Abstract
Background
The revised cardiac risk index (RCRI) is associated strongly with increased cardiac ischaemic risk and perioperative death. Associations with non-cardiac morbidity in non-cardiac surgery have not been explored. In the elective orthopaedic surgical population, morbidity is common but preoperative predictors are unclear. We hypothesized that RCRI would identify individuals at increased risk of non-cardiac morbidity in this surgically homogenous population.
Methods
Five hundred and sixty patients undergoing elective primary (>90%) and revision hip and knee procedures were studied. A modified RCRI (mRCRI) score was calculated, weighting intermediate and low risk factors. The primary endpoint was the development of morbidity, collected prospectively using the Postoperative Morbidity Survey, on postoperative day (POD) 5.
Results
Morbidity on POD 5 was more frequent in patients with mRCRI ≥3 {relative risk 1.7, [95% confidence interval (CI): 1.4–2.1]; P<0.001}. Time to hospital discharge was delayed in patients with mRCRI score ≥3 (log-rank test, P=0.0002). Pulmonary (P<0.001), infectious (P=0.001), cardiovascular (P=0.0003), renal (P<0.0001), wound (P=0.02), and neurological (P=0.002) morbidities were more common in patients with mRCRI score ≥3. Pre/postoperative haematocrit, anaesthetic/analgesic technique, and postoperative temperature were similar across mRCRI groups. There were significant associations with hospital stay, as measured by the area under the receiver-operating characteristic curves for mRCRI 0.64 (95% CI: 0.58–0.70) and POSSUM 0.70 (95% CI: 0.63–0.75).
Conclusions
mRCRI score ≥3 is associated with increased postoperative non-cardiac morbidity and prolonged hospital stay after elective orthopaedic procedures. mRCRI can contribute to objective risk stratification of postoperative morbidity.
Keywords: assessment, preanaesthetic; complications, morbidity; surgery, non-cardiac; surgery, orthopaedic
Key points.
The association of the revised cardiac risk index (RCRI) with non-cardiac morbidity after surgery has not been investigated.
RCRI was calculated in 560 patients undergoing major orthopaedic procedures.
Higher RCRI scores were associated with increased postoperative non-cardiac morbidity and length of hospital stay.
RCRI scoring may have a role in risk stratification to optimize health-care delivery.
The revised cardiac risk index (RCRI) has been used primarily to stratify the risk of perioperative ischaemic cardiac events, death, or both.1–3 Associations with non-cardiac morbidity in non-cardiac surgery have not been explored in a prospective study. Major joint replacement surgery is associated with postoperative morbidity,4,5 including perioperative cardiac ischaemic events,6 particularly in an increasingly elderly population with significant pre-existing co-morbid conditions.7,8 Several prospective studies have described significant postoperative morbidity that prolongs hospital stay in this population.7,9,10 These patients may be unable to undertake more objective measures of cardiorespiratory reserve, such as cardiopulmonary exercise testing11 since their primary surgical pathology limits mobility. The RCRI adds prognostic information to vascular patients identified as high risk by cardiopulmonary exercise testing.12 For the wider perioperative population, using this particular surgical subpopulation is a useful paradigm to explore whether in the absence of assessment of exercise capacity, various preoperative risk factors usefully predict prospectively recorded morbidity. We hypothesized that there would be a graded association between modified RCRI (mRCRI) score (including lower risk, relevant factors as defined by ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery),13 increased postoperative morbidity, and prolonged hospital stay after elective orthopaedic procedures.
Methods
In accordance with local Ethical Committee approval, patients presenting for elective major joint (knee and hip) replacement, including revision procedures, aged 50 yr and more were enrolled between March 2004 and April 2005 before operation at the University College London Hospital and Edinburgh Royal Infirmary.
Surgery and anaesthesia were conducted by consultant staff. Anaesthesia, standardized antibiotic prophylaxis, fluid therapy, and physiotherapy care were delivered according to usual local standard of care. Epidural anaesthesia was discontinued within 36 h to enable mobilization. Patient-controlled analgesia (morphine) was administered to patients who had undergone procedures under spinal anaesthesia. An acute pain service was available for consultation. Oral fluid and solid intake was encouraged to be resumed on postoperative day (POD) 1.
A priori, the mRCRI was calculated by weighting minor (×1) and intermediate factors (×2) as defined by the ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery (Table 1).13 We used the same definitions for renal insufficiency and ECG abnormalities (left ventricular hypertrophy, left bundle branch block, and ST-T abnormalities) described by the ACC/AHA 2007 Guidelines. We defined preoperative systemic hypertension as either systolic arterial blood pressure >160 mm Hg or diastolic arterial blood pressure >90 mm Hg or treatment for essential hypertension. We recorded prospectively the factors associated with postoperative morbidity: operative time,14 blood loss/postoperative haematocrit,15 and immediate postoperative temperature.16,17
Table 1.
