Abstract
Study Objectives:
The study provided an opportunity to observe sleep patterns in a college-age population attending the United States Military Academy.
Design:
This 4-year longitudinal study investigated sleep patterns of cadets. A stratified sample of 80 cadets had sleep patterns monitored using actigraphy for 8 months: one month in both fall and spring academic semesters over a 4-year period.
Setting:
Data were collected at the United States Military Academy, West Point, NY.
Participants:
Participants were members of the class of 2007 (n˜1300) ranging in age from 17 to 22 when entering USMA.
Measurements and Results:
A sample of the class (n = 80) wore wrist activity monitors and completed activity logs for one month in fall and spring academic semesters for the 4-year period. On average over the 4 years, cadets slept < 5.5 h on school nights. Cadets napped extensively, perhaps in an attempt to compensate for chronic sleep debt. Cadets slept more during fall than spring semesters. Male and female cadet sleep patterns varied dramatically, with males consistently receiving less sleep than females (˜21 m for nighttime sleep and ˜23 m for daily sleep).
Conclusions:
Cadet sleep at USMA is related to academic year, semester, season, sex, school day or weekend, and day of the week. These students suffer from chronic sleep debt. Restrictions imposed by the military academy limit the generalizability of the findings to other college age populations.
Citation:
Miller NL; Shattuck LG; Matsangas P. Longitudinal study of sleep patterns of United States Military Academy cadets. SLEEP 2010;33(12):1623-1631.
Keywords: Sleep deprivation, actigraphy, adolescent sleep patterns, college-age students, military education
RESEARCHERS HAVE REPORTED THE DISTINCT CHANGES THAT OCCUR IN SLEEP PATTERNS WHEN HUMANS ENTER ADOLESCENCE.1–4 These changes are marked by both a delay in and an extension of the major sleep period. When allowed to conform to individual sleep preference, individuals in this age group experience later bedtimes and awaken much later, a pattern that corresponds to the naturally occurring melatonin levels of this age group.5,6 While this change in sleep pattern coincides with pubertal onset in the teen years, Roenneberg et al. reported that this tendency to sleep late may continue throughout the lifespan.7 Their model of the timing of self-selected sleep identified 3 important determinants: genetic disposition, sleep debt accumulated on workdays, and light exposure. The study also identified significant differences between the amount of sleep for males and females (females had 17 m more sleep on weekdays), although sleep amount in the 2 groups was not significantly different on free days. Individual sleep requirements also vary considerably8,9 and have been attributed to differences in human physiology.10,11 Even though adults need on average approximately 7.5 to 8 h of daily sleep, both ends of this distribution exist with short sleepers (≤ 6.5 h of sleep) and long sleepers (≥ 8.5 h of sleep).10–13
Numerous studies indicate that sleep is often a problem for college-age students, with mounting evidence that this age group commonly suffers from disordered sleep patterns that often result in chronic sleep debt.14–18 This trend may be worsening, perhaps due in part to the 24-7 nature of life in the twenty-first century,19,20 which is marked by advances in technology that surround the individual with connectedness.21,22 With the omnipresence of the internet, laptop computers, and caffeine dispensaries, modern society differs dramatically from that of just a few decades ago. Today, there is little down time when individuals are forced to “tune out” and disconnect from technology.
This trend is especially alarming in light of a growing body of literature highlighting the association between chronic sleep debt and insomnia and a variety of physical and mental health issues.23–25 Additional evidence points to the role of sleep in maintaining the body's ability to ward off infections through the immune system.26 Along with the negative health consequences of sleep deprivation, its effect on individual cognitive performance has been documented in multiple studies.27–29 Memory consolidation, long-term recall, and retrieval, particularly of novel material, is affected by sleep restriction.30–32 Mishaps and safety violations are closely associated with inadequate sleep.33
Sleep deprivation is not uncommon in military life, especially during exercises, demanding training periods, and combat.34,35 For this reason, Army regulations address sleep related issues as part of combat/operational stress and battle fatigue (a military term for combat stress symptoms and reactions).36 Historically, many members of the military view sleep as an indulgence; sleep deprivation in the interest of duty is even revered.37 In military training and eduction settings, the schedule of activities is both rigorous and strictly enforced. Combined with extremely limited opportunities for sleep, the typical schedule often results in cumulative sleep debt and involuntary forced circadian desynchrony.18 Grades and other performance measures suffer when adolescents and young adults experience restricted sleep schedules. This finding was confirmed in a study of test scores of US Navy Recruits at Great Lakes, Illinois.38 In another study of military members, Killgore et al. found significant correlations between sleep and test scores in military students attending the Noncommissioned Officer and Warrant Officer Candidate Schools at Fort Rucker, AL.39 These studies point to a strong relationship between sleep and academic performance and are aligned with findings of controlled laboratory studies.
We do not completely understand the natural history of sleep in an individual. Few, if any, longitudinal studies observe sleep patterns over the course of an individual's life span. This study seeks to fill a portion of this gap by studying sleep patterns over a 4-year period in late adolescence and young adulthood. The conditions at USMA provide a natural laboratory to examine restricted sleep patterns in adolescents and young adults. The present study has 2 goals: (1) determine the key factors associated with Cadet sleep patterns at USMA; (2) evaluate whether and to what extent Cadets attending USMA, who are military and college-age students, are chronically sleep deprived.
Typical USMA Cadet Schedule
Over the course of a week, the schedules of cadets attending USMA fall into 2 distinct categories: school days (Monday through Friday), and weekends (Saturday and Sunday). On school days, USMA cadets follow a fairly rigid daily schedule. The Academy's senior leadership modifies the daily schedule from time to time based on feedback from the faculty, staff, and cadets. During this study, cadets arose no later than 06:30 (reveille) in order to attend a mandatory morning formation at 06:55. A mandatory “midnight lights out” policy was put in place at the beginning of the second year of the study. However, the researchers were aware of both authorized and unauthorized deviations from these policies. For example, cadets were authorized to leave their rooms no earlier than 05:15 to participate in individual or team athletic training prior to the morning formation. Several cadets reported staying up past the midnight “lights out” in order to complete their homework or their military duties. Therefore, even though the schedule afforded 6.5 h of protected sleep time, in practice, many cadets received much less sleep, either because they woke up prior to 06:30, went to sleep past midnight, or both. Table 1 shows a typical USMA cadet school day schedule.
Table 1.
