Abstract
The Chiari 1.5 malformation is defined as a tonsillar herniation within a Chiari I malformation with additional caudal descent of the brainstem through the foramen magnum. We describe a patient with Chiari I malformation who evolved to Chiari 1.5 malformation during longitudinal follow-up. A 15-year-old girl presented with neck pain during exercise for two years. She had been diagnosed with Chiari I malformation with mild hydrocephalus after minor cervical trauma at the age of six years. At that time, she was asymptomatic. After she complained of aggravated neck pain, neuroimaging (nine years after first imaging) revealed caudal descent of the brainstem and syringomyelia in addition to progression of tonsillar herniation. Posterior fossa decompressive surgery resulted in complete resolution of neck pain. Based on neuroimaging and operative findings, she was diagnosed as Chiari 1.5 malformation. Neuroimaging performed seven months after surgery showed an increased anterior-posterior diameter of the medulla oblongata and markedly decreased syringomyelia. This case demonstrates progressive developmental process of the Chiari 1.5 malformation as an advanced form of the Chiari I malformation.
Keywords: Chiari 1.5 malformation, Asymptomatic hydrocephalus, Syringomyelia
INTRODUCTION
The four traditional types of Chiari malformations represent various clinical and anatomical processes that entail varying degrees of hindbrain involvement. Chiari types I, II, and III involve varying degrees of herniation of rhombencephalic derivatives out of the posterior cranial fossa. Chiari IV malformation involves cerebellar hypoplasia or aplasia with no herniation of the hindbrain8). Chiari I malformation has been defined as downward herniation of the cerebellar tonsils through the foramen magnum, whereas Chiari II malformation is associated with spina bifida and includes herniation of the vermis with corresponding descent of the rhombencephalon4). Chiari 1.5 malformation specifically refers to the tonsillar herniation seen in Chiari I malformation but with the addition of an elongated brainstem and fourth ventricle3,10). The imaging incidence of asymptomatic Chiari I malformation was determined to be 0.1-1%9). Chiari 1.5 malformation is thought to be less common than the Chiari I malformation, although the exact incidence of Chiari 1.5 malformation is still unknown.
We describe a case of Chiari 1.5 malformation that showed progressive downward herniation of the tonsils and obex with newly developed syringomyelia over nine years of follow-up.
CASE REPORT
History
A 15-year-old girl presented with neck pain that had occurred during neck exercise for two years. Nine years ago, her sister had dropped the patient while carrying her on her back. At the local hospital, brain magnetic resonance imaging (MRI) revealed tonsillar herniation with mild ventriculomegaly. She had no other history of intracranial lesions such as craniosynostosis, meningitis or encephalitis, major head trauma, or violation of the subarachnoid space via, for example, lumbar puncture. As she reported no pain or other neurological symptoms, we recommended observation with serial MRI follow-up. Seven years after the initial accident, she complained of intermittent neck pain occurring on exercise. This pain became aggravated with neck extension. She did not have any symptoms, such as snoring, sleep apnea, weakness or paresthesia, other than neck pain.
