Abstract
Context
Pituitary adenomas are the most common lesions in the sellar region, but other pathologies need to be considered in the differential diagnosis.
Objective
To assess the prevalence of unusual sellar masses in a large series of patients, and identify clinicopathological factors which may aid the pre-operative diagnosis.
Design
Retrospective case series.
Patients
We analyzed the records of 1469 transsphenoidal procedures performed between 1998–2009. One hundred sixteen cases (7.9%) were not pituitary adenomas.
Measurements
Final pathologic diagnosis.
Results
One hundred sixteen patients (45 males, 71 females; mean age (±SD): 45±17 years) with non-adenomatous lesions were divided into four major etiologic groups: cystic lesions, (53%); benign neoplasms, (22%); malignancies, (16%), and inflammatory lesions, (9%). Rathke's cysts, the most common lesions, represented 42% of all cases. Twenty five percent of malignant lesions were metastases, and some of the malignancies (e.g., fibrosarcoma, lung metastasis) had a radiographic appearance suggestive of a pituitary adenoma. The most common presenting symptoms were visual field impairment (51%) and headache (34%). Pre-operative pituitary dysfunction was present in 58% of cases, with hyperprolactinemia (35%), hypogonadism (23%) and hypocortisolism (23%) found most frequently. Post-operative resolution of headache and visual symptoms occurred in 63% and 65% of patients respectively. Hyperprolactinemia resolved in 77% of cases.
Conclusions
A substantial minority of sellar masses are not pituitary adenomas. While they frequently present with the symptoms, hormone abnormalities, and radiographic appearance typical of pituitary tumors, the possibility of a non-adenomatous lesion needs to be considered in the differential diagnosis.
Keywords: transsphenoidal surgery, sellar masses, rathke cyst, non-adenomatous lesions, pituitary metastasis, vision loss, hypopituitarism, hyperprolactinemia
INTRODUCTION
Transsphenoidal surgery (TSS) is the preferred surgical approach for removal of masses in the sellar and parasellar regions (1–3). Although pituitary adenomas are the most common lesions in this area, there may be other etiologies (4).
In 1996, Freda et al. reported that 9% of sellar/parasellar masses were not pituitary adenomas, and described pathologies including cysts, other benign and malignant tumors, and inflammatory diseases (5). However, limited data have been published presenting the clinical, biochemical and radiographic characteristics typical of each lesion (6).
The aim of the present study is to assess the prevalence of non-adenomatous masses of the sella in a large series of patients who underwent TSS at one tertiary center, and identify clinicopathological factors associated with their etiology and pre-operative diagnosis.
METHODS
From January 1998 through April 2009, 1469 transsphenoidal procedures were performed by a single neurosurgeon (B.S.) for masses in the sellar and parasellar area. One hundred sixteen of them (7.9%) were not pituitary adenomas.
We retrospectively reviewed the records of these cases and collected all available clinical, biochemical, radiographic, and pathological data.
Lesions were classified into four major etiologic groups (Table 1): cysts (CYS) (N=62), benign neoplasms (BEN) (N=25), malignancies (MAL) (N=19), and inflammatory/infectious lesions (INF) (N=10). Cystic neoplasms, e.g., craniopharyngiomas, were considered as benign neoplasms rather than cysts. Preoperative MRIs were available in all patients. Radiographic analysis was based on radiology reports or neurosurgeon assessment. Neuro-ophthalmologic assessment was performed in 57 patients; confrontation visual fields and acuity testing were reported in 65 patients.
Table 1.
Diagnosis and demographics in 116 patients with sellar masses other than pituitary adenomas
| Major etiologic groups | MAL (Malignancies) | CYS (Cysts) | BEN (Benign lesions) | INF (Inflammation/ Infection) |
|---|---|---|---|---|
| 5 Metastasis - pancreas - kidney - lung - prostate |
49 Rathke's Cysts (RC) | 19 Craniopharyngio mas (CF) | 6 Hypophysitis (HP) | |
| 5 Chordomas | 12 Arachnoid cysts | 4 Meningiomas | 1 Sphenoid Sinusitis | |
| 2 Chondrosarcomas clivus | 1 Suprasellar cyst | 1 Clivus Hemangioma | 1 Chronic Infection | |
| 2 Germinomas | 1 Ependymoma | 1 Pituitary Hyperplasia | ||
| 1 SNUC* | 1 Fibrous Dysplasia | |||
| 1 Inverted Papilloma | ||||
| 1 Osteogenic sarcoma | ||||
| 1 Squamous carcinoma** | ||||
| 1 Fibrosarcoma | ||||
| Age (±SD) | 55±14*** | 42±16 | 47±21 | 39±13 |
| M/F | 8/11 | 20/42 | 13/12 | 4/6 |
| N= 116 (%) | 19 (16) | 62 (53) | 25 (22) | 10 (9) |
Sinonasal undifferentiated carcinoma
Invasive squamous carcinoma with features of sinonasal origin
p<0.01 vs. group CYS or INF
Pre- and postoperative assessments of pituitary function were performed according to currently accepted criteria (7), often by the referring physician prior to surgical referral. Laboratory tests were performed in several laboratories and abnormalities reported are based on the normal range indicated for each assay. Data regarding pre-operative hormone replacement were available for every patient, although formal testing at our institution was performed only post-operatively. This study was approved by the Institutional Review Board of Partners HealthCare.
PATHOLOGICAL ASSESSMENT
Pathological assessment was based upon intra-operative frozen section and/or cytological smears in combination with post-operative paraffin sections. Histological diagnosis was obtained from all solid masses. Pathology from biopsy of the cyst wall was available in 14/49 (28.5%) Rathke's cysts. In the absence of tissue from the cyst wall, the diagnosis was made based on examination of the cyst contents. RCC were characterized on the basis of mucoid, generally acellular, proteinaceous debris, sometimes with an inflammatory component, and the absence of fluid suggestive of a craniopharyngioma (6).