Typical school day schedule at USMA
| 06:30 | Reveille |
| 06:55–7:30 | Breakfast Formation (mandatory) |
| 07:35–11:45 | Class (55 minutes per class) or study time |
| 12:05–12:40 | Lunch |
| 12:45–13:40 | Commandant/Dean Time |
| 13:50–15:50 | Class or study |
| 16:10:17:45 | Intramural, club or intercollegiate athletics; parades; extracurricular activities; or free time |
| 18:30–19:15 | Supper (optional except Thursdays) |
| 19:15–19:30 | Cadet Duties |
| 19:30–20:30 | Study conditions/Extracurricular activities |
| 20:30–23:30 | Study time |
| 23:30 | Taps |
| 24:00 | Lights Out |
The mandatory midnight lights out policy was instituted at the beginning of fall 2004 and continued through spring 2007. Saturday and Sunday mornings provided the only opportunities for cadets to sleep late. Weekends also represent the major opportunity for cadets to engage in social activities. All cadets participate in athletics, either on intramural or intercollegiate teams.
METHODS
Participants
A stratified sample of 80 cadets of the USMA Class of 2007 (n˜1300) was randomly selected to wear wrist activity monitors (WAMs) and complete activity logs. This sample was selected on the basis of sex, unit (company to which the cadet was assigned), and athletic status (participation on either an intramural or an intercollegiate athletic team). The Corps of Cadets is comprised of approximately 85% males and 15% females. In order to have a sufficient number of females in the study for statistical purposes, females were over-sampled. Therefore, the 80 cadets in the sample at the beginning of each data collection period included 56 males (70%) and 24 females (30%). At the beginning of the study, all members of the Class of 2007 ranged in age from 17 to 22; the age of the sample of participants ranged from 18 to 23 (mean = 18.8 y, SD = 0.89 y, median = 19 y). When participants were lost from the study due to attrition, either from withdrawing from USMA or withdrawing from the sleep study, replacements were drawn from a pool of volunteers matched by sex, unit, and athletic status.
Although menstrual cycle is known is to be associated with lower reported sleep quality and increased sleep disturbances,40–43 this factor was not recorded during the study. Participants were treated in accordance with ethical standards established by the American Psychological Association. The research methods used in this study were approved by the USMA Human Subjects Use Committee. All participants gave written informed consent prior to participating in the study.
Equipment
Estimates of cadet sleep were obtained using wrist activity monitors (WAMs) (Actigraph Model AW-64; Mini Mitter Respironics, Inc.) Actigraphy has been used extensively as a method for the objective assessment of sleep,44,45 although some constraints do exist on its acceptability.46,47 Actigraphic recordings followed the recommendations of Standards of Practice Committee of the American Academy of Sleep Medicine (2002). Actigraphic epoch length was 60 sec. Participants were instructed to wear the WAMs on the non-dominant hand at all times of the day and night during the study period. Cadets filled out a paper and pencil activity log to indicate their activities during the study. This log divided each day into 15-m increments and was tailored to the specific activities of the military lifestyle at USMA.
Analysis of the actigraphic recordings was conducted using Actiware Version 5.01.0007 software with the following parameters: Epoch Length = 1 minute, Wake Threshold Selection = Medium, Sleep Interval Detection Algorithm = Immobile Minutes, Immobile Minutes for Sleep Onset = 10, Immobile Minutes for Sleep End = 10. The software facilitated the calculation of sleep episode duration. Statistical analysis was conducted with Microsoft Excel and JMP Release 7.0 from the SAS Institute.
Procedure
A stratified random sample of the students in the Class of 2007 (approximately 80 participants) was selected to wear WAMs concurrently for approximately 30 days during 4 fall academic semesters (2003 to 2006), and again during 4 spring academic semesters (2004 to 2007). In order to have equivalent fall and spring data collection, these periods were always situated between mid-October and early December, and from the beginning of March to early May. Each of the 8 data-collection periods included about 4 contiguous weeks of normal academic activities with no holiday or examination periods. Cadets were asked to fill out a daily activity log when they wore the wrist activity monitors. On these logs, participants indicated their work and rest activities, especially those periods when they slept or napped.
As much as possible, the same 80 cadets were studied through each of the eight 30-day data collection periods. Cadets lost to the study, either through attrition from the Academy or by choosing to drop out of the study, were replaced by cadets in the same year group. They were also matched by sex and athletic status. Sleep estimates (sleep episode duration, and bedtime/wakeup time) were derived from the actigraphic recordings in conjunction with event markers (when used), and were verified by the self-reported activity logs. After determining the bed and wakeup times, the Actiware software was used to calculate sleep duration.
Sleep estimates based only on self-report (i.e., sleep estimates from activity logs without actigraphy data) were excluded from the analysis to avoid systematic errors.48 However, sleep estimates when only actigraphy was available were included. Because cadets have a rigid and tightly controlled daily schedule, assessing nightly sleep episodes was straightforward. The assessment of naps was not as simple, however. The cadet daily schedule includes class attendance and study time during which activity is decreased. In the absence of sleep logs, these periods of low activity could erroneously be scored as naps. During the academic year (AY) 2004 (i.e., fall 2003 and spring 2004), cadets did not fill out the activity logs consistently; thus, sleep logs were not used for analysis of sleep during AY 2004 and nap analysis was not conducted for AY 2004. The study protocol was approved in advance by both the Naval Postgraduate School and USMA Institutional Review Boards. Each participant provided written informed consent before enrolling in the study.
Analytical Approach
The analytical approach was designed to assess the amount of sleep received by Cadets at USMA and to determine if this quantity was related to a number of independent variables: academic year (2003–2007), semester (first through eighth), season (fall or spring), day category (school day or weekend), week day (Sunday through Saturday), and sex (male or female). The main dependent variables examined were nighttime sleep (that is, the major nightly sleep episode) and daily sleep (24-h total). Actigraphic recordings were used to determine bedtime, wakeup time, and sleep episode duration. These data were entered into a Microsoft Excel spreadsheet. Statistical analysis was conducted with Excel and JMP Release 7.0. When needed, data normality was assessed with the Shapiro-Wilk W test. Analysis of variance, effect size calculation, and nonparametric tests were used when appropriate to assess the study responses. Statistical significance was indicated for 2-tailed P values < 0.05.
RESULTS
Table 2 shows the number of cadets whose sleep was used for analysis by semester and year. The table also indicates the numbers and percentages of males and females and the attrition rate for each semester. There were 2 major causes of data loss: equipment failure and cadet attrition. In a few cases each semester, actigraphy data were lost due to mechanical failures of the WAMs. In addition, each semester, a small percentage of cadets chose to withdraw from the study (either to leave USMA or for other reasons). The highest cadet attrition rate occurred in the fall semester of 2005. This time point coincided with a major decision point in a cadet's education; at that point, cadets had to leave or make a final commitment to remain at USMA. If cadets decided to remain at the academy, they incurred an obligation of 5 years of military service upon graduation. The attrition rate in Table 2 refers to the aggregated percentage of cadets who withdrew from the study for that specific semester, whatever the reason. To fill in for those cadets lost to attrition the previous semester, we recruited additional members from the Class of 2007, matching by sex and athletic status, to ensure that there were 80 study participants enrolled at all times.