Radiologic finding
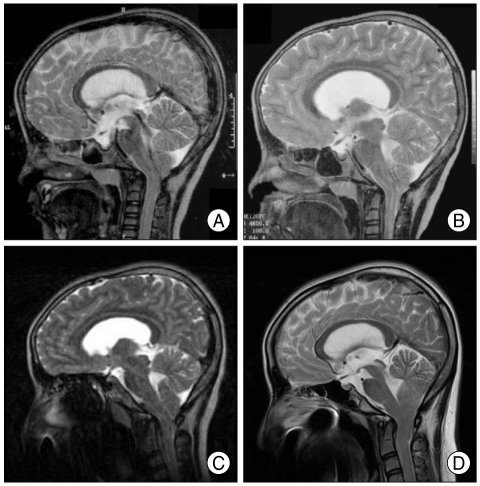
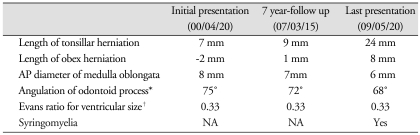
The initial MRI revealed a 7-mm descent of the cerebellar tonsil below the foramen magnum (basion-opisthion line, or McRae line6,13)) with mild ventriculomegaly (Evans ratio2 : 0.33). The obex was 2 mm superior to the foramen magnum, and the anterior-posterior (AP) diameter of the medulla oblongata was 8 mm. The angulation of the odontoid process13) was 75° (Fig. 1A). To evaluate the obex herniation, we measured the distance of the obex to the McRae line6,13). When it became difficult to identify the obex by sagittal MRI imaging, we looked for it at the midpoint between the fourth ventricle outlet and the opening of the central canal by axial MRI imaging and transferred this position to the sagittal MRI imaging. To evaluate the angulation of the odontoid process, we measured the angle by drawing one horizontal line through a midpoint of the synchondrosis between the base and apex of the odontoid process and a second line through the midpoint of the synchondrosis and apex of the odontoid process on a midsagittal MRI section13). Spinal MRI was not undertaken at that time, so it was not known the presence or degree of syringomyelia. The two-year follow-up MRI revealed almost no change in tonsillar herniation or mild ventriculomegaly, with the same Evans ratio (0.33); the patient remained asymptomatic (Fig. 1B). Seven years after the minor cervical trauma, she began to complain of neck pain. At that time, MRI showed a slight increase in tonsillar herniation (9 mm), and the obex was 1 mm inferior to the foramen magnum (Fig. 1C). The nine-year follow-up MRI revealed substantial progression of tonsillar herniation compared to the initial MRI (Fig. 1D) (Table 1). The extent of tonsillar herniation below the foramen magnum was determined to be 24 mm by midsagittal MRI. Tonsillar herniation was asymmetric: the right tonsillar herniation was down to the C-2 level, whereas the left tonsillar herniation reached the C-1 level (Fig. 2A). The obex was 8 mm inferior to the foramen magnum. The AP diameter of the medulla oblongata was 6 mm, resulting in a flattened and elongated appearance in the midsagittal section. The angulation of the odontoid process progressed from 75° to 68°. The Evans ratio of ventriculomegaly was the same (0.33). A spinal MRI demonstrated syringomyelia involving C-6 to T-10 levels (Fig. 2B).
Fig. 1.
Midsagittal brain MR images showing the cervicomedullary junction and high cervical spine obtained in a 15-year-old girl presenting with neck pain exercise. Note the nine-year gradual progression of cerebellar tonsillar herniation from 7 mm (A) to 24 mm (D), the descent of the obex from 2 mm above the foramen magnum (A) to 8 mm below (D) and the thinning of the medulla oblongata from 8 mm (A) to 6 mm (D). A : Initial sagittal T2-weighted MR image, B : 2 years, C : 7 years, and D : 9 years after the initial presentation.
Table 1.
Clinical summary of patient MRI findings
*Angulation of odontoid process13) was measured by connecting one horizontal line through a midpoint of the synchondrosis between the base and apex of the odontoid process with another line through the apex of the odontoid and the midpoint of the synchondrosis on a midsagittal MR section, †Evans ratio2 was measured from T2-weighted axial images, defined as the maximum width between the tips of the frontal horns of the lateral ventricles divided by the maximum transverse intracranial diameter, i.e., the maximum distance between the two sides of the inner table of the skull at the same plane with the measure of frontal horn width. AP : anterior-posterior, NA : non-applicable
Fig. 2.
A : Coronal T1-weighted MR image. Note the asymmetric herniation of the cerebellar tonsils: the left tonsil is found to lie at the posterior aspect of the C-1 level and the right tonsil at the C-2 level. B : Midsagittal T2-weighted whole spine MR image presenting syringomyelia from the C-6 to the T-10 level.
Operation
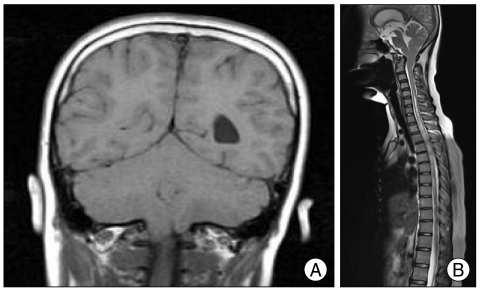
The patient underwent suboccipital craniectomy (2.5 × 2.5 cm), C-1 total laminectomy and C-2 partial laminectomy, right cerebellar tonsillectomy, and duraplasty. Extradurally, the craniovertebral junction was tight, and dural sac pulsation was invisible. Intradurally, the cerebellar tonsils showed asymmetric herniation; greater caudal descent of the right tonsil was evident (Fig. 3A). The maximum distance of tonsillar herniation below the foramen magnum was 25 mm. The dorsal side of the medulla oblongata looked humped, as though something had pushed the medulla backward. The obex and medulla were elongated and caudally displaced to the lower portion of the C-1 level (Fig. 3B). The obex was 15 mm inferior to the foramen magnum. Operative findings confirmed the diagnosis of Chiari 1.5 malformation.
