing loss. The squares represent mean RAU scores for fast-acting WDRC (filled) and CL (open) for listeners with mild-to-moderate hearing loss. Error bars represent ± 2 standard deviations about the mean.
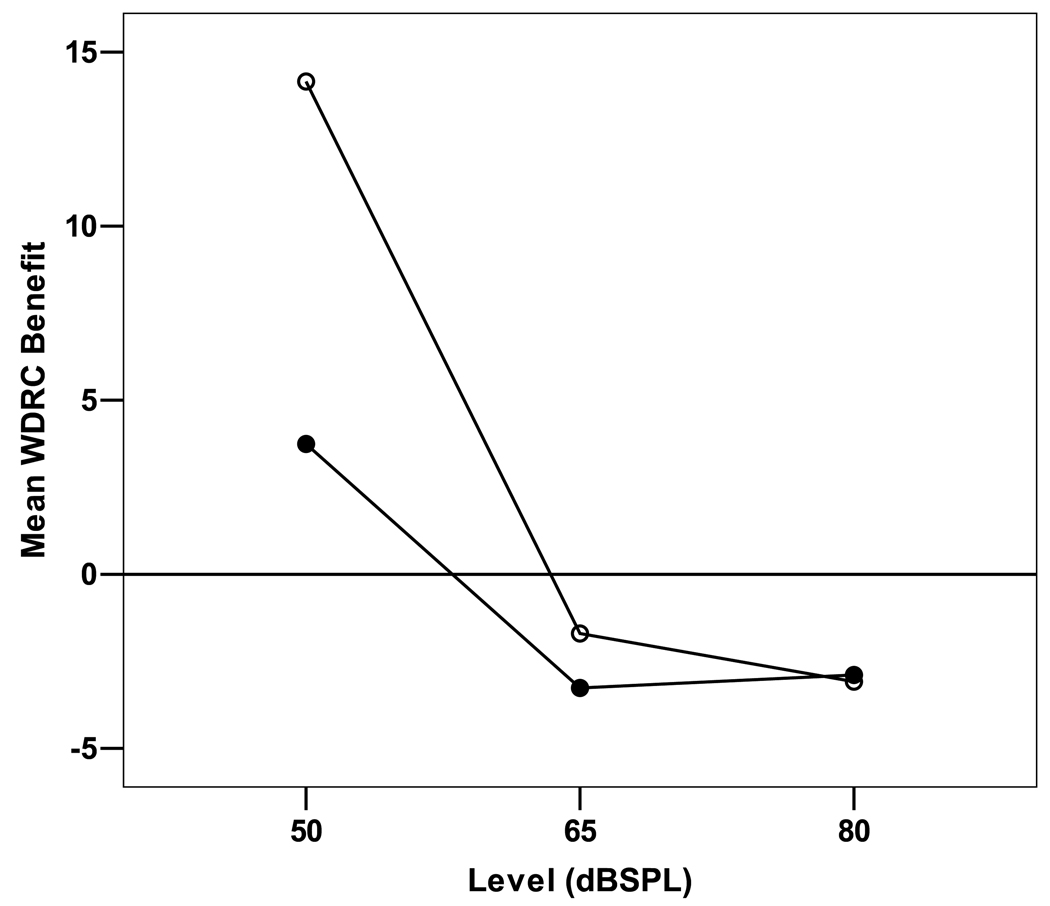
WDRC Benefit
The main interest of this study was to evaluate the effect of level and audibility on improvement in performance with fast-acting WDRC compared to CL amplification for listeners with severe and mild-to-moderate hearing loss. Therefore, listeners’ percent correct scores were converted to WDRC benefit. WDRC benefit was defined as the score (in RAU) in the fast-acting WDRC condition minus score (in RAU) in the CL condition.
A two-way repeated measures ANOVA was performed to evaluate the effect of level2 on WDRC benefit. The within-subject factor was input level (50, 65 and 80 dB SPL). The between-subject factor was group (mild-to-moderate and severe). The interaction between group and level was not significant, F (1.4, 44.96) = 2.224; p = .134. The main effect of level was significant, F (1.4, 44.96) = 12.553; p < .001. Paired-sample t-tests were performed to assess this level effect. Results indicated that listeners’ WDRC benefit was statistically higher for 50 versus 65 dB SPL, t (33) = 3.880, p < .001 as well as 50 versus 80 dB SPL, t (33) = 4.163, p <.001. The WDRC benefit was not statistically different for 65 versus 80 dB SPL, t (33) = .425, p = .673. These results suggest that for both group of listeners, improvement in performance with fast-acting WDRC amplification was greatest for soft speech (i.e. 50 dB SPL) compared to conversational and high level speech. The main effect of group was marginally significant at a p-value of .06, F (1, 32) = 3.869; p = .058. Taken together the results show weak evidence that listeners with severe hearing loss received more WDRC benefit compared to their counterparts with mild-to-moderate hearing loss.
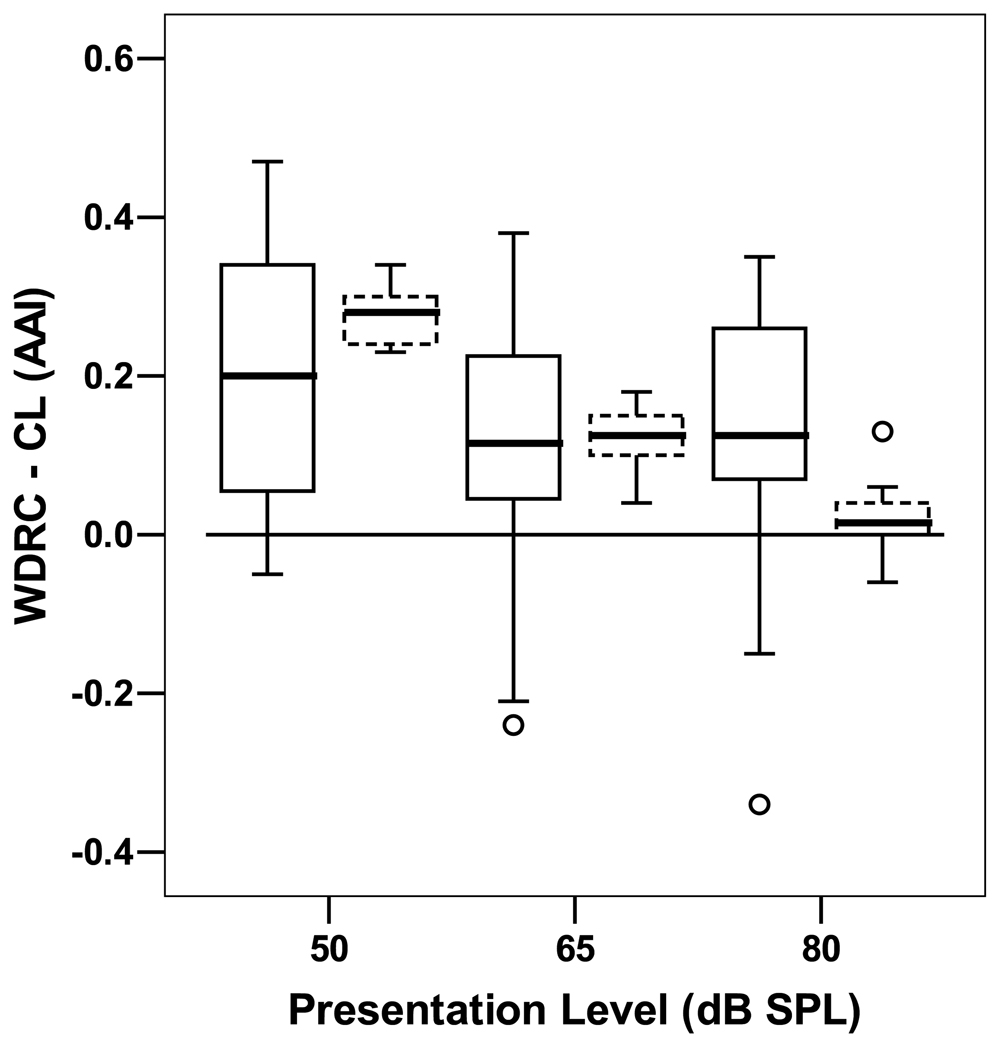
Audibility
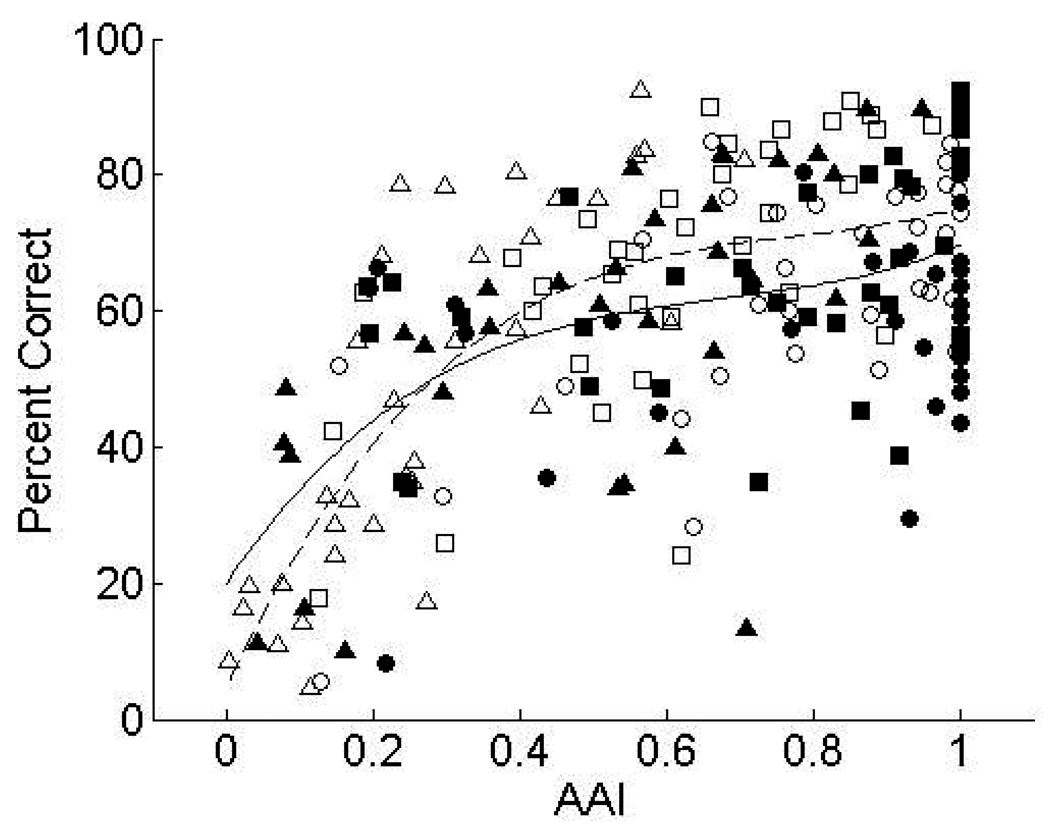
To investigate the role of audibility on WDRC benefit, audibility was quantified using the Aided Audibility Index (AAI) as described earlier. The correlation between AAI and WDRC benefit scores (i.e. WDRC minus CL) was significant r (100) = .20, p <. 001 across both WDRC and CL. Figure 5 shows a stronger positive correlation between audibility (AAI) and absolute recognition scores for CL (R2 = .469) compared to fast-acting WDRC (R2 = .254) amplification. This figure also shows considerable variability in the data.
Figure 5.
Scatter plot representing Aided Audibility Index values (x-axis) versus percent correct score (y-axis). The filled symbols represent fast-acting WDRC amplification and the unfilled symbols represent CL amplification. The triangles represent 50dB SPL; the squares represent 65dB SPL; and the circles represent 80 dB SPL. The regression lines represent the relationship between percent correct score and AAI for CL (dotted) and fast-acting WDRC (solid) amplification.
