Abstract
Objective
Anterior cervical corpectomy with fusion (ACF) or laminoplasty may be associated with substantial number of complications for treating multilevel cervical ossification of the posterior longitudinal ligament (OPLL) with significant cord compression. For more safe decompression and stabilization in multilevel cervical OPLL with prominent cord compression, we propose circumferential cervical surgery (selective ACF and laminoplasty) based on our favorable experience.
Methods
Twelve patients with cervical myelopathy underwent circumferential cervical surgery and all patients showed multilevel OPLL with signal change of the spinal cord on magnetic resonance imaging (MRI). A retrospective review of clinical, radiological, and surgical data was conducted.
Results
There were 9 men and 3 women with mean age of 56.7 years and a mean follow up period of 15.6 months. The average corpectomy level was 1.16 and laminoplasty level was 4.58. The average Japanese Orthopedic Association score for recovery was 5.1 points and good clinical results were obtained in 11 patients (92%) (p < 0.05). The average space available for the cord improved from 58.2% to 87.9% and the average Cobb's angle changed from 7.63 to 12.27 at 6 months after operation without failure of fusion (p < 0.05). Average operation time was 8.36 hours, with an estimated blood loss of 760 mL and duration of bed rest of 2.0 days. There were no incidences of significant surgical complications, including wound infection.
Conclusion
Although the current study examined a small sample with relatively short-term follow-up periods, our study results demonstrate that circumferential cervical surgery is considered favorable for safety and effectiveness in multilevel OPLL with prominent cord compression.
Keywords: Ossification of the posterior longitudinal ligament, Anterior cervical corpectomy with fusion, Laminoplasty, Japanese Orthopedic Association score
INTRODUCTION
Most patients with cervical ossification of the posterior longitudinal ligament (OPLL) are asymptomatic; however, patients with severe spinal cord compression may be predisposed to symptoms of cervical radiculopathy or myelopathy15). Surgical treatment is advised for patients with severe symptoms or signs of growth activity of OPLL.
The surgical treatments of cervical OPLL includes anterior cervical corpectomy with fusion (ACF) and posterior decompression such as laminoplasty or laminectomy. However, the appropriate surgical approach for treating multilevel cervical OPLL with significant cord compression remains controversial given that the indication of each surgical technique has unique advantages and disadvantages.
Recently, circumferential cervical surgery (selective ACF and laminoplasty) has been performed for more safe decompression and stabilization in patients of multilevel cervical OPLL with significant cord compression. We reviewed our experience of single stage circumferential cervical surgery, over the past four years, in twelve patients with multilevel cervical OPLL with signal change of the spinal cord on MRI due to significant cord compression, considering clinical, radiological, and surgical aspects.
MATERIALS AND METHODS
Population
From September 2005 to April 2008, a total of 12 patients of multilevel cervical OPLL with the spinal cord ischemia on MRI underwent single stage circumferential cervical surgery. The average age of the patients was 56.7 years (range, 50-66). Nine patients were male (75%) and 3 were female (25%). The average symptom duration was 8.0 months (range, 1-36), and the average follow-up period after surgery was 15.6 months (range, 6-41).
Indication
The indications for single stage circumferential cervical surgery in our study include multilevel OPLL with prominent cord compression resulting signal change in the spinal cord on cervical MRI and severe neurological symptoms (the ratio of SAC is less than 60%), with/without loss of cervical lordosis. The multilevel OPLL means that the involved vertebral body levels are 3 or more levels on cervical computed tomography (CT) and the prominent cord compression means that the ratio of space available for the cord (SAC) is less than 60% of spinal canal diameter with mushroom- or hill-shaped OPLL.