STATISTICAL ANALYSIS
Quantitative outcomes are presented as mean ± SD unless stated otherwise; categorical outcomes are presented as frequency count and proportion (%). To examine group differences, analysis of variance was used for continuous variables, and χ2 or Fisher's exact test for categorical variables. A test with p-value <0.05 was considered statistically significant. All analyses were carried out using SAS 9.2 (SAS Institute, Inc., Cary, NC).
RESULTS
Pathologic diagnoses of non-pituitary sellar masses
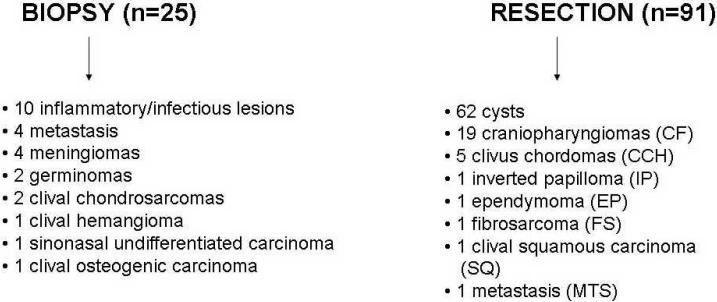
The pathologic diagnoses are shown in Table 1 and Figure 1. Non-neoplastic cystic lesions were most common, found in 62 /116 (53%) of cases. Forty-nine of the cysts (49/62; 79%) were Rathke's cysts, 12 (12/62; 19%) were arachnoid cysts; the biopsy of one cyst wall was fibrous tissue and was considered non-diagnostic. Benign neoplasms were found in 25 patients (22%), including 19 craniopharyngiomas (76%), 4 meningiomas (16%), one clivus hemangioma (4%) and one primary ependymoma of the sella (4%). The pathological evaluation of the ependymoma has been previously reported (8).
Figure 1.
1A Surgical procedures on 116 non-adenomatous sellar masses. 1B Outcome after treatment in 91 resected non-adenomatous lesions.
* Data are missing for 1 Rathke's cyst (RC), 1 craniopharyngioma (CF) and 1 clivus chordoma (CCH). Four RC with residual have no data on progression.
Malignant lesions were found in 19 cases (16%) including five metastases (26%), five clival chordomas (26%), two clival chondrosarcomas (11%), two germinomas (11%), and one each of the following: sinonasal undifferentiated carcinoma (SNUC), inverted papilloma, osteosarcoma, squamous cell carcinoma of sinus origin and primary fibrosarcoma of the sella. The five metastatic tumors included pancreatic islet cell, kidney, lung and prostate carcinomas, and one of unknown origin. The renal carcinoma and carcinoma of unknown origin both presented as sellar masses; the primary site of the other metastatic tumors was already known.
Inflammatory or infectious lesions (INF) were found in ten cases (8.6%), including five cases of hypophysitis (60%), and one each of the following: neurosarcoidosis, sphenoid sinusitis, pituitary hyperplasia, fibrous dysplasia, and chronic actinomyces infection in a patient who had previously undergone surgery for a clival chordoma.
Patient characteristics
Demographic data are shown in Table 1. Mean age at the time of surgery was 45±17 years (range: 13–88; median: 43 years). Patients with malignancies were significantly older than those with cysts or inflammatory lesions.
The male to female ratio overall was 1:1.6. Cysts were twice as common in females as in males: 42 females (34 Rathke's cysts, seven arachnoid cysts, one suprasellar cyst) vs. 20 males (15 Rathke's cysts, five arachnoid cysts) (p<0.01). Hypophysitis occurred more often in women (4/5 cases). There was no significant gender predominance in malignant or benign neoplasms.
Preoperative clinical characteristics
General symptoms
The preoperative clinical presentations are described in Table 2. The most common presenting symptoms were headache (34%), ophthalmologic complaints, including blurred vision/decreased acuity (22%) or diplopia/ptosis (9%), fatigue or weakness (10%), and dizziness (8%). Headache was the most common presentation in both those with cysts (47%) and inflammatory lesions (20%). The most common presenting complaint among patients with malignancies was diplopia/ptosis (47%), while among those with benign tumors it was blurred vision (28%). Prevalence of headache was significantly higher in patients with cysts as compared with the other etiologic groups (p<0.05).
Table 2.
Initial clinical presentation in 116 patients with sellar masses other than pituitary adenomas
| Etiologic groups | % of pts with symptoms | MAL (n=19) | CYS (n=62) | BEN (n=25) | INF (n=10) |
|---|---|---|---|---|---|
| Preoperative sign/symptom | |||||
| NEUROPSYCHIATRIC COMPLAINTS | |||||
| Headache | 34 | 3 (16) | 29 (47)** | 6 (24) | 2 (20) |
| Dizziness | 8 | 0 | 8 (13) | 1 (4) | 0 |
| Hearing loss | 4 | 1 (5) | 2 (3) | 2 (8) | 0 |
| Cognitive complaints | 3 | 1 (5) | 2 (3) | 0 | 1 (10) |
| OPHTHALMOLOGIC DYSFUNCTIONS | |||||
| Blurred vision/visual loss | 22 | 4 (21) | 15 (24) | 7 (28) | 0 |
| Diplopia/Ptosis (documentation of cranial nerve palsy) | 9 | 9 (47)#‡ | 1 (2) | 0 | 0 |
| Visual field impairment on testing* | 51 | 4 (67) | 13 (39) | 12 (71) | 0 |
| GENERAL | |||||
| Fatigue/weakness | 10 | 2 (11) | 7 (11) | 2 (8) | 1 (10) |
| Galactorrhea | 13 | 0 | 6 (14) | 1 (8) | 2 (33) |
Percentages are given in parentheses.
Percentage of visual field impairment was calculated on 57 available examinations. These are distributed as follows: 33 in group CYS; 6 in group MAL; 17 in group BEN; 1 in group INF
p<0.05 vs. the other groups
p<0.001 vs. group BEN or CYS
p<0.05 vs. group INF
Endocrine symptoms
Amenorrhea (17%), galactorrhea (13%), and male sexual dysfunction (18%), were the most common endocrine complaints.