Intermediate and minor cardiac risk factors
| Intermediate | History of ischaemic heart disease |
| History of compensated or prior heart failure | |
| History of cerebrovascular disease | |
| Diabetes mellitus | |
| Renal insufficiency (creatinine >177 µmol litre−1) | |
| Minor | Age >70 yr old |
| Abnormal ECG (LV hypertrophy, left bundle branch block, ST-T abnormalities) | |
| Rhythm other than sinus | |
| Uncontrolled systemic hypertension (systolic >160 mm Hg; diastolic >90 mm Hg) |
Postoperative morbidity was assessed, using a validated system10 (Table 2). Postoperative morbidity was recorded using the Postoperative Morbidity Survey (POMS). The POMS was administered by one of two study nurses to consenting patients on PODs 3, 5, 8, and 15. Day 3 POMS was not collected in the Edinburgh cohort. All data and mRCRI analyses were conducted independently of data collectors. POMS criteria were evaluated through direct patient questioning and examination, review of clinical notes and charts, retrieval of data from the hospital clinical information system, and/or consulting with the patient's caregivers. Patients were cared for by the normal attending clinicians who were blinded to the survey results. We also recorded patient age, gender, measures of preoperative risk [ASA Physical Status Score,18 and Physiologic and Operative Severity Score for the enUmeration of Mortality and Morbidity (POSSUM)],19 length of stay, mortality (at any point during hospital stay), and admission to the intensive care unit (ICU).
Table 2.
POMS-defined morbidity
| Pulmonary | Has the patient developed a new requirement for oxygen or respiratory support? |
| Infectious | Is the patient currently on antibiotics and/or has the patient had a temperature of ≥38°C in the last 24 h? |
| Renal | Does the patient have any of the following: |
| Oliguria (<500 ml day−1)? | |
| Creatinine (>30% from preop. level)? | |
| Urinary catheter in situ? | |
| Gastrointestinal | Unable to tolerate enteral diet (oral or tube feed)? |
| Is the patient experiencing nausea, vomiting, or abdominal distention? | |
| Cardiovascular | Has the patient undergone diagnostic tests or therapy within the last 24 h for any of the following: |
| New MI? | |
| Ischaemia or hypotension (requiring drug therapy or fluid therapy >200 ml h−1)? | |
| Atrial or ventricular arrhythmias? | |
| Cardiogenic pulmonary oedema/new anticoagulation (warfarin/heparin/fragmin)? | |
| Neurological | Does the patient have new confusion/delerium, focal deficit, or coma? |
| Wound complications | Has the patient experienced wound dehiscence requiring surgical exploration or drainage of pus from the op wound with/without isolation of organisms? |
| Haematological | Has the patient required any of the following within the last 24 h: rBC/platelets/FFP/cryoprecipitate? |
| Pain | Has the patient experienced surgical wound pain significant enough to require parenteral opioids or regional analgesia? |
Statistical analysis
Categorical data are summarized as absolute values (percentage). Continuous data are presented as mean (95% confidence intervals). Characteristics of patients with differing mRCRI scores were compared using the Fisher's exact test for trend, or analysis of variance, depending on the distribution and nature of the data. Statistical analyses (NCSS 2004, Kaysville, UT, USA) of time to discharge from hospital using the Kaplan–Meier survival plots (log-rank test) were used to assess the impact of mRCRI in the presence or absence of morbidity on length of stay. Multiple regression analysis was performed to assess the association of preoperative (age, ASA class, gender, and mRCRI score) and other evidence-based perioperative factors (POSSUM score, operative time, preoperative and postoperative haematocrit, and immediate postoperative temperature) with prolonged length of hospital stay (based on previous data at UCLH, with hospital stay >11 days for ≤10% patients).10 A value of P<0.05 was considered significant.
The study was powered on the basis of the results from the POMS conducted at Duke University Medical Center9 and University College London,10 with both centres consistently showing ∼40% of the patients to have one or more postoperative morbidities after similar orthopaedic procedures on POD 5. From these previous studies, our primary hypothesis was that patients with higher RCRI scores would sustain more morbidity. mRCRI scores were prospectively assigned into five classes: 0, 1, 2, 3, and ≥4. Thus, a sample size of ≥386 patients attains 90% power to detect an effect size (W) of 0.2 using a four degrees of freedom Fisher exact test with a significance level (α) of 0.05.20 The secondary outcome was length of hospital stay, analysed by the Kaplan–Meier survival plots (log-rank test).