Procedure
The first procedure was posterior expansive open door laminoplasty using the Hyrabayashi technique with titanium miniplates. This technique requires a pneumatic high-speed burr to create a gutter at the junction of the lamina and medial aspect of the lateral mass through the outer cancellous bone. The cancellous bone on the "opening" side of the laminoplasty was then removed, and the inner cortex was thinned. Using a 1- or 2-mm Kerrison rongeur, transaction of the lamina and ligamentum flavum was performed. A "greenstick osteotomy" was performed by carefully displacing the spinous processes toward the closing osteotomy side and elevating the opening side of the lamina with a nerve hook. Stabilization of each level was then performed using a titanium miniplate.
Secondly, selective ACF with plate-and-screw system was performed. The patient was placed in a supine position with the head slightly extended, and an oblique skin incision was made along the anterior border of the sternocleidomastoid muscle. After all necessary discectomy procedures were carried out, the selective corpectomy was performed in the most severe vertebral body (1-2 level), using a pneumatic high-speed drill under a microscope. Then, the ossified posterior longitudinal ligament was removed completely to decompress the spinal cord. After confirming the anterior protrusion of the thecal sac and good pulsation, an appropriate length of mesh with an allograft bone fragment was inserted inlay fashion. A constrained plate-and-screw system of the appropriate length was used to achieve anterior cervical fixation. After surgery, a Philadelphia brace was worn around the neck of patients for several weeks in order to induce cervical fusion.
Outcome parameters
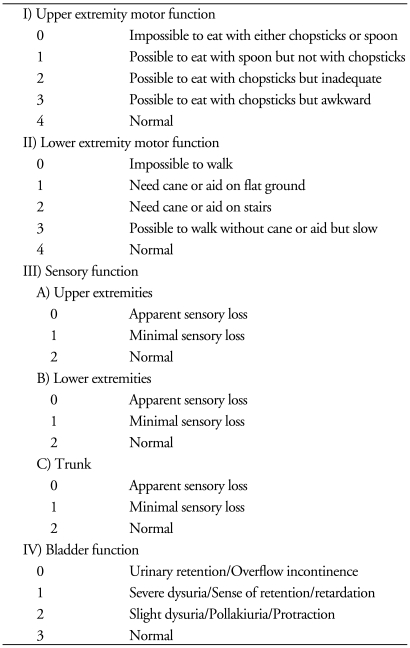
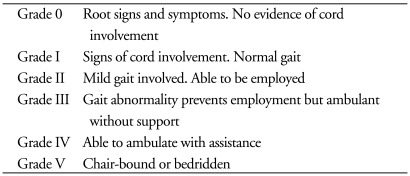
The clinical outcomes were assessed using the Japanese Orthopedic Association (JOA) scoring system (Table 1), Nurick's grade (Table 2), and Odom's criteria (Table 3) at the preoperative period, as well as at one month after operation and the last follow-up.
Table 1.
Japanese Orthopedic Association (JOA) scoring system
Table 2.
Nurick's classification of disability
Table 3.
