Abstract
The prevalence of chronic hepatitis B (HBV) among college-age US-born Asian and Pacific Islanders (A/PI) is not well known.
OBJECTIVES
To compare the prevalence of hepatitis B surface antigen (HBsAg) seropositivity in US-born to A/PI-born students at a public university.
PARTICIPANTS
Undergraduate who self-identified themselves as A/PI.
RESULTS
Of 145 US-born A/PI, 1.4% (C.I. = 0.0%, 3.3%) tested positive for HBsAg compared to 3.3% (C.I. = 0.5%, 6.1%) of the 152 A/PI-born students. Approximately 1/3 of all students were unaware of their HBV vaccination status.
CONCLUSIONS
HBsAg prevalence among A/PI undergraduates, including US-born, is considerably higher (3–11 times) than the mainstream US population (0.3–0.5%) and supports CDC recommendations for testing all persons of A/PI ancestry, including US-born persons whose parents were born in regions with HBsAg prevalence of ≥8%. Awareness of HBV vaccination status was relatively low and vaccination did not assure that individuals were HBsAg negative.
Background
According to the World Health Organization, approximately 2 billion people worldwide have been infected with the hepatitis B virus (HBV) and approximately 350 million are chronically infected1. In addition to causing cirrhosis, chronic hepatitis B is to a large extent responsible for hepatocellular carcinoma, the third leading cause of cancer mortality in the world2. Although only 0.3% – 0.5% of US residents are chronically infected with the HBV3, liver cancer mortality rates in the U.S. are experiencing the highest rate of increase among all types of cancers.4 Furthermore, in the U.S., between 2010 to 2030, liver cancer incidence rates are anticipated to increase by 59%, in part due to increasing numbers of Asian immigrants.4 Of U.S. residents chronically infected with HBV, 40% to 70% are foreign-born immigrants, principally from Asia and the Pacific Islands5 whose cancer rates are projected to increase by 132% by 2030.6 In the US, the NHANES III (1988–1994) study estimated the prevalence of chronic HBV to be 0.42% (95% CI = 0.32, 0.55).3 However, the NHANES population sampled was predominantly Caucasian and immigrants were underrepresented. Given that a large proportion of the HBV-infected population in the US is comprised of immigrants from countries with a high prevalence of chronic hepatitis B, such as Asia or the Pacific Islands7, the HBV prevalence in the US is likely underestimated.
Screening studies demonstrating a high prevalence of hepatitis B surface antigen (HBsAg) among Asian and Pacific Islanders (A/PI) living in the US8–10 led to recent recommendations to test persons born in geographic regions with HBsAg prevalence of ≥2% and US born persons not vaccinated at birth parents were born in geographic regions with HBsAg prevalence of ≥8%. However, data on the seroprevalence of HBsAg among young adult A/PI to support the latter recommendation are scant. In addition, the usefulness of self-reported HBV vaccination status in this group to predict HBV infection has not been studied.
The current study aimed to determine HBsAg prevalence in US-born A/PI college students and compare the result to the prevalence in A/PI-born college students, as well as to examine the awareness of HBV vaccination status among these students.
Methods
Recruitment
Undergraduate students aged 18 years and older matriculating at a large public university in California who had identified themselves as an A/PI ethnicity during enrollment were sent an invitation through their campus email account to volunteer to participate in a study about HBV. All students at the university are assigned an email account and its use is required for a variety of campus communications. Upon enrollment, students are also requested to self-identify their race and ethnicity. For this study we enrolled students who identified themselves as Chinese-American/Chinese, Vietnamese, Filipino, East Indian/Pakistani, Korean-American/Korean, Pacific Islander, and Other Asian (Table 1).
Table 1.
