Abstract
Background
Many of the individuals most at risk for HIV infection are also the most marginalized by our health care system. Lacking primary care providers, they rely on the Emergency Department for their health care needs and education. In this study, we evaluated the educational effectiveness of a brief post-test counseling video.
Methods
Stable patients presenting to the walk-in section of an urban ED were recruited for rapid HIV testing. Eligible patients were those who consented for the rapid HIV test and completed measures on condom intention and condom use self-efficacy. Before receiving their results, participants were randomized to either a fifteen-minute post-test educational video or to a post test educational session with an HIV counselor. Afterwards, both groups completed an assessment tool concerning HIV prevention and transmission.
Results
Of the 128 participants, 61 and 67 patients were randomized to the video and counselor groups, respectively. Mean knowledge scores were higher in the video group (76.20% vs 69.3%; 90% CI for the difference, 2.8, 11.2). As the lower bound of the CI for the difference was higher than the lower equivalence boundary (−5%), we infer that the video was at least as effective as the counselor educational session.
Conclusions
The use of an educational counseling video is a valid alternative for providing post–test education and prevention information during the waiting period associated with the 20-minute HIV rapid test. Without disruption in clinical flow, both testing and education can be accomplished in a meaningful way in a busy ED.
INTRODUCTION
Background
As of 2003, more than one million people in the United States are living with HIV/AIDS, with up to one-third unaware of their status. 1–6 The Centers for Disease Control and Prevention (CDC) supports an initiative to decrease the number of patients who are unaware of their HIV status. New CDC recommendations suggest that voluntary HIV testing should become a routine part of medical care, and non-traditional sites such as Emergency Departments (EDs), should provide access to HIV counseling and testing (C&T).4–6 The updated recommendations no longer require prevention counseling as part of HIV screening, especially if de-linking the two helps healthcare professionals achieve the primary goal of an increase in testing.7 Yet the CDC has recognized that patients might be more receptive to hear about HIV and to consider their risks at the time of testing, thus it is an opportune time to provide prevention messages.7 Inner-city EDs serve disadvantaged patient populations that have limited or no access to health care, and that often utilize the ED for their primary care. If testing were no longer linked to prevention counseling in EDs, high risk patients might not have any other means of obtaining HIV education and prevention information. Clearly the ideal is to identify a cost-effective strategy to provide prevention counseling at the time of testing, especially in settings that reach vulnerable, at-risk populations.
Importance
Rapid HIV testing provides expanded opportunities to identify and link HIV-infected individuals to care. The 20-minute waiting period for test results represents a convenient interval in which one can provide patients with HIV-prevention education. Attempts to respond to the CDC initiatives to provide rapid HIV C&T to more patients in EDs present many challenges. In particular, HIV C&T is time-consuming and stresses the already limited resources of those working in the ED. An imposing barrier to the provision of HIV-prevention education is the lack of time ED health care providers have for such efforts. If this information could be disseminated effectively using educational videos, it might be a practical solution to help deflect the cost of an increase in manpower that would otherwise accompany the increase in HIV testing.
The value of video education is that it can be available to patients in their chosen language, and can be repeated endlessly in a standardized manner for however many patients require the information. It provides consistent delivery of instruction and a favorable learning environment. Video education is confidential and gives patients the opportunity to learn communication and refusal skills with little or no embarrassment.8 This is especially important when the prevention messages focus on sexual behavior.9 Additionally, studies have demonstrated that patients have a better retention of information presented in video format than other methods of delivery.10–12
The practitioners in most EDs are busy seeing acutely ill patients. Even when time is available, they have trouble finding the best method to convey education and prevention messages, especially to patients with low literacy.13 Video counseling addresses this issue, because it is accessible to people with a wide range of reading skills.14 Moreover, in terms of HIV prevention for at-risk men, video-based, one-session interventions have proven to be cost-saving, in terms of averted medical costs. 15
Goals of This Investigation
The purpose of this study was to develop an educational video on HIV prevention and to test its effectiveness as compared to an in-person counseling session with trained HIV counselors, among ambulatory patients recruited for rapid HIV testing in the ED.