Odom's criteria
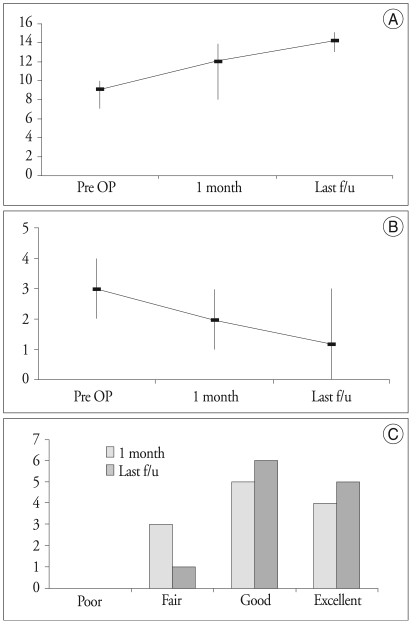
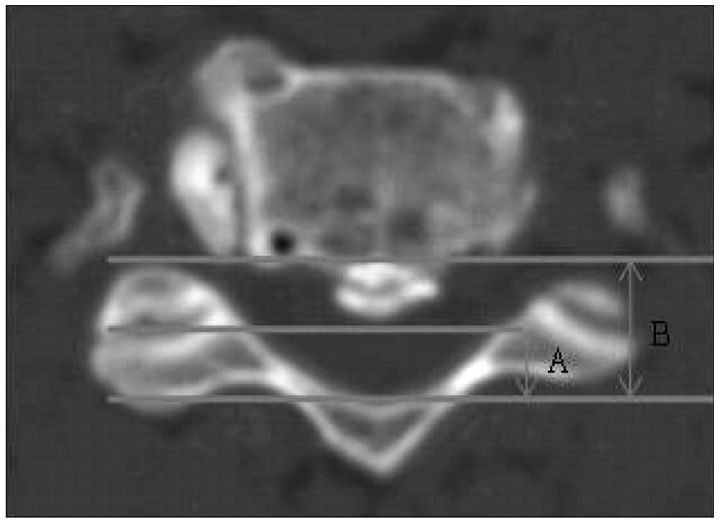
We examined the cervical MRI, cervical CT, dynamic X-rays prior to surgery, cervical CT after surgery, and follow-up dynamic X-rays during follow-up period. We evaluated the spinal canal diameter and the ratio of SAC using preoperative and postoperative cervical CT (Fig. 1). Also Cobb's angle was used to evaluate lordosis of the cervical spine using lateral X-rays on neutral position at preoperative period and the last follow-up (Fig. 2).
Fig. 1.
The ratio of the SAC is calculated as the ratio of SAC to the anteroposterior diameter of the spinal canal at the corresponding level on a cervical computed tomography. A : SAC. B : Anteroposterior diameter of the spinal canal. The ratio of SAC = A/B×100 (%).
Fig. 2.

Cobb's angle, for evaluation of cervical lordosis, is measured between intersecting lines drawn perpendicular to the bottom of the C2 vertebra and the bottom of the C7 or C6 vertebra in lateral view.
Surgical morbidities were evaluated by checking estimated blood loss (EBL), operation time, duration of postoperative bed rest, and operative complications such as neurologic deterioration, cerebrospinal fluid (CSF) leakage and wound infection.
RESULTS
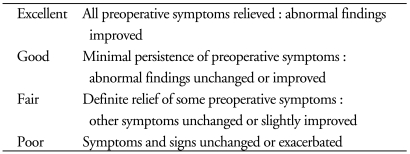
There were signal changes in the spinal cord on cervical MRI in all patients. With respect to OPLL shape, it was hill-shaped in 8 patients and mushroom-shaped in 4 patients. The mean OPLL level was 4.00 (range, 3-5), the mean corpectomy level was 1.16 (range, 1-2) and the mean laminoplasty level was 4.58 (range, 4-5) (Table 4).
Table 4.
Patient data
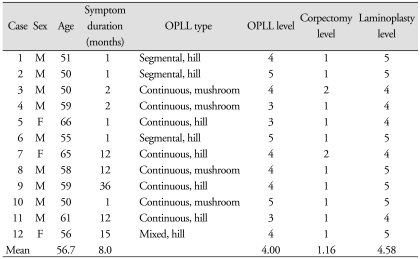
Clinical outcomes
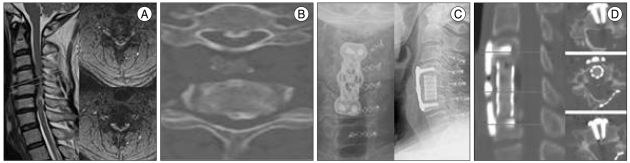
The mean preoperative JOA score was 9.1 (range, 7-10) which increased to 12.0 (range, 8-14) at the 1-month follow-up and further to 14.2 (range, 13-15) at the last follow-up (Fig. 3A). Nurick's grade also improved from 3.0 (range, 2-4) at pre-operation to 2.0 (range, 1-3) at the 1-month follow-up and 1.18 (range, 0-3) at the last follow-up (Fig. 3B). Both JOA score and Nurick's grade improved after the surgery and the improvement maintained during the follow-up period in all patients with statistical significance (p < 0.05, t-test).
