Abstract
The purpose of this study was to examine the moderating effects of cognitive risk factors in two mechanistically-distinct interventions. Forty-one patients with panic disorder and agoraphobia were randomly assigned to receive training aimed at altering respiration (Capnometry-assisted respiratory training, CART) or symptom appraisal (cognitive skill training, CT). Using a mixed effects regression model, we assessed whether reductions in panic symptom severity (PDSS) were moderated by the variables of interest. While improvement in PDSS did not differ among treatment modalities, moderating effects emerged. Individuals with greater initial levels of misappraisal showed smaller reduction in PDSS when receiving CT, but larger reduction when receiving CART. Greater lack of perceived control was predictive of worse outcome in CART, but better outcome in CT. Better homework compliance was related to greater reductions in PDSS irrespective of condition. The findings illustrate the complexity of moderating influences within and between distinct interventions.
Panic disorder with or without agoraphobia (PD) is a common emotional disorder with a lifetime prevalence of approximately 4.7% (Kessler, Chiu, Demler, & Walters, 2005). It is associated with high rates of disability and high levels of economic and medical costs (Deacon, Lickel, & Abramowitz, 2008; Keller et al., 1994; Klerman, Weissman, Ouellette, Johnson, & Greenwald, 1991; Leon, Portera, & Weissman, 1995). While psychosocial interventions for PD are well established and generally effective (Barlow, Gorman, Shear, & Woods, 2000; Mitte, 2005), not all patients benefit equally, as attested by considerable drop-out rates (Haby, Donnelly, Corry, & Vos, 2006) and symptom retention following treatment (Brown & Barlow, 1995). Thus, maximizing treatment response is critical given the high personal, social, and medical costs associated with this disorder.
The identification of variables that impact response to treatment is therefore crucial to gain a better insight for whom, and under what circumstances, treatment will be most beneficial (Kraemer, Frank, & Kupfer, 2006; Kraemer, Wilson, Fairburn, & Agras, 2002). However, despite general consensus that such knowledge will “serve as a basis for maximizing treatment effects and ensuring that critical features are generalized to clinical practice” (Kazdin & Nock, 2003, p. 117), research remains surprisingly sparse. Furthermore, examining the extent to which certain types of interventions are more or less likely to be beneficial for preexisting characteristics remains largely unknown. In our review of this research below and thereafter, we will adopt the terminology proposed by Kraemer et al. (2006), referring to factors that affect outcome regardless of treatment condition as predictors, and those that impact outcome differentially across treatments as moderators. Whereas predictors offer clinical insight, only moderators facilitate optimal treatment selection.
Among the studies that have investigated prognostic factors in different types of PD interventions are the recent studies by Milrod and colleagues (Milrod et al., 2007; Klass et al., 2009). Results suggested that the presence of a comorbid cluster C diagnosis (associated with lack of self-assertion and autonomy) moderated treatment outcome, in that greater reductions in panic symptom severity were observed in patients receiving panic-focused psychodynamic psychotherapy (PFPP; Milrod et al., 2007) compared to those receiving applied relaxation (Milrod et al., 2007). In contrast, patients who had suffered personal loss prior to treatment benefited more from applied relaxation as opposed to PFPP (Klass et al., 2009). The findings illustrated that a specific therapeutic focus can moderate the effect certain personality aspects or experiences that otherwise are indicative of poorer prognosis.
Fearful appraisal of bodily sensations has also been considered a likely predictor or moderator of outcome. According to Clark (1986) and McNally (1994), it is the fearful interpretation of these sensations (the catastrophic appraisals), not the sensations themselves, that is thought to trigger attacks. Hicks and colleagues (2005) tested whether preexisting catastrophic cognitions would moderate differential short- and long-term treatment outcome in cognitive-behavioral therapy (CBT) versus pharmacological treatment for PD. More intense fears of social catastrophes predicted poorer outcome at posttreatment and follow-up, whereas thoughts related to physical and mental catastrophes did not predict changes in panic symptom severity. These relations did not vary by the type of intervention patients received. A second moderator study examined the effect of initial levels dysfunctional agoraphobic cognitions, panic severity, and other prognostic indices on outcome in brief versus standard forms of CBT delivery for PD (Dow, Kenardy, Johnston, Newman, Taylor, & Thomson, 2007). Moderating effects indicated that those with more severe levels of panic severity and misappraisal had less positive outcomes when receiving brief CBT. The authors attribute the differential outcomes to the lowered opportunity to challenge and resolve panic-related misattributions. Other studies that examine maladaptive cognitions as predictors of outcome found similar results. Keijsers, Hoogduin, and Schaap (1994) observed poorer outcome in PD patients with higher levels of catastrophic cognitions prior to the initiation of an exposure-based treatment. Similarly, stronger automatic catastrophic cognitions predicted smaller reductions in anxiety sensitivity in response to a brief, one-session CBT-type intervention for PD (Schneider & Schulte, 2008). On the other hand, Chambless and Gracely (1988) and Aaronson et al. (2008) failed to find such associations. Taken together, the few studies examining symptom appraisal as a predictor of treatment outcome have yielded inconsistent findings. In the studies in which a predictor effect was found, higher baseline levels of fearful appraisals were related to poorer outcomes. Studies examining moderating effects of symptom appraisal across treatment modalities remain sparse and yield inconsistent findings.
Perceived control, or lack thereof, has been viewed as another potent determinant for the etiology and maintenance of PD (Barlow, 2002; Mineka & Kelly, 1989; White, Brown, Somers, & Barlow, 2006). Unexpected bursts of emotions (true alarms or false alarms) are thought to cause vulnerable individuals to view their own emotions and bodily reactions as being out of their control. Such lack of internal control over one’s own emotional response can consequently facilitate a catastrophic interpretation of bodily sensation and avoidance of situations and behaviors that are likely to trigger them. Despite its apparent clinical importance in PD, there is no published research examining its prognostic value. One might expect, however, that those with lower perceived control would be less likely to benefit from treatment as they may harbor beliefs that could undermine their own progress. For example, lack of controllability may affect patients’ expectations of their ability to ever change their panic symptoms. This may become particularly apparent in patients’ ability and motivation to engage in skill practice and application outside the therapy session, a factor that is viewed as one of the most essential elements of cognitive and behavioral therapy.