Neurological findings
In the 57 patients with formal visual field examinations, 29 (51%) showed impairment. Ophthalmologic signs were most common in patients with malignancies; forty-seven percent of patients with malignant lesions had diplopia or ptosis (p<0.01 vs patients with cysts (2%) or benign lesions (0%); p<0.05 vs. patients with inflammatory lesions (0%)). Four of 19 patients with malignancies (21%) had blurred vision/visual loss, and 4 out of 6 (67%) with data available had visual field impairment. Sixth nerve palsies were seen in five patients, all with malignancies; another patient with a recurrent chondrosarcoma presented with multiple cranial neuropathies.
No significant differences between the groups were observed in the prevalence of any other reported symptoms or signs.
Preoperative pituitary function
The overall incidence of pre-operative endocrine dysfunction is shown in Table 3. Based on formal testing and/or hormone replacement data, there were 64 endocrine abnormalities in the 45/116 (39%) patients who presented with at least one hormone insufficiency. These included 22/64 cases of hyperprolactinemia (34%), 15/64 of hypogonadism (23%) and 13/64 cases of central hypothyroidism (20%). Adrenal insufficiency was diagnosed in 14 patients (23%). One patient with a malignancy had been started on DDAVP for diabetes insipidus prior to TSS. Because the assessment of GH deficiency was not part of the routine pre-operative evaluation, it is not included in this assessment of pituitary function.
Table 3.
Pituitary function before and after transsphenoidal surgery.
| MAL (n=19) | CYS (n=62) | BEN (n=25) | INF (n=10) | |||||
|---|---|---|---|---|---|---|---|---|
| Cases of pituitary disturbances | Preexisting | Persistent | Preexisting | Persistent | Preexisting | Persistent | Preexisting | Persistent |
| Hypothyroidism | 2 | 2 | 6 | 4 | 2 | 2 | 3 | 3 |
| Hyperprolactinemia | 2 | 0 | 16 | 4 | 2 | 0 | 2 | 1 |
| Hypogonadism | 4 | 4 | 6 | 4 | 2 | 2 | 3 | 2 |
| Hypocortisolism | 2 | 2 | 7 | 6 | 2 | 2 | 3 | 3 |
| Total | 10 | 8 | 35 | 18 | 8 | 6 | 11 | 9 |
| No. of new cases after TSS (%) | ||||||||
| Hypothyroidism | 0 | 0 | 0 | 0 | ||||
| Hyperprolactinemia | 0 | 0 | 0 | 0 | ||||
| Hypogonadism | 1 | 1 | 2 | 0 | ||||
| Hypocortisolism | 1 | 2 | 2 | 0 | ||||
| Permanent DI | 2 | 1 | 0 | 0 | ||||
| Total of new cases | 4 | 4 | 4 | 0 | ||||
| Follow-up (months) | 46±33 | 35±30 | 67±38^‡ | 25±9 | ||||
Follow-up is expressed as mean ± SD; DI: diabetes insipidus. Data regarding pre-operative hormone replacement were available for every patient.
Impairment of more than one axis was observed in a given patient was as follows:
- group MAL (two pts. with two axes altered; one pt. with four axes altered)
- group CYS (five pts. with two axes altered; three pts. with three axes altered)
- group BEN (two pts. with two axes altered; one pt. with three axes altered)
- group INF (one pts. with two axes altered; one pt. with three and one pt. with four axes altered)
p<0.05 vs. group INF
p<0.01 vs. group CYS
No difference was observed in the prevalence of any specific hormone dysfunction between the four groups.
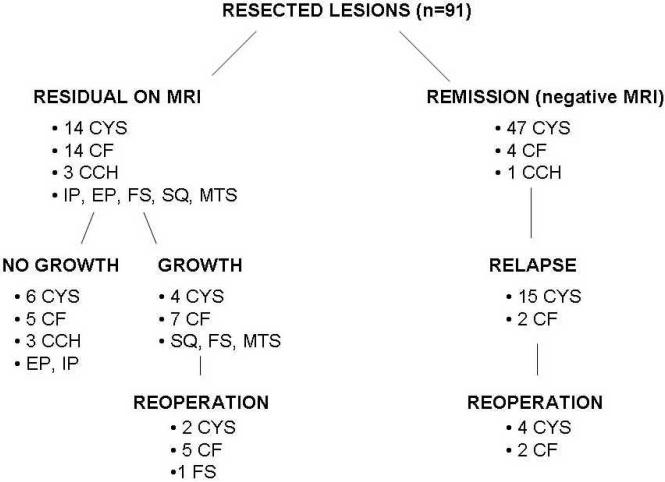
Radiographic characteristics
The radiographic characteristics of the cystic lesions are shown in Table 4 and Figure 2. In general, Rathke's cysts exhibited some degree of rim enhancement, as opposed to minimal/ no enhancement in arachnoid cysts. Arachnoid cysts typically contained fluid of CSF density, while the imaging characteristics of the contents of Rathke's cysts were variable. One arachnoid cyst was a large lesion measuring 4 cm in its maximum diameter, hyperintense on T2-weighted images, which compressed the cavernous sinuses bilaterally and abutted the undersurface of the optic chiasm. Another cyst, measuring 1.3 cm, appeared as isointense on T1, relatively isointense on T2 relative to cortex, and showed a slight post-contrast enhancement. It was contiguous with the superior aspect of the pituitary gland and extended superiorly producing mass effect, elevation of the optic chiasm and left-deviation of the stalk. These findings were considered suggestive of cystic macroadenoma or, alternatively, inflammation processes or craniopharyngioma. The pathology examination was not diagnostic, showing a fibrous-walled cyst with hemorrhage. Craniopharyngiomas usually contained an enhancing solid component. One craniopharyngioma was thought to be either a cystic adenoma or a Rathke's cyst with a component of high-protein fluid or hemorrhage on MRI. Another craniopharyngioma appeared as a solid enhancing mass with several small cystic appearing areas. A partially calcified craniopharyngioma measured 4.5 cm and extended anteriorly into the sphenoid sinus and posteriorly to the ethmoid-air cells. It also eroded both anterior and posterior clinoid processes bilaterally. The ependymoma appeared as a 2 cm mass expanding the sella, extending to the left cavernous sinus and superiorly abutting the undersurface of the chiasm. It was radiographically consistent with a macroadenoma. Two meningiomas had equivocal MRI characteristics, suggesting a possible alternative diagnosis of adenoma. One of them was a homogeneously enhancing 2 cm- intrasellar lesion which was indistinguishable from the pituitary and extended to the right cavernous sinus and along the tentorium. The other arose from the right lateral wall of the sella and extended to the chiasm.