Discussion
In general, auditory filter bandwidths broaden as thresholds increase (Dubno & Dirks, 1990; Laroche ,Hetu, Quoc, Josserand, & Glasberg, 1992). Broadened auditory filters result in reduced spectral resolution abilities especially for listeners with severe hearing loss. Consequently, these listeners might rely more on temporal rather than spectral cues, perhaps rendering them more susceptible to temporal distortion from fast-acting WDRC amplification. Our working hypothesis was that listeners with severe hearing loss would show reduced benefit with fast-acting WDRC amplification because they are more susceptible to temporal distortion from fast-acting WDRC amplification (e.g., Jenstad & Souza, 2005) than listeners with mild-to-moderate hearing loss.
This hypothesis was not supported by the results because (1) a marginal but non-significant difference (p = 0.058) in recognition scores was found between the two groups. (2) Even if we consider the fact that the between-group difference approached significance, Figure 4 suggests this is due to greater benefit for the severe hearing loss group, particularly at the lower input levels. Presumably, this was because the listeners with severe hearing loss benefited most from the improved audibility provided by fast-acting WDRC amplification. Figure 6 shows the improvement in AAI with fast-acting WDRC relative to CL for each input level and subject group. Several points are apparent from this figure. (1) There is more variability in the audibility benefit of fast-acting WDRC amplification for the severe loss group. (2) Listeners with mild-to-moderate loss had slightly greater audibility improvement for the 50 dB SPL input level, but with less improvement in speech recognition (see Figure 4). However, this relationship needs to be considered in the context of their higher overall scores. Because the shape of the function relating audibility to recognition is not linear (Amlani, Punch & Chung, 2002), it is likely that the lower WDRC benefit for this group was due to both CL and fast-acting WDRC recognition scores falling in the highest (asymptotic) portion of the function. This assumption was not evaluated because the small N and single vowel /i/ context did not allow sufficient data points to generate a transfer function to predict performance in each condition. (3) Listeners with severe hearing loss continued to experience audibility improvement with WDRC, even at the highest input level. Despite this continued improvement in audibility, they show no greater benefit than the mild-moderate group.