Results
Patient population
The individual component variables for each mRCRI score >0 are shown in Table 3. Baseline characteristics for each mRCRI score (Table 4) in both centres (Edinburgh, n=130 patients; University College Hospital, n=430 patients) were similar across groups. BMI (P=0.57), previous or current smoking habit (P=0.37), and analgesic techniques did not differ (data not shown), other than the predictable age difference in groups with an mRCRI score ≥1. Twenty-one patients were admitted to ICU electively, which was associated with higher mRCRI score. Two patients died after operation (0.3%). Ninety-four per cent of the patients were anaesthetized by consultant grade staff and all cases were supervised by consultants.
Table 3.
Breakdown of mRCRI component variables for each mRCRI score >0. Numbers of patients (% of total for each mRCRI category) positive for intermediate and minor preoperative risk factors are shown
| mRCRI group |
||||
|---|---|---|---|---|
| 1 | 2 | 3 | ≥4 | |
| Intermediate | ||||
| Ischaemic heart disease | 5 (3%) | 8 (10%) | 18 (31%) | 42 (78%) |
| Congestive cardiac failure | 1 (1%) | 2 (3%) | 6 (3%) | 12 (22%) |
| Cerebrovascular event | 1 (1%) | 5 (6%) | 8 (14%) | 8 (11%) |
| Diabetes mellitus | 6 (3%) | 22 (27%) | 22 (38%) | 24 (44%) |
| Renal insufficiency | 2 (1%) | 3 (4%) | 9 (16%) | 26 (38%) |
| Minor | ||||
| Age >70 | 123 (70%) | 58 (72%) | 52 (90%) | 46 (85%) |
| ECG abnormalities | 16 (9%) | 25 (31%) | 28 (48%) | 36 (66%) |
| Non-sinus rhythm | 2 (1%) | 6 (7%) | 7 (12%) | 13 (24%) |
| Hypertension | 19 (10%) | 33 (41%) | 24 (41%) | 28 (52%) |
Table 4.
Perioperative patient characteristics according to the RCRI score. Mean (95% CI) are shown, other than for age (median, inter-quartile range) with absolute numbers (% of total) shown for each procedure type. P-values refer to differences between RCRI groups (Fisher's exact test or anova, as appropriate). * and # denote differences between RCRI groups (post hoc Tukey's test)
| mRCRI score |
P-value | |||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | ≥4 | ||
| Number | 192 | 175 | 81 | 58 | 54 | |
| Age (yr) | 62* (61–64) | 74 (73–76) | 71 (68–72) | 74 (71–77) | 75 (73–76) | <0.0001 |
| Male (%) | 35 | 38 | 45 | 38 | 45 | 0.59 |
| White cell count | 6.7 (6.4–7.1) | 7.6 (6.3–8.8) | 7.4 (6.9–8.0) | 7.7 (6.8–8.5) | 6.5 (5.8–7.3) | 0.46 |
| THR [n (%)] | 88 (37) | 73 (31) | 35 (15) | 21 (9) | 21 (8) | 0.77 |
| TKR [n (%)] | 92 (32) | 92 (32) | 41 (14) | 32 (11) | 28 (10) | |
| Revision | ||||||
| Total [n (THR):n (TKR)] | 12 (9:3) | 10 (6:4) | 5 (3:2) | 5 (3:2) | 5 (4:1) | 0.72 |
| % total operations | 6 | 6 | 6 | 9 | 9 | |
| Operative time (min) | 155 (148–162) | 143 (137–149) | 151 (139–163) | 158 (140–175) | 154 (134–174) | 0.19 |