Fig. 3.
A : Intraoperative photograph of the cervicomedullary junction following suboccipital decompression and C-1 total and C-2 partial laminectomy, revealing well-formed, peg-like tonsils extending to the posterior arch of the atlas (white arrowhead; left tonsil) and the C-2 level (black arrowhead; right tonsil). B : A photograph acquired after right partial tonsillectomy. The arrow indicates the obex.
Based on operative diagnosis, tonsillectomy was added to achieve more active posterior fossa decompression. No shunt operation for hydrocephalus or syringomyelia was performed.
Postoperative course
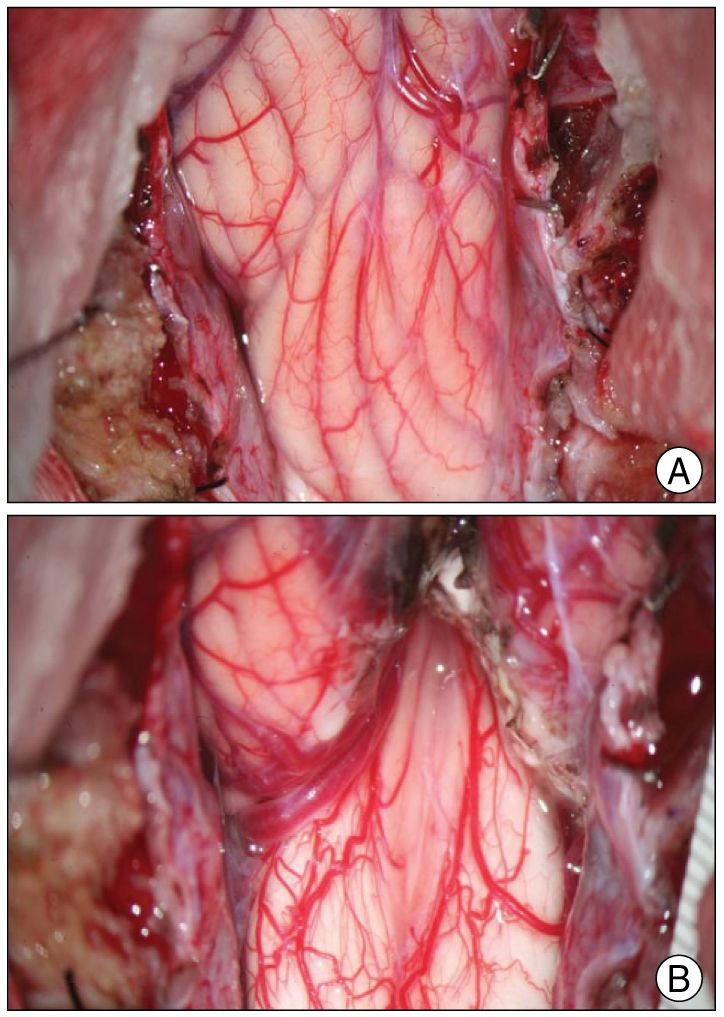
The patient's neck pain disappeared completely after surgery. No additional symptoms occurred postoperatively. She has engaged in full physical activity, including swimming, and showed a Karnofsky Performance Scale score of 100 over a follow-up period of ten months. Postoperative MRI performed seven months after surgery showed increased an AP diameter of the medulla (12 mm) and markedly decreased syringomyelia (Fig. 4).
Fig. 4.

A sagittal T2-weighted MR image taken seven months after surgery shows increased anterior-posterior diameter of the medulla (from 6 mm to 12 mm) and markedly decreased cervical syringomyelia.