Distribution of Reported Country of Birth of A/PI Students and Mothers of US-Born Students, n (%)
| Mothers of US-Born Students | A/PI-Born Students | |
|---|---|---|
| All Countries | 145 | 1521 |
| Country | ||
| China | 41 (28.3) | 61 (40.1) |
| Vietnam | 32 (22.1) | 38 (25.0) |
| US | 24 (16.6) | NA |
| Taiwan | 17 (11.7) | 20 (13.2) |
| Korea | 9 (6.2) | 12 (7.9) |
| Laos | 8 (5.5) | 0 (0.0) |
| Japan | 3 (2.1) | 6 (3.9) |
| Thailand | 1 (0.7) | 4 (2.6) |
| Other | 10 (6.9)2 | 11 (7.2)3 |
Seven subjects born in low prevalence countries were excluded.
Burma, Cambodia, India, Malaysia (2 each); Micronesia and Philippines (1 each)
Burma and India (2 each); Bangladesh, Cambodia, Indonesia, Malaysia, Philippines, Samoa and Singapore (1 each)
Recruitment emails were sent during the Fall quarters of 2007 and 2008 to all undergraduate students who had identified themselves as being of an A/PI. Students interested in participating in the study replied to the recruitment email with their name, gender, age, ethnicity, and country of birth. Equal numbers of US-born and foreign-born students were invited to attend recruitment meetings. Invitations to the meetings were based on the order in which replies to the initial recruitment email were received. At the meetings, a presentation on HBV was given and details of the study were explained. Following the presentation, written informed consent was obtained, a questionnaire administered, and a blood sample taken for HBsAg testing. Meeting dates were held on campus throughout the year with each meeting date comprising three or four 30-minute sessions with approximately 15–20 students per session. Individual results of the HBsAg serology were sent to each student by US mail. Students who tested positive were also advised in the letter to seek further medical care from their physician, have family members tested and avoid behaviors that can spread HBV. Of note, all students are required to carry health insurance either through the university or privately. The study was approved by the Institutional Review Board and written informed consent was obtained from all participants.
Statistical analysis
Seven participants were foreign-born A/PI students but not born in Asia or Pacific Islands and were excluded from the analysis. Because age was not normally distributed, the two-sided Wilcoxon-Mann-Whitney test was used. The two-sided Fisher’s exact test was used to compare the US-born group to the Asia-born group for HBsAg seropositivity, the proportion of females and HBV vaccine status. A 95% confidence interval was obtained based the exact binomial method. Participants who were unsure of their HBV vaccination status were excluded from the comparison analysis, but included in all other analyses. Simple logistic regression was used to evaluate whether HBsAg positivity was statistically significantly associated with each of these factors: country of birth, gender, age, HBV vaccination status, and parent’s country of birth
Results
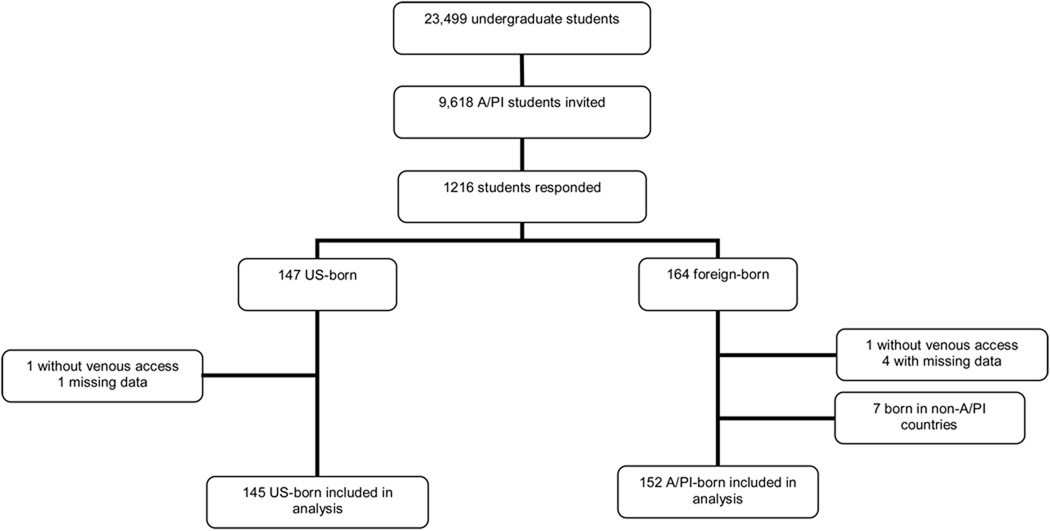
According to university statistics compiled for Fall 2007, there were 23,499 undergraduate students at the university, among which 9,618 students (42%) identified themselves as an A/PI ethnicity. 612 students responded to the first email invitation and 604 students who did not respond to the first email responded to the second email invitation (Figure 1). Between November 1, 2007 and November 24, 2008, 311 students were enrolled in the study; complete serologic, demographic and questionnaire data were available on 304 students.