Table 4.
Radiographic characteristics of the cystic lesions
| Rathke's cysts | Arachnoid cyst | Undetermined cyst | Craniopharyngiomas | |
|---|---|---|---|---|
| T1 characteristics | ||||
| Low | 34 (69) | 12 (100) | 1 | 3 (30) |
| High | 12 (24) | 7 (70) | ||
| Mixed | 3 (6) | |||
| T2 characteristics | ||||
| Low | 1 | |||
| High | 42 (86) | 12 (100) | ||
| Mixed | 7 (14) | |||
| Enhancement after contrast | 7 (14) | 2 (15) | 1 | 9 (90) |
| Calcifications | 2 (10) | 0 | 5 (56) | |
| Localization | ||||
| Intrasellar | 25 (51) | 8 (66) | ||
| Suprasellar | 2 (2) | 0 | 2 (11) | |
| Intra/Suprasellar | 22 (45) | 4 (33) | 1 | 17 (89) |
Percentages are expressed in parentheses and are calculated on the basis of the available records for each characteristic.
Figure 2.
Difficult radiographic differentials. 2A–B: Cystic abnormalities. 2A shows a large cystic lesion with uniformly hypodense contents and no obvious solid component, suggestive of a Rathke's cleft cyst; at operation biopsy of the wall was consistent with a craniopharyngioma. 2B also shows a large cystic lesion with heterogeneous contents, bright on T1 with and without contrast and a thickened enhancing wall, suggestive of a craniopharyngioma; biopsy of the lining showed this to be a Rathke's cyst. 2C–D: Malignancies masquerading as adenomas. 2C shows an MRI read initially as showing a macroadenoma with sphenoid sinusitis; at operation it proved to be a poorly differentiated carcinoma of lung origin. 2D shows an MRI initially read as showing a macroadenoma; at operation initial pathology was read as an adenoma with dense fibrosis; upon recurrence it was found to have de-differentiated into a malignant primary fibrosarcoma of the sella.
Malignancies were generally widely invasive. The preoperative radiographic differential diagnosis in cases of malignancies did usually include malignant tumors (either primary or metastatic). In four cases cases, however, (fibrosarcoma, osteosarcoma, squamous carcinoma and lung metastasis) the malignancy was not expected on the basis of pre-operative imaging. Some of these (e.g., fibrosarcoma, lung metastasis) had the radiographic appearance of pituitary adenomas (Figure 2, C–D). In particular, the fibrosarcoma appeared as a mass expanding the sella with a suprasellar component which elevated the optic chiasm. Even in retrospect, the radiographic appearance is non-diagnostic.
The squamous carcinoma of the clivus and the sellar osteosarcoma also were radiographically misdiagnosed. The squamous carcinoma of the clivus appeared as an expansile lesion involving the clivus, extending through the posterior wall of the sphenoid sinuses bilaterally and eroding the sella. The lesion was partially enhancing and appeared bright on T2 with partial cystic contents. These features were thought suggestive of chordoma or metastasis, so a malignancy was suspected, although not a primary sinus tumor. The sellar osteosarcoma extended into the right cavernous sinus and sphenoid sinus causing an intrasphenoidal hemorrhage. Its appearance was thought to resemble a subacute pituitary apoplexy with hemorrhage.
The two chondrosarcomas were extremely invasive. One of them appeaared as an extensive skull base lesion involving most of the clivus, petrous medially, and extending into the sphenoid and posterior nasopharynx; there also was early brainstem compression. The other chondrosarcoma appeared as a mass centered in the sphenoid sinus, with anterior extension to the ethmoid air cells. The SNUC appeared on MRI as a 2 cm mass involving the sphenoid sinus, invading the sella and the left cavernous sinus. The invasiveness and the radiographic characteristics were consistent with intrinsic sinus or bony tumor, or a metastasis.
The inflammatory lesions, especially hypophysitis, were characterized by homogeneous enhancement indistinct from the normal gland, as opposed to extrinsic compressive lesions. The cases of lymphocytic hypophysitis appeared as enlarging masses indistinct from the gland. The case of granulomatous hypophysitis appeared as a 2 cm sellar mass which was indistinct from the gland and had homogenous enhancement. The radiographic diagnosis was consistent with meningioma, hypophysitis or, les likely, metastasis. Initial radiographic evaluation of the case of neurosarcoidosis was consistent with pituitary macroadenoma, in that it appeared as a 1.6 cm enhancing mass involving the pituitary, although involvement of the infundibulum was also noted.
Outcome
Mean follow-up was 42±34 months (range: 0–132). Longer duration of follow-up was available in patients with benign tumors compared to those with inflammatory lesions or cysts (p<0.05 and p<0.01 respectively) (Table 3).
To assess outcome, patients were divided into two groups based on whether the purpose of the intervention was diagnostic or therapeutic. In general, only a biopsy or subtotal resection was performed for invasive lesions. Rathke's cleft cysts and arachnoid cysts were drained or fenestrated, while a total removal was attempted in most cases of encapsulated tumors.