Fig. 3.
Graphs showing JOA score (A), Nurick's grade (B) and Odom's criteria (C) before the surgery and during the follow-up. The improvement at 1 month and last follow-up are statistically significant compared with the preoperative values (p < 0.05, t-test). A : The mean JOA score recovery from pre-operation (pre OP) to last follow-up (f/u) was 5.1 points (from 9.1 to 14.2). B : The mean Nurick's grade recovery from pre-operation (pre OP) to last follow-up (f/u) was 1.82 (from 3.0 to 1.18). C : Cinical success rate according to Odom's criteria was increased from 75% to 91.6% through follow-up periods.
According to Odom's criteria, the results were excellent in 4 patients (33.3%), good in 5 patients (41.7%), and fair in 3 patients (25%) at the 1-month follow-up, and excellent in 5 patients (41.7%), good in 6 patients (50%), and fair in 1 patient (8.3%) at the last follow-up. Therefore, the clinical success rate according to Odom's criteria was 91.6% (Fig. 3C).
Radiological outcomes
The mean spinal canal diameter increased from 11.66 mm (range, 9.15-13.60) at pre-operation to 17.60 mm (range, 15.71-19.92) at post-operation. Additionally, the mean ratio of SAC of the corpectomy level improved from 58.2% (range, 44.1-60.0) to 87.9% (range, 80.1-100). The mean Cobb's angle increased from 7.63° (range, 5.15-9.60) at preoperation to 12.27° (range, 8.63-23.57) at the last follow-up. The improvement was statistically significant in both ratio of SAC and cervical lordotic angle (p < 0.05, t-test).
There was no case of cervical instability, instrument breakdown, or fusion failure during follow-up period (Fig. 4, 5).
Fig. 4.
A 65-year-old woman presented with gait disturbance 12 months ago. A : Pre-operative cervical MRI demonstrates severe spinal cord compression at C4, 5, 6, 7 levels with high signal change on T2-weighted imaging. B : Pre-operative C-CT shows continuous and hill-shaped OPLL in C5, 6 levels with 60% (7.7/12.8mm) of SAC. C : Laminoplasty C4, 5, 6, 7, corpectomy C5, 6, anterior cervical interbody fusion C4-7 and anterior cervical plate fixation C4-7 are done. D : Postoperative cervical CT shows increased SAC from 60% to 100%.
Fig. 5.
A 58-year-old man presented with motor weakness in both upper extremities 12 months ago. A : Pre-operative cervical MRI reveales severe spinal cord compression at C4, 5, 6, 7 levels with high signal change on T2-weighted imaging. B : Pre-operative cervical CT shows continuous and hill-shaped OPLL in C4, 5 levels with 44% (4.4/10.1 mm) of SAC. C : Laminoplasty C3, 4, 5, 6, 7, corpectomy C5, anterior cervical interbody fusion C4-6, and anterior cervical plate fixation C4-6 are done. D : Postoperative cervical CT shows increased SAC from 44% to 100%.
Surgical morbidity
The mean operation time was 8.36 hours (range : 6-10), EBL was 760 mL (range : 300-1,500), need of transfusion was 1.18 packs (range : 0-4), and duration of bed rest was 2.0 days (range : 1-5). Fortunately, there were no major surgical complications such as aggravation of neurological symptoms by cord injury, C5 nerve palsy, CSF leakage, wound infection, injury of adjacent organs, or hoarseness except for a single case of temporary pneumonia and temporary swallowing difficulty.