Figure 1.
Study design, recruitment and enrollment of Asian and Pacific Islander undergraduate university students for the study of HBsAg seroprevalence.
Of the enrolled subjects with complete data (n=304), 145 (47.70%) were born in the US and 159 (52.30%) were born in foreign countries (Tables 1 and 2). Seven of the foreign-born students were born in non-A/PI countries including Australia (2), Brazil (1), Canada (1), England (1), Germany (1), and Saudi Arabia (1) and were excluded from analysis. Among the US-born students, 121 (83.45%) were born to immigrant mothers, all from Asian countries or the Pacific Islands. There was no statistically significant difference in gender between the US-born and A/PI-born groups (63% female versus 63% female, respectively, p = 0.90). Note that females comprise 56% of the total undergraduate population, but the gender distribution in the population of A/PI undergraduate students is not available. The mean (+/− standard deviation) age of US-born (19.5 ± 1.3 y) was significantly lower than of A/PI-born students (20.6 ± 2.8, P<0.0001).
Table 2.
Comparison of HB seropositivity and Vaccination Status in US-born to Asia/Pacific Islander-born students
| US-born (n = 145) | A/PI-born (n = 152) | |
|---|---|---|
| Age (mean +/− SD) | 19.5 ± 1.3 y | 20.6 ± 2.8 y * |
| Gender (Female) | 92 (63.4%) | 95 (62.5%) |
| HBsAg positive | 2 (1.4%) | 5 (3.3%) |
| Self-reported HBV Vaccination | ||
| Yes | 99 (68.3%) | 95 (62.5%) |
| No | 2 (1.4%) | 3 (2.0%) |
| Unsure | 44 (30.3%) | 54 (35.5%) |
p < 0.001 (two-sided Wilcoxon-Mann-Whitney test)
Overall, nearly one-third of all students (32.9%) reported that they did not know if they had received the HBV vaccine. There was no statistically significant difference (P = 0.7) in self-reported HBV vaccination between the US-born (69.7%, C.I. = 61.5%, 77.0%) and A/PI-born (64.5%, C.I. = 56.3%, 72.1%) groups.
Of the total sample, 7 students (2.3%) tested positive for HBsAg: 2 students from the US-born group (1.4%, C.I. = 0.0%, 3.3%) and 5 from the A/PI-born group (3.3%, C.I. = 0.5%, 6.1%). Both HBsAg-positive US-born students were born of immigrant mothers (Korea and Vietnam, respectively), giving a prevalence of 1.7% (C.I. = 0.0%, 3.9%) among US-born students born of immigrant mothers (Table 3). Of the five A/PI-born HBsAg-positive students, one was born in China and four in Vietnam. There was no statistically significant difference in HBsAg prevalence between the US-born group and the A/PI-born group (P = 0.45). Of the 7 HBsAg seropositive students, 4 recalled having received the HBV vaccine.
Table 3.