| POSSUM | 15* (15–15) | 18 (17–18) | 17 (16–18) | 18 (17–19) | 20# (18–21) | |
| POSSUM-predicted morbidity (%) | 15.5 | 21.2 | 20.2 | 24 | 29.4 | <0.0001 |
| Elective ICU admissions (%) | 1 | 2 | 6 | 10* | 11* | 0.0003 |
| Postoperative temperature | 36.1 (36.0–36.2) | 36.1 (36.0–36.2) | 36.2 (36.0–36.3) | 36.3 (36.1–36.4) | 36.1 (35.9–36.3) | 0.4 |
| Preoperative haematocrit | 0.40 (0.39–0.41) | 0.40 (0.39–0.41) | 0.41 (0.40–0.42) | 0.39 (0.38–0.40) | 0.39 (0.37–0.42) | 0.35 |
| Postoperative haematocrit | 0.32 (0.31–0.32) | 0.31 (0.30–0.32) | 0.32 (0.30–0.33) | 0.30 (0.28–0.32) | 0.31 (0.29–0.34) | 0.53 |
RCRI score and morbidity
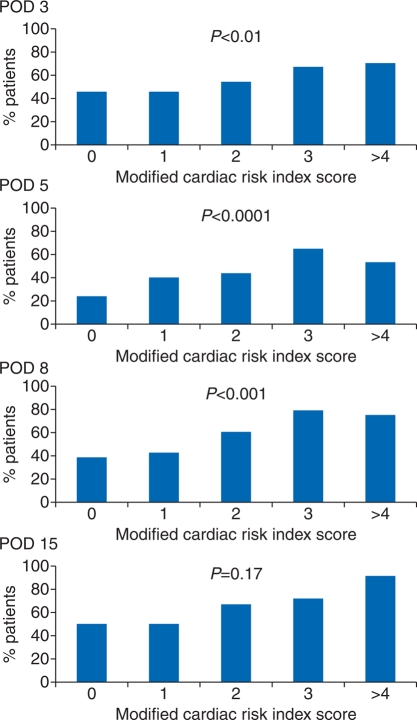
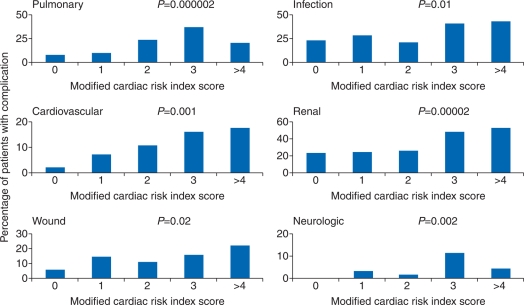
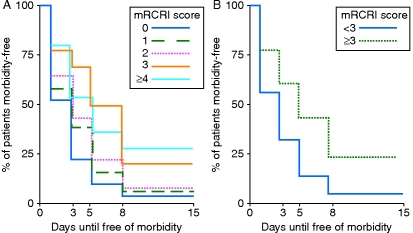
Serial total postoperative morbidity events as defined by POMS for each mRCRI score are shown in Figure 1. Postoperative morbidity occurred more frequently in patients with higher mRCRI ≥3 on POD 5 [relative risk (RR) 1.7 (95% CI: 1.4–2.1); P<0.0001]. This relationship was also maintained on POD 3 [RR 1.3 (95% CI: 1.1–1.6); P=0.01] and POD 8 [RR 1.7 (95% CI: 1.3–2.2); P=0.0002]. Pulmonary [RR 1.9 (95% CI: 1.2–3.0); P<0.0001], infectious [RR 1.5 (95% CI: 1.1–2.1); P=0.001], cardiovascular [RR 2.3 (95% CI: 1.3–4.1); P=0.0003], renal [RR 1.6 (95% CI: 1.2–2.2); P<0.0001], wound [RR 1.7 (95% CI: 1.1–2.9); P=0.04], and neurological [RR 4.1 (95% CI: 1.5–11.3); P=0.01] morbidities were more likely to be sustained by patients with RCRI score ≥3 (Fig. 2). Similar patterns were observed for both hospitals (see Supplementary material). Patients in preoperative mRCRI ≥3 groups sustained postoperative morbidity for longer (Fig. 3), becoming free of morbidity later in their postoperative course than patients with preoperative mRCRI ≤3 [log-rank test; hazards ratio (HR) 1.7 (95% CI: 1.3–2.1); P=0.01]. Both mRCRI [area under the receiver-operating characteristic curve 0.62 (95% CI: 0.57–0.67)] and POSSUM [area under the receiver-operating characteristic curve 0.64 (95% CI: 0.57–0.68)] scores demonstrated similar modest ability to predict postoperative morbid events.
Fig 1.
Preoperative mRCRI score and POMS-defined morbidity at any time point on PODs 3, 5, 8, and 15. Day 3 POMS was not collected in the Edinburgh cohort. The percentage of patients in each mRCRI group sustaining morbidity is shown. P-values refer to differences between mRCRI groups (Fisher's exact test).
Fig 2.
Individual morbidity domains recorded at any pre-defined POMS data collection time point according to the mRCRI group. Day 3 POMS was not collected in the Edinburgh cohort. Note that variable prevalence between different morbidity domains. P-values refer to differences between mRCRI groups (Fisher's exact test).