Indeed, greater homework compliance (skill practice and application) has been associated with better outcomes in studies of anxiety (Edelman & Chambless, 1993; Leung & Heimberg, 1996; Westra, Arkowitz, & Dozois, 2009; Westra, Dozois, & Marcus, 2007) and depression (Rees, McEvoy, & Nathan, 2005). Whereas homework compliance in and of itself may be an important determinant of treatment success in these investigations, findings in PD, albeit limited in number, have yielded mixed results (Edelman & Chambless, 1993; Schmidt & Woolaway-Bickel, 2000; Woods, Chambless, & Steketee, 2002). A number of factors may account for these inconsistent findings. For example, some studies operationalize homework compliance as the quantity of time spent practicing a particular skill, while others examine the quality of the homework done. In addition, none of these studies used objective measures to assess compliance, but used diaries or retrospective questionnaires, both of which can be misrepresented as they are vulnerable to a host of biases (Meuret, Wolitzky-Taylor, Twohig, & Craske, submitted; Newman, Kenardy, Herman, & Taylor, 1997).
Taken together, little is known about the prognostic value of cognitive risk factors in PD. Discovering factors that explain variations in outcome within and across therapeutic approaches is critical for adjusting existing treatment programs. Furthermore, it is critical to establish whether such factors are predictors of treatment outcome (i.e., they effect outcomes from different treatments in the same manner), or if they are moderators of outcome (i.e., they impact treatments differently). If a factor is a moderator of treatment outcome, then patients with that characteristic may benefit more from one treatment over another. Such knowledge is crucial to facilitate optimal treatment selection and thus enhance treatment success. To identify moderators, several methodological requirements are needed. First, the proposed moderator must be tested in more than one intervention. That is, if we assume a certain moderator to be better suited for a particular intervention, we should ideally contrast this intervention with a mechanistically-distinct intervention type. Second, to more precisely understand the aspects of the interventions that are impacted by the moderator, one should test the moderator in interventions that focus on specific mechanisms. For example, to determine if a moderator affects outcomes in therapies focused on maladaptive cognitions, it is important that at least one of the interventions exclusively target cognitive restructuring, and is not paired with additional therapeutic techniques. Similarly, the other interventions against which to compare should also target a specific mechanism, and does not include aspects similar to the other intervention. Finally, it is important to control for additional factors that are closely related to therapeutic processes that may influence the results. Thus, several plausible moderators should be tested simultaneously to verify that the moderator itself is responsible for any outcome differences, and not its relation with other variables that might be responsible for the outcome.
The aim of this study was to expand upon previous research by specifically testing the moderating effects of multiple cognitive risk factors (catastrophic appraisal and perceived control) in two mechanistically-distinct interventions. The first intervention focused on changing cognitions (cognitive skill training, or CT), whereas the second, capnometry-assisted respiratory training, or CART (Meuret, Wilhelm, Ritz, & Roth, 2008), was aimed at changing aberrant respiratory patterns; in particular, lower than normal levels of carbon-dioxide (PCO2), or hypocapnia. Prior analyses on the efficacy and mechanisms of these interventions (Meuret, Rosenfield, Seidel, Bhaskara, & Hofmann, in press) showed that panic symptom severity was significantly and equally reduced in both CT and CART. However, the pathways by which these reductions were achieved differed substantially between conditions.
In addition, we sought to enhance our understanding of the association between homework compliance and outcome by employing objective measures of compliance, and by examining this association in the distinct interventions (CT and CART). We operationalized compliance as the number of sessions completed, a number which was based on electronically validated diary records.
The effects of all three variables (homework compliance, symptom appraisal, and perceived control) were tested simultaneously in both treatment conditions. This strategy provided better estimation of the true effects of each moderator while controlling for other potential moderators and allows the inclusion of all patients regardless of whether they “dropped out” of the study. The effects of the proposed predictors and moderators on changes in panic symptom severity (Panic Disorder Severity Scale, PDSS, Shear et al., 1997) were examined using data from a recent randomized-control trial (Meuret, Rosenfield, Seidel, in press).
On the basis of previous theory and empirical findings, we tested the following hypotheses: First, regarding initial levels of catastrophic cognitions, although previous studies yielded mixed results, it seems reasonable to expect that patients with higher levels of catastrophic cognitions would show better response to CT than CART, since only CT directly targets and manipulates maladaptive cognitions. Second, although no evidence exists regarding the effect of initial level of perceived emotional control on treatment outcome, we expect a lack of perceived control to predict worse treatment outcome. We further expect this outcome to be independent of treatment condition, since neither intervention directly targets emotional control. Finally, we expected homework compliance be related to better outcome, regardless of condition.
METHOD
Overview of the Design
This study is based on data from a randomized-controlled intervention trial for patients with panic disorder and agoraphobia. Patients were assigned to receive five individual, weekly, one-hour sessions of respiratory skill training (CART) or cognitive skill training (CT). Clinical assessments were administered throughout treatment. The study was initiated at the Center for Anxiety and Related Disorders at Boston University and completed at Southern Methodist University and was approved by both local ethics committees. Details of the trial are reported elsewhere (Meuret et al., in press).
Participants
Forty-one patients with a principal DSM-IV diagnosis of panic disorder and agoraphobia (PDA) were enrolled in a randomized-controlled trial of CART (N = 21) and CT (N = 20) (Meuret et al., in press). Participants, aged 20 to 75, were predominantly female, white, married, and well-educated. The majority reported moderate to severe agoraphobic avoidance (Panic Disorder Severity Scale—Item 4, Shear et al., 1997). Forty-four percent had at least one additional current DSM-IV Axis I diagnosis and more than half of the participants were on a stable dose of psychotropic medication. Patients were excluded from participation if they met criteria for a history of bipolar disorder, suicidality, substance abuse or dependence, psychosis or delusional disorders, presence of an organic mental disorder, chronic respiratory disease, seizures, or severe unstable medical illness.