Figure 4.
Mean WDRC (i.e. WDRC minus CL score) benefit score in RAU across level for each listener group. Data points above the zero line indicate better performance with fast-acting WDRC amplification and data points below this line indicate better performance with CL amplification. Open circles represent listeners with severe hearing loss and filled circles represent listeners with mild-to-moderate hearing loss.
Figure 6.
Box plots representing main AAI difference (fast-acting WDRC minus CL) across level for listeners with mild-to-moderate hearing loss (dotted) and listeners with severe hearing loss (solid).
It is also of interest that mean WDRC benefit was negative (i.e. better performance with the CL condition) at 65 and 80 dB SPL (Figure 4). It is possible that once optimum audibility is achieved, susceptibility to WDRC-induced distortion does occur. This pattern can also be seen by the shallower slope of the fast-acting WDRC line versus the CL line in Figure 5. Put differently, the audibility benefits of fast-acting WDRC dominate for low level speech whereas subtle distortion from fast-acting WDRC begins to dominate at conversational and higher speech input levels. Recall also that as the input level increased, there was an increased likelihood that the high-compression ratio output limiting was activated, and the output signal represented the combined effects of fast-acting WDRC processing and compression limiting.
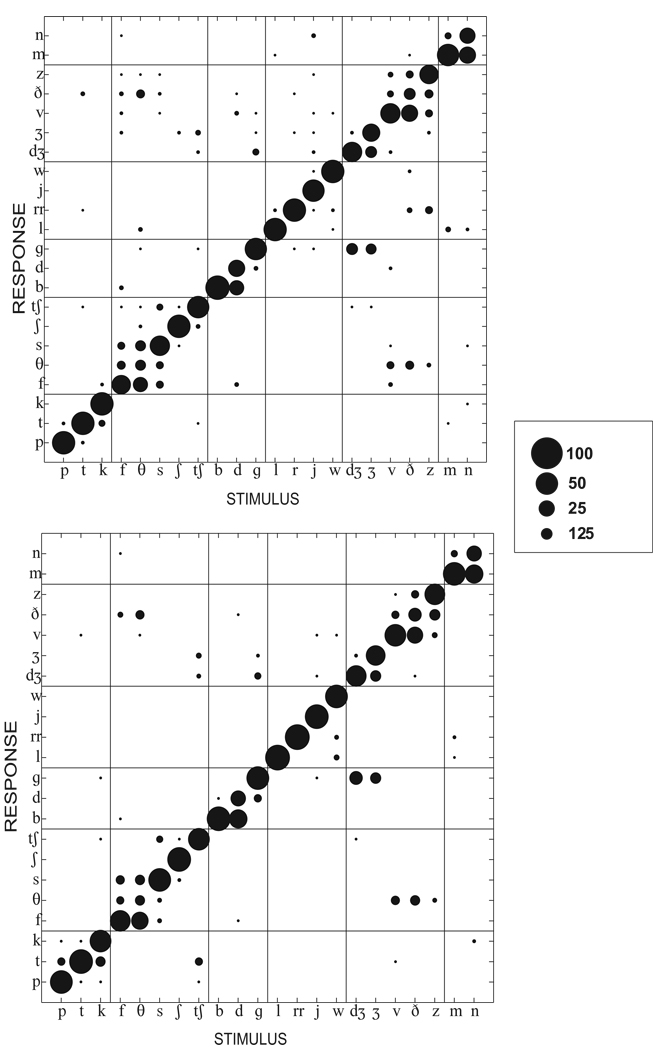
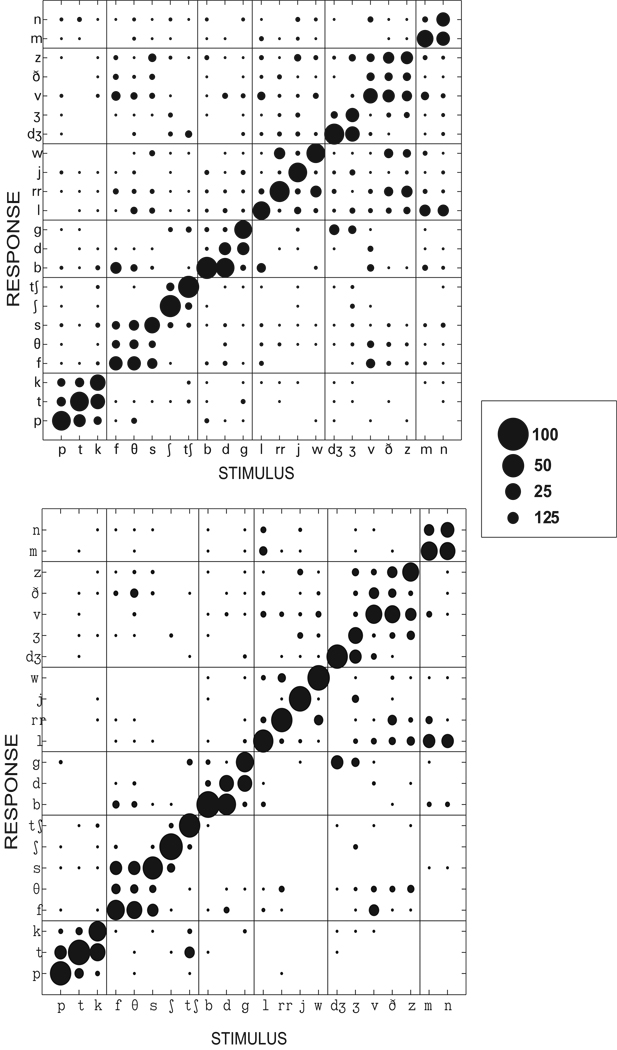
What, exactly, is happening to the acoustic signal to cause reduced recognition from WDRC at higher input levels? Acoustic cues for recognition of different phoneme categories (Kent & Read, 2002) suggest that some consonant features may be more susceptible than others to modifications resulting from fast-acting WDRC amplification. Thus, it was also of interest to examine the specific consonant errors made by both listener groups. One potential factor was temporal distortion caused by WDRC. Listeners with severe hearing loss, due to reduced spectral resolution, might rely more on temporal cues than listeners with mild-moderate hearing loss. Additionally, temporal cues are more likely to be distorted for the group with severe hearing loss because of the compression parameters required to provide sufficient hearing aid gain (i.e. low kneepoints, high compression ratios).
Consonant confusions support the idea that listeners with severe hearing loss exhibit susceptibility to fast-acting WDRC-induced temporal distortions. This type of signal processing has been proposed to alter temporal envelope cues (Boothroyd et al, 1988; Jenstad & Souza, 2005) which are cues to consonant manner (Rosen, 1992). The most common (non-place) confusions observed were made between affricates and stops, or between fricatives and affricates. For example, listeners with mild-to-moderate loss (Figure 7) responded /γι/ for either /δZι/ or /Zι/. Listeners with severe hearing loss (Figure 8) made that error as well as responding / τι / as in Tom for / τΣι / as in CHair.
Figure 7.