METHODS
Study Design
The study was a non-blinded randomized trial with two arms. Both groups viewed a previously studied pre-test counseling video which contained all the elements required by New York State law to be discussed in pre-test counseling. It included information on HIV transmission, definition of AIDS and HIV infection, the nature and meaning of the HIV test, benefits of testing, reporting, partner notification and the definition of voluntary and mandatory testing. After the patients viewed this video, the research assistants administered the rapid HIV test. The control group received standard HIV post-test, in-person counseling while waiting for rapid HIV test results. The intervention group viewed an HIV prevention video in either English or Spanish. After completing an evaluation survey of the video, the intervention group received standard HIV post-test, in-person counseling. Both groups received their rapid HIV test result after their post-test counseling session. If the result was negative, further counseling was available if the patient had more questions or if he/she was at a high-risk for contracting the virus. Patients who tested positive were informed of their results by a provider and walked to the HIV clinic in the hospital by the research assistant. The research protocol was approved by the institutional review boards (IRB) at the Albert Einstein College of Medicine and the Health and Hospitals Corporation.
Setting
A convenience sample of stable patients recruited in the Jacobi Medical Center Urgent Care Area (UCA), a walk-in section of the adult ED. Jacobi Medical Center is an inner-city hospital, level I trauma and tertiary care center, located in the Bronx, New York. Emergency Medicine physicians staff the UCA Monday through Friday from 8am to 4pm. All patients seen in the UCA are ambulatory and non-acute.
Selection of Participants
Eligible patients for enrollment in this study were those 18 years of age and older visiting the UCA for any reason, between July 5, 2005 and October 5, 2005. This was a non-targeted HIV testing approach, all patients who did not fit exclusion criteria were recruited for the study. Everyone who participated received point-of-care testing. Patients were ineligible for the study if they were clinically unstable, had a previously confirmed diagnosis of HIV, tested for HIV within the past six-months or were unable to understand the consent process.
Intervention
We developed a fifteen-minute rapid HIV post-test video that focused on the use of condoms as a positive behavior. The video demonstrated how to properly use male and female condoms and dental dams. Additional information in the video included interpretation of HIV test results, partner notification and domestic violence information. The education and prevention messages in the video were conveyed by one of the co-authors. The video was explicitly designed to include information that conveyed the essential elements that are required to be discussed within the post-test counseling session, as per New York State law. The video was appropriate for an eighth grade language level and was also translated into Spanish.
Data Collection and Processing
Two research assistants in the UCA used a standardized scripted approach to describe the study to potential participants. Written informed consent was obtained in either English or Spanish. Individuals who declined to participate were verbally consented to obtain reasons for their refusal. All eligible participants who agreed to participate in the study were randomized to either the control group or the intervention group. A randomization scheme was generated using a computer-generated block randomization, (available online at www.randomization.com). Randomization assignments were placed in sealed opaque envelopes that were sequentially opened by the research assistants after the patient signed the informed consent.