Surgery for diagnosis
A limited biopsy for diagnosis was performed in 25 lesions (Figure 1), when either the tumor was invasive and unresectable, or resection was not indicated: all ten patients with inflammatory lesions, four invasive metastases, four meningiomas, two clival chondrosarcomas, two germinomas, one clivus hemangioma, one sino-nasal undifferentiated carcinoma, and one clivus osteogenic sarcoma. No patient with an inflammatory/ infectious lesion underwent further surgery after the initial biopsy. The four patients with invasive metastases were treated with focused radiation and/or chemotherapy. The sellar lesion in the patient with metastatic prostate carcinoma appeared stable at last follow-up. The patients with metastases from the pancreatic islet cell carcinoma and renal cell carcinoma died despite treatment. The other patient with metastasis was lost to follow-up.
The two patients with germinomas underwent stereotactic radiotherapy to the tumor bed plus fractionated radiotherapy to the neuraxis; both remain in remission. The cases of chondrosarcoma and invasive menigiomas had radiotherapy after the biopsy and appear stable with limited follow-up. The patient with SNUC underwent radiotherapy after the biopsy, but had rapid progression of the disease. The patient with osteogenic sarcoma was postoperatively treated with chemotherapy, but lost to follow-up.
Surgery with therapeutic intent
TSS as primary therapy was performed in all 62 cystic lesions (Figure 1), and for the 19 craniopharyngiomas (all predominantly cystic), five clivus chordomas, inverted papilloma, ependymoma, fibrosarcoma, metastasis from lung carcinoma and the squamous carcinoma.
Cysts
A post-drainage remnant of the cyst wall was detected radiographically in 14/61 (23%) cysts with data available. Radiographic progression was seen in 40% of the 10 with further data available, but only 2 required re-operation (2/10, 20%) after a mean of 30±24 months. Forty-seven patients with a cyst had no post-drainage residual on the postoperative MRI. Fifteen (32%) had a radiographic recurrence over time, and 4/15 (27%) required reoperation after a mean of 23±26 months (median: 15 months). All 6 patients requiring a re-operation had a Rathke's cyst. Four recurred once, one recurred twice, and one recurred four times.
Cystic Craniopharyngiomas
Nineteen patients with cystic craniopharyngiomas had drainage and/or attempted resection (Figure 1). In 14/18 (78%) patients with follow-up data available, there was residual enhancement of the cyst wall on MRI post-operatively; in 7/14 (50%) there was enlargement of the residual cyst on follow-up. Four out of eighteen patients (22%) with craniopharyngiomas had no obvious tumor seen on MRI after the first TSS, suggestive of complete resection. Two of them (50%) experienced a recurrence. Overall 7/18 (39%) patients required reoperation for cyst recurrence. Fifteen patients with a craniopharyngioma underwent post-operative radiotherapy at our institution and two patients had already received radiotherapy elsewhere.
Sellar ependymoma
Patient with this lesion had transsphenoidal debulking; a craniotomy was recommended, but he chose to be followed without progression.
Clivus Chordomas
Four of the 5 clivus chordomas had follow-up data available. Two of them underwent radiotherapy without progression. One had gross total resection and has been followed without recurrence. One refused postoperative radiotherapy and has been followed without progression.
Other Malignancies
The patient with the inverted papilloma had radiotherapy on the residual with no sign of recurrence at last follow-up. The patients with the primary fibrosarcoma, invasive squamous cell carcinoma and metatstatic lung carcinoma all died despite a combination of radiation and chemotherapy.
Postoperative resolution of symptoms
Twenty-five of 40 (63%) patients who presented with headache reported postoperative resolution. Headache resolved in 21/29 (72%) patients with cysts, 3/6 (50%) of those with benign neoplasms, and in one patients with malignancies. Five of 8 patients with persistent headache in the group CYS had a Rathke's cyst extending to the suprasellar region. Seventeen patients of 26 (65%) who complained of blurred vision before TSS reported improvement: 12/15 in those with cysts (80%) and 5/7 (71%) those with benign tumors.
Alteration in pituitary function after TSS
Postoperative pituitary function is shown in Table 3. Five patients had hypopituitarism on the basis of previous treatment; these patients were excluded from the analysis. Of 64 preoperative endocrine abnormalities, 23 had recovered after TSS (34%). Of these 23, 17 were cases of hyperprolactinemia (77%), three of hypogonadism (14%), two of central hypothyroidism (9%) and one of hypocortisolism.
Twelve new cases of endocrine dysfunction occurred after TSS (12/116; 10%) (Table 3). When the four major etiologic groups were analyzed separately, the difference in new post-operative endocrine dysfunction was not significant.
DISCUSSION
This study is the largest description of TSS for sellar masses other than pituitary adenomas published to date. We have shown that, of 1469 transsphenoidal procedures performed in our Center between 1998–2009 for masses in the sellar/parasellar region, 116 (7.9%) were not pituitary adenomas. Overall, 53% of the masses were cysts; 22% were benign neoplasms, 16% malignant neoplasms, and 9% were inflammatory lesions. Rathke's cysts, the most common lesions, represented 42% of all cases. Twenty-six percent of malignant lesions were metastases. Of note, some of the malignancies (e.g., fibrosarcoma, lung metastasis) had the radiographic appearance of pituitary adenomas. Freda described 83 non-pituitary masses of 911 TSS performed between 1981–1996. Our results agree with the spectrum of diagnoses reported in that series. They found that Rathke's cysts represented the most common lesion, at 28%, followed by craniopharyngiomas (14%), metastases (12%), chordomas (11%), and meningiomas (10%); inflammatory lesions represented 8% overall (5). Our study characterizes the presenting symptoms and signs, discusses the radiographic features, and reports surgical outcome in terms of clinical improvement, relapse rate, and adjunctive treatment. It is valuable to compare these series reported over a decade apart, as well as others that address some of the specific pathologies.
Symptoms and signs at presentation
Headache
Headache was the most common presenting complaint, seen in 34% of cases overall and in 47% of patients with cystic lesions. In another study, headache also was the most common non-endocrine preoperative symptom in patients with cystic lesions, reported by 65% of patients with a Rathke's cyst and 60% of those with an arachnoid cyst (6). Headache was the most frequent non-endocrine symptom in patients with inflammatory lesions in our cohort, as well as in another large series (15).