Scatter plot of consonant errors for listeners with mild-to-moderate hearing loss for WDRC 50 dB SPL (upper panel) and 65 dB SPL (lower panel). Circles along the diagonal represent correct responses. Circles off the diagonal and within a specific grid represent place of articulation errors and other circles off the diagonal represent consonant manner and voicing errors. The legend represents mean percent correct correct or incorrect responses.
Figure 8.
Scatter plot of consonant errors for listeners with severe hearing loss for WDRC 50 dB SPL (upper panel) and 65 dB SPL ( lower panel).
Another possible reason for these confusions may be due to level-induced distortions from output limiting in combination with the high presentation level of the amplified speech at 65 dB SPL and 80 dB SPL. Studies have shown that the cues to consonant perception changes in quiet versus noise (e.g. Kent & Read, 2002). For example, while phoneme rise time is a salient cue to affricate perception in quiet, listeners drop this cue and use duration for affricate perception in noise (Van Heuven, 1987). The factors driving consonant confusions for normal hearing listeners in noise would not necessarily be the same as the factor driving consonant confusions for amplified speech presented in quiet for listeners with mild-to-moderate and severe hearing loss. Thus, level-induced distortion may not be reason for the affricate for stops confusions noted in these listeners.
On the other hand, the greater gain and higher MPO settings for fast-acting WDRC compared to CL amplification may have contributed to the stop/affricate errors observed for listeners with severe hearing loss. The MPO differences between the fast-acting WDRC and CL settings were 5 dB for listeners with mild-to-moderate hearing loss and 7 dB SPL for the listeners with severe hearing loss. This was a relatively small difference and may not have affected the overall confusion patterns.
A study by Souza et al. (2005) reported similar stop/affricate confusions even in the absence of output limiting for subjects with severe hearing loss presented with speech signals at 70 dB SPL. They attributed this particular confusion to altered temporal cues such as the phoneme rise time. In addition, other researchers have noted that the overshoot from the attack time of a fast-acting compressor might have these types of manner confusions (Dreschler, 1988b; Yund & Buckles, 1995). Hickson and Byrne (1997) reported that fast-acting WDRC amplification degraded perception of stop consonants (albeit with a higher compression ratio than used here).
Because this study did not measure acoustic distortion, we can only speculate from documented effects of fast-acting WDRC on the temporal properties of speech (Jenstad & Souza, 2005) in combination with the consonant errors analyzed here. One factor that has been previously identified is the time constant of the compressor; particularly the release time (Jenstad & Souza 2005) which can be set over a very wide range clinically. In regard to speech audibility, severe hearing loss is best fit by shorter time constants that allow maximum gain for low-intensity consonants. For that reason, fast time constants were used in this study to maximize audibility. The small negative impact of fast-acting WDRC amplification only occurred for conversational and higher speech levels. It has been suggested that such effects may be alleviated by using longer time constants (e.g. Gatehouse, Naylor, & Elberling, 2006a, 2006b; Moore, 2008, Plomp, 1994). A sub-project in our laboratory tested 11 of the 20 listeners with severe hearing loss on the same consonant recognition task but with a slow (1400 msec) release time in the low frequency channel instead of the fast (100 msec) time constant used in this study. The results revealed that eight of the eleven listeners performed better with the low-frequency slow-acting WDRC at 65 dB SPL (Souza et al., 2007). Thus, the negative benefit of fast-acting WDRC on speech recognition might have been reduced or eliminated if a longer time constant had been used, but it is not clear to what extent that would offset the audibility advantage. This study does show that there is a potential negative effect of fast-acting WDRC on speech recognition even in clinically realistic protocols but the audibility benefits of fast-acting WDRC likely outweigh the negative effects for low level speech, especially for listeners with severe hearing loss.
In addition to the effects of WDRC, listeners’ confusion matrices revealed that listeners with mild-to-moderate loss made few place of articulation errors, while listeners with severe hearing loss made many place errors. This confusion is consistent with the idea that listeners with severe hearing loss, because of their large deficits in audibility and reduced spectral resolution, cannot access all the spectral cues needed for identifying place features. Although match to target was very good, audibility was slightly lower, on average, for the severe group (see table 3) and this may be one of the factors resulting in the greater place errors for listeners with severe hearing loss.
Table 3.
Mean aided audibility Index (AAI) for each listener group using WDRC and CL across 50, 65 and 80dB SPL
| Listener Group | Mean AAI | STD | Mean AAI | STD | Mean AAI | STD |
|---|---|---|---|---|---|---|
| 50 dB SPL | 50 dB SPL | 65dB SPL | 65 dB SPL | 80dB SPL | 80dB SPL | |
| Mild-to-Moderate | ||||||
| WDRC | .74 | .12 | .92 | .09 | .99 | .36 |
| CL | .46 | .13 | .79 | .10 | .97 | .05 |
| WDRC - CL | .28 | .13 | .02 | |||
| Severe | ||||||
| WDRC | .38 | .23 | .59 | .27 | .74 | .30 |
| CL | .16 | .10 | .48 | .17 | .62 | .25 |
| WDRC -CL | .22 | .11 | .12 | |||
Confounding Variables
Factors in addition to audibility and temporal distortion could have influenced the results, especially the high variance in WDRC benefit among listeners with severe hearing loss. Remember that the assumption was that listeners with severe hearing loss have broadened auditory filters, which consequently implied that these listeners were more dependent upon temporal cues in speech. The two listener groups were separated on the basis of pure tone thresholds. Thus, their spectral resolution abilities were assumed based on threshold. Although there is a consensus that auditory filter bandwidth increases with threshold elevation (Dubno & Dirks, 1990; Laroche,Hetu, Quoc, Josserand, & Glasberg, 1992), studies have shown varying auditory filter bandwidths among listeners with equal thresholds (Nelson, 1991; Glasberg & Moore, 1986). Because spectral resolution was not measured, it was not known if spectral resolution varied among the listeners with severe hearing loss and the listeners with mild-to-moderate hearing loss and if this could explain the observed variance in WDRC benefit among listeners. For example, although one of the listeners (S4) from Table 2 had a PTA corresponding to the mean PTA of the listeners with severe hearing loss, her scores approximated that of the listeners with mild-to-moderate hearing loss. Her unaided speech discrimination score was 100%, which was 38% above the average speech discrimination score for the listeners with severe hearing loss. Noting that this subject’s aided and unaided speech scores were close to that of the listeners with mild-to-moderate hearing loss, one is inclined to suggest that she may have better spectral resolution. A follow up study, using measures of spectral resolution, could parse out the effect of spectral resolution on consonant recognition and WDRC benefit.
Table 2.