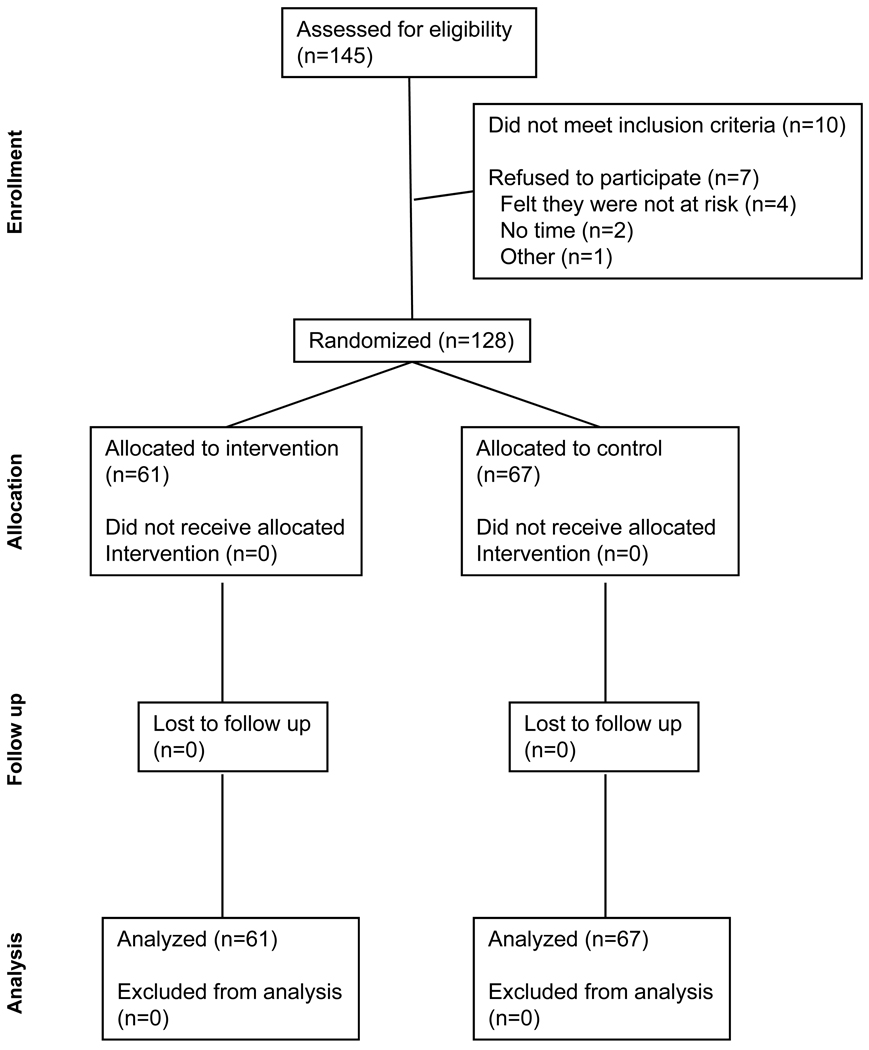
After consenting, participants first responded to a demographic survey, a risk assessment survey, a self-efficacy measure and a condom intention measure. All participants then received pre-test counseling by viewing the same 6-minute pre-HIV test video. It contained all the elements required by New York State law to be discussed in pre-test counseling (as stated in the study design section). Post-test HIV counseling is required by New York State law and followed the viewing of the HIV prevention video. The control group received standard HIV post-test, in-person counseling, while waiting for their HIV test results. The intervention group viewed the HIV prevention video and then received standard HIV post-test, in-person counseling while waiting for HIV test results. The post-test video included a demonstration of how to properly use condoms, and information on interpretation of HIV test results, partner notification and domestic violence. Since the HIV-prevention video was an untested method of conveying information, standard HIV post-test counseling was also given, to provide the standard of care to patients randomized to the intervention arm of the study. (See figure 1)
Figure 1.
Profile of randomized control trial
All participants were administered a ten-question true-false measure of retained information. Measures were administered in either English or Spanish. Those in the control group took the true-false knowledge measure after receiving post-test counseling. Those in the intervention group viewed the HIV prevention video, took the same ten-question measure of retained information, and then had a standard counseling session after the measure was completed.
Outcome Measures
The primary outcome for the study was the participant’s score on the ten-question measure. To create this measure, questions were adapted from the New York State Department of Health HIV Questions & Answers Booklet and modified to true-false responses at a fifth-grade reading level, as determined by Microsoft Word’s Flesh-Kincade grade level instrument (Microsoft Corp, Redmond, WA). The measure was circulated among the co-investigators, including HIV and Infectious Disease specialists, for consensus. The measure was initially created in English, and then translated into Spanish (see appendix A). The primary outcome measure, the number of correct answers on the ten-question measure, formed a score that ranged from 0% to 100% correct.
Statistical Analysis
Equivalence methods were used in order to evaluate whether the video was at least as good as the counselor in conveying knowledge about HIV prevention. The null hypothesis for the equivalence method is that the mean score on the true-false measure assessing retained knowledge of HIV post-test counseling in the intervention group is lower than the mean in the counseling group. The alternative hypothesis is that the mean score of the intervention is at least as high as the mean exam score of the counseling group. The groups would be considered equivalent if the mean score on the measure in the intervention group was no more than 5% lower than the mean score of those who saw the counselor. We calculated the 90% equivalence confidence interval (CI) and the corresponding one-tailed test around the difference in exam scores.