DISCUSSION
Controversy exists regarding the appropriate method of surgery in cases of cervical radiculomyelopathy due to cervical OPLL. The selection of a anterior or posterior decompression depends on numerous factors, including cervical alignment and contour, the number of vertebral segments involved in the stenosis, the type of OPLL, the cause of the spinal cord compression (ventral, dorsal, or combined spinal canal pathology), a patient's symptom and metabolic factors, and the surgeon's experience with various surgical techniques6,7,10,11,25). The most important factors in patient selection for a particular procedure are the clinical symptoms and the radiographic alignment of the spine. Appropriate patient selection maximizes the chance of optimal neurological outcome and minimizes complication18,29).
Since Robinson and Smith22), in 1955, first carried out the anterior approach, many reports have demonstrated the advantages and disadvantages of ACF with plate-and-screw system in cases of cervical OPLL. The anterior approach is favored because of the surgical effectiveness by direct removal and decompression of OPLL and the prevention of cervical instability due to cervical spinal realignment, reconstruction, internal fixation, and fusion8,16,29).
However, in cases of multilevel OPLL involving more than 3 levels, ACF is not satisfactory because of instrument failure, graft extrusion, pseudoarthrosis, subsidence, and fusion failure24). Vaccaro et al.27) reported that fusion failure was 9% in cases involving fewer than 2 levels and 50% in cases involving more than 3 levels. Further, Sasso et al.23) reported that fusion failure was 6% in those involving more than 2 levels and 71% in those involving more than 3 levels. Therefore, ACF is recommended in cases of OPLL involving fewer than 3 levels.
When adhesion between OPLL and dura mater is severe due to thick and mushroom- or hill-shaped OPLL, surgical complications such as iatrogenic cervical cord injury, CSF leakage due to tearing of dura mater, and massive bleeding, and occasionally, progression of cord compression and cord injury following insufficient removal of OPLL can occur4,8,14,16,19,25). Nakase et al.19), Mayr et al.17), Bazaz et al.1), and Ozgen et al.21) reported that the complication rate of ACF, including injury to the dura mater and spinal cord, CSF leakage, problem with instruments, and fusion failure, was 11-27%, and suggested that surgeons must take care to avoid such complication as the tearing of dura mater and cord contusion during ACF. Shim et al.24) suggested that the effectiveness of ACF may be not satisfactory in severe cases of cervical OPLL involving more than 50% of spinal canal diameter. Therefore, in multilevel cervical OPLL with prominent cord compression, the use of ACF alone may be insufficient and dangerous.
A posterior decompression is favored due to ease of surgical techniques, the efficacy in long segments, the ability to directly decompress the nerve root, the rare occurrences of complications such as cord injury, problems with instrument, and adjacent segment disease29). In particular, laminoplasty can be used to expand spinal canal with preservation of the posterior structure of the cervical spine.
However, by using the posterior approach, the effectiveness of surgery may be unsatisfactory due to the inability to directly remove the OPLL, which may be the major cause of neurological deficits. Progression of OPLL may aggravate a patient's symptoms, especially in cases of severe OPLL involving more than 50-60% of spinal canal diameter11,26,29). Ogawa et al.20) carried out laminoplasty in 72 patients, and they reported that 15.3% of patients complained of worsened symptoms, more than 2 points on the JOA score, and improvement of symptoms was 41% of patients during a 5-year follow-up period. Further, Kawaguchi et al.13) reported that 24% of patients complained of worsened symptom during a 10-year follow-up period, and Iwasaki et al.9) reported that improvement of symptoms was 60% in patients during a similar 10-year follow-up period. Moreover, Iwasaki et al.9), Chiba et al.3), and Kawaguchi et al.12) reported that progression of OPLL occurred in 70-73% of patients after laminoplasty.
The potential for the development of spinal instability or kyphosis is another disadvantage of the laminoplasty. Postoperative spinal instability or kyphosis can cause progressive myelopathy or radiculopathy such as C5 nerve root palsy, limitation of motion, and neck pain2,14,19,28,29). Motoki et al.10) carried out laminoplasty in 66 patients, and they reported that postoperative loss of cervical lordosis occured in 12 patients (18%). Yonenobu et al.30) reported that C5 nerve root palsy occurred in 13 of 384 patients, and Dai et al.5) reported that postoperative radiculopathy occurred in 37 of 287 patients (12.9%). Therefore, results of posterior decompression alone may be poor in cases of prominent cord compression and loss of cervical lordosis at pre-operation.