Interventions
To assess aspects of efficacy, mediation, and moderation, CART and CT were matched for duration (four weeks), length of sessions (60 minutes), provision of rationale, and administration (trained psychologists or graduate students). The interventions were also matched for structure of between-session exercises (see homework assignments). Special attention was paid to minimize diffusion across the treatments or other components of therapy (e.g., exposure). Treatment expectancy and credibility was high and did not differ by condition. A detailed description, including results on treatment adherence, can be found in Meuret et al. (in press).
Cognitive Training (CT)
The training was based on the cognitive model by Clark (1986) that maladaptive thoughts contribute to symptom development and maintenance of PD/A. Based on an adapted version of Craske, Barlow, and Meadows’ (2000) cognitive therapy module, the training components included: (a) educating patients about the exacerbation of panic symptoms through catastrophic thoughts (vicious cycle), (b) assisting the identification of negative cognitions associated with physical sensation triggers of recent panic attacks, (c) practice replacing maladaptive cognitions with noncatastrophic explanations, and (d) instructing patients in between-session exercises during which they reflected upon recent or upcoming panic-related events. They were asked to identify catastrophic thoughts, associated cognitive errors, and to generate noncatastrophic and more realistic appraisals, that are recorded in writing (homework diaries).
Capnometry-Assisted Respiratory Training (CART)
CART is based on the theory that sustained levels of hypocapnia contribute to symptom development and maintenance of PD/A (Meuret, Wilhelm, & Roth, 2001, 2004; Meuret et al., 2008). Training components include: (a) educating patients about the exacerbation of panic symptoms through hypocapnia, (b) directing their attention to potentially detrimental respiratory patterns, (c) teaching techniques to alter end-tidal PCO2, using capnometer feedback and (d) instructing patients in between-session exercises. The exercises included a 10-minute paced breathing phase during which patients monitored their PCO2 and respiration rate, using a portable capnometry device. This phase is followed by a 5-minute transfer period during which patients are asked to maintain certain respiratory patterns without pacing tones, but with continued PCO2 biofeedback. The overall goal was to breathe shallowly, slowly, and regularly while increasing or maintaining a PCO2 in a normocapnic range (40 mmHg +/− 3).
Homework Assignments
To standardize homework comparability and dose, between-session assignments were matched in duration (17-minutes) and number (twice daily), but differed in content. For both conditions, each between-session exercise started with a baseline recording for two minutes followed by a 15-minute practice period during which patients applied their respective skill. The beginning and end of each exercise period was prompted by an audio recording. In addition to ongoing recording of respiratory physiology (portable capnometry with electronic date, time, and duration stamp), patients in both groups were asked to complete a brief symptom rating (DSM-IV symptoms) before and after each exercise (exercise log). Patients assigned to CT used the same log to record their cognitive restructuring exercises in writing. Exercises were reviewed and discussed during weekly training sessions with therapists to assist patients in identifying examples of successful acquisition of their skills and to support further skill improvement.
The electronic time stamp provided objective confirmation that the assignments were done as reported in the homework logs, and at the times that were reported. Treatment compliance was defined as number of completed homework sessions, and was assessed by matching electronic capnometry records with the homework log entries. Patients in both conditions completed approximately 64% of the 52 assigned homework exercises, CART = 33.8 (SD: 13.3); CT = 32.8 (SD: 16.7), a result that did not differ significantly by condition.
Measures
All measures, except the PDSS, were assessed at pretreatment and at sessions 2, 3, 4, and 5. PDSS was measured at pretreatment and session five (four weeks apart).
The dependent variable, the Panic Disorder Severity Scale (PDSS; Shear et al., 1997), is a standard outcome measure in PD intervention studies. It is a semi-structured 7-item clinician-administered interview scale which provides a global rating of panic severity (here referred to as panic symptom severity). Severity ratings range from 0 to 4 (none, mild, moderate, severe, extreme). Interrater reliability for this study (based on pre- and posttreatment independent assessments) was excellent, ICC (2, 1) = 0.97 and 0.96, respectively (Shrout & Fleiss, 1979).
Two measures were used to capture panic-related cognitions. The first was a composite measure reflecting symptom appraisal formed by combining the Body Sensations Questionnaire (BSQ; Chambless, Caputo, Bright, & Gallagher, 1984) and the Anxiety Sensitivity Index (ASI; Reiss, Peterson, Gursky, & McNally, 1986). Both measures tap into fear of sensations associated with autonomic arousal. They both have good psychometric properties (Chambless et al., 1984; Reiss et al., 1986) and were highly correlated r = .63. Consequently, both measures were converted to z-sore and combined to form a composite measure of symptom appraisal (ASI/BSQ).
Perceived emotional control was assessed using the Anxiety Control Questionnaire (ACQ; Rapee, Craske, Brown, & Barlow, 1996). It measures the degree to which individuals perceive that they have control, or lack control, over aversive events such as external threats (e.g., resolving problems) or internally generated sensations. We reverse scored this measure so that higher scores on the ACQ were indicative of a greater lack of control. Thus, higher scores on both cognitive measures reflected greater dysfunction. The questionnaire has shown excellent psychometric properties (Rapee et al., 1996).
Homework compliance was operationalized as the number of homework sessions completed.
ANALYTIC PROCEDURE
We used a mixed effects regression model (MRM) to analyze the data. MRMs allow all participants to be included in the analyses regardless of missing data/assessments, appropriately accounts for the correlation between repeated measures within individual over time, and is thus considered the preferred method to analyze longitudinal psychiatric data (Gibbons et al., 1993; Hamer & Simpson, 2009). Since we were primarily interested in investigating variables that impact the slope of change in PDSS over time, our MRM included Time (coded 0 and 1) as a predictor of outcome (PDSS), and interactions between Time and our potential moderators (i.e., baseline levels of cognitive misappraisal and lack of control). We also assessed the triple interactions between Time, the proposed moderators, and treatment condition to determine if the effects of the potential moderators differed between treatment modalities.
In addition, to insure that the effects of the potential moderators were not due to their relation with baseline level of PDSS or to homework compliance, we added the following terms involving these control variables to the MRM analysis: baseline PDSS, homework compliance (number of homework sessions completed), the interactions of these two control variables with Time, and the interactions between the control variables, Time, and treatment condition. Finally, the treatment condition × Time interaction was included to assess for treatment differences in reductions in PDSS over time. Henceforth, we will use the term reductions in panic symptom severity (or PDSS) to refer to the effect of Time on PDSS.