Table 2.
Participating cadets with actigraphy data
| Semester | Participants | Males | Females | Attrition rate |
|---|---|---|---|---|
| Fall 2003 (AY 2004-1) | 73 | 51 (70%) | 22 (30%) | - |
| Spring 2004 (AY 2004-2) | 75 | 52 (69%) | 23 (31%) | 2.5% |
| Fall 2004 (AY 2005-1) | 74 | 53 (72%) | 21 (28%) | 5.0% |
| Spring 2005 (AY 2005-2) | 69 | 50 (73%) | 19 (28%) | 1.3% |
| Fall 2005 (AY 2006-1) | 72 | 51 (71%) | 21 (29%) | 8.8% |
| Spring 2006 (AY 2006-2) | 55 | 35 (64%) | 20 (36%) | 0.0% |
| Fall 2006 (AY 2007-1) | 69 | 49 (71%) | 20 (29%) | 2.5% |
| Spring 2007 (AY 2007-2) | 56 | 40 (71%) | 16 (29%) | 3.8% |
Over the entire 4-year data collection period, 13,645 days of activity and rest were examined. This number included 17,285 individual sleep episodes, comprising both nighttime sleep and daytime naps. Each of the 8 data collection periods was approximately 30 contiguous days in length. In order to calculate daily sleep (that is, the amount of sleep obtained in a 24-h period), naps taken during the day had to be combined with the night's sleep either before or after the nap. That is, a nap taken during the day on Friday could have been added to the previous Thursday night's sleep episode or to the sleep episode on Friday night. Daily sleep (that is, the amount of sleep obtained in a 24-h period) was calculated by combining any nap taken during the day with the prior night's sleep. For AY 2005, 2006, and 2007, the average daily (24 h) sleep was 5 h 46 m (SD = 1 hr 28 m, median = 5 h 33 m). Napping data were not recorded for AY 2004; therefore, daily sleep could not be estimated. Over all 4 years of this study, average bedtime, wake time, and actual nighttime sleep are shown in Table 3.
Table 3.
Average bedtime, wakeup time and actual nighttime sleep per day category (school or weekend night)
| Parameter | School night | Weekend night | Combined |
|---|---|---|---|
| Bedtime | 00:25 | 01:11 | 00:35 |
| SD = 1 h 06 m | SD = 1 h 42 m | SD = 1 h 18 m | |
| Wakeup time | 06:18 | 08:35 | 06:43 |
| SD = 51 m | SD = 2 h 12 m | SD = 1 h 40 m | |
| Actual nighttime sleep | 5 h 03 m | 6 h 29 m | 5 h 24 m |
| SD = 1 h 02 m | SD = 1 h 51 m | SD = 1 h 25 m | |
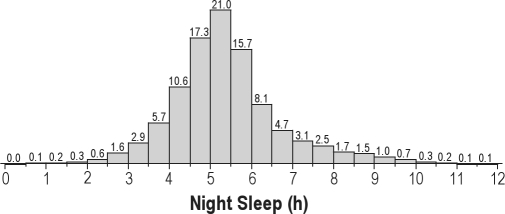
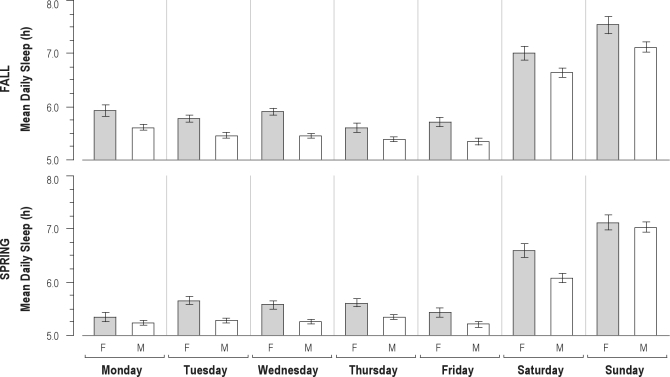
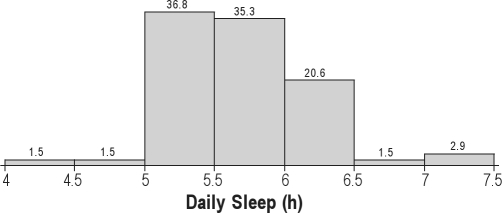
Figure 1 shows the distribution of nighttime sleep across all participants for the entire 4-year period.
Figure 1.
Distribution of nighttime sleep duration (for all participants over all four years, AY 2004–2007).
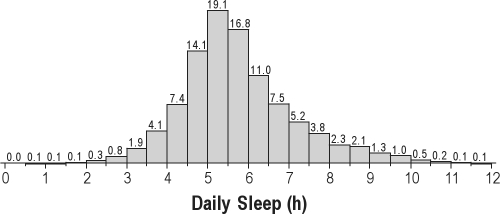
Figure 2 shows the 24-h daily sleep (nighttime sleep plus daytime naps) for the final 3 years at USMA. Daily sleep for the first year at USMA (AY 2004) is not included because cadets did not fill out activity logs for that year.
Figure 2.
Distribution of daily sleep duration (all participants for AY 2005, 2006, and 2007).
Analysis of variance and effect size analysis showed that sleep time (either nighttime or daily sleep) was associated with academic year, semester, season (fall or spring), sex, weekday/weekend category (that is, school day or weekend), and day of the week. Table 4 shows the significance level of these findings. (See text and subsequent tables and figures for direction of these parameter effects.)
Table 4.