Subject demographics and absolute percent correct scores
| Subject | Age | PTA | WDRC (50) | CL(50) | WDRC(65) | CL(65) | WDR(80) | CL(80) |
|---|---|---|---|---|---|---|---|---|
| MM7 | 56 | 28 | 90 | 82 | 87 | 87 | 82 | 75 |
| MM4 | 75 | 33 | 75 | 68 | 68 | 75 | 54 | 63 |
| MM6 | 80 | 35 | 80 | 83 | 89 | 79 | 67 | 79 |
| MM15 | 41 | 35 | 90 | 84 | 92 | 87 | 90 | 89 |
| MM3 | 64 | 37 | 70 | 92 | 83 | 91 | 80 | 78 |
| MM8 | 30 | 38 | 83 | 76 | 87 | 89 | 80 | 85 |
| MM5 | 79 | 40 | 54 | 46 | 61 | 63 | 53 | 62 |
| MM14 | 62 | 40 | 82 | 71 | 78 | 87 | 76 | 71 |
| MM11 | 90 | 42 | 62 | 58 | 56 | 56 | 55 | 54 |
| MM9 | 67 | 45 | 83 | 76 | 80 | 88 | 80 | 82 |
| MM2 | 84 | 47 | 66 | 79 | 64 | 72 | 67 | 77 |
| MM12 | 73 | 52 | 69 | 57 | 63 | 70 | 64 | 63 |
| MM13 | 67 | 52 | 74 | 55 | 77 | 80 | 69 | 75 |
| MM10 | 60 | 53 | 83 | 80 | 80 | 84 | 66 | 72 |
| Mean | 66 | 41 | 76 | 72 | 76 | 79 | 70 | 73 |
| S19 | 67 | 60 | 81 | 78 | 83 | 85 | 81 | 74 |
| S13 | 27 | 63 | 40 | 38 | 45 | 59 | 44 | 51 |
| S5 | 67 | 65 | 64 | 29 | 61 | 69 | 50 | 60 |
| S6 | 76 | 65 | 39 | 33 | 59 | 69 | 59 | 71 |
| S11 | 89 | 65 | 13 | 17 | 39 | 24 | 45 | 44 |
| S14 | 63 | 65 | 58 | 24 | 49 | 52 | 46 | 54 |
| S9 | 22 | 67 | 55 | 20 | 58 | 68 | 59 | 70 |
| S15 | 64 | 68 | 48 | 14 | 49 | 60 | 57 | 66 |
| S16 | 41 | 70 | 61 | 32 | 66 | 74 | 65 | 77 |
| S17 | 62 | 70 | 63 | 55 | 65 | 65 | 55 | 60 |
| S18 | 69 | 70 | 59 | 47 | 59 | 61 | 48 | 50 |
| S4 | 55 | 72 | 57 | 68 | 77 | 90 | 80 | 85 |
| S10 | 80 | 72 | 34 | 29 | 58 | 50 | 59 | 61 |
| S20 | 84 | 73 | 35 | 35 | 35 | 45 | 30 | 28 |
| S22 | 75 | 65 | 65 | 36 | 70 | 76 | 61 | 77 |
| S21 | 50 | 83 | 49 | 16 | 64 | 63 | 57 | 63 |
| S1 | 53 | 75 | 40 | 11 | 57 | 64 | 61 | 49 |
| S2 | 64 | 83 | 16 | 20 | 35 | 26 | 35 | 33 |
| S12 | 23 | 90 | 10 | 5 | 34 | 18 | 8 | 5 |
| S7 | 62 | 95 | 11 | 9 | 64 | 42 | 66 | 52 |
| Mean | 60 | 72 | 45 | 31 | 56 | 58 | 53 | 57 |
A second possible influence on the results was individual differences in hearing aid experience. Gatehouse (1982) stated that the true effects of different hearing aid frequency responses become apparent after listeners are allowed an acclimatization period of 6 to 12 weeks. Furthermore, Arlinger, Byrne, Dirks, Neuman, Ponton, et al. (1996) also stated that the best method of comparing different hearing aid frequency responses using speech tests should allow a period of acclimatization. In order to reduce an acclimatization bias, these studies suggest that a testing protocol that incorporates an acclimatization period may reduce bias between new and experienced users. Indeed, some studies such as Marriage and Moore (2003) as well as Marriage et al. (2005) allowed their subjects to acclimatize to the test instrument prior to data collection, thus their procedure controlled for confounding effects of varied hearing aid experience.
In the present study, listeners had varied levels of hearing aid experience. Some investigators (Gatehouse, 1982; Arlinger et al., 1996) have suggested that lack of hearing aid experience may mask the true effect of different hearing aid settings. This claim calls into question whether the three listeners with unilateral severe hearing loss in this study may have nullified some of the effects of WDRC versus CL amplification. It is hard to decipher because 1) these studies evaluated the effects of different hearing aid frequency gain settings rather than linear versus linear processing and 2) this claim is still being actively investigated. Some investigators have reported that objective performance increases with hearing aid experience (Kuk, Potts, Valente, Lee, & Picirrillo, 2003; Reber & Kompis, 2005; Yund et al., 2006), while others have not shown a significant change in objective speech recognition (Flynn, Davis & Pogash, 2004; Humes, Wilson, Barlow & Garner, 2002). Munro and Lutman (2003) suggested that hearing aid experience may influence measured hearing aid benefit as presentation level of the speech signal increases from 55 to 69 dB SPL. Their results suggests that differences between the experienced and inexperienced listeners in this study may exist for conversational (i.e. 65 dB SPL) and high (i.e. 80 dB SPL) speech. Although the present study did not control for or focus on the effects of hearing aid experience, a comparison of scores for those with and without hearing aid experience may provide information (albeit not well-controlled) as to whether these differences played a role. That comparison showed no difference in WDRC benefit at 50 dB SPL, t( 32) = 1.91, p = .065, 65 dB SPL, t(32) = 1.038, p = .307,and 80 dB SPL t(32) = -.838, p = .408.
Clinical Implications
A number of factors must be considered when deciding how to set the compression parameters of a fast-acting WDRC hearing aid, or whether to even use compression. Fast-acting WDRC affects, in a complex manner, the audibility and temporal cues of speech. The results indicated that both group of listeners with mild-to-moderate and severe hearing loss benefited from fast-acting WDRC for low level speech but not for conversational or high level speech. Other studies have also shown that fast-acting WDRC amplification improves recognition of low input level speech (Kam & Wong, 1999; Moore et al., 1999; Souza & Turner, 1998). Therefore, clinically a decision has to be made as to whether the audibility of low level speech is more important than the potential temporal distortions caused by fast-acting WDRC at higher speech input levels.
The test environment and speech material used in this study were different from continuous discourse in varied real-world background noises. Also, recall that subjective ratings were not evaluated in this study but previous studies have shown that fast-acting WDRC amplification may be superior to CL amplification for perceived quality of speech (Davies-Venn et al., 2007; Kam & Wong, 1999) and/or comfort of high level speech (Boike & Souza, 2000; Jenstad, Pumford, Seewald & Cornelisse, 2000; Kam & Wong, 1999; Larson et al., 2002; Lunner et al., 1998; Souza et al., 2002). When audibility and speech recognition performance are equated, fast-acting WDRC may have a subjective advantage over CL, especially for listeners with an aversion to high level sounds. Thus, considerations must be made for real-world speech conditions and subjective ratings for WDRC. One should also consider age and etiology of the listener’s hearing loss (Gatehouse et al, 2006b). Other individual variables such as communicative demands, compensatory communication strategies, and hearing aid experience must also be considered.