DISCUSSION
The etiology of Chiari I malformation remains unclear. One of the theories proposed for the pathogenesis of this condition involves the presence of a pressure differential between the cranial and spinal subarachnoid space. This theory indicates an alteration in cerebrospinal fluid (CSF) circulation and relative obstruction of CSF flow at the foramen magnum9). Presumably, an intermittent vector of force then develops with each Valsalva maneuver, which can lead to the progressive downward movement of developing tissue through the foramen magnum12).
In the present case, the patient was incidentally found to have tonsillar herniation and mild ventriculomegaly. She was asymptomatic at the first presentation and for more than seven years afterwards. When she presented with neck pain, all parameters indicating posterior fossa crowding except ventriculomegaly showed progression. Syringomyelia was also detected at this time. Interestingly, the location of the obex changed from 2 mm above the foramen magnum to 8 mm below. Therefore, the diagnosis was changed from Chiari I to Chiari 1.5 malformation. This single case analysis could not clarify the exact mechanism of progression of tonsillar and obex herniation. However, increased grades of odontoid retroflexion might be associated with progression of tonsillo-medullary elongation with newly developed syringomyelia in the present case. Tubbs et al.13) reported that higher grades of odontoid angulation are more often associated with a caudally displaced obex and an increased incidence of syringomyelia. They speculated that the displaced brainstem caused by a posteriorly tilted odontoid process contributed to the compression at the craniocervical junction and disturbance of CSF circulation at the level of the obex. Regarding the cause of progression of odontoid angulation, we do not have a definite answer yet. Greiz7) recently proposed the partial obstruction of the CSF flow channel around the craniocervical junction and Venturi effect with enhanced intramedullary pulse pressure causing extracellular fluid accumulation in the distended cord as the mechanism of the formation of the syringomyelia in Chiari I malformation6). Retroflexion of the odontoid process, herniated tonsils and brainstem (obex) are all anatomic substrates of Chiari malformation for the partial obstruction of the subarachnoid space at the rostralmost cervical cord.
Differential diagnosis between Chiari I malformation and Chiari 1.5 malformation is important because of the differences in operative strategy and treatment outcome. Tubbs et al.11-13) reviewed 130 symptomatic pediatric Chiari I malformation patients and 22 of them were Chiari 1.5 malformation patients. Clinical manifestations and symptomatic outcomes were similar between the two groups in terms of degree of tonsillar herniation (Chiari I malformation vs. Chiari 1.5 malformation : 7 mm vs. 12.7 mm), the angulation of the odontoid process (98.0° vs. 84.4°), hydrocephalus (11% vs. 9.1%), syringomyelia (58% vs. 50%), scoliosis (17% vs. 27%) and postoperative improvement of symptoms (83% vs. 82%). However, the incidence of unresolved syringomyelia after posterior fossa decompressive surgery was nearly two-fold higher in Chiari 1.5 malformation (13.6%) than in Chiari I malformation (6.9%). A significant number of Chiari 1.5 malformation patients required repeated posterior fossa operations for persistent syringomyelia. Persistence of syrinx can be attributed to irreversible spinal cord change secondary to progressive gliosis or insufficient decompression of "crowding" around the foramen magnum caused by dense constrictive bands, intradural arachnoid adhesion or veils.1,5) Neuroimaging can indicate typical radiological characteristics in Chiari 1.5 malformation. However, it is not always easy to make an accurate preoperative diagnosis because posterior fossa crowding might prevent identification of posterior fossa structures. And, there is different methodology between clinicians to measure the distance of the tosil, obex from the McRae line. To evaluate tonsillar (or obex) hernation, we drew a perpendicular line from the tonsillar tip(or obex) to the McRae line, but Tubbs13) drew a distance between the tonsillar tip (or obex) and a midpoint of McRae line. There is chance of overestimation with Tubbs's method compared to our method. At operation, we measured the distance beneath foramen magnum (opisthion). In the present study, there was a discrepancy in the degree of obex descent between radiological and intraoperative measurements (8 mm vs. 15 mm). This reflects the difficulty of obtaining an accurate obex location with neuroimaging. However, neck flexion during the operation might partly explain this discrepancy. For operative diagnosis, the levels of C-1, C-2, and obex are drawn compared to the level of the foramen magnum to estimate the extent of brainstem elongation. When the patient is confirmed to have Chiari 1.5 malformation, a more active surgical strategy with sufficient foramen magnum decompression, including tonsillectomy and meticulous fenestration of intradural arachnoid adhesions and veils, is needed to achieve resolution of syringomyelia and prevent the need for repeated operations.