Since there were two assessments per patient, only one random effect was possible in the MRM. We chose to analyze a random-intercept model, since there was significant variability in the intercept, χ2 (38) = 189.99, p < .001. For completeness, we tested the fixed intercept, random-slopes model as well. Analyses indicated that the between patient variability in slopes of improvement in PDSS was not significant, χ2 (38) = 38.36, p = .45, supporting the use of the aforementioned random-intercept model.
For decomposing the interactions, the three-way interactions between the moderators, treatment condition, and Time were examined in detail using the approach suggested by Aiken and West (1991). Our focus was the influence of the moderator on reductions in PDSS over time (the slope of Time on PDSS), and whether this effect depended on treatment condition. Thus, we examined the impact of the interactions of the moderators with treatment condition on reductions in PDSS. These interactions were examined in two ways. First, we looked at the effect of the moderator on improvement in PDSS in each treatment condition separately, by alternately coding the treatments 0 and 1 (performing one analysis with CT= 0, CART= 1, and the next analysis with CART= 0, CT= 1; Aiken & West, 1991). Thus, we were able to test the relation between each moderator and reductions in PDSS in both CT and CART. Second, we examined the effect of treatment condition on the reductions in PDSS for patients who were high (or low) on each moderator. Again using the approach by Aiken and West (1991) we performed two analyses to ascertain these relations: (1) centering the moderator alternately at a high level (1 SD above the mean) and then (2) centering the moderator at a low level (1 SD below the mean), performing separate analyses, each using the different centered variable. The first analysis will thus yield the effect of treatment on reductions in PDSS for those who are high on the moderator, while the second yields condition differences on reductions in PDSS for those low on the moderator.
RESULTS
Baseline Characteristics
None of the socio-demographic characteristics varied by treatment group (all ps > .35). Baseline levels of the study variables are displayed in Table 1. Baseline levels of the moderators did not vary by treatment condition (ps > .50). However, it is important to point out that baseline levels of some of the measures were correlated. Higher baseline PDSS was related to more negative cognitive appraisals, r (39) = .60, p < .001, and to greater lack of perceived control r (39) = .53, p = .001. Baseline levels of lack of control and negative appraisals were also related, r (39) = .61, p < .001. The fact that lack of control and negative cognitive appraisals were related to PDSS at baseline supports the importance of controlling for the effects of baseline PDSS in the moderator analysis.
TABLE 1.
Pretreatment Levels of Demographic and Clinical Characteristics
| Variable | CART (n = 21) |
CT (n = 20) |
χ2(df) | t(df) | ||
|---|---|---|---|---|---|---|
| N(%) | M(SD) | N(%) | M(SD) | |||
| Subject Characteristics | ||||||
| Male | 4(19.1) | 3(15.0) | .12(1) | |||
| Age (years) | 31.42(8.93) | 35.00(10.64) | −1.13(39) | |||
| White | 18(85.7) | 18(90.0) | .98(3) | |||
| Family and Social Background | ||||||
| Education (years) | 16.05(2.40) | 15.55(2.44) | .66(39) | |||
| Married | 10(47.6) | 8(40.0) | 4.89(4) | |||
| Additional Axis I Diagnosis | 8(40.0) | 10(58.8) | 1.30(1) | |||
| Use of Psychotropic Medication | 13(61.9) | 15(75.0) | .81(1) | |||
| Clinical Characteristics | ||||||
| ASI | 35.34(9.39) | 33.75(12.44) | .45(37) | |||
| BSQ | 2.17(.64) | 2.25(.86) | −.33(37) | |||
| ASI/BSQ | .02(1.57) | −.02(2.05) | .07(37) | |||
| ACQ | 69.74(15.34) | 74.42(14.49) | −.98(37) | |||
| PDSS | 17.72(3.10) | 16.95(5.36) | .57(39) | |||
Note. None of the differences between treatment groups was significant. CART: Capnometry-assisted Respiratory Training; CT: Cognitive Skill Training; ASI/BSQ: Composite of z-scored Anxiety Sensitivity Index and Body Sensations Questionnaire; ACQ: Anxiety Control Scale; PDSS: Panic Disorder Severity Scale.
Previous analyses of this data set demonstrated that cognitive misappraisal, perceived control, and PDSS improved significantly over time, and that reductions in PDSS over time did not differ between treatment conditions (Meuret et al., in press). The effect sizes for within subject improvement on the PDSS for CT and CART were 2.25 and 2.68, respectively, and thus comparable to standard CBT (e.g., Barlow et al., 2000).
Moderator Analysis
In order to minimize the number of predictors in the regression model, we first removed all nonsignificant 3-way interactions (in this case, only treatment × time × homework was nonsignificant). To further minimize the number of predictors in the model, we then recomputed the model and deleted predictors with b = 0.00 and p = 1.00 (the main effects for condition, misappraisal, lack of control, and homework). The results of this final model are displayed in Table 2.
TABLE 2.
Results of the MRM Analysis, with Each Treatment Condition Coded 0
| Effect | Regression Coefficients for CART (CART = 0) | Regression Coefficient for CT (CT = 0) s |
|---|---|---|
| Time | −0.93*** | −0.93*** |
| PDSS | 0.62*** | 0.62*** |
| Time × PDSS | 0.05 | −0.46*** |
| Time × Condition | 0.00 | 0.00 |
| Time × Misappraisal | −0.17* | 0.11* |
| Time × Lack of Control | 0.35** | −0.01 |
| Time × Homework | −0.10* | −0.10* |
| Time × PDSS × Condition | −0.52*** | 0.52*** |
| Time × Misappraisal × Condition | 0.27*** | −0.27*** |
| Time × Lack of Control × Condition | −0.36* | 0.36* |
Note. CART: Capnometry-assisted Respiratory Training; CT: Cognitive Skill Training; PDSS: Panic Disorder Severity Scale.
p < .05,
p < .01,
p < .001.
