Abstract
Background
Esophagectomy with gastric tube reconstruction results in a variety of postoperative nutrition-related symptoms that may influence the patient’s nutritional status.
Methods
We developed a 15-item questionnaire, focusing on the nutrition-related complaints the first year after an esophagectomy. The questionnaire was filled out the first week after discharge and 3, 6, and 12 months after surgery. The use of enteral nutrition, meal size and frequency, social aspects related to eating, defecation pattern, and body weight were recorded at the same time points. We analyzed the relationship between the baseline characteristics and the number of nutrition-related symptoms, as well as the relationship between those symptoms and body weight with linear mixed models.
Results
We found no significant within-patient change for the total number of nutrition-related symptoms (P = 0.67). None of the baseline factors were identified as predictors of the complaint scores. The most frequently experienced complaints were early satiety, postprandial dumping syndrome, inhibited passage due to high viscosity, reflux, and absence of hunger. One year after surgery, meal sizes were still smaller, the social aspects of eating were influenced negatively, and patients experienced an altered stool frequency. Directly after the surgical procedure 78% of the patients lost weight, and the entire postoperative year the mean body weight remained lower (P = 0.47). We observed no association between the complaint scores and body weight (P = 0.15).
Conclusions
After an esophagectomy, most patients struggle with nutrition-related symptoms, are confronted with nutrition-related adjustments and a reduced body weight.
Introduction
An esophagectomy with gastric tube reconstruction, mainly performed as a potentially curative treatment in patients with cancer of the esophagus or cardia, is often related to a number of postoperative nutrition-related complaints [1–5]. Dysphagia, pain during alimentation, hoarseness, reflux, early satiety, abnormal gastric emptying, dumping syndrome, increased stool frequency, and fluctuations in bodyweight are frequently reported complaints after this surgical procedure [6–17].
These nutrition-related complaints might affect the nutritional status negatively by increasing the risk of malnutrition and reducing the quality of life [18–21]. Little is known about the short-term and long-term occurrence of or changes in these symptoms. There is also no detailed information about nutrition-related adjustments (e.g., the need for enteral nutrition, altered meal size and meal frequency, social aspects, stool consistency and stool frequency) or nutritional status in terms of body weight after esophagectomy.
Most previous studies evaluated the nutrition-related symptoms only once or twice in the first postoperative year. Furthermore, these studies did not use specific questionnaires to evaluate these nutrition-related symptoms systematically and in greater depth [7, 9, 12, 13, 15, 22].
In the present study, we addressed the following research questions: (1) Does this patient have nutrition-related symptoms and have these symptoms increased or decreased during the first year after esophagectomy? (2) Are nutrition-related adjustments necessary after esophagectomy? (3) What is the patient’s nutritional status in terms of body weight and how has this status changed during the first year after esophagectomy? (4) Are nutrition-related symptoms significantly influenced by patient characteristics and surgery-related characteristics? (5) Is there a significant correlation between the nutrition-related symptoms and postoperative bodyweight?
Patients and methods
All consecutive postoperative patients who underwent a transhiatal or transthoracic esophagectomy with gastric tube reconstruction for both malignant and benign diseases at the surgical department of the Academic Medical Center, University Hospital of Amsterdam (The Netherlands) were considered eligible for inclusion in this study. Patients were screened for inclusion during a 4-year period (2002–2005).
The following exclusion criteria were applied: patients suffering from a diabetes-related neuropathy, a neurological disease, ulcerative colitis, Crohn’s or celiac disease, and patients with a proven allergy. Patients who were unable to speak and/or read Dutch were also excluded, as they were unable to fill out the questionnaire.
The main goal of our study was to describe the nutritional symptoms directly related to the surgical procedure. Therefore, patients were excluded if they had a proven recurrence of a malignant disease or had another life-threatening disease.
The protocol was approved by the institutional review board (Ethics Committee) of the Academic Medical Center at the University of Amsterdam. All patients were informed and gave written consent.
Surgical procedure
The esophageal resection was carried out either via the transhiatal or the transthoracic approach and the reconstruction of the digestive tract was performed by a gastric tube [6, 23, 24]. Although a cervical gastroesophageal anastomosis has a leakage rate with less devastating consequences, the percentage of benign strictures is higher. However, the gastric tube is generally preferred over a colonic interposition because there is a lower morbidity rate and a better postoperative quality of life [25]. Esophageal resections are rarely performed for benign diseases such as achalasia, because gastric tube reconstruction still causes a variety of symptoms.