Fig 3.
Time for patients to become morbidity-free after operation according to the preoperative mRCRI category. (a) mRCRI groups ≥3 sustained longer periods of postoperative morbidity (P=0.01). (b) Time to become morbidity-free after operation according to the preoperative mRCRI score ≥3 vs <3.
mRCRI score and length of hospital stay
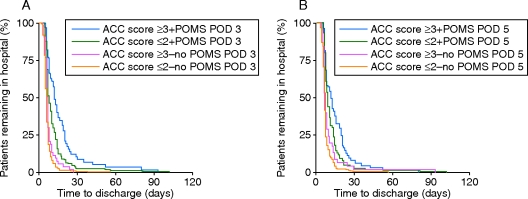
mRCRI scores ≥3 were associated with longer hospital stay (P=0.001; Fig. 4). The sum of the mRCRI score was associated with longer hospital stay, rather than specific intermediate and minor RCRI factors. The presence of intermediate risk factors alone increased the risk of morbidity on POD 5 [RR 1.2 (95% CI: 1.1–1.4); P=0.003]. Similarly, the presence of minor risk factors alone increased the risk of morbidity on POD 5 [RR 2.0 (95% CI: 1.5–2.7); P<0.0001]. Sustaining morbidity on either PODs 3 or 5 was associated strongly with prolonged length of stay. Prolonged hospital stay was more likely in patients with mRCRI ≥3 compared with those with mRCRI ≤2 who also sustained early (POD 3) morbidity [Fig. 5a; HR 1.6 (95% CI: 1.2–2.1); P<0.00001]. Similarly, for patients who sustained morbidity on POD 5, those with mRCRI ≥3 also experienced a longer hospital stay compared with those with mRCRI ≤2 [Fig. 5b; HR 1.4 (95% CI: 1.1–1.8); P=0.04]. RCRI ≥3 patients who did not sustain early morbidity (on PODs 3 and 5) were also more likely to remain in hospital for longer compared with patients with mRCRI ≤2 who also avoided POMS-defined morbidity on days 3 and 5 [HR 1.3 (95% CI: 1.03–1.7); P=0.02]. Both mRCRI [area under the receiver-operating characteristic curve 0.64 (95% CI: 0.58–0.70)] and POSSUM [area under the receiver-operating characteristic curve 0.70 (95% CI: 0.63–0.75)] scores demonstrated similar modest ability to predict prolonged length of hospital stay (defined a priori as >11 days). Multiple regression analysis identified mRCRI ≥3 as the only perioperative factor that associated with prolonged length of hospital stay (P=0.003).
Fig 4.
Length of hospital stay according to the mRCRI group. (a) Median (25th–75th percentiles) length of stay for each preoperative mRCRI score. Asterisks denote differences between mRCRI groups (P=0.03). (b) Time-to-discharge analysis showing relationship between each preoperative mRCRI score and length of hospital stay (until 30 days after operation). (c) Length of stay was persistently higher in morbidity-free patients with preoperative mRCRI ≥3. For clarity, discharge rates for mRCRI grouped into scores ≥3 or <3 are shown as for (b), for 30 days after operation (P=0.01).
Fig 5.
Time-to-discharge analyses demonstrating the impact of morbidity and mRCRI group on length of hospital stay. The presence of any POMS-defined morbidity on POD 3 (a: log-rank test, P=0.005) and POD 5 (b: log-rank test, P=0.01) was associated with prolonged hospital stay, within each mRCRI group. Length of stay was persistently higher in morbidity-free patients with mRCRI ≥3 on both PODs 3 and 5.
Discussion
These data demonstrate two major findings. First, non-cardiac morbidity is more common than cardiac morbidity, yet is associated strongly with higher preoperative cardiac risk as defined by the mRCRI. Secondly, mRCRI and POSSUM appear to be inadequate predictors of postoperative morbidity in individual patients for routine clinical practice.