Results for our control variables (baseline level of PDSS and homework compliance) showed that they were significantly related to reductions in PDSS, reinforcing their importance as control variables in the analysis. In particular, the triple interaction between Time, baseline PDSS, and treatment condition was significant, b = −.52, t(58) = 3.48, p = .001. Examining the effect of baseline PDSS on rates of improvement within each condition separately, we found that higher baseline panic symptom severity was predictive of greater reductions in PDSS in the CT condition, b = −.46, t(58) = 4.45, p < .001, but it was unrelated to improvement in the CART condition, b = .05, t(58) = .43, p = .67 (see Table 2). Since those with higher baseline panic severity had greater reductions in the CT condition, it is interesting to investigate whether (in CT) those with higher baseline PDSS improved fast enough to catch up with those with lower baseline PDSS. To examine this possibility, we recoded Time so that posttraining was coded 0 (pre = −1, post = 0), and treatment was coded CT = 0, CART = 1. In this coding scheme, the main effect for baseline PDSS is the effect of baseline PDSS on posttraining PDSS scores in CT. This main effect was not significant, b = .15, t(58) = 1.49, p = .15, indicating that a patient’s baseline PDSS did not significantly affect their final PDSS score (i.e., those with higher baseline PDSS were able to “catch up with” those with lower baseline PDSS).
Concerning our other control variable, homework compliance, it was associated with reductions in panic symptom severity regardless of treatment condition. In particular, better compliance was associated with greater reductions in PDSS, b = −.10, t(58) = 1.98, p = .05, regardless of treatment condition.
Effect of Baseline Symptom Appraisal
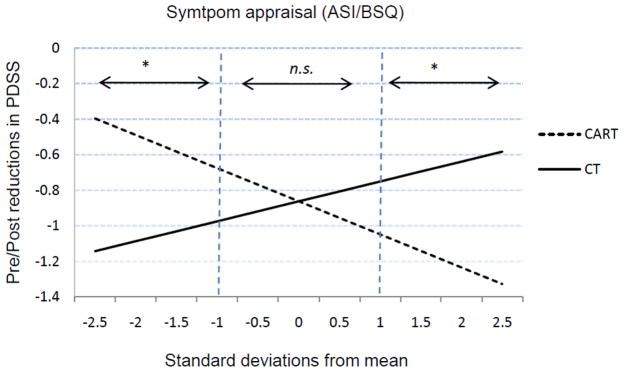
The results also indicated a significant 3-way interaction between Time, condition, and baseline negative appraisal, b = .27, t(58) = 3.47, p = .001. Thus, the impact of negative appraisal on reductions in panic severity over time was different for the different treatment conditions. Following Aiken and West (1991), we explored the relation between negative appraisal and change in PDSS over time in each treatment condition by alternately coding CT and CART as 0 and rerunning the analyses (see Table 2). In CT, higher baseline negative appraisal predicted smaller reductions in PDSS, b = .11, t(58) = 2.37, p < .05 (Figure 1), whereas higher negative appraisals were predictive of greater reductions in PDSS in CART, b = −.17, t(58) = 2.59, p = .01 (Figure 1). Likewise, we tested whether individuals with high or low levels of misappraisals were differentially impacted by the two treatments over time. Those individuals with high levels of baseline negative appraisals (1 SD above the mean) improved faster in CART than in CT, b = .49, t(58) = 2.47, p < .05. For those low in baseline negative appraisals, individuals in CT improved faster than those in CART, b = −.50, t(58) = −2.99, p < .005. No differences between the two treatment conditions were found at mean levels of negative appraisal, p = .99.
FIGURE 1.
Pre-Post reductions in PDSS in CART and CT as a function of baseline cognitive misappraisal (ASI/BSQ). CART = capnometry-assisted respiratory training; CT = cognitive skill training. ns = non significant differences between treatment conditions; *p < .05, significant differences between treatment conditions.
Effect of Baseline Perceived Control
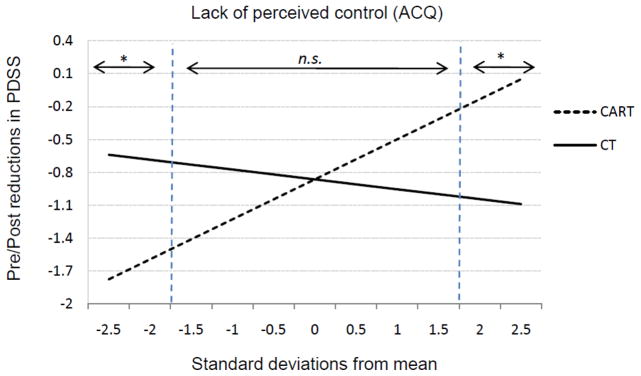
Similarly to misappraisal, baseline levels of perceived control affected reductions in PDSS differently in the two treatment conditions (i.e., the triple interaction between Time, lack of perceived control, and treatment condition was significant), b = −.36, t(58) = 2.51, p < .05. Decomposing this interaction by examining the effect of lack of control within each treatment condition, we found that, in CART, greater lack of control was related to lower reductions in PDSS over time, b = .35, t(58) = 3.22, p < .005 (Figure 2), whereas its effect in CT was not significant, b = .01, t(58) = .07, p = .94. Similarly, we evaluated the effect of treatment condition on change in PDSS for individuals high and low in perceived control (1 SD above or below the mean). Here, patients with high lack of control showed greater reductions in PDSS when receiving CT compared to CART, b = .36, t(58) = 2.37, p < .05 (Figure 2). On the other hand, those with low lack of control had greater reductions in CART compared to CT, but the differences were only significant for patients with very low lack of control (1.75 SD below the mean), b = .62, t(58) = 2.03, p = .05. Rate of improvement did not differ among conditions for mean levels of lack of control, p = .99.
FIGURE 2.
Pre-Post reductions in PDSS in CART and CT for very high to very low levels of lack of perceived control (ACQ). CART = capnometry-assisted respiratory training; CT = cognitive skill training. ns = non significant differences between treatment conditions; *p < .05, significant differences between treatment conditions.