Baseline assessments
Patient-related baseline data (age, sex, presence of malignancy, neoadjuvant treatment, admission duration), physical status (preoperative bodyweight, body mass index [BMI], co-morbidity, preoperative complaints), and surgery-related characteristics (American Society of Anesthesiolgists [ASA] classification, type of surgical procedure, postoperative complications) were collected during the first postoperative week from electronic medical records and dietician records.
Postoperative nutritional care
According to our hospital’s standard guidelines, postoperative patients were initially fed through a surgically placed jejunostomy feeding tube. Tube feeding uses a complete liquid enteral formula, which is given during the period when the patient is not allowed to eat or drink or is otherwise unable to meet nutritional needs. Seven days after the start of tube feeding, possible cervical leakage was evaluated by x-swallow. Oral food intake began with small, frequent meals during the day only if no leakage was found. The amount of tube feeding was tailored to the oral intake achieved and guided by a dietician. Sip feeding units (small portions of highly concentrated drinks) were prescribed as supplementary feeding. Sip feeding is prescribed in case of an insufficient intake of nutrients, and is a complete enteral formula to be taken orally as a beverage rich in energy, proteins, and micronutrients.
Follow-up assessments
For the purpose of the present study, a 15-item feeding questionnaire was developed at our hospital. This questionnaire focused on the nutrition-related symptoms experienced by individual patients. The aim of the questionnaire was to describe the patient’s complaints during the preceding week and covered the following items: (1) dysphagia and reflux (8 items) and (2) stomach content and dumping syndrome (7 items). The total score ranged from 0 (no complaints) to 15 (suffering from all complaints, see Appendix). The feeding questionnaire was pre-tested on 15 patients, adjusted, and then re-tested on another sample of 10 patients before the start of the study.
Patients were asked to fill out the questionnaire at home before each planned follow-up assessment during the first week after discharge, and then at 3, 6, and 12 months after surgery. Follow-up assessments took place in the outpatient clinic. A dietician collected the questionnaires and discussed the reported nutrition-related symptoms with the patients. In addition, nutrition-related adjustments in terms of enteral nutrition, meal size and meal frequency, the nutrition-related social aspects, stool consistency and stool frequency, and the nutritional status in terms of body weight were recorded at this session.
Meal sizes were compared to the preoperative situation and classified as “equal,” “increased,”or “decreased.” Meal frequency was defined as the number of meals, snacks, and/or beverages a patient consumed during a 24 h period (day and night). These meals were categorized as <3 times, 3 times, 4–6 times, or >6 times per 24 h.
The social aspects related to eating and drinking were evaluated by three questions: (1) experiencing fear of eating or drinking, (2) experiencing pleasure in eating and drinking, and (3) going out to dinner (to a restaurant or to family/friends). Fear was categorized as “never,” “seldom,” “often,” or “always.” Pleasure in eating and drinking and going out to dinner were compared to the preoperative situation and were categorized as “no(t),” “less,” “equal,”or “more.”
The defecation pattern was compared to the preoperative situation. It was divided into frequency (<1 stool, 1 stool, 2 stools, >2 stools [including frequency]) within a 24-h period and consistency (thin as water, slush, solid, or other [including description]).
In order to calculate weight loss, patients were asked to estimate their weight one month prior to each study assessment.
Statistical analyses
Baseline patient characteristics, physical status, surgery-related characteristics, the presence of nutrition-related symptoms, intake of enteral nutrition (tube feeding and sip feeding), meal size, meal frequency, body weight, nutrition-related social aspects, and defecation patterns were summarized using descriptive statistics.
The Kolmogorov-Smirnov test was used to test whether the patient-related and surgery-related characteristics were normally distributed. Differences between proportions and mean scores were analyzed with the χ2 test or the two group t-test when appropriate.
The repeated data structure of the nutrition-related complaint scores (both total and subscale scores) were analyzed with a linear mixed model (LMM). In this approach we included all complaint scores as measured at the various follow-up visits. Hence, in case of relapse of the malignant disease or death, the data of the patients (before these events) were also included in the mixed models. The LMM was repeated after including the baseline patient and surgery-related characteristics (age, sex, preoperative tube feeding, neo-adjuvant treatment, surgical procedure, and postoperative complications) that were assumed to predict the complaint scores.