Visual symptoms
Visual problems were reported by 22% of all patients. Fifty percent of the formal visual field examinations showed some degree of impairment; but this study would have been requested in patients with likely deficits. Freda et al. reported that visual field problems were the most common complaints in their series (5). Mejico et al. showed that patients with pituitary adenomas were 3.8 times more likely to complain of any visual disturbance than those with non-adenomatous lesions (9).
Visual field impairment and cranial neuropathy were the most frequent preoperative findings in patients with malignant tumors (67% and 47%, respectively), and VIth nerve palsies were seen only in this group. Branch found that visual field defects and extraocular nerve palsies were present in 50% and 43%, respectively, of 14 patients with metastases (10). Aaberg documented cranial neuropathy in 42% of patients with metastatic lesions compared to fewer than 5% of those with pituitary adenomas (11). In the present study, visual field impairment and visual loss were also the most frequent non-endocrine symptoms in the group with benign neoplasms. Visual compromise was also the most common complaint in two other large series of patients with craniopharyngiomas (12–13).
Visual field defects and decreased visual acuity were common preoperative complaints in patients with cystic lesions, reported in 39% and 24%, respectively. A previous study of patients with symptomatic Rathke's cysts also documented visual field defects and headache as the most prevalent complaints (51.7% and 49%, respectively) (14). Although Freda et al. did not detail symptoms for each diagnosis, they observed that visual compromise was one of the most common findings in patients with Rathke's cysts (5). None of the patients with inflammatory lesions in our series presented with visual problems, although other studies have reported that these symptoms are not uncommon (15).
Post-operative improvements
In our series, post-surgical resolution of headache occurred in many patients (63%), the majority of whom had cystic lesions. Cyst decompression was also associated with post-surgical resolution of visual complaints in 80% of patients. Shin showed that headache and ophthalmological problems resolved in 82% and 70% of Rathke's cysts, respectively (6). In our group with benign tumors, primarily craniopharyngiomas, resolution of visual symptoms was observed in 71% of cases. Previous reports have noted visual improvement after transsphenoidal decompression of craniopharyngiomas in 47% to 94% of cases; significantly higher than after a transcranial approach, although the anatomy necessitating a craniotomy may be quite different (6, 13, 16–17).
Endocrine dysfunction
Hyperprolactinemia was the most frequent preoperative endocrine dysfunction, described in 34% of those patients who presented with hormone abnormalities, most commonly in those with cystic lesions (26%). Shin found that hyperprolactinemia was the most common hormone dysfunction at presentation in patients with Rathke's cysts (46%) (6). In our study, no difference was observed in the prevalence of any specific hormone dysfunction between the four groups, suggesting that assessment of hormone dysfunction does not assist with the differential diagnosis.
Comparison can be made with series that report specific endocrine outcomes by diagnosis. In our series, hyperprolactinemia resolved in 72% of patients. Voelker et al. documented resolution of hyperprolactinemia in 70% of patients with Rathke's cysts (14). Honegger et al. showed that pituitary function did not change significantly after surgery for craniopharyngiomas, with the exception of hyperprolactinemia, which improved in 16/19 patients with this preoperative abnormality (12).
Preoperative diabetes insipidus (DI) has been advocated as an important finding in patients with pituitary metastases, with a prevalence between 28% and 70% (10, 18). Although our series includes only five patients with metastases, one did present with DI. Post-surgical DI has a variable incidence, depending on tumor location in relation to the stalk and the posterior pituitary (19). Transient DI was documented in 7% of patients, whereas permanent DI or transient hyponatremia each occurred in 2% of patients, consistent with previous reports mainly focusing on pituitary adenomas (19–22). Other studies have shown a relatively high incidence of DI after surgery for Rathke's cleft cysts and craniopharyngiomas (6, 12–13, 22); the incidence of postoperative DI may depend upon whether the cyst was drained or excised (23). Nemergut reported a 9.7% incidence of permanent DI after resection of Rathke's cysts (22). Benveniste et al. reported a 6% incidence of permanent DI following decompression and biopsy of Rathke's cysts, which was significantly lower than the 67% incidence observed after resection (23). In our series, new postoperative permanent DI was only observed in one patient with an arachnoid cyst and in two patients with malignancies, for an overall incidence of <3%.
Recurrence
Twenty-nine percent of Rathke's cysts showed radiographic evidence of recurrence after the first intervention, although only 13% required re-operation. Early case reports with a limited number of subjects with Rathke's cysts described a recurrence rate of 5–10% (14, 24–25). In contrast, later studies have suggested that Rathke's cysts may relapse more frequently than previously assumed (5–6, 26). Mukherjee et al. found that 4/12 (33%) patients with a Rathke's cyst recurred and three required re-exploration (26). This discrepancy may be partly explained by small sample sizes, by differences in the definition of “relapse,” or by differences in surgical technique, i.e., drainage vs. excision. For instance, Shin found that 19% of Rathke's cysts recurred radiographically, where definite lesions were visualized by postoperative imaging, but the number requiring re-exploration was not specified (6). This paper also described the overlap in pathological characteristics between craniopharyngiomas and Rathke's cysts which may have both similar contents and epithelial lining. Since a number of our patients with Rathke's cysts were diagnosed on the basis of cyst contents only, it is possible that we have underestimated the number of craniopharyngiomas, which may have an increased rate of recurrence.
Freda et al., however, focused only on lesions requiring reoperation, and reported a 13% recurrence rate (5). It has been suggested that the recurrence rate of Rathke's cysts may depend in part upon the histological characteristics of the cyst wall and contents (27–28), the presence of stratified squamous epithelium (26), or with chronic inflammation, macrophages, cholesterol clefts and hemosiderin (6). Inflammatory infiltrate has been hypothesized to be an important marker of early recurrence in Rathke's cysts; it may perhaps promote fluid re-accumulation (23). Although we identified no histological predictor of relapse, it remains possible that pathological characteristics are associated with recurrence risk (23, 29).