When OPLL involves the multilevel cervical spine with prominent cord compression resulting spinal cord ischemia on MRI with/without loss of cervical lordosis, ACF or laminoplasty alone procedure may cause a poor prognosis and some complications. If we carry out ACF only, we must also perform long level fusion, and then complications such as fusion failure or adjacent segment disease may occur. Moreover, because of adhesion and narrow SAC, it seems to be highly risky for intraoperative tearing of dura mater, spinal cord injury, or insufficient removal of OPLL. On the contrary, if we carry out laminoplasty only, the effect of surgery may be insufficient due to the existence of OPLL and the postoperative kyphosis may also occur. Therefore, in such cases, circumferential cervical surgery should be considered.
The multilevel laminoplasty for posterior decompression is frist performed, providing the safe migration of the spinal cord to the posterior part of spinal canal. Secondly, selective corpectomy and removal of OPLL in the most severe segment (1-2 level) and fusion with a plate-and-screw system is carried out. Through this, the multilevel vertebral body can be decompressed effectively with a low risk for occurrence of the intraoperative complication, with a prevention of the fusion failure, and with a maintenance of the cervical lordosis.
In the current study, increases of SAC and spinal canal diameter following sufficient direct removal of OPLL, and with regard to patient's satisfaction, improvement of clinical outcomes such as JOA score, Nurick's grade, and Odom's criteria were significant. Surgical complications such as aggravation of neurological symptoms due to iatrogenic spinal cord injury or CSF leakage due to tearing of dura mater did not occur. Also, radiological findings, including nonoccurrence of fusion failure and spinal instability, and increase of cervical lordotic angle during the follow-up period were satisfactory.
Despite its inconvenience, time requirement, potential to cause large EBL, and high risk of surgical morbidity such as wound infection, the completion of selective ACF and laminoplasty in a single day is tolerable in carefully selected patients18). In the current study, surgical outomes including EBL, operation time, and duration of bed rest were tolerable. Other than one case of postoperative temporary pneumonia, no major surgical morbidity occurred.
There were limitations in our study. The number of patients was too small and the follow-up period was too short. Furthermore, we did not evaluate the biomechanical effect and contribution of each technique alone on the circumferential cervical surgery. Additional study is required to compare circumferential cervical surgery to ACF or laminoplasty alone in cases of identical operative indications.
CONCLUSION
Although we chose a small sample size and used short term follow-up periods, the results indicate that single stage circumferential cervical surgery, in multilevel OPLL with prominent cord compression resulting spinal cord ischemia on MRI and severe neurological symptoms, seems favorable for direct selective decompression with low risk of iatrogenic cord injury and fusion failure, and for maintenance of cervical lordosis.