The course of body weight during the first postoperative year was also evaluated by a linear mixed model with and without the complaint scores as covariate. All analyses were executed in SPSS version 16.0 (SPSS Corp. Chicago IL).
Results
During the period of the study (2002–2005), 140 patients underwent an esophagectomy with gastric tube reconstruction. Of these patients, 134 (96%) were eligible for the study. In total, 96 patients took part in the study. Sixty of them (63%) completed the one-year follow-up. Forty-one patients filled out the questionnaire at all time points during the first postoperative year (Fig. 1). The baseline characteristics of the 96 patients who took part in the study are summarized in Table 1.
Fig. 1.
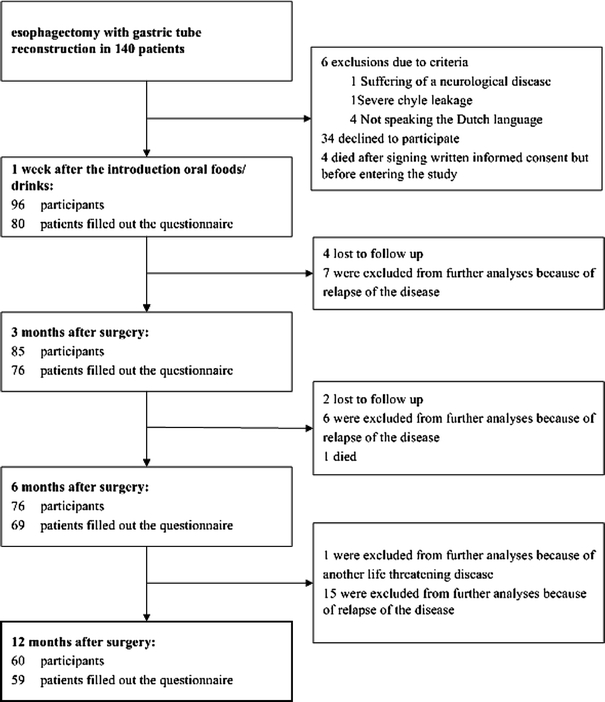
Study flow chart
Table 1.
Baseline characteristics of the patient group (n = 96)
| Total population (n = 96) | Completers one year follow-up (n = 60) | Non- completers (n = 36) | Completers vs non- completers (P value) | |
|---|---|---|---|---|
| Patient-related characteristics | ||||
| Age, yearsa | 62 (10) | 60 (10) | 63 (10) | 0.27 |
| Male genderb | 73 (76) | 48 (80) | 25 (69) | 0.23 |
| Presence of malignancyb | 93 (97) | 58 (97) | 35 (97) | 1.00 |
| Neoadjuvant treatmentb | 1.00 | |||
| Chemotherapy | 11 (11) | 6 (10) | 5 (14) | |
| Chemotherapy and radiotherapy | 18 (19) | 12 (20) | 6 (17) | |
| Admission durationa | 20 (8) | 19 (9) | 20 (7) | 0.64 |
| Physical status-related characteristics | ||||
| Preoperative body weighta | 79.0 (15.8) | 79.9 (16.2) | 78.3 (15.3) | 0.56 |
| Preoperative weight loss | 49 (51) | 33 (55) | 16 (44) | 0.40 |
| BMIa | 26.0 (3.9) | 26.1 (3.9) | 26.2 (4.2) | 0.80 |
| Underweight BMI < 18.5 < 65 years | 4 (4) | 4 (7) | 0 (0) | |
| Underweight BMI < 20.0 > 65 years | 1 (1) | 0 (0) | 1(3) | |
| Obesity BMI > 30 | 13 (14) | 9 (15) | 4 (11) | |
| Co-morbidityb | ||||
| Cardiovascular diseases | 46 (48) | 27 (45) | 19 (53) | 0.80 |
| Pulmonary diseases | 21 (22) | 13 (22) | 9 (25) | 0.80 |
| Diseases of the urinary tract | 19 (20) | 13 (22) | 6 (17) | 0.79 |
| Renal diseases | 6 (6) | 5 (8) | 1 (3) | 0.41 |
| Diabetes mellitus | 6 (6) | 3 (5) | 3 (8) | 1.00 |
| Preoperative complaintsb | ||||
| Dysphagia | 69 (72) | 41 (68) | 28 (78 | 0.49 |
| Epigastric/retrosternal pain | 24 (25) | 14 (23) | 10 (28) | 0.47 |
| Hiccups | 9 (9) | 4 (7) | 5 (14) | 0.72 |
| Anorexia | 2 (2) | 1 (2) | 1 (3) | 1.00 |
| Preoperative tube-feeding | 7 (7) | 5 (8) | 2 (6) | 1.00 |
| Surgery-related characteristics | ||||
| ASA classificationb | ||||
| ASA 3 | 20 (21) | 10 (17) | 10 (28) | 0.33 |
| ASA 4 | 1 (1) | 1 (2) | ||
| Surgical procedureb | 0.73 | |||
| Transthoracic esophageal resection | 50 (52) | 32 (53) | 18 (50) | |