DISCUSSION
The aim of this study was to examine the degree to which initial levels of panic-related cognitions (catastrophic appraisal and perceived control) were predictive of panic symptom reductions, and whether the effect would be moderated by the type of intervention the patient received. The mechanistically-distinct psychosocial interventions each focused exclusively on manipulating one specific factor related to PD: catastrophic cognitions (in CT) or aberrant respiratory patterns (in CART). Although both interventions have been shown to effectively and equally reduce panic symptom severity, reductions were achieved through different pathways, consistent with their underlying models (Meuret et al., in press).
As predicted, we found a moderating effect for baseline cognitive misappraisal. However, the relation was counter to our expectation. Individuals with greater initial levels of catastrophic cognitions showed smaller reduction in panic symptom severity when receiving CT, but showed greater improvements when receiving CART. The findings in the CT condition are consistent with previous studies which generally found that higher baseline misappraisal was related to poorer outcome in cognitive/behavioral interventions (Hicks et al., 2005; Keijsers et al., 1994; Schneider & Schulte, 2008). However, the findings are novel in that they suggest differential responding to a cognitive risk factor across two very different types of interventions. Whereas misappraisal has been studied in a number of investigations as a predictor of treatment outcome, moderation across more than one treatment condition has been tested in only few studies (Hicks et al., 2005; albeit only social catastrophe; Dow et al., 2007). In contrast, patients with lower levels of catastrophic cognitions showed larger reductions in panic severity when receiving CT compared to CART. One explanation for the differential response to treatment modalities may relate to the pathways by which change in panic severity was achieved. The data suggest that specific types of PD patients (those with very high levels of catastrophic cognitions) are more resistant to change when receiving CT. Those patients may be entrenched in their panic related cognitions. As a result, they have greater difficulty changing such cognitions and attributions through logic and theory, resulting in smaller reductions in panic symptom severity. For example, in CT, fearful cognitions, such as concerns about suffocating when feeling sensations of shortness of breath, would be targeted by disputing and countering them with alternative explanations (e.g., You have never suffocated even when feeling very short of breath). While such theoretical argument may be persuasive in the moment it could be undermined by entrenched negative attributions. Indeed, our findings suggest that individuals with moderate to low levels of catastrophic cognitions respond better compared to those who are more intensively plagued by mal-adaptive attributions.
Compared to CT, CART offers patients with direct and objective physiological feedback (via capnometry) about their feared bodily functions, which are most often cardiorespiratory in nature (e.g., shortness of breath, heart racing; Meuret et al., 2006). The repeated feedback of PCO2, respiration rate, heart rate, and oxygen saturation is likely to have a powerful cognitive and biological impact. Patients learn that certain bodily processes (e.g., decreased levels of PCO2) are related to emotional states but are not catastrophic in nature (e.g., shortness of breath is due to reduced levels of PCO2, not lack of oxygen). They also learn that these biological processes can be altered and consequently result in less symptom production. Thus, the direct physiological feedback and manipulation is likely to negate the mystical nature of bodily sensations. Furthermore, the alteration of physiological states (e.g., hypocapnia) has been shown to mediate reductions in catastrophic thinking and panic symptom severity (Meuret et al., in press; Meuret, Rosenfield, Hofmann, Suvak, & Roth, 2009).
An interesting, albeit unexpected, moderating effect was further observed for baseline level of lack of perceived emotional control. In accordance with our predictions, individuals who believed themselves to have limited situational and emotional control over threatening events demonstrated less improvement in panic symptom severity. However this relation was only true for individuals receiving CART. Thus, high initial levels of control led to greater success in response to a biofeedback technique that required exercising control over bodily functions. In CT, initial overall levels of control were not predictive of outcome. However individuals with extremely low perceived control showed greater improvements in CT than in CART. It could be speculated that patients with fatalistic convictions or helpless reliance on others are more receptive to cognitive restructuring exercises because the exercises provide an opportunity to dispute their convictions. The findings illustrate the complexity of the moderating influences within, but also between, distinct interventions.
Taken together, whereas overall improvement did not differ among treatment modalities, moderating effects specific to pretreatment characteristics emerged. That is, individuals with higher initial levels of catastrophic cognitions or with lower lack of control have better outcomes when receiving CART. In contrast, low initial levels of catastrophic cognitions or greater lack of control were related to better outcome when receiving CT. It is crucial to highlight that these findings relate to different underlying processes specific to patients’ characteristics. That is, the influencing effects of one moderator are controlled for while examining the effects of another (e.g., the unique effect of perceived emotional control, controlling for misappraisal, initial panic severity, and homework compliance).
Homework compliance (defined as the number of homework assignments completed) was related to greater reductions in PDSS. The finding is consistent with the majority of studies for anxiety disorders (Edelman & Chambless, 1993; Leung & Heimberg, 1996; Westra, Arkowitz, & Dozois, 2009). Furthermore, the results suggest that amount of practice using a given technique is directly related to improvement in outcomes, seemingly regardless of therapeutic technique. This finding underscores the need to develop general approaches that can enhance homework compliance across a variety of therapeutic interventions.
No relation was found between initial panic symptom severity and reductions in PDSS for CT, a finding that is consistent with earlier research in cognitive or behavior type interventions (e.g., Chambless & Gracely, 1988; Emmelkamp & van den Hout, 1983; but Aaronson et al., 2008). However, a significant relation was found for CART, where higher initial levels of panic symptom severity were predictive of greater reductions therein. These effects may simply reflect regression to the mean.
Despite the intriguing findings of this study, some limitations deserve mention. While the current study is the first of its type to objectively assess the effect of quantity of homework compliance on outcome (in two distinct PD interventions), the effect of the quality of homework done was not evaluated. Concerning our MRM model, we had ten predictors and only 79 total observations. Although this ratio is higher than what is typically recommended (Tabachnick & Fidell, 2007), we pursued a reasonable approach to reduce the number of predictors. More specifically, we excluded all higher order interactions that were not significant. Additionally, every retained predictor was significant in at least one of the follow-up analyses decomposing the higher order interactions. Deleting some of these significant predictors (or examining moderators separately) would have led to bias in the calculation of the remaining regression coefficients. It should be noted that Mass and Hox (2005) have shown that regression coefficients and variance components in MRM analyses are unbiased and accurate in sample sizes as low as 30 subjects as long as one uses restricted maximum likelihood estimation.