Sample size calculation, determined a priori, required 59 patients in each group for a power of 85%, equivalence limit of −5% and an alpha of 0.05. nQuery Advisor release 3.0 (Cork, Ireland, 1999) was used to calculate the sample size. Baseline characteristics of the intervention and control groups, as well as incidence of HIV positive patients, were compared using Student’s t-test for continuous variables and chi-square tests for categorical variables. All statistical analyses were performed using Stata SE 9.2 (StataCorp, College Station, TX). For all analyses, p-values are 2-tailed with an alpha of 0.05 considered for statistical significance. EquivTest 1.0 (Cork, Ireland, 1998) was used to assess equivalence.17
RESULTS
Figure 1 summarizes enrollment and patient flow. A total of 145 patients were approached for recruitment in this study. Of the 145, 7 refused to participate, 10 were ineligible and 128 (88.3%) agreed to participate. The most common reason for non-eligibility was having been recently tested for HIV (n=7). The reasons why most eligible patients refused were “I feel I am not at risk” (n=4) and “I have no time” (n=2). (See figure 1)
The patients who were randomized to either group were similar with regards to age, gender, preferred language and prior HIV C&T (table 1).
Table 1.
Characteristics of the cohort randomized to each group*
| Characteristic | Intervention n=61 |
Control n=67 |
Total n=128 |
p-value |
|---|---|---|---|---|
| Sex (male) | 65.6 (40) | 58.2 (39) | 61.6 (79) | 0.39 |
| Marital -Single | 81.4 (48) | 75.0 (45) | 78.2 (93) | 0.40 |
| Age (years) | 29.2 ± 8.2 | 31.4 ± 10.3 | 30.4 ± 9.4 | 0.20 |
| Hispanic (yes) | 46.15 (24) | 59.32 (35) | 46.9 (52) | 0.17 |
| Preferred Language | 0.69 | |||
| English | 88.5 (54) | 83.6 (56) | 85.9 (110) | |
| Spanish | 9.8 (6) | 14.9 (10) | 12.5 (16) | |
| French | 1.6 (1) | 1.5 (1) | 1.6 (2) | |
| Tested for HIV before (yes) | 74.1 (43) | 69.7 (46) | 71.8 (89) | 0.58 |
| Return For Results (yes) | 71.19 (42) | 69.4 (43) | 70.3 (85) | 0.83 |
| Prior HIV Counseling (yes) | 60.7 (37) | 55.2 (37) | 57.8 (74) | 0.53 |
Continuous variables presented as mean ± sd with p-value calculated by student’s t-test. Categorical variables presented as percent (n) with p-value calculated by chi-square. Percentages may not total to 100 due to rounding.
Mean knowledge scores were higher in the intervention than in the control group (76.2 ± 14.0% vs. 69.3 ± 14.5%). The difference between the group means on the HIV test was thus 6.98 ± 2.5% with a 90% CI of 2.8, 11.2. The lower end of the CI, 2.8 was higher than the equivalence limit, −5.
LIMITATIONS
There are several limitations to this study. Generalizability of the methods may not hold for all health care sites nationally due to a difference in state laws regarding HIV testing, counseling and consent. Also, the study participants were all non-acute, ambulatory, urgent care patients and this may account for the high participation rate, as compared to an ED population. Next, the measure used to determine knowledge retention was not a formally validated research tool. The essential domains of information that were important to cover were consistent with what the NYSDOH considered to be basic HIV/AIDS facts and required within the post-test counseling sessions. Lastly, the counselors were not blinded to the study protocol. However, the counselors were not allowed to see the video or know its content. All counselors received standard training according to NYS DOH and CDC guidelines. Therefore, the assumption is that all patients are given the same necessary material within their post-test counseling session. Not blinding the counselors could conceivably alter their performance within the sessions to influence the results of the study.