In summary, this study evaluated the effects of linear and non-linear amplification on age-matched listeners with mild-to-moderate and severe hearing loss at a variety of speech input levels. Audibility significantly influenced the results but accounted for less than half of the variance. Results indicated that fast-acting WDRC provides improved speech recognition for low level speech with very slight degradation of speech understanding at higher input levels. To better understand the variability in results, future studies should incorporate measures of spectral resolution.
Acknowledgments
This work was supported by the National Institute of Health (NIDCD) R01 DC 006014, P30 DC 04661 and the Bloedel Hearing Research Grant.
Footnotes
As part of the test protocol, insertion gain values were measured at 50 and 65 dB SPL, but not 80 dB SPL. In order to compute a full set of AAI values, ad hoc data was collected for insertion gain at 80 dB SPL, as follows. The test hearing instrument was re-programmed using the stored programming parameters for each listener and coupler gain was measured. RECD values were determined by computing the difference between coupler and real-ear gain for a measured condition (i.e. CL 65 dB SPL or fast-acting WDRC 65 dB SPL) for each listener. The individually measured RECDs were within the range of published standard adult RECDs (Dillon, 2001). The RECD values were added to the coupler gain values to obtain expected insertion gain at 80 dB SPL.
The assumption of sphericity was violated for level; all reported results for level reflect the Greenhouse-Geisser adjustment for degrees of freedom
References
- Amlani AM, Punch JL, Ching TYC. Methods and Applications of the Audibility Index in Hearing Aid Selection and Fitting. Trends Amplif. 2002;6(3):81–129. doi: 10.1177/108471380200600302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arlinger S, Gatehouse S, Bentler RA, Byrne D, Cox RM, Dirks DD, et al. Report of the Eriksholm Workshop on Auditory Deprivation and Acclimatization. Ear and Hearing. 1996;17(3):87S–98S. doi: 10.1097/00003446-199617031-00009. [DOI] [PubMed] [Google Scholar]
- Barker C, Dillon H, Newall P. Fitting low ratio compression to people with severe and profound hearing losses. Ear Hear. 2001;22(2):130–141. doi: 10.1097/00003446-200104000-00006. [DOI] [PubMed] [Google Scholar]
- Bentler RA, Pavlovic CV. Transfer functions and correction factors used in hearing aid evaluation and research. Ear Hear. 1989;10(1):58–63. doi: 10.1097/00003446-198902000-00010. [DOI] [PubMed] [Google Scholar]
- Boike KT, Souza PE. Effect of compression ratio on speech recognition and speech-quality ratings with wide dynamic range compression amplification. J Speech Hear Res. 2000;43(2):456–468. doi: 10.1044/jslhr.4302.456. [DOI] [PubMed] [Google Scholar]
- Boothroyd A, Nittrouer S. Mathematical treatment of context effects in phoneme and word recognition. J Acoust Soc Am. 1988;84(1):101–114. doi: 10.1121/1.396976. [DOI] [PubMed] [Google Scholar]
- Boothroyd A, Springer N, Smith L, Schulman J. Amplitude compression and profound hearing loss. Journal of Speech and Hearing Research. 1988;31(3):362–376. doi: 10.1044/jshr.3103.362. [DOI] [PubMed] [Google Scholar]
- Bor S, Souza P, Wright R. Multichannel compression: effects of reduced spectral contrast on vowel identification. J Speech Hear Res. 2008;51(5):1–13. doi: 10.1044/1092-4388(2008/07-0009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne D, Dillon H. The National Acoustics Laboratories’ (NAL) new procedure for selecting gain and frequency response of a hearing aid. Ear Hear. 1986;7(4):257–265. doi: 10.1097/00003446-198608000-00007. [DOI] [PubMed] [Google Scholar]
- Couvereur C. Implementation of a one-third-octave filter bank in matlab [computer software] 1997 Retrieved November 5, 2005 from http://citeseer.ist.psu.edu/24150.html.
- Davies-Venn E, Souza P, Fabry DA. Speech and Music Quality Ratings for Linear and Non-linear Hearing Aid Circuitry. J Am Acad Audiol. 2007;18(8):688–699. doi: 10.3766/jaaa.18.8.6. [DOI] [PubMed] [Google Scholar]
- Davies-Venn E, Souza P. Speech recognition with custom versus uniform compression ratios. Poster presented at the American Academy of Audiology Convention; Charlotte, NC. 2008. Apr, [Google Scholar]
- DeGennaro S, Braida LD, Durlach NI. Multichannel syllabic compression for severely impaired listeners. J Rehabil Res Dev. 1986;23(1):17–24. [PubMed] [Google Scholar]
- Dillon H. Hearing Aids. New York; Sydney: Thieme: Boomerang Press; 2001. [Google Scholar]
- Dillon H. NAL-NL1: A new procedure for fitting non-linear hearing aids. Hear J. 1999;52(4):10–16. [Google Scholar]
- Dillon H, Teresa Ching GK, Karolina Smeds Justin, Zakis RK. Factors affecting the prescription of hearing aids, and the NAL NAL-NL2 prescription. Paper presented at the American Academy of Audiology; Denver, CO. 2007. [Google Scholar]
- Dubno JR, Dirks DD. Associations among frequency and temporal resolution and consonant recognition for hearing-impaired listeners. Acta Otolaryngol Suppl. 1990;469:23–29. [PubMed] [Google Scholar]
- Dreschler WA. The effect of specific compression settings on phoneme identification in hearing-impaired subjects. Scan Audiol. 1988b;17(1):35–43. doi: 10.3109/01050398809042178. [DOI] [PubMed] [Google Scholar]
- Flynn MC, Dowell RC, Clark GM. Aided speech recognition abilities of adults with a severe or severe-to-profound hearing loss. J Speech Lang Hear Res. 1998;41(2):285–299. doi: 10.1044/jslhr.4102.285. [DOI] [PubMed] [Google Scholar]
- Flynn MC, Davis PB, Pogash R. Multiple-channel non-linear power hearing instruments for children with severe hearing impairment: long-term follow-up. Int J Audiol. 2004;43(8):479–485. doi: 10.1080/14992020400050061. [DOI] [PubMed] [Google Scholar]
- Fu G, Zeng T, Shannon R, Soli D. Importance of tonal envelope cues in Chinese speech recognition. J Acoust Soc Am. 1998;104(1):505–510. doi: 10.1121/1.423251. [DOI] [PubMed] [Google Scholar]
- Gatehouse S. The time course and magnitude of perceptual acclimatization to frequency responses: Evidence from monaural fitting of hearing aids. The Journal of the Acoustical Society of America. 1992;92:1258. doi: 10.1121/1.403921. [DOI] [PubMed] [Google Scholar]