Large epidemiological studies have shown that perioperative morbidity is associated with dramatic differences in post-discharge life expectancy across different operations and health systems.21 In the past, retrospective chart review has been frequently used to assess the type and frequency of complications. This approach has many methodological limitations including that the frequency and accuracy of reported complications might be inadequate for accurately assessing risk.22 POMS is the only published prospective method for describing short-term morbidity after major surgery and is a reliable and validated survey with high inter-rater reliability.10 POMS domains identify morbidity of a type and severity that could delay discharge from hospital and are recorded from indicators defining clinically important consequences rather than traditional diagnostic categories. The importance of prospectively gathering morbidity data in a defined, rigorous manner is borne out by the failure of administrative databases to satisfactorily describe postoperative complications.23,24 Our data demonstrate that in a surgical population undergoing orthopaedic operations performed by limited numbers of consultant surgical and anaesthetic teams, the RCRI is associated clearly with prospectively acquired, standardized measures of morbidity. We have also shown that morbidity is clearly associated with longer hospital stay, consistent with previous validation studies of POMS.10
In this high-volume orthopaedic population, the intrinsic limitation of patients' exercise capacity,25 plus the cost and expertise required by certain preoperative tests,11 may necessitate an alternative objective assessment of perioperative risk. A clear association was observed between pre-existing, chronic medical morbidity and the recognition by clinicians that postoperative care in a critical care environment was appropriate for many patients in the higher mRCRI groups. However, the association between higher mRCRI score, development of morbidity, and length of hospital stay persisted, regardless of immediate postoperative environment. Several other evidence-based factors that influence postoperative morbidity were similar between mRCRI groups. The high standard of anaesthetic management of these patients across mRCRI groups was demonstrated by normal postoperative temperatures and the attainment of haematocrit levels above those associated with increased risk of cardiac ischaemia.15,16 Our outcome data (hospital length of stay and in-hospital mortality) stand favourably with national4 and international5 comparisons. This includes data from recent large studies from the USA, where although the mean length of stay appears shorter, more than 48% of the patients are transferred to skilled nursing, intermediate care facilities.5 Furthermore, up to 9% US orthopaedic patients are readmitted to hospital within 3 months. After major hip or knee surgery in the US Medicare system, 10% patients were readmitted within 30 days after discharge, representing 1.5% of all surgical re-admissions.26 Failure to rehabilitate, pneumonia, postoperative infections, and gastrointestinal dysfunction (including bleeding) were among the commonest problems associated with re-admission. Thus, we observed similar patterns of morbidity reported in other hospitals and health-care systems27–30 who do not use POMS.
This is an observational, two-centre study with inherent limitations, notwithstanding that we conducted an adequately powered study that is the largest prospectively defined and collected set of morbidity data in a very specific, tightly defined surgical subpopulation. We cannot assume that all higher risk patients were appropriately treated medically before operation. Since no intervention was conducted, these data can only provide associative conclusions. Minor risk factors have not been shown to be independently associated with increased perioperative cardiac risk. Thus, the assumption that the minor risk factors are weighted appropriately requires further exploration. However, it is well recognized that abnormalities in the baseline ECG of randomly selected, asymptomatic populations are associated with subsequent all-cause mortality, including cardiovascular and coronary heart disease,31,32 independently of other risk factors.33
Clinical implications
These data provide three significant clinical implications. First, the occurrence of early morbidity on POD 3 was associated strongly with length of stay within both high- and low-risk mRCRI groups. Nevertheless, these data demonstrate that higher mRCRI is associated with more overall complications and longer hospital stay even in the absence of early postoperative morbidity. Secondly, cardiovascular morbidity—specifically, cardiac ischaemia—was a relatively infrequently recorded morbidity domain. Individual mRCRI factors, even intermediate factors such as previous myocardial infarction or heart failure, were not associated with morbidity and length of stay. Rather, the composite mRCRI score, many domains of which are not directly related to cardiovascular morbidity, conferred greater risk of postoperative morbidity. This finding is consistent with the lack of specific cardiac morbidity and an overall constellation of multiple, chronic morbidities, perhaps reflecting general deconditioning and likely lack of cardiorespiratory reserve. Thirdly, the modest predictive value of mRCRI was similar to the performance of POSSUM for predicting morbidity, suggesting that other objective measures require exploration. By definition, POSSUM cannot perform as a true preoperative predictor of morbidity since the POSSUM score can only be calculated after surgery. Objective measures of cardiopulmonary reserve including cardiopulmonary exercise testing have been reported in the orthopaedic population but are often deemed to be impractical due to the limitations imposed by musculoskeletal pain, deformity, or both. In one small study, only ∼60% of the patients with end-stage arthritis of the hip and knee were able to undertake conventional bicycle ergometry.25 Thus, stratifying risk on the basis of plasma biomarkers, such as brain natriuretic peptide,34 may confer additional predictive value.
In conclusion, greater preoperative cardiac risk is associated with an increased risk of non-cardiac morbidity and delayed discharge from hospital in elective orthopaedic surgery. Further work is required to ascertain whether perioperative interventions can be based upon the mRCRI. With increases in the prevalence of arthritis, obesity, and an ageing population, the need for measuring orthopaedic postoperative outcome/morbidity based upon appropriate risk stratification will be of great importance in driving quality health care.