References
- 1.Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery : a prospective study. Spine (Phila Pa 1976) 2002;27:2453–2458. doi: 10.1097/00007632-200211150-00007. [DOI] [PubMed] [Google Scholar]
- 2.Chiba K, Ogawa Y, Ishii K, Takaishi H, Nakamura M, Maruiwa H, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy--average 14-year follow-up study. Spine (Phila Pa 1976) 2006;31:2998–3005. doi: 10.1097/01.brs.0000250307.78987.6b. [DOI] [PubMed] [Google Scholar]
- 3.Chiba K, Yamamoto I, Hirabayashi H, Iwasaki M, Goto H, Yonenobu K, et al. Multicenter study investigating the postoperative progression of ossification of the posterior longitudinal ligament in the cervical spine : a new computer-assisted measurement. J Neurosurg Spine. 2005;3:17–23. doi: 10.3171/spi.2005.3.1.0017. [DOI] [PubMed] [Google Scholar]
- 4.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 5.Dai L, Ni B, Yuan W, Jia L. Radiculopathy after laminectomy for cervical compression myelopathy. J Bone Joint Surg Br. 1998;80:846–849. doi: 10.1302/0301-620x.80b5.8580. [DOI] [PubMed] [Google Scholar]
- 6.Epstein N. Ossification of the cervical posterior longitudinal ligament: a review. Neurosurg Focus. 2002;13:ECP1. doi: 10.3171/foc.2002.13.2.16. [DOI] [PubMed] [Google Scholar]
- 7.Epstein NE. Circumferential cervical surgery for ossification of the posterior longitudinal ligament : a multianalytic outcome study. Spine (Phila Pa 1976) 2004;29:1340–1345. doi: 10.1097/01.brs.0000127195.35180.08. [DOI] [PubMed] [Google Scholar]
- 8.Gok B, Sciubba DM, McLoughlin GS, McGirt M, Ayhan S, Wolinsky JP, et al. Surgical treatment of cervical spondylotic myelopathy with anterior compression : a review of 67 cases. J Neurosurg Spine. 2008;9:152–157. doi: 10.3171/SPI/2008/9/8/152. [DOI] [PubMed] [Google Scholar]
- 9.Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K. Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine : More than 10 years follow up. J Neurosurg. 2002;96:180–189. [PubMed] [Google Scholar]
- 10.Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, et al. Surgical strategy for cervical myelopahty due to ossification of the posterior longitudinal ligament : Part 1 : Clinical results and limitations of laminoplasty. Spine (Phila Pa 1976) 2007;32:647–653. doi: 10.1097/01.brs.0000257560.91147.86. [DOI] [PubMed] [Google Scholar]
- 11.Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, et al. Surgical strategy for cervical myelopahty due to ossification of the posterior longitudinal ligament : Part 2 : Advantages of anterior decompression and fusion over laminoplasty. Spine (Phila Pa 1976) 2007;32:654–660. doi: 10.1097/01.brs.0000257566.91177.cb. [DOI] [PubMed] [Google Scholar]
- 12.Kawaguchi Y, Kanamori M, Ishihara H, Nakamura H, Sugimori K, Tsuji H, et al. Progression of ossification of the posterior longitudinal ligament following en bloc cervical laminoplasty. J Bone Joint Surg Am. 2001;83-A:1798–1802. doi: 10.2106/00004623-200112000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Kawaguchi Y, Kanamori M, Ishihara H, Ohmori K, Nakamura H, Kimura T. Minimum 10-year followup after en bloc cervical laminoplasty. Clin Orthop Relat Res. 2003:129–139. doi: 10.1097/01.blo.0000069889.31220.62. [DOI] [PubMed] [Google Scholar]
- 14.Kim JG, Kim SW, Lee SM, Shin H. Surgical result of the combined anterior and posterior approach in treatment of cervical spondylotic myeolopathy. J Korean Neurosurg Soc. 2006;39:188–191. [Google Scholar]