Imaging
Imaging helped formulate presumptive preoperative diagnoses and, in most cases, the radiographic features were consistent with final pathologic diagnosis. Rathke's cysts may have a variable imaging appearance depending on the nature of the cyst contents, making the differential diagnosis between cystic adenomas and craniopharyngiomas challenging in some cases, as shown in Figure 2 (14, 30). Although most Rathke's cysts in this series had low T1 signal on MRI as expected, 24% were hyperintense. Fourteen percent of them showed slight post-contrast enhancement, previously reported as a rare occurrence (30).
We observed other cases of equivocal imaging. Two of four meningiomas were partly intrasellar and hypointense on T1 with diffuse enhancement on MRI, mimicking a pituitary adenoma as previously described by others (31).
Inflammatory lesions, such as lymphocytic hypophysitis or neurosarcoidosis, do not always present with typical radiographic features (30). In our series, a case of lymphocytic hypophysitis resembled a Rathke's cyst, and imaging of neurosarcoidosis was consistent with a macroadenoma. As shown in Figure 2, a macroadenoma was also suspected in cases of the fibrosarcoma, lung metastasis and ependymoma, whereas the osteosarcoma mimicked pituitary apoplexy and the squamous carcinoma of the clivus appeared as a chordoma or metastasis.
Conclusion
Approximately 8% of surgically-treated sellar masses from our Center over the past decade were not pituitary adenomas. Headache and visual symptoms as well as pituitary dysfunction were commonly associated with these masses, and these abnormalities often resolved postoperatively. Hyperprolactinemia was the most frequent endocrine alteration at clinical presentation; it recovered in most patients after surgery.
Typical radiographic characteristics for each etiologic group were usually present, but it is important to recognize that preoperative imaging may be misleading, despite significant improvement in imaging quality over the years. Given the relatively high incidence of these non-pituitary lesions, it is important for all clinicians involved in the evaluation of these patients to consider a broad differential diagnosis.
Acknowledgement
This work was supported in part by the following grant: ULI RR0257801
We appreciate statistical advice provided by Douglas Hayden of the Biostatistics Center, Massachusetts General Hospital and Harvard Medical School.
Abbreviations
- TSS
transsphenoidal surgery
- MAL
malignancies
- BEN
benign lesions
- CYS
cystic lesions
- INF
inflammatory lesions
Footnotes
The authors have nothing to declare.
References
- 1.Laws ER., Jr. Pituitary surgery. Endocrinology and Metabolism Clinics of North America. 1987;16:647–665. [PubMed] [Google Scholar]
- 2.Ciric I, Ragin A, Baumgartner C, Pierce D. Complications of transsphenoidal surgery: results of a national survey, review of the literature, and personal experience. Neurosurgery. 1997;40:225–236. doi: 10.1097/00006123-199702000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Barker FG, Klibanski A, Swearingen B. Transsphenoidal surgery for pituitary tumors in the United States, 1996–2000: mortality, morbidity, and the effects of hospital and surgeon volume. Journal of Clinical Endocrinology and Metabolism. 2003;88:4709–4719. doi: 10.1210/jc.2003-030461. [DOI] [PubMed] [Google Scholar]
- 4.Jagannathan J, Kanter AS, Sheedan JP, Jane JA, Jr., Laws ER., Jr. Benign brain tumors: sellar/parasellar tumors. Neurologic Clinics. 2007;25:1231–1249. doi: 10.1016/j.ncl.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Freda PU, Wardlaw SL, Post KD. Unusual causes of sellar/parasellar masses in a large transsphenoidal surgical series. Journal of Clinical Endocrinology and Metabolism. 1996;81:3455–3459. doi: 10.1210/jcem.81.10.8855784. [DOI] [PubMed] [Google Scholar]
- 6.Shin JL, Asa SL, Woodhouse LJ, Smyth HS, Ezzat S. Cystic lesions of the pituitary: clinicopathological features distinguishing craniopharyngioma, Rathke's cleft cyst, and arachnoid cyst. Journal of Clinical Endocrinology and Metabolism. 1999;84:3972–3982. doi: 10.1210/jcem.84.11.6114. [DOI] [PubMed] [Google Scholar]
- 7.Vance ML. Perioperative management of patients undergoing pituitary surgery. Endocrinology and Metabolism Clinics of North America. 2003;32:355–365. doi: 10.1016/s0889-8529(03)00003-3. [DOI] [PubMed] [Google Scholar]
- 8.Scheithauer BW, Swearingen B, Whyte ET, Auluck PK, Stemmer-Rachamimov AO. Ependymoma of the sella turcica: a variant of pituicytoma. Hum Pathol. 2009;40:435–440. doi: 10.1016/j.humpath.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Mejico LJ, Miller NR, Dong LM. Clinical features associated with lesions other than pituitary adenoma in patients with an optic chiasmal syndrome. American Journal Ophthalmology. 2004;137:908–913. doi: 10.1016/j.ajo.2003.12.038. [DOI] [PubMed] [Google Scholar]
- 10.Branch CL, Laws ER., Jr. Metastatic tumors of the sella turcica masquerading as primary pituitary tumors. Journal of Clinical Endocrinology and Metabolism. 1987;65:469–474. doi: 10.1210/jcem-65-3-469. [DOI] [PubMed] [Google Scholar]