Significant predictors of nighttime and daily sleep duration (based on average sleep amount per cadet)
| Parameter | Nighttime Sleep All AY |
Daily Sleep AY 2005, 2006, 2007 |
||
|---|---|---|---|---|
| Test statistic/P-value | Effect size Cohen's d or f2 | Test statistic/P-value | Effect size Cohen's d or f2 | |
| Academic year | F3,310 = 9.85 | f2 = 0.08 | F2,230 = 17.9 | f2 = 0.16 |
| P < 0.0001 | P < 0.0001 | |||
| Semester | F7,533 = 7.46 | f2 = 0.10 | F5,387 = 11.74 | f2 = 0.15 |
| P < 0.0001 | P < 0.0001 | |||
| Season | 1-sided t = 1.749 | d = 0.26 | F1,176 = 6.07 | d = 0.37 |
| P = 0.0409 | P = 0.0147 | |||
| Sex | F1,95 = 10.21 | d = 0.79 | F1,95 = 11.36 | d = 0.86 |
| P = 0.0019 | P = 0.0011 | |||
| Day category | F1,192 = 263.9 | d = 2.33 | F1,183 = 207.7 | d = 2.12 |
| P < 0.0001 | P < 0.0001 | |||
| Week day | F6,670 = 128.6 | f2 = 1.15 | F6,634 = 93.4 | f2 = 0.88 |
| P < 0.0001 | P < 0.0001 | |||
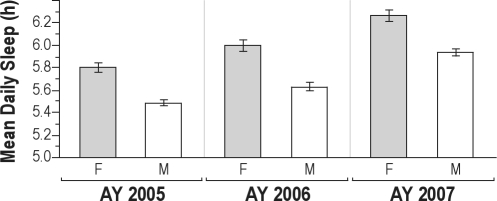
Many of the cadets napped; quite possibly, this napping was a strategy to compensate for the chronic sleep deprivation they experienced. Over one-quarter (26.2%) of all cadet-days (n = 2541) included at least one nap episode. The overall effect of napping on daily sleep of all participants (the average increase from nighttime to daily sleep) was 4.4% or 17.3 m (SD = 9.3% or SD = 39.2 m). For only those cadet-days which included nap episodes, the effect of napping on daily sleep increased by 16.8% or 66.1 m (SD = 11.1%, median = 14.1% or SD = 51.4 m, median = 50.0 m). The average daily sleep (per cadet by semester) increased annually by 12 and 19 m across the last 3 years at USMA (F2,230 = 17.9911, P < 0.0001). Cadets obtained the least daily sleep (AY 2004 excluded) during their second year at the USMA (5.56 h), while receiving the most daily sleep during the fourth year (6.07 h). As seen in Figure 3, this increase in daily sleep across years was significant for both male and female cadets (P < 0.0001) for each year of the study.
Figure 3.
Daily sleep by sex (F,M) and academic year (AY) for AY 2005, 2006 and 2007.
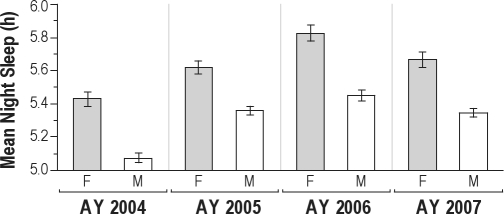
Figure 4 illustrates the change in nighttime sleep by academic year and sex. Nighttime sleep increased consistently over the first 3 years, but there was a significant decrease in nighttime sleep during the fourth year (F3,310 = 9.8522, P < 0.0001), corresponding to the increased demands and responsibilities faced by cadets in their final year at USMA. Figure 4 shows that this annual pattern was consistent for both male and female cadets.
Figure 4.
Nighttime sleep by sex (F,M) and academic year (AY).
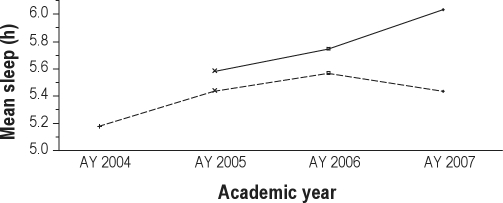
Figure 5 shows the average daily (24-h) and nighttime sleep by academic year. Cadets employed napping strategies during the day quite possibly to supplement their nighttime sleep during the last 3 years. They received the least nighttime sleep during their first year at the Academy, then received significantly more in the 2 subsequent years, with nighttime sleep amount dropping again in their final year. This drop in nighttime sleep probably is caused by additional duties and responsibilities during the final year and is compensated, to some extent, by an increase in daytime napping.
Figure 5.
Average nighttime and daily sleep by academic year (AY). The dotted line shows the average sleep during the night, while the solid line is the average level of daily (24 h) sleep.
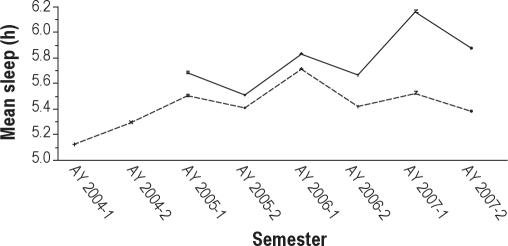
Seasonal Trends
The next step in the analysis was to investigate nighttime and daily sleep patterns by semester. Figure 6 shows an obvious zigzag pattern between sleep in the spring and fall semesters. This pattern is evident for both daily (solid line) and nighttime (dashed line) sleep. With the single exception of the first semester, cadets slept significantly less in the spring than in fall semester. Again, daily sleep for AY 2004 is excluded from the analysis since cadets did not report their napping in the first year of the study.
Figure 6.
Nighttime and daily sleep by semester. The dashed line shows the average sleep during the night, while the solid line is the average level of daily (24 h) sleep.
As shown in Table 5, the seasonal difference in sleep quantity also resulted in differences in bedtime and wake-up time. There were significant differences for all categories except for bedtime on school nights. These results are based on AY 2005, 2006, and 2007 only. After AY 2004, the administrative leadership at USMA instituted a mandatory lights out policy that promoted earlier bedtimes. It should be noted that the early morning mandatory breakfast formation requires cadets to wake up earlier than they would otherwise choose and quite possibly, earlier than their civilian counterparts.
Table 5.
Seasonal effect on bedtimes and wake-up times for school nights and weekend nights for Academic Years 2005, 2006, and 2007
| Time | Fall | Spring | Test statistic | P-value | Effect size (Cohen's d) | |
|---|---|---|---|---|---|---|
| School nights | ||||||
| Bed time | 00:23 | 00:21 | F1,7508 = 1.26 | 0.2625 | 0.03 | |
| Wake-up | 06:16 | 06:13 | F1,7508 = 6.21 | 0.0127 | 0.05 | |
| Weekend nights | ||||||
| Bed time | 01:17 | 00:53 | F1,2242 = 30.81 | < 0.0001 | 0.24 | |
| Wake-up | 08:56 | 08:16 | F1,2242 = 53.36 | < 0.0001 | 0.31 | |
As can be seen in Table 6, this pattern of less sleep in the spring semester was seen for both males and females (analysis based on average sleep per cadet by semester for AY 2005 – 2007).
Table 6.