Prevalence rates of HBsAg in University Undergraduate Students in California, USA
| Prevalence (95% confidence interval) | |
|---|---|
| Asian/Pacific Islander Born (n = 152) | 3.3% (0.5% – 6.1%) |
| US Born (n = 145) | 1.4% (0.0% – 3.3%) |
| US Born of Immigrant Mothers (n = 121) | 1.7% (0.0% – 3.9%) |
| Chinese Born (n = 61) | 1.6% (0.0% – 4.8%) |
| Vietnamese Born (n = 38) | 10.5% (0.8% – 20.3%) |
Simple logistic regression did not reveal any significant associations between HBsAg positivity and country of birth, gender, age, or parents’ country of birth. Presence of HBsAg was negatively associated with reported HBV vaccination (OR 0.03, P = 0.01). In other words, a reported lack of HBV vaccination was associated with an increased risk of testing positive for HBsAg.
Comment
Previous studies of the prevalence of chronic HBV infection in Asians and Pacific Islander living in the US have focused mostly on older adult populations. In New York City, 15% of A/PI participants born outside the US had chronic HBV infection with a mean age of 45 years (range: 20–83 years).10 In a clinic serving the Asian community in the San Francisco Bay Area, the prevalence of chronic HBV infection was reported to be 8.9% with a median age of 52.9 years (range: 18–101 years).9 A survey of 6,130 unvaccinated Korean-Americans between 1988 and 1990 in the eastern US found an overall HBsAg prevalence of 6.1%.8 These rates are considerably higher than either the US-born or A/PI-born groups studied in this paper and may be related to demographic factors associated with college students, such as younger age and higher socioeconomic status.
Our study population was considerably younger than prior studies and the 1.7% prevalence in US-born A/PI students whose mothers were immigrants and should have been screened for HBV during pregnancy demonstrates the need to target this population for screening. In 1984, the Centers for Disease Control and Prevention (CDC) recommended screening for HBsAg in pregnant women in groups known to be at high risk for HBV infection.11 The CDC expanded this recommendation to routinely screen all pregnant women for HBsAg in 1988.12 However, proper implementation of screening and appropriate prophylaxis of infants has been inadequate. A study in New York City from July 1987 to June 1988 found that only 59% of infants born to HBsAg-positive mothers received HBV immune globulin and 3 doses of the vaccine.13 Two years after the 1988 CDC recommendation, a survey of birthing hospitals in 14 States found that 96.5% of pregnant women were screened for HBsAg, but the rate of administration of HBV immune globulin and 3 doses of the vaccine for the newborn was only 71%.14
In our study, nearly one in three of all students reported not knowing their HBV vaccination status, despite the university requirement for all students younger than 18 years of age to document HBV vaccination prior to matriculation. In addition, although reporting a history of HBV vaccination was associated with a lower risk of testing positive for HBsAg, 4 of the 7 students who tested positive for HBsAg reported that they had received the HBV vaccine. These results suggest that self-reported HBV vaccination status is not a reliable predictor of HBsAg status and should not preclude HBV screening.
Overall, the prevalence of HBsAg among A/PI students in our study was 2.3%; 1.4% in US-born students and 3.3% in A/PI-born students. Although there was no statistically significant difference between these two groups, the results indicate that these percentages are approximately 3– 11 fold higher than the US population at large3. Even for students born in the US, this study found that the rate of chronic HBV infection is at least 10 times greater than the rate of infection among the general US-born non-institutionalized population.5 Somewhat concerning is that these rates are similar to those found in Korean-Americans under 20 years of age prior to universal infant vaccination8. In that study, the HBsAg seroprevalence for those less than 20 years was 2.7% (12/452) for the US-born and 5.5% for the Korean-born groups.
Limitations
Our findings should be interpreted within the context of limitations, principally of the small sample size. Our study was underpowered to detect a difference between the two groups. Thus, what we have reported should be considered a pilot study that deserves both amplification and replication. Another limitation was the predominance of females in our study. We believe this reflected the demographic composition of our study population, as females constitute the majority of the students enrolled at the university. The gender composition of our study population may have caused us to underestimate the true prevalence in young adult A/PI as previous studies have shown a higher prevalence of HBsAg among males.8–10 Finally, HBV vaccination status relied on self-reported information and not documented completion of the 3 dose vaccination series or HBs antibody. We documented considerable lack of awareness of HBV vaccination status, as approximately one-third of the respondents were unsure of their own vaccination status. We believe our study results exemplify the greater need for health education among undergraduates regarding their own health as well as empirically documenting that HBV vaccination is no assurance of being HBsAg seronegative.