- 11.Aaberg TM, Jr, Kay M, Sternau L. Metastatic tumors to the pituitary. American Journal of Ophthalmology. 1995;119:779–785. doi: 10.1016/s0002-9394(14)72785-0. [DOI] [PubMed] [Google Scholar]
- 12.Honegger J, Buchfelder M, Fahlbusch R. Surgical treatment of craniopharyngiomas: endocrinological results. Journal of Neurosurgery. 1999;90:251–257. doi: 10.3171/jns.1999.90.2.0251. [DOI] [PubMed] [Google Scholar]
- 13.Chakrabarti I, Amar AP, Couldwell W, Weiss MH. Long-term neurological, visual, and endocrine outcomes following transnasal resection of craniopharyngioma. Journal of Neurosurgery. 2005;102:650–657. doi: 10.3171/jns.2005.102.4.0650. [DOI] [PubMed] [Google Scholar]
- 14.Voelker JL, Campbell RL, Muller J. Clinical, radiographic, and pathological features of symptomatic Rathke's cleft cysts. Journal of Neurosurgery. 1991;74:535–544. doi: 10.3171/jns.1991.74.4.0535. [DOI] [PubMed] [Google Scholar]
- 15.Beressi N, Beressi JP, Cohen R, Modigliani E. Lymphocytic hypophysitis. A review of 145 cases. Annales de Medecine Interne (Paris) 1999;150:327–341. [PubMed] [Google Scholar]
- 16.Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M. Surgical treatment of craniopharyngiomas: experience with 168 patients. Journal of Neurosurgery. 1999;90:237–250. doi: 10.3171/jns.1999.90.2.0237. [DOI] [PubMed] [Google Scholar]
- 17.Van Effenterre R, Boch AL. Craniopharyngiomas in adults and children: a study of 122 surgical cases. Journal of Neurosurgery. 2002;97:3–11. doi: 10.3171/jns.2002.97.1.0003. [DOI] [PubMed] [Google Scholar]
- 18.McCormick PC, Post KD, Kandji AG, Hays AP. Metastatic carcinoma to the pituitary gland. British Journal of Neurosurgery. 1989;3:71–80. doi: 10.3109/02688698909001028. [DOI] [PubMed] [Google Scholar]
- 19.Olson BR, Gumowski J, Rubino D, Oldfield EH. Pathophysiology of hyponatremia after transsphenoidal pituitary surgery. Journal of Neurosurgery. 1997;8:499–507. doi: 10.3171/jns.1997.87.4.0499. [DOI] [PubMed] [Google Scholar]
- 20.Hensen J, Henig A, Fahlbusch R, Meyer M, Boehnert M, Buchfelder M. Prevalence, predictors, and patterns of postoperative polyuria and hyponatraemia in the immediate course after transsphenoidal surgery for pituitary adenomas. Clinical Endocrinology. 1999;50:431–439. doi: 10.1046/j.1365-2265.1999.00666.x. [DOI] [PubMed] [Google Scholar]
- 21.Taylor SL, Tyrrell JB, Wilson CB. Delayed onset of hyponatremia after transsphenoidal surgery for pituitary adenomas. Neurosurgery. 1995;37:649–654. doi: 10.1227/00006123-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 22.Nemergut EC, Zuo Z, Jane JA, Jr, Laws ER., Jr. Predictors of diabetes insipidus after transsphenoidal surgery: a review of 881 patients. Journal of Neurosurgery. 2005;103:448–454. doi: 10.3171/jns.2005.103.3.0448. [DOI] [PubMed] [Google Scholar]
- 23.Benveniste RJ, King WA, Walsh J, Lee JS, Naidich TP, Post KD. Surgery of Rathke's cleft cysts: technical considerations and outcomes. Journal of Neurosurgery. 2004;101:577–584. doi: 10.3171/jns.2004.101.4.0577. [DOI] [PubMed] [Google Scholar]
- 24.Raskind R, Brown HA, Mathis J. Recurrent cyst of the pituitary: 26-year follow-up from first decompression. Journal of Neurosurgery. 1968;28:595–599. doi: 10.3171/jns.1968.28.6.0595. [DOI] [PubMed] [Google Scholar]
- 25.Marcincin RP, Gennarelli TA. Recurrence of symptomatic pituitary cysts following transsphenoidal drainage. Surgical Neurology. 1982;30:197–203. doi: 10.1016/0090-3019(82)90184-7. [DOI] [PubMed] [Google Scholar]
- 26.Mukherjee JJ, Islam N, Kaltsas G, Lowe DG, Charlesworth M, Afshar F, Trainer PJ, Monson JP, Besser GM, Grossman AB. Clinical, radiographic, and pathological features of patients with Rathke's cleft cysts: tumors that may recur. Journal of Clinical Endocrinology and Metabolism. 1997;82:2357–2362. doi: 10.1210/jcem.82.7.4043. [DOI] [PubMed] [Google Scholar]
- 27.Matsushima T, Fukui M, Ohta M, Yamakawa Y, Takaki T, Okano H. Ciliated and goblet cells in craniopharyngioma. Light and electron microscopic studies at surgery and autopsy. Acta Neuropathology (Berlin) 1980;50:199–205. doi: 10.1007/BF00688754. [DOI] [PubMed] [Google Scholar]
- 28.Fager CA, Carter H. Intrasellar epithelial cysts. Journal of Neurosurgery. 1966;24:77–81. doi: 10.3171/jns.1966.24.1.0077. [DOI] [PubMed] [Google Scholar]
- 29.Kim JE, Kim JH, Kim OL, Paek SH, Kim DG, Chi JG, Jung HW. Surgical treatment of symptomatic Rathke's cleft cysts: clinical features and results with special attention to recurrence. Journal of Neurosurgery. 2004;100:33–40. doi: 10.3171/jns.2004.100.1.0033. [DOI] [PubMed] [Google Scholar]
- 30.Fitzpatrick M, Tartaglino LM, Hollander MD, Zimmerman LA, Flanders AE. Imaging of sellar and parasellar pathology. Radiologic Clinics of North America. 1999;37:101–121. doi: 10.1016/s0033-8389(05)70081-6. [DOI] [PubMed] [Google Scholar]
- 31.Nozaki K, Nagata I, Yoshida K, Kikuchi H. Intrasellar meningioma: case report and review of the literature. Surgical Neurology. 1997;47:477–452. doi: 10.1016/s0090-3019(96)00244-3. [DOI] [PubMed] [Google Scholar]