- Gatehouse S, Naylor G, Elberling C. Linear and nonlinear hearing aid fittings - 1. Patterns of benefit. Int J Audiol. 2006a;45(3):130–152. doi: 10.1080/14992020500429518. [DOI] [PubMed] [Google Scholar]
- Gatehouse S, Naylor G, Elberling C. Linear and nonlinear hearing aid fittings - 2. Patterns of candidature. Int J Audiol. 2006b;45(3):153–171. doi: 10.1080/14992020500429484. [DOI] [PubMed] [Google Scholar]
- Gutnick HN. Consonant-feature transmission as a function of presentation level in hearing-impaired listeners. J Acoust Soc Am. 1982;72(4):1124–1130. doi: 10.1121/1.388321. [DOI] [PubMed] [Google Scholar]
- Hawkins DB, Walden BE, Montgomery A, Prosek RA. Description and validation of an LDL procedure designed to select SSPL90. Ear Hear. 1987;8(3):162–169. doi: 10.1097/00003446-198706000-00006. [DOI] [PubMed] [Google Scholar]
- Hickson L, Byrne D. Consonant perception in quiet: effect of increasing the consonant-vowel ratio with compression amplification. J Am Acad Audiol. 1997;8(5):322–332. [PubMed] [Google Scholar]
- Hopkins K, Moore BCJ. Moderate cochlear hearing loss leads to a reduced ability to use temporal fine structure information. J Acoust Soc Am. 2007;122(2):1055–1068. doi: 10.1121/1.2749457. [DOI] [PubMed] [Google Scholar]
- Hornsby B, Trine T, Ohde R. The Effects of High Presentation Levels on Consonant Feature Transmission in Normal-Hearing Subjects. J Acoust Soc Am. 2005;118(3):1719–1729. doi: 10.1121/1.1993128. [DOI] [PubMed] [Google Scholar]
- Humes LE, Wilson DL, Barlow NN, Garner C. Changes in Hearing-Aid Benefit Following 1 or 2 Years of Hearing-Aid Use by Older Adults. J Speech Hear Res. 2002;45(4):772–782. doi: 10.1044/1092-4388(2002/062). [DOI] [PubMed] [Google Scholar]
- Humes LE, Christensen LA, Bess FH, Hedley A. A Comparison of the Benefit Provided by Well-Fit Linear Hearing Aids and Instruments with Automatic Reductions of Low-Frequency Gain. J Speech Hear Res. 1997;40(3):666–685. doi: 10.1044/jslhr.4003.666. [DOI] [PubMed] [Google Scholar]
- Jenstad LM, Seewald RC, Cornelisse LE, Shantz J. Comparison of linear gain and wide dynamic range compression hearing aid circuits: Aided speech perception measures. Ear Hear. 1999;20(2):117–126. doi: 10.1097/00003446-199904000-00003. [DOI] [PubMed] [Google Scholar]
- Jenstad LM, Souza PE. Quantifying the effect of compression hearing aid release time on speech acoustics and intelligibility. J Speech Hear Res. 2005;48(3):651–667. doi: 10.1044/1092-4388(2005/045). [DOI] [PubMed] [Google Scholar]
- Jerger J. Clinical experience with impedence and audiometry. Arch Otolaryngol. 1970;92(4):311–324. doi: 10.1001/archotol.1970.04310040005002. [DOI] [PubMed] [Google Scholar]
- Kam AS, Wong LN. Comparison of performance with wide dynamic range compression and linear amplification. J Am Acad Audiol. 1999;10(8):445–457. [PubMed] [Google Scholar]
- Kent RD, Read C. Acoustic Analysis of Speech. Albany, NY: Singular/Thomason Learning; 2002. [Google Scholar]
- Killion MC, Niquette PA, Gudmundsen GI, Revit LJ, Banerjee S. Development of a quick speech-in-noise test for measuring signal-to-noise ratio loss in normal-hearing and hearing-impaired listeners. J Acoust Soc Am. 2004;116(4):2395–2405. doi: 10.1121/1.1784440. [DOI] [PubMed] [Google Scholar]
- Kuk F, Potts L, Valente M, Lee L, Picirrillo Evidence of Acclimatization in Persons with Severe-to-Profound Hearing Loss. J Am Acad Audiol. 2003;14(3):84–99. doi: 10.3766/jaaa.14.2.4. [DOI] [PubMed] [Google Scholar]
- Laroche C, Hetu R, Quoc HT, Josserand B, Glasberg B. Frequency selectivity in workers with noise-induced hearing loss. Hear Res. 1992;64(1):61–72. doi: 10.1016/0378-5955(92)90168-m. [DOI] [PubMed] [Google Scholar]
- Larson VD, Williams DW, Henderson WG, Luethke LE, Beck LB, Noffsinger D, et al. A multi-center, double blind clinical trial comparing benefit from three commonly used hearing aid circuits. Ear Hear. 2002;23(4):269–276. doi: 10.1097/00003446-200208000-00001. [DOI] [PubMed] [Google Scholar]
- Lunner T, Hellgren J, Arlinger S, Elberling C. A digital filterbank hearing aid: Predicting user preference and performance for two signal processing algorithms. Ear Hear. 1997;18(1):12–25. doi: 10.1097/00003446-199702000-00002. [DOI] [PubMed] [Google Scholar]
- Marriage JE, Moore BCJ. New speech tests reveal benefit of wide-dynamic-range, fast-acting compression for consonant discrimination in children with moderate-to-profound hearing loss. Int J Audiol. 2003;42(7):418–425. doi: 10.3109/14992020309080051. [DOI] [PubMed] [Google Scholar]
- Marriage JE, Moore BCJ, Stone MA, Baer T. Effects of three amplification strategies on speech perception by children with severe and profound hearing loss. Ear Hear. 2005;26(1):35–47. doi: 10.1097/00003446-200502000-00004. [DOI] [PubMed] [Google Scholar]
- Miller G, Nicely P. An analysis of perceptual confusions among English consonants. J Acoust Soc Am. 1955;27(2):338–352. [Google Scholar]
- Moore BCJ. The Choice of Compression Speed in Hearing Aids: Theoretical and Practical Considerations and the Role of Individual Differences. Trends Amplif. 2008;12(2):103–112. doi: 10.1177/1084713808317819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore BC, Glasberg BR. A comparison of two-channel and single-channel compression hearing aids. Audiol. 1986;25(4):210–226. [PubMed] [Google Scholar]
- Moore BCJ, Glasberg BR. Frequency discrimination of complex tones with overlapping and non-overlapping harmonics. J Acoust Soc Am. 1990;87:2163–2177. doi: 10.1121/1.399184. [DOI] [PubMed] [Google Scholar]
- Moore BCJ, Glasberg BR. A model of loudness perception applied to cochlear hearing loss. Auditory Neuroscience. 1997;3(3):289–311. [Google Scholar]
- Moore BCJ, Glasberg BR, Hopkins K. Frequency discrimination of complex tones by hearing-impaired subjects: Evidence for loss of ability to use temporal fine structure. Hearing Research. 2006;222:16–27. doi: 10.1016/j.heares.2006.08.007. [DOI] [PubMed] [Google Scholar]