| Transhiatal esophageal resection | 46 (48) | 28 (47) | 18 (50) | |
| Postoperative complicationsb | 60 (63) | 35 (58) | 25 (69) | 0.27 |
BMI body mass index, ASA American Society of Anesthesiologists score
aMean (SD)
b n (%)
Patient and surgery-related characteristics did not significantly differ between the patients who completed the study (n = 60) and those who dropped out (n = 36) during the one-year follow-up.
Nutrition-related symptoms
On average, patients suffered from seven nutrition-related complaints during the four follow-up moments (Table 2). Linear mixed modeling showed no significant within-patient change in the number of symptoms over time for the total population (P = 0.67). There was also no time-related change in the two subscale scores concerning dysphagia/reflux (P = 0.80) and stomach content/dumping syndrome (P = 0.71).
Table 2.
Mean number (±SD) of nutrition-related complaints and average body weight of the patients measured at four time points during the one-year follow-up
| 1 week (n = 80) | 3 months (n = 76) | 6 months (n = 69) | 12 months (n = 59) | P Valuea | |
|---|---|---|---|---|---|
| Total sum score of complaintsb | 7.0 (3.0) | 7.3 (2.9) | 7.4 (3.1) | 7.4 (3.6) | 0.67 |
| Subscale | |||||
| Dysphagia and refluxc | 3.3 (1.9) | 3.4 (2.0) | 3.5 (2.0) | 3.5 (2.4) | 0.80 |
| Stomach content and dumping syndromed | 3.7 (1.5) | 3.9 (1.5) | 3.8 (1.7) | 3.9 (1.8) | 0.71 |
| Body weight | 74.3 (13.7) | 74.2 (12.7) | 74.7 (12.1) | 73.9 (12.7) | 0.47 |
a P values based on linear mixed models
bRange total subscore: 0 points (complaints free) to 15 points (suffering from all complaints)
cSubscale dysphagia and reflux: 0 points to 8 points (suffering from all complaints)
dSubscale stomach content and dumping syndrome: 0 points to 7 points (suffering from all complaints)
In addition, none of the baseline factors appeared to be a significant predictor for the complaint scores: age (P = 0.84), sex (P = 0.20), preoperative tube-feeding (P = 0.54), neo-adjuvant treatment (P = 0.09), surgical procedure (P = 0.14), and postoperative complications (P = 0.78).
The five most frequent nutrition-related symptoms experienced by the patients were early satiety, postprandial dumping syndrome, inhibited passage due to high viscosity, reflux, and absence of hunger (Table 3). During the entire postoperative year a large number (about 90%) of the patients experienced early satiety, whereas about 75% of the patients suffered from postprandial dumping syndrome. About 50% of the study population experienced hunger one year after the operation. There was no difference between the type of symptoms in patients who completed the study and those who dropped out.
Table 3.