- 15.Kim YS, Chin DK, Cho YE, Jin BH, Yoon YS, Park JP, et al. Surgical treatment for ossification of the posterior longitudinal ligament of the cervical spine. J Korean Neurosurg Soc. 1997;26:1237–1245. [Google Scholar]
- 16.Matz PG, Pritchard PR, Hadley MN. Anterior cervical approach for the treatment of cervical myelopathy. Neurosurgery. 2007;60:S64–S70. doi: 10.1227/01.NEU.0000215399.67006.05. [DOI] [PubMed] [Google Scholar]
- 17.Mayr MT, Subach BR, Comey CH, Rodts GE, Haid RW., Jr Cervical spinal stenosis : outcome after anterior corpectomy, allograft reconstruction, and instrumentation. J Neurosurg. 2002;96:10–16. doi: 10.3171/spi.2002.96.1.0010. [DOI] [PubMed] [Google Scholar]
- 18.Mummaneni PV, Haid RW, Rodts GE., Jr Combined ventral and dorsal surgery for myelopathy and myeloradiculopathy. Neurosurgery. 2007;60:S82–S89. doi: 10.1227/01.NEU.0000215355.64127.76. [DOI] [PubMed] [Google Scholar]
- 19.Nakase H, Park YS, Kimura H, Sakaki T, Morimoto T. Complications and long-term follow-up results in titanium mesh cage reconstruction after cervical corpectomy. J Spinal Disord Tech. 2006;19:353–357. doi: 10.1097/01.bsd.0000210113.09521.aa. [DOI] [PubMed] [Google Scholar]
- 20.Ogawa Y, Toyama Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, et al. Long-term results of expansive open-door laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine. J Neurosurg Spine. 2004;1:168–174. doi: 10.3171/spi.2004.1.2.0168. [DOI] [PubMed] [Google Scholar]
- 21.Ozgen S, Naderi S, Ozek MM, Pamir MN. A retrospective review of cervical corpectomy : indications, complications and outcome. Acta Neurochir (Wien) 2004;146:1099–1105. doi: 10.1007/s00701-004-0327-z. discussion 1105. [DOI] [PubMed] [Google Scholar]
- 22.Robinson RA, Smith GW. Anterolateral cervical disk removal and interbody fusion for cervical disk syndrome. Bull Johns Hopkins Hosp. 1955;96:223–224. [Google Scholar]
- 23.Sasso RC, Ruggiero RA, Jr, Reilly TM, Hall PV. Early reconstruction failures after multilevel cervical corpectomy. Spine. 2003;28:140–142. doi: 10.1097/00007632-200301150-00009. [DOI] [PubMed] [Google Scholar]
- 24.Sim SJ, Cho JH, Yoo SI, Kown YD, Lee YS. Clinical analysis of postoperative prognostic factors of cervical anterior decompression and interbody fusion for OPLL. J Korean Neurosurg Soc. 2000;29:360–364. [Google Scholar]
- 25.Stewart TJ, Schlenk RP, Benzel EC. Multiple level discectomy and fusion. Neurosurgery. 2007;60:S143–S148. doi: 10.1227/01.NEU.0000217015.96212.1B. [DOI] [PubMed] [Google Scholar]
- 26.Tani T, Ushida T, Ishida K, Iai H, Noguchi T, Yamamoto H. Relative safety of anterior microsurgical decompression versus laminoplasty for cervical myelopathy with a massive ossified posterior longitudinal ligament. Spine (Phila Pa 1976) 2002;27:2491–2498. doi: 10.1097/00007632-200211150-00013. [DOI] [PubMed] [Google Scholar]
- 27.Vaccaro AR, Falatyn SP, Scuderi GJ, Eismont FJ, McGuire RA, Singh K, et al. Early failure of long segment anterior cervical plate fixation. J Spinal Disord. 1998;11:410–415. [PubMed] [Google Scholar]
- 28.Vitarbo E, Sheth RN, Levi AD. Open-door expansile cervical laminoplasty. Neurosurgery. 2007;60:S154–S159. doi: 10.1227/01.NEU.0000215353.94448.16. [DOI] [PubMed] [Google Scholar]
- 29.Wiggins GC, Shaffrey CI. Dorsal surgery for myelopathy and myeloradiculopathy. Neurosurgery. 2007;60:S71–S81. doi: 10.1227/01.NEU.0000215379.90537.0B. [DOI] [PubMed] [Google Scholar]
- 30.Yonenobu K, Hosono N, Iwasaki M, Asano M, Ono K. Neurologic complications of surgery for cervical compression myelopathy. Spine (Phila Pa 1976) 1991;16:1277–1282. doi: 10.1097/00007632-199111000-00006. [DOI] [PubMed] [Google Scholar]