- Moore BCJ, Johnson JS, Clark TM, Pluvinage V. Evaluation of a dual-channel full dynamic-range compression system for people with sensorineural hearing-loss. Ear and Hearing. 1992;13:349–370. doi: 10.1097/00003446-199210000-00012. [DOI] [PubMed] [Google Scholar]
- Moore BC, Peters RW, Stone MA. Benefits of linear amplification and multichannel compression for speech comprehension in backgrounds with spectral and temporal dips. J Acous Soc Am. 1999;105:400–411. doi: 10.1121/1.424571. [DOI] [PubMed] [Google Scholar]
- Munro KJ, Lutman ME. The effect of speech presentation level on measurement of auditory acclimatization to amplified speech. J Acoust Soc Am. 2003;114(1):484–495. doi: 10.1121/1.1577556. [DOI] [PubMed] [Google Scholar]
- Pittman AL, Stelmachowicz PG. Perception of Voiceless Fricatives by Normal-Hearing and Hearing-Impaired Children and Adults. J Speech Lang Hear Res. 2000;43(6):1389–1401. doi: 10.1044/jslhr.4306.1389. [DOI] [PubMed] [Google Scholar]
- Plomp R. Noise, amplification, and compression: considerations of three main issues in hearing aid design. Ear Hear. 1994;15(1):2–12. [PubMed] [Google Scholar]
- Nittrouer S, Boothroyd A. Context effects in phoneme and word recognition by young-children and older adults. J Acoust Soc Am. 1990;87(6):2705–2715. doi: 10.1121/1.399061. [DOI] [PubMed] [Google Scholar]
- Reber MB, Kompis M. Acclimatization in first-time hearing aid users using three different fitting protocols. Auris Nasus Larynx. 2005;32(4):345–351. doi: 10.1016/j.anl.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Resnick SB, Dubno JR, Hoffnung S, Levitt H. Phoneme errors on a nonsenese syllable test. J Acoust Soc Am. 1975;58(1):S114–S114. [Google Scholar]
- Rosen S. Temporal information in speech- acoustic, auditory and linguistic aspects. Philos Trans R Soc Lond B Biol Sci. 1992;336(1278):367–373. doi: 10.1098/rstb.1992.0070. [DOI] [PubMed] [Google Scholar]
- Rosen S, Faulkner A, Smith DJ. The psychoacoustics of profound hearing impairment. Acta Otolaryngol Suppl. 1990;469:16–22. [PubMed] [Google Scholar]
- Scollie S, Seewald R, Cornelisse L, Moodie S, Bagatto M, Laurnagaray D, et al. Desired Sensation Level Multistage Input/Output Algorithm. Trends Amplif. 2005;9(4):159–197. doi: 10.1177/108471380500900403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbecoe RL, Studebaker GA. Supplementary formulas and tables for calculating and interconverting speech recognition scores in transformed arcsine units. Int J Audiol. 2004;43(8):442. doi: 10.1080/14992020400050056. [DOI] [PubMed] [Google Scholar]
- Souza P. Effects of Compression on Speech Acoustics, Intelligibility, and Sound Quality. Trends Amplif. 2002;6(4):131–165. doi: 10.1177/108471380200600402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza PE, Bishop RD. Improving speech audibility with wide dynamic range compression in listeners with severe sensorineural loss. Ear Hear. 1999;20(6):461–470. doi: 10.1097/00003446-199912000-00002. [DOI] [PubMed] [Google Scholar]
- Souza PE, Turner CW. Quantifying the contribution of audibility to recognition of compression-amplified speech. Ear Hear. 1999;20(1):12–20. doi: 10.1097/00003446-199902000-00002. [DOI] [PubMed] [Google Scholar]
- Souza PE, Turner CW. Multichannel compression, temporal cues, and audibility. J Speech Lang Hear Res. 1998;41(2):315–326. doi: 10.1044/jslhr.4102.315. [DOI] [PubMed] [Google Scholar]
- Souza P, Brennan M, Davies-Venn E. Using short vs. long time constants in severe loss. Talk presented at the American Auditory Society Research Meeting; Scottsdale, AZ. 2007. [Google Scholar]
- Souza PE, Jenstad LM, Folino R. Using multichannel wide-dynamic range compression in severely hearing-impaired listeners: effects on speech recognition and quality. Ear Hear. 2005;26(2):120–131. doi: 10.1097/00003446-200504000-00002. [DOI] [PubMed] [Google Scholar]
- Stelmachowicz P, Lewis D, Creutz T. Boys Town National Center. Omaha Nebraska; 1994. Situational Hearing-Aid Response Profile (SHARP, version 6.0) [Google Scholar]
- Stone MA, Moore BC. Syllabic compression: Effective compression ratios for signals modulated at different rates. Br J Audiol. 1992;26(6):351–361. doi: 10.3109/03005369209076659. [DOI] [PubMed] [Google Scholar]
- Strom KE. The HR 2006 Dispenser Survey. Hear Rev. 2006;13(6):16. [Google Scholar]
- Studebaker GA. A "Rationalized" Arcsine Transform. J Speech Hear Res. 1985;28(3):455–462. doi: 10.1044/jshr.2803.455. [DOI] [PubMed] [Google Scholar]
- Van Heuven VJ. Reversal of the rise time cue in the affricate fricative contrast, an experiment on the silence of sound. In: Schouten MEH, editor. The psychophysics of speech perception. Martinus Nijhoff; 1987. pp. 181–187. [Google Scholar]
- Verschuure H, Prinsen TT, Dreschler WA. The effects of syllabic compression and frequency shaping on speech-intelligibility in hearing-impaired people. Ear Hear. 1994;15(1):13–21. doi: 10.1097/00003446-199402000-00003. [DOI] [PubMed] [Google Scholar]
- Verschuure J, Maas AJ, Stikvoort E, de Jong RM, Goedegebure A, Dreschler WA. Compression and its effect on the speech signal. Ear Hear. 1996;17(2):162–175. doi: 10.1097/00003446-199604000-00008. [DOI] [PubMed] [Google Scholar]
- Verschuure J, Benning FJ, Van Cappellen M, Dreschler WA, Boeremans PP. Speech Intelligibility in Noise with Fast Compression Hearing Aids. Intl J Audiol. 1998;37(3):127–150. doi: 10.3109/00206099809072968. [DOI] [PubMed] [Google Scholar]
- Wilson RH, Zizz CA, Shanks J, Causey GD. Normative data in quiet, broad-band noise, and competing message for northwestern university auditory test NU-6 by a female speaker. J Speech Hear Dis. 1990;55(4):771–778. doi: 10.1044/jshd.5504.771. [DOI] [PubMed] [Google Scholar]
- Yund EW, Buckles KM. Enhanced speech perception at low signal-to-noise ratios with multichannel compression hearing aids. J Acoust Soc Am. 1995;97(2):1224–1240. doi: 10.1121/1.412232. [DOI] [PubMed] [Google Scholar]
- Yund EW, Roup CM, Simon HJ, Bowman GA. Acclimatization in wide dynamic range multichannel compression and linear amplification hearing aids. J Rehabil Res Dev. 2006;43(4):517–535. doi: 10.1682/jrrd.2005.06.0099. [DOI] [PubMed] [Google Scholar]