The effect of season on nighttime and daily sleep by sex for Academic Years 2005, 2006, and 2007
| Sex | Time | Test statistic | P-value | Effect size (Cohen's d) |
|---|---|---|---|---|
| Males | Nighttime Sleep | F1,284 = 9.16 | 0.0027 | 0.36 |
| Daily sleep | F1,284 = 3.88 | 0.0017 | 0.38 | |
| Females | Nighttime Sleep | F1,105 = 7.41 | 0.0076 | 0.53 |
| Daily sleep | F1,105 = 7.97 | 0.0057 | 0.54 |
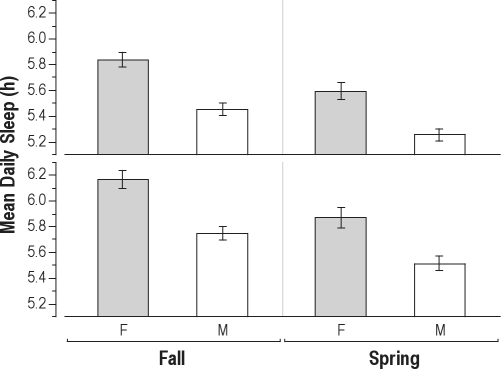
Consistent for both sexes, the decrease in sleep amount from fall to spring semesters ranged from 12 to 15 m for nighttime sleep (females: fall = 5.84 h, spring = 5.59 h; males: fall = 5.45 h, spring = 5.25 h), and from 14 to 18 m for daily sleep (females: fall = 6.17 h, spring = 5.87 h; males: fall = 5.75 h, spring = 5.52 h). In this study population, male cadets got consistently less sleep than their female counterparts. This difference was approximately 21 m for nighttime sleep and 23 m for daily sleep amount. The seasonal effect by sex is shown in Figure 7.
Figure 7.
Difference in sleep amount for females (F) and males (M). Nighttime and daily sleep are based on AY 2005, 2006, and 2007.
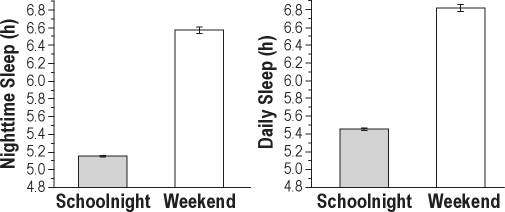
Analysis of variance of cadets' sleep patterns showed that there was a significant difference in the amount of sleep on school nights compared to weekend nights. For both nighttime and daily sleep, cadets received significantly less sleep on school nights compared to weekend nights. When averaging over all semesters, this difference was approximately 1.4 h, as seen in Figure 8. That is, cadets received 27% more sleep on weekend nights than on school nights.
Figure 8.
Difference between nighttime and daily sleep for school and weekend nights. Nighttime sleep is based on AY 2004–2007; Daily sleep is based on AY 2005, 2006, and 2007.
When analyzing sleep on a day-to-day basis, there are clearly 2 distinct categories: schooldays (Monday to Friday) and weekends. As already shown, cadets received significantly more sleep on the 2 weekend nights. Sleep on school nights is fairly homogeneous due to the inflexibility of the USMA schedule. Saturday and Sunday sleep patterns are significantly different from each other, however (nighttime sleep for all AY: F1,3237 = 162.7313, P < 0.0001, Cohen's d = 0.45; daily sleep for AY 2005, 2006, and 2007: F1,2228 = 94.7078, P < 0.0001, Cohen's d = 0.41). In general, cadets received more daily sleep on Sunday (i.e., sleep on Saturday nights plus Sunday naps) than on Saturday (i.e., sleep on Friday night plus Saturday naps) Δ = 0.81 h; daily sleep for AY 2005, 2006, and 2007: Δ = 0.74 h). The sex differences (all P < 0.001) are illustrated in Figure 9.
Figure 9.
Sex differences in daily sleep by season and day of the week (AY 2005, 2006, and 2007).
Sex Differences
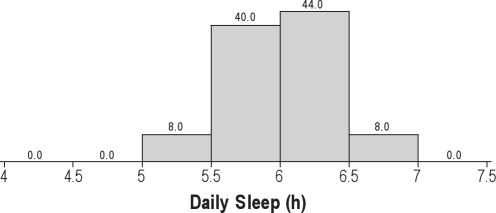
We examined the amount of sleep received by individual cadets using average daily sleep amounts (i.e., sleep received in a 24-h period). Average daily sleep per participant during AY 2005, 2006, and 2007 ranged from 4.39 h to 7.35 h. Sex played a significant role in determining sleep amount (F1,91 = 11.7235, P = 0.0009, Cohen's d = 0.84), with male cadets receiving an average of 5.68 h daily sleep, whereas female cadets received 6.04 h. Furthermore, males, as compared to females, had more variability in daily sleep as shown in Table 7.
Table 7.
Average daily sleep variability by sex (in hours for AY 2005, 2006, and 2007)
| Sex | Min | 10% quantile | 25% quantile | Median | 75% quantile | 90% quantile | Max |
|---|---|---|---|---|---|---|---|
| Females | 5.37 | 5.49 | 5.74 | 6.11 | 6.34 | 6.53 | 6.91 |
| Male | 4.39 | 5.20 | 5.38 | 5.61 | 6.01 | 6.19 | 7.35 |
The distribution of sleep for males and females is illustrated in Figures 10 and 11.
Figure 10.
Average daily sleep for male participants (AY 2005, 2006, and 2007).
Figure 11.
Average daily sleep for female participants (AY 2005, 2006, and 2007).
As already noted, cadets slept significantly more on weekends. The average increase of daily sleep per participant was 1.31 h (SD = 1.07 h), or 25.0% (SD = 21.8%). The increase in daily sleep on weekends was related to daily sleep on school nights. That is, those cadets who slept less during the week probably attempted to compensate for their accumulated sleep debt by sleeping more on weekends. This effect was more pronounced for male cadets. These results are shown in Table 8 (one outlier deleted).
Table 8.
Difference in daily sleep between school nights and weekends by sex
| Sex | Difference in Daily Sleep | Test statistic/P-value | Correlation r |
|---|---|---|---|
| Males | Abs | F1,260 = 37.6, P < 0.0001 | −0.36 |
| % | F1,260 = 69.5, P < 0.0001 | −0.46 | |
| Females | Abs | F1,98 = 3.56, P = 0.0623 | −0.19 |
| % | F1,98 = 10.2, P = 0.0019 | −0.31 |
DISCUSSION
This study assessed cadet sleep patterns at USMA, and evaluated whether, and to what extent, these military, college-age students are chronically sleep deprived. Our results show that sleep of cadets at USMA is associated with academic year, semester, season, sex, day category (school day or weekend), and day of the week.