Supplementary material
Supplementary material is available at British Journal of Anaesthesia online.
Conflict of interest
M.M. is National Clinical Lead for the Enhanced Recovery Partnership Programme, Department of Health.
Funding
This work was supported by an Academy Medical Sciences/Health Foundation Clinician Scientist Award to (G.L.A.), Surgical Outcomes Research Centre, Comprehensive Biomedical Research Centre, University College London Hospitals NHS Trust/University College London, and The Centre for Anaesthesia, Pain Management and Critical Care, University College London. This work was undertaken at UCLH/UCL who received a proportion of funding from the Department of Health's NIHR Biomedical Research Centre funding scheme.
Supplementary Material
Acknowledgements
SOuRCe Investigators: C. Majetowsky, M. Mutch, S. Cone, D. Levett, M. Hamilton, M. Emberton, J. Browne, J. Van Der Muelen, F. Haddad, N. Lees, N. Moran, and J.W. Scollay.
References
- 1.Lee TH, Marcantonio ER, Mangione CM, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–9. doi: 10.1161/01.cir.100.10.1043. [DOI] [PubMed] [Google Scholar]
- 2.Lindenauer PK, Fitzgerald J, Hoople N, Benjamin EM. The potential preventability of postoperative myocardial infarction: underuse of perioperative beta-adrenergic blockade. Arch Intern Med. 2004;164:762–6. doi: 10.1001/archinte.164.7.762. [DOI] [PubMed] [Google Scholar]
- 3.Lindenauer PK, Pekow P, Wang K, Mamidi DK, Gutierrez B, Benjamin EM. Perioperative beta-blocker therapy and mortality after major noncardiac surgery. N Engl J Med. 2005;353:349–61. doi: 10.1056/NEJMoa041895. [DOI] [PubMed] [Google Scholar]
- 4.Smith ID, Elton R, Ballantyne JA, Brenkel IJ. Pre-operative predictors of the length of hospital stay in total knee replacement. J Bone Joint Surg Br. 2008;90:1435–40. doi: 10.1302/0301-620X.90B11.20687. [DOI] [PubMed] [Google Scholar]
- 5.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007;89:526–33. doi: 10.2106/JBJS.F.00952. [DOI] [PubMed] [Google Scholar]
- 6.Jules-Elysee K, Urban MK, Urquhart B, Milman S. Troponin I as a diagnostic marker of a perioperative myocardial infarction in the orthopedic population. J Clin Anesth. 2001;13:556–60. doi: 10.1016/s0952-8180(01)00337-3. [DOI] [PubMed] [Google Scholar]
- 7.Ackland GL, Scollay JM, Parks RW, de B I, Mythen MG. Pre-operative high sensitivity C-reactive protein and postoperative outcome in patients undergoing elective orthopaedic surgery. Anaesthesia. 2007;62:888–94. doi: 10.1111/j.1365-2044.2007.05176.x. [DOI] [PubMed] [Google Scholar]
- 8.Peled E, Keren Y, Halachmi S, et al. Patients aged 80 and older undergoing orthopedic or urologic surgery: a prospective study focusing on perioperative morbidity and mortality. Gerontology. 2009;55:517–22. doi: 10.1159/000235617. [DOI] [PubMed] [Google Scholar]
- 9.Bennett-Guerrero E, Welsby I, Dunn TJ, et al. The use of a postoperative morbidity survey to evaluate patients with prolonged hospitalization after routine, moderate-risk, elective surgery. Anesth Analg. 1999;89:514–9. doi: 10.1097/00000539-199908000-00050. [DOI] [PubMed] [Google Scholar]
- 10.Grocott MP, Browne JP, Van der MJ, et al. The Postoperative Morbidity Survey was validated and used to describe morbidity after major surgery. J Clin Epidemiol. 2007;60:919–28. doi: 10.1016/j.jclinepi.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Older P, Hall A, Hader R. Cardiopulmonary exercise testing as a screening test for perioperative management of major surgery in the elderly. Chest. 1999;116:355–62. doi: 10.1378/chest.116.2.355. [DOI] [PubMed] [Google Scholar]
- 12.Carlisle J, Swart M. Mid-term survival after abdominal aortic aneurysm surgery predicted by cardiopulmonary exercise testing. Br J Surg. 2007;94:966–9. doi: 10.1002/bjs.5734. [DOI] [PubMed] [Google Scholar]