Percentage of patients who experienced the five most frequent nutrition-related complaints during the one-year follow-up
| Complainta | 1 week (n = 80) | 3 months (n = 76) | 6 months (n = 69) | 12 months (n = 59) |
|---|---|---|---|---|
| Early satiety | 71 (89) | 66 (87) | 60 (87) | 53 (90) |
| Postprandial dumping syndrome | 59 (74) | 59 (78) | 54 (78) | 44 (75) |
| Inhibited passage due to high viscosity | 42 (53) | 48 (63) | 41 (59) | 37 (63) |
| Reflux of food/fluid | 48 (60) | 41 (54) | 45 (65) | 36 (61) |
| Absence of hunger | 61 (76) | 43 (57) | 39 (57) | 30 (51) |
aAll values are expressed as n (%)
Nutrition-related adjustments: enteral nutrition
After discharge from the hospital, tube feeding was continued in 38 of the 80 patients (48%) who filled out the questionnaire during the first week after discharge. Their mean intake was 990 ml (range: 500–2,000 ml) and was mainly administered (79%) during the night. Six months after surgery only two patients still used nightly tube feeding to achieve their nutritional goals, and 12 months after surgery there was one such patient.
Sip feeding was started in 25% of the study population after discharge, and 12 months after surgery it was still used by 22%. Mean daily consumption of sip feeding was 300 ml (range: 70–600 ml) during the first 3 postoperative months and remained 230 ml (range: 40–400 ml) at 12 months.
Nutrition-related adjustments: meal sizes and meal frequency
Meal sizes were reduced compared to preoperative measurements according to 99% of the patients the first week after discharge; 12 months after surgery 92% of the patients still reported eating smaller meals compared to the preoperative situation. In addition, the number of meals remained high during the entire postoperative year; 12 months after the operation 58% of the patients had 3–6 meals a day, and 27% consumed as many as 6–9 snacks and small meals.
Nutrition-related adjustments: social aspects
One year after surgery, 16% of the study population still experienced eating or drinking in the company of others as unpleasant, and more than 50% of the patients went out less often to eat at a restaurant or with family or friends. The same proportion experienced a range from less pleasure to no pleasure in eating and drinking in general.
Nutrition-related adjustments: stool consistency and stool frequency
With regard to stool consistency, 81% of the patients defined their stool consistency before the surgical procedure as “solid.” Only 2% defined it as being “slush.” Although the consistency at 12 months was defined as “solid” by 48% of the patients, “slush” by 22%, and as “variable” by 30% (solid–slush, slush–thin as water), no significant change in stool consistency was demonstrated (P 0.17). In this group of survivors of the first postoperative year, their preoperative and postoperative stool consistencies were not significantly different.
Before surgery, a stool frequency of 1 stool per day was common in 65% of the total study population, 4% had > 2 stools and 10% had < 1. One year after surgery, 45% of the remaining participants had one stool per day, 8% had > 2 per day, and almost 30% had < 1 per day. Patients who survived the first postoperative year showed a significant alteration in postoperative stool frequency (increase or decrease) compared to the preoperative frequency (P < 0.001).
Nutritional status: body weight
At the time of discharge from the hospital, 75 patients (78%) had lost body weight (mean: 6.2 ± 5.6 kg) compared to their preoperative body weight. During the entire postoperative year, the mean body weight of the total population remained stable at a reduced level (P = 0.47) (see Table 2). No significant association between the complaint scores and body weight was observed (P = 0.15).
Discussion
This prospective longitudinal cohort study shows that patients who underwent an esophagectomy with gastric tube reconstruction suffered from a number of persistent, nutrition-related symptoms during the entire first postoperative year. Early satiety, postprandial dumping, inhibited passage due to high viscosity, reflux of food and/or fluids, and the absence of hunger were the most frequently reported nutrition-related symptoms. We demonstrated that time (in this case the first 12 postoperative months) is unrelated to the number of nutrition-related symptoms. The persistent symptoms could not be explained by a range of patient or surgery-related characteristics.
The large majority of patients ate smaller meals with a relatively high frequency during the first year of follow-up. After one year, the surgical procedure still influenced the nutrition-related social aspects of eating, and patients also experienced an altered stool frequency. A reduction of body weight occurred directly after the surgical procedure, and the majority of patients were unable to return to their preoperative weight. The weight reduction could not be explained by the nutrition-related complaints.