CONCLUSION
We report a case of Chiari I malformation that evolved to Chiari 1.5 malformation by gradual progressive descent of the tonsils and obex. Long-term imaging surveillance of asymptomatic Chiari I malformation is needed for early detection of clinical progression. In the case of advanced form of Chiari 1.5 malformation, sufficient posterior fossa decompression including tonsillectomy for normalizing CSF circulation around the foramen magnum is necessary.
References
- 1.Armonda RA, Citrin CM, Foley KT, Ellenbogen RG. Quantitative cine-mode magnetic resonance imaging of Chiari I malformations : an analysis of cerebrospinal fluid dynamics. Neurosurgery. 1994;35:214–223. doi: 10.1227/00006123-199408000-00006. discussion 223-224. [DOI] [PubMed] [Google Scholar]
- 2.Bersani G, Paolemili M, Quartini A, Clemente R, Gherardelli S, Iannitelli A, et al. Neurological soft signs and cerebral measurements investigated by means of MRI in schizophrenic patients. Neurosci Lett. 2007;413:82–87. doi: 10.1016/j.neulet.2006.11.032. [DOI] [PubMed] [Google Scholar]
- 3.Capra V, De Marco P, Merello E, Baffico AM, Baldi M, Divizia MT, et al. Craniosynostosis, hydrocephalus, Chiari I malformation and radioulnar synostosis : probably a new syndrome. Eur J Med Genet. 2009;52:17–22. doi: 10.1016/j.ejmg.2008.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Cardoso M, Keating RF. Neurosurgical management of spinal dysraphism and neurogenic scoliosis. Spine (Phila Pa 1976) 2009;34:1775–1782. doi: 10.1097/BRS.0b013e3181b07914. [DOI] [PubMed] [Google Scholar]
- 5.Chang HS, Nakagawa H. Hypothesis on the pathophysiology of syringomyelia based on simulation of cerebrospinal fluid dynamics. J Neurol Neurosurg Psychiatry. 2003;74:344–347. doi: 10.1136/jnnp.74.3.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cronin CG, Lohan DG, Mhuircheartigh JN, Meehan CP, Murphy J, Roche C. CT evaluation of Chamberlain's, McGregor's, and McRae's skull-base lines. Clin Radiol. 2009;64:64–69. doi: 10.1016/j.crad.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 7.Greitz D. Unraveling the riddle of syringomyelia. Neurosurg Rev. 2006;29:251–263. doi: 10.1007/s10143-006-0029-5. discussion 264. [DOI] [PubMed] [Google Scholar]
- 8.Koehler PJ. Chiari's description of cerebellar ectopy (1891). With a summary of Cleland's and Arnold's contributions and some early observations on neural-tube defects. J Neurosurg. 1991;75:823–826. doi: 10.3171/jns.1991.75.5.0823. [DOI] [PubMed] [Google Scholar]
- 9.Meadows J, Kraut M, Guarnieri M, Haroun RI, Carson BS. Asymptomatic Chiari Type I malformations identified on magnetic resonance imaging. J Neurosurg. 2000;92:920–926. doi: 10.3171/jns.2000.92.6.0920. [DOI] [PubMed] [Google Scholar]
- 10.Snyder P. Chiari malformation and syringomyelia. Radiol Technol. 2008;79:555–558. [PubMed] [Google Scholar]
- 11.Tubbs RS, Iskandar BJ, Bartolucci AA, Oakes WJ. A critical analysis of the Chiari 1.5 malformation. J Neurosurg. 2004;101:179–183. doi: 10.3171/ped.2004.101.2.0179. [DOI] [PubMed] [Google Scholar]
- 12.Tubbs RS, McGirt MJ, Oakes WJ. Surgical experience in 130 pediatric patients with Chiari I malformations. J Neurosurg. 2003;99:291–296. doi: 10.3171/jns.2003.99.2.0291. [DOI] [PubMed] [Google Scholar]
- 13.Tubbs RS, Wellons JC, 3rd, Blount JP, Grabb PA, Oakes WJ. Inclination of the odontoid process in the pediatric Chiari I malformation. J Neurosurg. 2003;98:43–49. doi: 10.3171/spi.2003.98.1.0043. [DOI] [PubMed] [Google Scholar]