DISCUSSION
The advent of rapid HIV testing increases the likelihood that HIV testing in the Emergency Department (ED) setting will become a widespread practice. The availability of the rapid test has eliminated an obstacle to HIV testing in the ED: follow–up for giving patients their results. Rather than waiting days or weeks to give the result from a blood sample to the patient, results are now possible within 20 minutes. In addition to the positive impact of knowing one’s status, early detection and treatment of HIV infection can reduce the risk of transmission to others while improving one’s quality of life and prolonging its duration.2, 3, 18 The ED sees a significant percentage of patients who are unaware that they are HIV positive; since many do not receive care from a primary care physician it can be argued that the ED visit is an opportunity to test patients that should not be wasted. We have shown that the time burden of pre-test counseling can be eliminated with the use of a pre-test counseling video.16 Yet several barriers remain, one of which is providing appropriate education to patient’s who desire testing. Providing education about the implications of the test, as well as valuable HIV prevention information, can be an incredibly daunting task when multiplied by the numbers of patients seen during a busy ED shift. We now seek to provide a mechanism with which to deliver needed HIV prevention information to our vulnerable patient population without taking the time of busy ED providers. HIV counselors are currently available in our institution during daytime weekday hours. Providing EDs with HIV testing capability, especially during the off hour shifts, would be a valuable service. However, it would be a burden for the practitioner to counsel each patient about the meaning of the test as well as provide the motivation for the patient to consider altering their behaviors in a way that might decrease their risk. Though face-to-face counseling may be preferable, it is not always a viable option in emergent care settings, underscoring the need for another method of providing education and prevention messages.
CONCLUSION
The use of an educational post-test counseling video is a valid alternative for providing post–test counseling education and prevention information during the 20 minute period that a patient must wait for his or her rapid test result. Utilizing video counseling as well as the rapid test allows EDs to achieve the goal of routine HIV testing without sacrificing the opportunity to provide education and prevention messages.
FUTURE DIRECTIONS
We have demonstrated that high quality HIV risk reduction education and HIV testing need not be mutually exclusive. In our facility, we are pursuing a fully-fledged HIV counseling/testing program that incorporates the elements of the model proposed here with high volume HIV testing and complete linkage to HIV specialty care for those who are diagnosed as HIV-infected. Of equal importance to ED patients who test HIV-negative will be the linkage to ongoing protracted behavior modification outpatient services to reduce their risk of HIV infection.
Appendix A
Latex condoms reduce the risk for HIV transmission? (circle) True False
Lambskin condoms protect against HIV transmission? (circle) True False
-
Most people who are at high risk for HIV should be tested every 3 months?
(circle) True False
-
You are legally required to give your doctor information on all your partners?
(circle) True False
Any information you give your doctor about your partner(s) will be forwarded to the Department of Health if you are HIV positive? (circle) True False
-
If you were recently infected with HIV, your test may still be negative?
(circle) True False
A woman who is HIV+ and pregnant is not at risk of transmitting the disease to her unborn child? (circle) True False
-
Female condoms are helpful in protecting against HIV transmission?
(circle) True False
-
Oil based lubricants make latex condoms less protective in preventing HIV?
(circle) True False
Using male and female condoms together make them more effective in preventing HIV? (circle) True False
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Yvette Calderon, Jacobi Medical Center/Albert Einstein College of Medicine.
Jason Leider, Jacobi Medical Center/Albert Einstein College of Medicine.
Susan Hailpern, Albert Einstein College of Medicine.
Marianne Haughey, Jacobi Medical Center/Albert Einstein College of Medicine.
Reena Ghosh, Jacobi Medical Center/Albert Einstein College of Medicine.
Pamela Lombardi, Jacobi Medical Center/Albert Einstein College of Medicine.
Polly Bijur, Albert Einstein College of Medicine.
Laurie Bauman, Albert Einstein College of Medicine.