Our findings differ from those reported in the literature; we observed a number of persistent complaints, while other studies described a decrease in the nutrition-related symptoms that were experienced [6, 7, 13, 14, 26]. These differences could be explained by the design and execution of our study. Our primary aim was to evaluate the nutrition-related symptoms that patients experienced. In other studies, these nutritional aspects were secondary and were therefore not described or studied in detail. In some studies, retrospective data were used, or data were collected through postal surveys, without patient contact [8, 11, 22, 27, 28]. If the symptoms of postoperative patients were assessed by caregivers, only a maximum of two nutrition-related symptoms were scored [1, 7, 9]. In addition, the symptoms were evaluated only once or twice during the first postoperative year, at non-comparable time points, and mainly by using generic quality-of-life instruments (RSC, EORTC QLQ-C30, EOS 24, Moss SF-20SF-36). These multidimensional measures assess various health domains and do not specifically focus on nutrition-related symptoms [7–9, 11, 14, 15, 22, 27, 28].
We developed a questionnaire to evaluate the experienced nutrition-related symptoms prospectively at specific time points during the first postoperative year. After the questionnaires were completed, the responses were always discussed with the patients, and unclear answers or contradictions were clarified.
Another explanation for the difference in findings compared to the literature could be that, with our instrument, questions could only be answered by yes (presence of symptom) or no (absence of symptom), making a gradual alteration of a symptom less obvious. Some of the generic quality-of-life instruments have scaled answer options, making small changes in the experienced nutrition-related symptoms clearer.
A relationship between the nutrition-related symptoms and the type of surgery has been suggested in other studies [6, 7, 10, 27, 29]. As we expected, we found no difference in the number and severity of symptoms between patients who underwent a transhiatal or a transthoracic procedure, making this explanation doubtful in our population.
The findings of Ryan et al. [16], who described an insufficient oral intake at discharge in 60% of their patients after esophagectomy, was confirmed in our study. However, in our study, almost 75% of patients were dependent on enteral nutrition after discharge at some point in time. To our knowledge, our study is the first that has demonstrated the continuing need for nutritional support during a long postoperative period, when early satiety inhibits the consumption of sufficient quantities of food. In accordance with the literature, our patients tended to eat smaller but more frequent meals to compensate for this phenomenon; in cases where tube feeding was mainly used during the first 3 postoperative months, over 20% of the study population still needed sip feeding 2 months after the operation to achieve their nutritional targets [11].
Our research does not support the hypothesis that tube feeding inhibits oral intake, suppresses appetite, and increases satiety in patients after esophagectomy. Stratton et al. showed that tube feeding did not reduce oral intake significantly and had only a slightly negative influence on appetite [30]. According to our hypothesis, the reduced intake and early satiety after esophagectomy are mainly caused by the surgical reconstruction itself.
Although preoperative loss of body weight did occur in 50% of our study population, the mean preoperative BMI was still 26.0 (± 3.9). This finding was also reported by Steyn et al., who noted that preoperative weight loss in patients with esophageal carcinoma did not result per se in underweight, due to the prevalence of overweight or obesity in the Western world [31]. Nevertheless, we must be vigilant with regard to undesired preoperative weight loss in this population, as it associated with postoperative morbidity and therefore needs to be identified and treated at the earliest possible preoperative stage [18–21].
After surgery, both patients and caregivers are focused on undesired weight loss and/or fluctuations in body weight [8, 10–12, 14, 25, 32]. In the present study, we showed that weight loss occurs directly after surgery, followed by a stable reduced postoperative weight. Similar to the findings of Moraca and McLarty, only 25% of our population returned to their preoperative weight one year after surgery [8, 11]. This may explain why the five preoperatively malnourished patients in this study were incapable of gaining weight postoperatively and remained malnourished during the entire postoperative year.
Our follow-up time was probably not long enough to show adaptation, a reduction of nutrition-related symptoms, and an increase in body weight. Although it is assumed that a physically and emotionally stable situation is achieved 6 months after the operation, it is our clinical experience that an actual maximum physical status occurs only 2 or 3 years after the surgery [7, 13].
Studies in patients with esophageal malignancies are invariably handicapped by high mortality and relapse rates of the study subjects; about 40% of the patients dropped out of our study mainly due to recurrence, and ultimately a substantial number of these patients died. However, these rates are comparable with those in the literature, where disease recurrence affects 30% of the patients during the first postoperative year [7].
Regarding our research design, because a substantial number of patients with incomplete follow-up could introduce methodological flaws, we investigated the nutrition-related compliant scores and body weights within the framework of a linear mixed regression technique.