The major conclusion from this longitudinal study is that cadets experience significant and chronic sleep deprivation during their four years of study at USMA. Given that the physiologically recommended requirement for sleep in adolescents and young adults is 8.5 to 9.25 h,49 the cadet sleep debt is considerable, averaging over 3 hours per day for each day they attend USMA. Upon graduation, cadets have accumulated a sleep debt of thousands of hours per individual cadet. Although there are large individual differences in vulnerability to sleep deprivation,50 there is no question that this entire population is sleep deprived. Even on weekends, when cadets sleep more than on schoolnights, these students consistently receive much less sleep than is recommended for their (or any) age group. On average, cadets receive 5 h 3 m of sleep at night and only 5 h 27 m (median = 5 h 23 m) for daily (24 h) sleep on schooldays, significantly less than the 7 h 4 m of average night sleep reported in the Wolfson and Carskadon (1998) survey of sleep in 19 year olds 25 or other related studies.15,19,51
Most of the differences in sleep reported in this study are less than 30 minutes in duration; however, in this constrained environment for these chronically sleep-deprived cadets, 30 minutes represents a substantial discrepancy. A striking finding is that participants in the USMA study receive on average only 1 h 24 m of “catch-up” sleep on weekends, whereas other studies with college students report increased sleep during weekends51 or an additional 2 hours on weekends.19,25 The cadets at USMA are not only more sleep deprived than their civilian peers, but they also obtain less catch-up sleep than is needed during weekends to compensate for their accumulated sleep debt. The potentially negative effects of this sleep restriction include risks to both academic performance and health.27,28,52,53 The increase in daily sleep on weekends compared to school nights was more pronounced in those cadets who slept less during the week. This finding indicated that the greater the sleep debt accumulated during week days, the more pronounced the cadets' need to compensate for the lost sleep on weekends.
A further concern resulting from this study is the future behavior of these military cadets. As part of their collegiate experience, they have been forced to practice poor sleep hygiene which could quite possibly result in lifelong habits that could follow them into their military careers. This possibility is especially worrisome in light of the potential for degraded decision making and impaired judgment by these cadets once they leave the academy and begin active duty military service. Harrison and Horne reviewed the impact of sleep deprivation on various cognitive activities, including decision making.54 While many studies focus on the effects of sleep deprivation on simple and monotonous task performance, realistic tasks such as high-level decision making are commonly experienced by managers and military leaders who work extended hours during times of crises. In their review, they suggest that sleep deprivation may not affect complex rule-based logical task performance—perhaps due to the heightened interest and compensatory efforts by participants. However, they conclude that sleep deprivation does affect decisions that involve creative solutions, dynamic replanning, managing competing demands, and complex communication—all critical macro-cognitive activities inherent in military environments. Harrison and Horne discuss the critical role of the prefrontal cortex (PFC) in tasks of this nature and suggest that sleep deprivation “presents particular difficulties for sleep-deprived decision makers who require these latter skills during emergency situations.”54 Recent studies have also linked sleep deprivation and changes in the activity of the PFC, strengthening this argument.
Our analysis shows two distinct patterns in USMA cadet sleep: an annual pattern with cadets getting progressively more sleep with each year, and a seasonal pattern with less sleep in spring than in fall semesters. During the last year at USMA, cadets received more daily sleep than during their previous years. However, in this final year, they got less sleep at night but took more naps during the day, probably attempting to compensate, resulting in an overall increase in daily sleep. The study shows that the closer cadets get to graduation, the more sleep they obtain. However, in general, discretionary time also increased with seniority, raising the question about whether the increase in sleep is situational or developmental. We are not able to distinguish between these two potential causes. Nevertheless, the rigid daily schedule at USMA, combined with the significant effect of cadet seniority in daily activities, provide evidence that this increase in sleep can reasonably be situational.
As has been reported in this paper, cadets received more nighttime sleep in fall 2004 than fall 2003. There are at least three factors that contributed to this increase. First, there was a mandatory lights out policy for the Corps of Cadets that was implemented in fall 2004. After data from the first year of the longitudinal study were analyzed, the authors presented the results to the Academy's senior leadership (spring 2004). Subsequent discussions considered various courses of action to increase the amount of sleep cadets received. The Superintendent decided to reinstate a mandatory lights out policy at the beginning of the fall 2004 semester. While this decision was less than ideal in the middle of a longitudinal study, the authors had no control over this change in schedule. Second, freshman cadets often have duties they must carry prior to breakfast. These duties require them to awaken early. When they become sophomore cadets they are no longer required to perform these duties. Third, the general trend at the Academy is that, as cadets progress from freshmen to seniors, they have more discretionary time, as well as more privileges and responsibilities. Cadets may use at least some of their increased discretionary time to get more sleep.
In line with other findings, we found seasonal differences in the sleep patterns of cadets. Other researchers have reported seasonal differences in sleep with individuals getting significantly more sleep in fall and winter than in spring and summer.55,56 This same pattern is evident in the USMA cadets with one notable exception. In their first semester (fall of 2003) cadets got less sleep than in the spring semester. We attribute this anomalous finding to the fact that cadets had just arrived at USMA and were experiencing the stress that often accompanies indoctrination into military education and training regimens.
Our study also found significant sex differences in sleep patterns. Males sleep less than females in every condition, whether fall or spring, day of the week, weekend, or school night. One possible explanation for this finding may be social differences between males and females57 or differences in the amount of sleep needed based on the sleep/wake circadian cycle.58 We did not control for menstrual cycle, since this was not the focus of the current study. However, since we collected approximately one month of data for each of the eight semesters of the study, it is certain that menstrual cycles are represented in the variability of the data. Any menstrual cycle effect would be expected to decrease female cadets' sleep, therefore reducing the difference in sleep found in females as compared to male cadets. Still another possible explanation for the sex differences we observed may be differences in circadian chronotype. Supporting this idea, a recent study by Adan and Natale conducted in a large university population that showed significant differences in circadian typology between males and females (P < 0.0001), with the males presenting a more pronounced evening preference.59
The generalizability of these findings to the rest of the population is limited for a number of reasons. The specific attributes of the military academic environment with its highly structured schedule are in clear contradiction to the latitude found in the daily schedule of typical college life. There is much less variability in the cadet sleep patterns than those of a typical college student because of the rigidity of the cadet daily schedule. In addition, the corps of cadets represents a highly selected population and may not be representative of the general population or of college-age students elsewhere. The participants who chose to remain in the study (and to remain at USMA) represent a self-selected population, in that they may be better able to tolerate sleep deprivation than the general college student population. Finally, the attrition rates (i.e., attrition from the Academy or from the study) are explained by the fact that this is a longitudinal study spanning eight one-month data collection periods over four years. Even though the replacement cadets were demographically matched with those choosing to withdraw, the drop-out rate is always an issue of concern in longitudinal studies.