Despite these limitations, the current findings represent an important step forward in our understanding of the role of panic-related cognitions in predicting response in mechanistically-distinct interventions for panic disorder.
Acknowledgments
Writing of this article was partially supported by Grant R01HL089761-01A1 (awarded to Dr. Meuret) from the National Institutes of Health and the generous support of the Beth and Russell Siegelman Foundation (Dr. Meuret). Dr. Hofmann is supported by NIMH Grant MH079236. He is also a paid consultant of Merck Pharmaceuticals.
Footnotes
We are grateful to Ms. Ashton Jeter for her assistance with this manuscript.
Contributor Information
Alicia E. Meuret, Southern Methodist University
Stefan G. Hofmann, Boston University
David Rosenfield, Southern Methodist University.
References
- Aaronson CJ, Shear MK, Goetz RR, Allen LB, Barlow DH, White KS, et al. Predictors and time course of response among panic disorder patients treated with cognitive-behavioral therapy. Journal of Clinical Psychiatry. 2008;69:418–124. doi: 10.4088/jcp.v69n0312. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford; 2002. [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. The Journal of the American Medical Association. 2000;283:2573–2574. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Long-term outcome in cognitive-behavioral treatment of panic disorder: Clinical predictors and alternative strategies for assessment. Journal of Consulting and Clinical Psychology. 1995;63:754–765. doi: 10.1037//0022-006x.63.5.754. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Caputo GC, Bright P, Gallagher R. Assessment of fear in agoraphobics: The body sensations questionnaire and the agoraphobic cognitions questionnaire. Journal of Consulting and Clinical Psychology. 1984;52:1090–1097. doi: 10.1037//0022-006x.52.6.1090. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Gracely EJ. Prediction of outcome with in vivo treatment of agoraphobics. In: Hand I, Wittchen H-U, editors. Panic and phobia. II. Berlin: Springer; 1988. pp. 209–220. [Google Scholar]
- Clark DM. A cognitive approach to panic. Behavior Research and Therapy. 1986;24:461–470. doi: 10.1016/0005-7967(86)90011-2. [DOI] [PubMed] [Google Scholar]
- Craske MG, Barlow DH, Meadows E. Mastery of your anxiety and panic: Therapist guide for anxiety, panic, and agoraphobia (MAP-3) San Antonio, TX: Psychological Corporation; 2000. [Google Scholar]
- Deacon B, Lickel J, Abramowitz JS. Medical utilization across the anxiety disorders. Journal of Anxiety Disorders. 2008;22:344–350. doi: 10.1016/j.janxdis.2007.03.004. [DOI] [PubMed] [Google Scholar]
- Dow MG, Kenardy JA, Johnston DW, Newman MG, Taylor CB, Thomson A. Prognostic indices with brief and standard CBT for panic disorder: II. Moderators of outcome. Psychological Medicine. 2007;37:1503–1509. doi: 10.1017/S0033291707000682. [DOI] [PubMed] [Google Scholar]
- Edelman RE, Chambless DL. Compliance during sessions and homework in exposure-based treatment of agoraphobia. Behaviour Research and Therapy. 1993;31:767–773. doi: 10.1016/0005-7967(93)90007-h. [DOI] [PubMed] [Google Scholar]
- Emmelkamp PMG, van den Hout A. Failure in treating agoraphobia. In: Foa EB, Emmelkamp PMG, editors. Failures in behavior therapy. New York: Wiley; 1983. pp. 58–81. [Google Scholar]
- Gibbons RD, Hedeker D, Elkin I, Waternaux C, Kraemer HC, Greenhouse JB, et al. Some conceptual and statistical issues in analysis of longitudinal psychiatric data: Application to the NIMH treatment of depression collaborative research program dataset. Archives of General Psychiatry. 1993;50:739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- Haby MM, Donnelly M, Corry J, Vos T. Cognitive behavioural therapy for depression, panic disorder and generalized anxiety disorder: a meta-regression of factors that may predict outcome. The Australian and New Zealand Journal of Psychiatry. 2006;40:9–19. doi: 10.1080/j.1440-1614.2006.01736.x. [DOI] [PubMed] [Google Scholar]
- Hamer RM, Simpson PM. Last observation carried forward versus mixed models in the analysis of psychiatric clinical trials. The American Journal of Psychiatry. 2009;166:639–641. doi: 10.1176/appi.ajp.2009.09040458. [DOI] [PubMed] [Google Scholar]
- Hicks TV, Leitenberg H, Barlow DH, Gorman JM, Shear MK, Woods SW. Physical, mental, and social catastrophic cognitions as prognostic factors in cognitive-behavioral and pharmacological treatments for panic disorder. Journal of Consulting and Clinical Psychology. 2005;73:506–514. doi: 10.1037/0022-006X.73.3.506. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Keijsers GP, Hoogduin CA, Schaap CP. Predictors of treatment outcome in the behavioural treatment of obsessive-compulsive disorder. The British Journal of Psychiatry. 1994;165:781–786. doi: 10.1192/bjp.165.6.781. [DOI] [PubMed] [Google Scholar]
- Keller MB, Yonkers KA, Warshaw MG, Pratt LA, Gollan JK, Massion AO, et al. Remission and relapse in subjects with panic disorder and panic with agoraphobia: A prospective short-interval naturalistic follow-up. The Journal of Nervous and Mental Disease. 1994;182:290–296. doi: 10.1097/00005053-199405000-00007. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and co-morbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klass ET, Milrod BL, Leon AC, Kay SJ, Schwalberg M, Li C, et al. Does interpersonal loss preceding panic disorder onset moderate response to psychotherapy? An exploratory study. The Journal of Clinical Psychiatry. 2009;70:406–411. doi: 10.4088/jcp.08m04248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM, Ouellette R, Johnson J, Greenwald S. Panic attacks in the community. Social morbidity and health care utilization. The Journal of the American Medical Association. 1991;265:742–746. [PubMed] [Google Scholar]