To our knowledge, this is the first study describing nutrition-related symptoms of patients, adjustments, and body weight at multiple, specific time points during a one-year follow-up period after esophagectomy. However, it is unknown whether suffering from a serious number of nutrition-related symptoms after this operation leads to altered food choices and indirectly influences the intake of macro- and micronutrients. Therefore, a study to address the ability of patients to reach their recommended daily intakes of nutrients is being performed.
In conclusion, the present study shows that in the first year after an esophagectomy with gastric tube reconstruction, the majority of patients struggle with persistent nutrition-related symptoms, nutrition-related adjustments in terms of meal size, meal frequency, nutrition-related social aspects, and altered stool frequency. They must also struggle to achieve a sustained body weight. Therefore, at specific postoperative time points, both surgeon and dietitian should inform the patient about the occurrence of postoperative nutrition-related symptoms, which could be persistent. In addition, they should also systematically assess the specific symptoms of each patient, and evaluate the nutritional status of that patient in terms of body weight, to improve the patient’s quality of life and to prevent malnutrition.
Acknowledgments
The authors gratefully acknowledge Joyce T. Haver, RD, Department of Dietetics of the Academic Medical Centre, University of Amsterdam, for her help and support during the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Appendix
Appendix.
The 15 item feeding questionnaire
| No. | Did you experience last week … |
|---|---|
| Section 1. Dysphagia and reflux | |
| 1 | … pain during swallowing |
| 2 | … swallowing the wrong way |
| 3 | … the viscosity inhibits the passage around the cervical suture |
| 4 | … a lump in your throat |
| 5 | … the need to retch as food sticks around the cervical suture |
| 6 | … food returning to your mouth after swallowing as it sticks around the cervical suture |
| 7 | … reflux of food and / or stomach contain towards your mouth |
| 8 | … a painful feeling and / or a feeling of burning behind your breast-bone |
| Section 2. Stomach content and dumping syndrome | |
| 9 | … early satiety |
| 10 | … absence of hunger |
| 11 | … food returning to your mouth after eating too much |
| 12 | … nausea |
| 13 | … vomiting |
| 14 | … one or more complaints ½ an hour to 1 hour after a meala |
| 15 | … one or more complaints 1–2 hours after a mealb |
Items were scored in terms of presence (1 point) or absence (0 point)
aFor example, the need to rest, belly pain, nausea, dizziness, exhausting, blushing, diarrhea, palpitation of the heart, sweating
bFor example, paleness, hunger, restless, dizziness, headache, yawning, palpitation of the heart, sweating, trembling
References
- 1.O’Rourke I, Tait N, Bull C, et al. Oesophageal cancer: outcome of modern surgical management. Aust N Z J Surg. 1995;65:11–16. doi: 10.1111/j.1445-2197.1995.tb01739.x. [DOI] [PubMed] [Google Scholar]
- 2.Bartels H, Stein HJ, Siewert JR. Preoperative risk analysis and postoperative mortality of oesophagectomy for resectable oesophageal cancer. Br J Surg. 1998;85:840–844. doi: 10.1046/j.1365-2168.1998.00663.x. [DOI] [PubMed] [Google Scholar]
- 3.Parshad R, Singh RK, Kumar A, et al. Adenocarcinoma of distal esophagus and gastroesophageal junction: long-term results of surgical treatment in a North Indian Center. World J Surg. 1999;23:277–283. doi: 10.1007/PL00013179. [DOI] [PubMed] [Google Scholar]
- 4.Lerut T, Coosemans W, Decker G, et al. Extended surgery for cancer of the esophagus and gastroesophageal junction. J Surg Res. 2004;117:58–63. doi: 10.1016/j.jss.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Lagarde SM, de Boer JD, ten Kate FJ, et al. Postoperative complications after esophagectomy for adenocarcinoma of the esophagus are related to timing of death due to recurrence. Ann Surg. 2008;247:71–76. doi: 10.1097/SLA.0b013e31815b695e. [DOI] [PubMed] [Google Scholar]