- 13.Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. J Am Coll Cardiol. 2007;50:1707–32. doi: 10.1016/j.jacc.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Bennett-Guerrero E, Panah MH, Barclay GR, et al. Decreased endotoxin immunity is associated with greater mortality and/or prolonged hospitalization after surgery. Anesthesiology. 2001;94:992–8. doi: 10.1097/00000542-200106000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Hogue CW, Jr, Goodnough LT, Monk TG. Perioperative myocardial ischemic episodes are related to hematocrit level in patients undergoing radical prostatectomy. Transfusion. 1998;38:924–31. doi: 10.1046/j.1537-2995.1998.381098440856.x. [DOI] [PubMed] [Google Scholar]
- 16.Frank SM, Fleisher LA, Breslow MJ, et al. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. J Am Med Assoc. 1997;277:1127–34. [PubMed] [Google Scholar]
- 17.Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334:1209–15. doi: 10.1056/NEJM199605093341901. [DOI] [PubMed] [Google Scholar]
- 18.American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24:111. [Google Scholar]
- 19.Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991;78:355–60. doi: 10.1002/bjs.1800780327. [DOI] [PubMed] [Google Scholar]
- 20.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 21.Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:326–41. doi: 10.1097/01.sla.0000179621.33268.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Story DA, Fink M, Leslie K, et al. Perioperative mortality risk score using pre- and postoperative risk factors in older patients. Anaesth Intensive Care. 2009;37:392–8. doi: 10.1177/0310057X0903700310. [DOI] [PubMed] [Google Scholar]
- 23.Romano PS, Chan BK, Schembri ME, Rainwater JA. Can administrative data be used to compare postoperative complication rates across hospitals? Med Care. 2002;40:856–67. doi: 10.1097/00005650-200210000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Romano PS, Schembri ME, Rainwater JA. Can administrative data be used to ascertain clinically significant postoperative complications? Am J Med Qual. 2002;17:145–54. doi: 10.1177/106286060201700404. [DOI] [PubMed] [Google Scholar]
- 25.Philbin EF, Ries MD, French TS. Feasibility of maximal cardiopulmonary exercise testing in patients with end-stage arthritis of the hip and knee prior to total joint arthroplasty. Chest. 1995;108:174–81. doi: 10.1378/chest.108.1.174. [DOI] [PubMed] [Google Scholar]
- 26.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 27.Hamel MB, Henderson WG, Khuri SF, Daley J. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc. 2005;53:424–9. doi: 10.1111/j.1532-5415.2005.53159.x. [DOI] [PubMed] [Google Scholar]
- 28.Hamel MB, Toth M, Legedza A, Rosen MP. Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee: decision making, postoperative recovery, and clinical outcomes. Arch Intern Med. 2008;168:1430–40. doi: 10.1001/archinte.168.13.1430. [DOI] [PubMed] [Google Scholar]
- 29.McNicol L, Story DA, Leslie K, et al. Postoperative complications and mortality in older patients having non-cardiac surgery at three Melbourne teaching hospitals. Med J Aust. 2007;186:447–52. doi: 10.5694/j.1326-5377.2007.tb00994.x. [DOI] [PubMed] [Google Scholar]
- 30.Liu LL, Leung JM. Predicting adverse postoperative outcomes in patients aged 80 years or older. J Am Geriatr Soc. 2000;48:405–12. doi: 10.1111/j.1532-5415.2000.tb04698.x. [DOI] [PubMed] [Google Scholar]
- 31.De BD, De BG, Kornitzer M, Blackburn H. Prognostic value of ECG findings for total, cardiovascular disease, and coronary heart disease death in men and women. Heart. 1998;80:570–7. doi: 10.1136/hrt.80.6.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Daviglus ML, Liao Y, Greenland P, et al. Association of nonspecific minor ST-T abnormalities with cardiovascular mortality: the Chicago Western Electric Study. J Am Med Assoc. 1999;281:530–6. doi: 10.1001/jama.281.6.530. [DOI] [PubMed] [Google Scholar]
- 33.Kumar A, Lloyd-Jones DM. Clinical significance of minor nonspecific ST-segment and T-wave abnormalities in asymptomatic subjects: a systematic review. Cardiol Rev. 2007;15:133–42. doi: 10.1097/01.crd.0000249382.65955.14. [DOI] [PubMed] [Google Scholar]
- 34.Ryding AD, Kumar S, Worthington AM, Burgess D. Prognostic value of brain natriuretic peptide in noncardiac surgery: a meta-analysis. Anesthesiology. 2009;111:311–9. doi: 10.1097/ALN.0b013e3181aaeb11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.