REFERENCES
- 1.Glynn M, Rhodes P. Estimated HIV Prevalence at the End of 2003. National HIV Prevention Conference; Atlanta, GA: 2005. Jun, Vol Abstract 595. [Google Scholar]
- 2.National HIV Testing Day at CDC-funded HIV counseling, testing, and referral sites--United States, 1994–1998. MMWR Morb Mortal Wkly Rep. 2000 Jun 23;49(24):529–532. [PubMed] [Google Scholar]
- 3.CDC posts new HIV testing, referral guidelines. AIDS Alert. 2002 Jan;17(1):8–10. 12. [PubMed] [Google Scholar]
- 4.Revised guidelines for HIV counseling, testing, and referral. MMWR Recomm Rep. 2001 Nov 9;50(RR-19):1–57. quiz CE51-19a51-CE56-19a51. [PubMed] [Google Scholar]
- 5.Rothman RE, Ketlogetswe KS, Dolan T, et al. Preventive care in the emergency department: should emergency departments conduct routine HIV screening? a systematic review. Acad Emerg Med. 2003 Mar;10(3):278–285. doi: 10.1111/j.1553-2712.2003.tb02004.x. [DOI] [PubMed] [Google Scholar]
- 6.Rothman RE. Current Centers for Disease Control and Prevention guidelines for HIV counseling, testing, and referral: critical role of and a call to action for emergency physicians. Ann Emerg Med. 2004 Jul;44(1):31–42. doi: 10.1016/j.annemergmed.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006 Sep 22;55(RR-14):1–17. quiz CE11-14. [PubMed] [Google Scholar]
- 8.Evans AE, Edmundson-Drane EW, Harris KK. Computer-assisted instruction: an effective instructional method for HIV prevention education? J Adolesc Health. 2000 Apr;26(4):244–251. doi: 10.1016/s1054-139x(99)00093-2. [DOI] [PubMed] [Google Scholar]
- 9.Kiene SM, Barta WD. A brief individualized computer-delivered sexual risk reduction intervention increases HIV/AIDS preventive behavior. J Adolesc Health. 2006 Sep;39(3):404–410. doi: 10.1016/j.jadohealth.2005.12.029. [DOI] [PubMed] [Google Scholar]
- 10.Reznik M, Sharif I, Ozuah PO. Use of interactive videoconferencing to deliver asthma education to inner-city immigrants. J Telemed Telecare. 2004;10(2):118–120. doi: 10.1258/135763304773391585. [DOI] [PubMed] [Google Scholar]
- 11.Weston J, Hannah M, Downes J. Evaluating the benefits of a patient information video during the informed consent process. Patient Educ Couns. 1997 Mar;30(3):239–245. doi: 10.1016/s0738-3991(96)00968-8. [DOI] [PubMed] [Google Scholar]
- 12.Fureman I, Meyers K, McLellan AT, et al. Evaluation of a video-supplement to informed consent: injection drug users and preventive HIV vaccine efficacy trials. AIDS Educ Prev. 1997 Aug;9(4):330–341. [PubMed] [Google Scholar]
- 13.Brock TP, Smith SR. Using digital videos displayed on personal digital assistants (PDAs) to enhance patient education in clinical settings. Int J Med Inform. 2006 Nov 16; doi: 10.1016/j.ijmedinf.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 14.Weinhardt LS, Mosack KE, Swain GR. Development of a Computer-based Risk-reduction Counseling Intervention: Acceptability and Preferences Among Low-income Patients at an Urban Sexually Transmitted Infection Clinic. AIDS Behav. 2006 Sep 22; doi: 10.1007/s10461-006-9163-x. [DOI] [PubMed] [Google Scholar]
- 15.Pinkerton SD, Johnson-Masotti AP, Holtgrave DR, et al. Using cost-effectiveness league tables to compare interventions to prevent sexual transmission of HIV. Aids. 2001 May 4;15(7):917–928. doi: 10.1097/00002030-200105040-00012. [DOI] [PubMed] [Google Scholar]
- 16.Calderon Y, Haughey M, Bijur PE, et al. An educational HIV pretest counseling video program for off-hours testing in the emergency department. Ann Emerg Med. 2006 Jul;48(1):21–27. doi: 10.1016/j.annemergmed.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Calderon Y, Haughey M, Gennis P, et al. In reply. Annals of Emergency Medicine. 2007;49(3):380–381. [Google Scholar]
- 18.Chow S, Liu J. Design and Analysis of Bioavailability and Bioequivalence Studies. New York, NY: Marcel Dekker Inc.; 1992. [Google Scholar]
- 19.Advancing HIV prevention: new strategies for a changing epidemic-United States, 2003. MMWR Morb Mortal Wkly Rep. 2003 Apr 18;52(15):329–332. [PubMed] [Google Scholar]