- Kraemer HC, Frank E, Kupfer DJ. Moderators of treatment outcomes: Clinical, research, and policy importance. The Journal of the American Medical Association. 2006;296:1286–1289. doi: 10.1001/jama.296.10.1286. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Leon AC, Portera L, Weissman MM. The social costs of anxiety disorders. The British Journal of Psychiatry. 1995;27:19–22. [PubMed] [Google Scholar]
- Leung AW, Heimberg RG. Homework compliance, perceptions of control, and outcome of cognitive-behavioral treatment of social phobia. Behaviour Research and Therapy. 1996;34:423–432. doi: 10.1016/0005-7967(96)00014-9. [DOI] [PubMed] [Google Scholar]
- Mass CJM, Hox JJ. Sufficient sample sizes for multilevel modeling. Methodology. 2005;1:86–92. [Google Scholar]
- McNally RJ. Panic disorder: A critical analysis. New York: Guilford; 1994. [Google Scholar]
- Meuret AE, Rosenfield D, Hofmann SG, Suvak MK, Roth WT. Changes in respiration mediate changes in fear of bodily sensations in panic disorder. Journal of Psychiatric Research. 2009;43:634–641. doi: 10.1016/j.jpsychires.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Rosenfield D, Seidel A, Bhaskara L, Hofmann SG. Respiratory and cognitive mediators of treatment change in panic disorder: Evidence for intervention specificity. Journal of Consulting and Clinical Psychology. doi: 10.1037/a0019552. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Wilhelm FH, Ritz T, Roth WT. Feedback of end-tidal pCO2 as a therapeutic approach for panic disorder. Journal of Psychiatric Research. 2008;42:560–568. doi: 10.1016/j.jpsychires.2007.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meuret AE, Wilhelm FH, Roth WT. Respiratory biofeedback-assisted therapy in panic disorder. Behavior Modification. 2001;25:584–605. doi: 10.1177/0145445501254006. [DOI] [PubMed] [Google Scholar]
- Meuret AE, Wilhelm FH, Roth WT. Respiratory feedback for treating panic disorder. Journal of Clinical Psychology. 2004;60:197–207. doi: 10.1002/jclp.10245. [DOI] [PubMed] [Google Scholar]
- Meuret AE, White KS, Ritz T, Roth WT, Hofmann SG, Brown T. Panic attack symptom dimensions and their relationship to illness characteristics in panic disorder. Journal of Psychiatric Research. 2006;6:520–527. doi: 10.1016/j.jpsychires.2005.09.006. [DOI] [PubMed] [Google Scholar]
- Meuret AE, Wolitzky-Taylor KB, Twohig MP, Craske MG. Coping skills and exposure therapy in panic disorder and agoraphobia: Latest advances and future directions. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milrod B, Leon AC, Busch F, Rudden M, Schwalberg M, Clarkin J, et al. A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. The American Journal of Psychiatry. 2007;164:265–272. doi: 10.1176/ajp.2007.164.2.265. [DOI] [PubMed] [Google Scholar]
- Mineka S, Kelly KA. The relationship vetween anxiety, lack of control, and loss of control. In: Steptoe A, Appels A, editors. Stress, personal control, and health. New York: Wiley; 1989. pp. 163–191. [Google Scholar]
- Mitte K. A meta-analysis of the efficacy of psycho- and pharmacotherapy in panic disorder with and without agoraphobia. Journal of Affective Disorders. 2005;88:27–45. doi: 10.1016/j.jad.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Newman MG, Kenardy J, Herman S, Taylor CB. Comparison of palmtop-computer-assisted brief cognitive-behavioral treatment to cognitive-behavioral treatment for panic disorder. Journal of Consulting and Clinical Psychology. 1997;65:178–183. doi: 10.1037//0022-006x.65.1.178. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Craske MG, Brown TA, Barlow DH. Measurement of perceived control over anxiety-related events. Behavior Therapy. 1996;27:279–293. [Google Scholar]
- Rees CS, McEvoy P, Nathan PR. Relationship between homework completion and outcome in cognitive behaviour therapy. Cognitive Behaviour Therapy. 2005;34:242–247. doi: 10.1080/16506070510011548. [DOI] [PubMed] [Google Scholar]
- Reiss S, Peterson R, Gursky D, McNally R. Anxiety sensitivity, anxiety frequency, and the prediction of fearfulness. Behavior Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Woolaway-Bickel K. The effects of treatment compliance on outcome in cognitive-behavioral therapy for panic disorder: Quality versus quantity. Journal of Consulting and Clinical Psychology. 2000;68:13–18. doi: 10.1037//0022-006x.68.1.13. [DOI] [PubMed] [Google Scholar]
- Schneider R, Schulte D. Catastrophic associations predict level of change in anxiety sensitivity in response to cognitive-behavioural treatment for panic. Behaviour Research and Therapy. 2008;46:557–727. doi: 10.1016/j.brat.2008.01.015. [DOI] [PubMed] [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, et al. Multicenter collaborative panic disorder severity scale. The American Journal of Psychiatry. 1997;154:1571–1575. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 5. Boston: Allyn and Bacon; 2007. [Google Scholar]
- Westra HA, Arkowitz H, Dozois DJ. Adding a motivational interviewing pretreatment to cognitive behavioral therapy for generalized anxiety disorder: A preliminary randomized controlled trial. Journal of Anxiety Disorders. 2009;23:1106–1117. doi: 10.1016/j.janxdis.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westra HA, Dozois DJ, Marcus M. Expectancy, homework compliance, and initial change in cognitive-behavioral therapy for anxiety. Journal of Consulting and Clinical Psychology. 2007;75:363–373. doi: 10.1037/0022-006X.75.3.363. [DOI] [PubMed] [Google Scholar]
- White KS, Brown TA, Somers TJ, Barlow DH. Avoidance behavior in panic disorder: The moderating influence of perceived control. Behaviour Research and Therapy. 2006;44:147–157. doi: 10.1016/j.brat.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Woods CM, Chambless DL, Steketee G. Homework compliance and behavior therapy outcome for panic with agoraphobia and obsessive compulsive disorder. Cognitive Behavior Therapy. 2002;31:88–95. [Google Scholar]