These findings are part of a larger study conducted at USMA, and are focused on the sleep patterns of the cadets. Subsequent articles will address napping patterns, patterns of attrition, and the effect of chronotype and personality traits on academic performance in USMA. This study is the first step towards a validated quantification of sleep patterns in military educational institutions. In light of the enormous challenges facing these military cadets upon graduation, the poor sleep hygiene that they have practiced during their four years in school fosters extremely bad habits that may carry over to the workplace. Our findings clearly demonstrate the significant sleep deprivation experienced by cadets, with all the negative consequences that this result implies.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
We would like to acknowledge the support provided by the senior leadership of the United States Military Academy, West Point, NY. Without their permission and unflagging encouragement, this study would never have been completed. We received funding for the study from the Program Executive Office – Soldier (PEO-Soldier) of the U.S. Army. Dr. Mary Carskadon and her colleagues in the Providence Sleep Research Interest Group (PSRIG) offered invaluable insights in the design and implementation of the study. Enthusiastic graduate students from the Naval Postgraduate School assisted in various analyses. Lastly, we acknowledge the selfless service of the Cadets of the Class of 2007 from the United States Military Academy, many of whom are currently serving their country both here and abroad.
Location of Work: Naval Postgraduate School, Monterey, CA and United States Military Academy, West Point, NY
REFERENCES
- 1.Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16:258–62. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- 2.Carskadon MA, Acebo C, Richardson GS, Tate BA, Seifer R. An approach to studying circadian rhythms of adolescent humans. J Biol Rhythms. 1997;12:278–89. doi: 10.1177/074873049701200309. [DOI] [PubMed] [Google Scholar]
- 3.Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21:871–81. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- 4.Wolfson AR, Carskadon MA. Understanding adolescents' sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7:491–506. doi: 10.1016/s1087-0792(03)90003-7. [DOI] [PubMed] [Google Scholar]
- 5.Carskadon MA. Patterns of sleep and sleepiness in adolescents. Pediatrician. 1990;17:5–12. [PubMed] [Google Scholar]
- 6.Carskadon MA. Factors influencing sleep patterns in adolescents. In: Carskadon MA, editor. Adolescent sleep patterns: Biological, social, and psychological influences. Cambridge, UK: Cambridge University Press; 2002. pp. 4–26. [Google Scholar]
- 7.Roenneberg T, Kuehnle T, Pramstaller PP, et al. A marker for the end of adolescence. Curr Biol. 2004;14:R1038–R1039. doi: 10.1016/j.cub.2004.11.039. [DOI] [PubMed] [Google Scholar]
- 8.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 9.Klerman EB, Dijk DJ. Interindividual variation in sleep duration and its association with sleep debt in young adults. Sleep. 2005;28:1253–9. doi: 10.1093/sleep/28.10.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aeschbach D, Sher L, Postolache TT, Matthews JR, Jackson MA, Wehr TA. A longer biological night in long sleepers than in short sleepers. J Clin Endocrinol Metab. 2003;88:26–30. doi: 10.1210/jc.2002-020827. [DOI] [PubMed] [Google Scholar]
- 11.Aeschbach D, Cajochen C, Landolt H, Borbëely AA. Homeostatic sleep regulation in habitual short sleepers and long sleepers. Am J Physiol. 1996;270:R41–53. doi: 10.1152/ajpregu.1996.270.1.R41. [DOI] [PubMed] [Google Scholar]
- 12.Webb WB. Are short and long sleepers different? Psychol Rep. 1979;44:259–264. doi: 10.2466/pr0.1979.44.1.259. [DOI] [PubMed] [Google Scholar]
- 13.Van Dongen HPA, Vitellaro KM, Dinges DF. Individual differences in adult human sleep and wakefulness: leitmotif for a research agenda. Sleep. 28:479–96. doi: 10.1093/sleep/28.4.479. [DOI] [PubMed] [Google Scholar]
- 14.Hicks RA, Mistry R, Lucero K, Lee L, Pellegrini R. The sleep duration and sleep satisfaction of college students: striking changes over the last decade (1978-1988) Percept Mot Skills. 1989;68:806. doi: 10.2466/pms.1989.68.3.806. [DOI] [PubMed] [Google Scholar]
- 15.Hicks RA, Pellegrini R. The changing sleep habits of college students. Percept Mot Skills. 1991;72:1106. doi: 10.2466/pms.1991.72.3c.1106. [DOI] [PubMed] [Google Scholar]
- 16.Hicks RA, Fernandez C, Pellegrini R. Striking changes in the sleep satisfaction of university students over the last two decades. Percept Mot Skills. 2001;93:660. doi: 10.2466/pms.2001.93.3.660. [DOI] [PubMed] [Google Scholar]
- 17.Gibson ES, Powles AP, Thabane L, et al. “Sleepiness” is serious in adolescence: Two surveys of 3235 Canadian students. BMC Public Health. 2006;6:116–25. doi: 10.1186/1471-2458-6-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller NL, Shattuck LG. Sleep patterns of young men and women enrolled at the United States Military Academy: results from year one of a four year longitudinal study. Sleep. 2005;28:837–41. doi: 10.1093/sleep/28.7.837. [DOI] [PubMed] [Google Scholar]
- 19.Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms. 2003;18:80–90. doi: 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- 20.Basner M. Is time for sleep declining among Americans? Sleep. 2010;33:13–14. doi: 10.1093/sleep/33.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carney CE, Edinger JD, Meyer B, Lindman L, Istre T. Daily activities and sleep quality in college students. Chronobiol Int. 2006;23:623–37. doi: 10.1080/07420520600650695. [DOI] [PubMed] [Google Scholar]
- 22.Shenghui L, Xinming J, Shenghu W, Fan J, Chonghuai Y, Xiaoming S. The impact of media use on sleep patterns and sleep disorders among school-aged children in China. Sleep. 2007;30:361–7. doi: 10.1093/sleep/30.3.361. [DOI] [PubMed] [Google Scholar]
- 23.Manni R, Ratti MT, Marchioni E, et al. Poor sleep in adolescents: A study of 869 17-year-old Italian secondary school students. J Sleep Res. 1997;6:44–9. doi: 10.1046/j.1365-2869.1997.00025.x. [DOI] [PubMed] [Google Scholar]
- 24.Naitoh P, Kelly T, Englund CE. Health effects of sleep deprivation. Occup Med. 1990;5:209–37. [PubMed] [Google Scholar]