Conclusions
In summary, the prevalence of HBsAg appears to be high in A/PI college students, including those born in the US and particularly those born of immigrant mothers, relative to the general US adult population. These findings support the CDC recommendations for testing US born persons whose parents were born in geographic regions with HBsAg prevalence of ≥8%.5 However, our results suggest that testing should not be limited, based upon self-reported vaccination status. In addition, HBsAg testing should precede vaccination in these individuals as recommended by the CDC5. Finally, we have demonstrated an efficient model for HBV screening that may be easily employed by other campuses with a high percentage of A/PI students.
Acknowledgements
Support for this study was provided by a research grant from Gilead Sciences, Inc.
Personnel time for M. Chen was furnished through U01 CA11460.
Statistical support was made possible by Grant Number UL1 RR024146 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on Reengineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
Footnotes
Conflict of Interest
C.L.B. has received honoraria and grant support from Gilead Sciences, Inc.
References
- 1. [Accessed August 31, 2008];Hepatitis B Fact sheet No. 204. 2008 http://www.who.int/mediacentre/factsheets/fs204/en/.
- 2.Parkin DM. Global cancer statistics in the year 2000. Lancet Oncol. 2001;2:533–543. doi: 10.1016/S1470-2045(01)00486-7. [DOI] [PubMed] [Google Scholar]
- 3.McQuillan GM, Coleman PJ, Kruszon-Moran D, Moyer LA, Lambert SB, Margolis HS. Prevalence of hepatitis B virus infection in the United States: the National Health and Nutrition Examination Surveys, 1976 through 1994. Am J Public Health. 1999;89:14–18. doi: 10.2105/ajph.89.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 5.Weinbaum CM, Williams I, Mast EE, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm Rep. 2008;57:1–20. [PubMed] [Google Scholar]
- 6.Smith BD, Smith GL, Hurria A, Hortobagyi GN, Buchholz TA. Future of cancer incidence in the United States: Burdens upon an aging, changing nation. J Clin Oncol. 2009 doi: 10.1200/JCO.2008.20.8983. [DOI] [PubMed] [Google Scholar]
- 7.Mast EE, Weinbaum CM, Fiore AE, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) Part II: immunization of adults. MMWR Recomm Rep. 2006;55:1–33. [PubMed] [Google Scholar]
- 8.Hann HW, Hann RS, Maddrey WC. Hepatitis B virus infection in 6,130 unvaccinated Korean-Americans surveyed between 1988 and 1990. Am J Gastroenterol. 2007;102:767–772. doi: 10.1111/j.1572-0241.2007.01060.x. [DOI] [PubMed] [Google Scholar]
- 9.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46:1034–1040. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- 10.Pollack H, Wan K, Ramos R, et al. Screening for chronic hepatitis B among Asian/Pacific Islander populations--New York City, 2005. MMWR Morb Mortal Wkly Rep. 2006;55:505–509. [PubMed] [Google Scholar]
- 11.Postexposure prophylaxis of hepatitis B. MMWR Morb Mortal Wkly Rep. 1984;33:285–290. [PubMed] [Google Scholar]
- 12.Prevention of perinatal transmission of hepatitis B virus: prenatal screening of all pregnant women for hepatitis B surface antigen. MMWR Morb Mortal Wkly Rep. 1988;37:341–346. 351. [PubMed] [Google Scholar]
- 13.Henning KJ, Pollack DM, Friedman SM. A neonatal hepatitis B surveillance and vaccination program: New York City, 1987 to 1988. Am J Public Health. 1992;82:885–888. doi: 10.2105/ajph.82.6.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hepatitis B vaccination--United States, 1982–2002. MMWR Morb Mortal Wkly Rep. 2002;51:549–552. 563. [PubMed] [Google Scholar]