- 25.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 26.Lange T, Perras B, Fehm HL, Born J. Sleep enhances the human antibody response to hepatitis A vaccination. Psychosom Med. 2003;65:831–5. doi: 10.1097/01.psy.0000091382.61178.f1. [DOI] [PubMed] [Google Scholar]
- 27.Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 28.Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 29.Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2005;25:117–29. doi: 10.1055/s-2005-867080. [DOI] [PubMed] [Google Scholar]
- 30.Karni A, Tanne D, Rubenstein BS, Askenasy JJ, Sagi D. Dependence on REM sleep of overnight improvement of a perceptual skill. Science. 1994;265:679–82. doi: 10.1126/science.8036518. [DOI] [PubMed] [Google Scholar]
- 31.Gais S, Plihal W, Wagner U, Born J. Early sleep triggers memory for early visual discrimination skills. Nat Neurosci. 2000;3:1335–9. doi: 10.1038/81881. [DOI] [PubMed] [Google Scholar]
- 32.Fenn KM, Nusbaum HC, Margoliash D. Consolidation during sleep of perceptual learning of spoken language. Nature. 2003;425:614–6. doi: 10.1038/nature01951. [DOI] [PubMed] [Google Scholar]
- 33.Mitler M, Carskadon MA, Czeisler CA, Dement WC, Dinges DF, Graeber RC. Catastrophes, sleep, and public policy: Consensus Report. Sleep. 1988;11:100–109. doi: 10.1093/sleep/11.1.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Miller NL, Shattuck LG, Matsangas P. Sleep and fatigue issues in continuous operations a survey of U.S. Army Officers. Behav Sleep Med. 2009 doi: 10.1080/15402002.2011.533994. Accepted for publication. [DOI] [PubMed] [Google Scholar]
- 35.Miller NL, Matsangas P, Shattuck LG. Fatigue and its effect on performance in military environments. In: Hancock PA, Szalma JL, editors. Performance under stress. Burlington, VT: Ashgate Publishing; 2008. pp. 231–50. [Google Scholar]
- 36.Department of the Army. Combat and Operational Stress Control - Manual for Leaders and Soldiers. Washington, DC: 2009. Field Manual No. 6-22.5. [Google Scholar]
- 37.Shay J. Ethical standing for commander self-care: the need for sleep. Parameters. 1998;28:93–105. [Google Scholar]
- 38.Miller NL, Dyche J, Andrews CH, Lucas TW. Navy boot camp: test score changes after two hour increase in sleep time. 2004 Meeting of the Association of Professional Sleep Societies; 2004 June; Philadelphia, PA. 2004. [Google Scholar]
- 39.Killgore WD, Estrada A, Wildzunas RM, Balkin TJ. Sleep and performance measures in soldiers undergoing military relevant training. 26th Army Science Conference: Transformational Army Science and Technology - Harnessing Disruptive S&T for the Soldier; 2008 December 1–4.2008. [Google Scholar]
- 40.Baker FC, Driver HS. Self-reported sleep across the menstrual cycle in young, healthy women. J Psychosom Res. 2004;56:239–43. doi: 10.1016/S0022-3999(03)00067-9. [DOI] [PubMed] [Google Scholar]
- 41.Manber R, Bootzin RR. Sleep and the menstrual cycle. Health Psychol. 1997;16:209–14. doi: 10.1037//0278-6133.16.3.209. [DOI] [PubMed] [Google Scholar]
- 42.Baker FC, Driver HS. Circadian rhythms, sleep, and the menstrual cycle. Sleep Med. 2007;8:613–22. doi: 10.1016/j.sleep.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 43.Driver HS, Werth E, Dijk DJ, Borbëely AA. The menstrual cycle effects on sleep. Sleep Med Clin. 2008;3:1–11. [Google Scholar]
- 44.Ancoli-Israel S, Cole R, Alessi G, Chambers M, Moorcroft W, Pollak CP. The role of actigraphy in the study of sleep and circadian rhythms. Sleep. 2003;26:342–392. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- 45.Littner M, Kushida CA, McDowell Anderson W, et al. Practice parameters for the role of actigraphy in the study of sleep and circadian rhythms: an update for 2002. Sleep. 2003;26:337–41. doi: 10.1093/sleep/26.3.337. [DOI] [PubMed] [Google Scholar]
- 46.Paquet J, Kawinska A, Carrier J. Wake detection capacity of actigraphy during sleep. Sleep. 2007;30:1362–9. doi: 10.1093/sleep/30.10.1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sadeh A, Acebo C. The role of actigraphy in sleep medicine. Sleep Med Rev. 2002;6:113–24. doi: 10.1053/smrv.2001.0182. [DOI] [PubMed] [Google Scholar]
- 48.Baker F. A comparison of subjective estimates of sleep with objective polysomnographic data in healthy men and women. J Psychosom Res. 1999;47:335–41. doi: 10.1016/s0022-3999(99)00017-3. [DOI] [PubMed] [Google Scholar]
- 49.Carskadon MA, Harvey K, Duke P, Anders TF, Litt IF, Dement WC. Pubertal changes in daytime sleepiness. Sleep. 1980;2:453–60. doi: 10.1093/sleep/2.4.453. [DOI] [PubMed] [Google Scholar]
- 50.Mastin DF, Peszka J, Poling T, Phillips R, Duke J. Personality as a predictor of the objective and subjective impact of sleep deprivation. Pers Individ Dif. 2005;39:1471–82. [Google Scholar]
- 51.Hawkins J, Shaw P. Self-reported sleep quality in college students: a repeated measures approach. Sleep. 1992;15:545–9. doi: 10.1093/sleep/15.6.545. [DOI] [PubMed] [Google Scholar]
- 52.Carskadon MA, Dement WC. Cumulative effects of sleep restriction on daytime sleepiness. Psychophysiology. 1981;18:107–13. doi: 10.1111/j.1469-8986.1981.tb02921.x. [DOI] [PubMed] [Google Scholar]
- 53.Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night. Sleep. 1997;20:267–77. [PubMed] [Google Scholar]
- 54.Harrison Y, Horne JA. The impact of sleep deprivation on decision making: a review. J Exp Psychol. 2000;6:236–49. doi: 10.1037//1076-898x.6.3.236. [DOI] [PubMed] [Google Scholar]
- 55.Lehnkering H, Siegmund R. Influence of chronotype, season, and sex of subject on sleep behavior of young adults. Chronobiol Int. 2007;24:875–88. doi: 10.1080/07420520701648259. [DOI] [PubMed] [Google Scholar]
- 56.Anderson JL, Rosen LN, Mendelson WB, et al. Sleep in fall/winter seasonal affective disorder: effects of light and changing seasons. J Psychosom Res. 1994;38:323–37. doi: 10.1016/0022-3999(94)90037-x. [DOI] [PubMed] [Google Scholar]
- 57.Wilson GD. Personality, time of day and arousal. Pers Individ Differ. 1990;11:153–68. [Google Scholar]
- 58.Wever RA. Properties of human sleep-wake cycles: parameters of internally synchronized free-running rhythms. Sleep. 1984;7:27–51. doi: 10.1093/sleep/7.1.27. [DOI] [PubMed] [Google Scholar]
- 59.Adan A, Natale V. Gender differences in morningness-eveningness preference. Chronobiol Int. 2002;19:709–20. doi: 10.1081/cbi-120005390. [DOI] [PubMed] [Google Scholar]