- 6.Finley FJ, Lamy A, Clifton J, et al. Gastrointestinal function following esophagectomy for malignancy. Am J Surg. 1995;169:471–475. doi: 10.1016/S0002-9610(99)80197-4. [DOI] [PubMed] [Google Scholar]
- 7.Wainwright D, Donovan JL, Kavadas V, et al. Remapping the body: learning to eat again after surgery for esophageal cancer. Qual Health Res. 2007;17:759–771. doi: 10.1177/1049732307302021. [DOI] [PubMed] [Google Scholar]
- 8.Moraca RJ, Low DE. Outcomes and health-related quality of life after esophagectomy for high-grade dysplasia and intramucosal cancer. Arch Surg. 2006;141:545–549. doi: 10.1001/archsurg.141.6.545. [DOI] [PubMed] [Google Scholar]
- 9.Blazeby JM, Williams MH, Brookes ST, et al. Quality of life measurement in patients with oesophageal cancer. Gut. 1995;37:505–508. doi: 10.1136/gut.37.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gawad KA, Hosch SB, Bumann D, et al. How important is the route of reconstruction after esophagectomy: a prospective randomized study. Am J Gastroenterol. 1999;94:1490–1496. doi: 10.1111/j.1572-0241.1999.01131.x. [DOI] [PubMed] [Google Scholar]
- 11.McLarty AJ, Deschamps C, Trastek VF, et al. Esophageal resection for cancer of the esophagus: long-term function and quality of life. Ann Thorac Surg. 1997;63:1568–1572. doi: 10.1016/S0003-4975(97)00125-2. [DOI] [PubMed] [Google Scholar]
- 12.De Leyn P, Coosemans W, Lerut T. Early and late functional results in patients with intrathoracic gastric replacement after oesophagectomy for carcinoma. Eur J Cardiothorac Surg. 1992;6:79–84. doi: 10.1016/1010-7940(92)90079-D. [DOI] [PubMed] [Google Scholar]
- 13.Ludwig DJ, Thirlby RC, Low DE. A prospective evaluation of dietary status and symptoms after near-total esophagectomy without gastric emptying procedure. Am J Surg. 2001;181:454–458. doi: 10.1016/S0002-9610(01)00600-6. [DOI] [PubMed] [Google Scholar]
- 14.Baba M, Aikou T, Natsugoe S, et al. Appraisal of ten-year survival following esophagectomy for carcinoma of the esophagus with emphasis on quality of life. World J Surg. 1997;21:282–285. doi: 10.1007/s002689900229. [DOI] [PubMed] [Google Scholar]
- 15.Conroy T, Marchal F, Blazeby JM. Quality of life in patients with oesophageal and gastric cancer: an overview. Oncology. 2006;70:391–402. doi: 10.1159/000099034. [DOI] [PubMed] [Google Scholar]
- 16.Ryan AM, Rowley SP, Healy LA, et al. Post-oesophagectomy early enteral nutrition via a needle catheter jejunostomy: 8-year experience at a specialist unit. Clin Nutr. 2006;25:386–393. doi: 10.1016/j.clnu.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 17.Page RD, Oo AY, Russell GN, et al. Intravenous hydration versus naso-jejunal enteral feeding after esophagectomy: a randomised study. Eur J Cardiothorac Surg. 2002;22:666–672. doi: 10.1016/S1010-7940(02)00489-X. [DOI] [PubMed] [Google Scholar]
- 18.Baldwin C, Weekes CE (2008) Dietary advice for illness-related malnutrition in adults. Cochrane Database of Systematic Reviews Issue 1. Art. No.: CD002008. doi:10.1002/14651858.CD002008.pub3 [DOI] [PubMed]
- 19.Wilson MMG, Vaswani S, Liu D, et al. Prevalence and causes of undernutrition in medical outpatients. Am J Med. 1998;104:56–63. doi: 10.1016/S0002-9343(97)00279-9. [DOI] [PubMed] [Google Scholar]
- 20.Stratton RJ, Green CJ, Elia M (2003) Disease related malnutrition: an evidence-based approach to treatment, 1st edn. CABI Publishing, Cambridge
- 21.Guideline Perioperative Nutrition. Dutch Institute for Healthcare Improvement CBO, Utrecht (2007) http://www.cbo.nl/product.richtlijnen/folder2002102312843/rl_periovoed_07.pdf
- 22.De Boer AG, van Lanschot JJ, van Sandick JW, et al. Quality of life after transhiatal compared with extended transthoracic resection for adenocarcinoma of the esophagus. J Clin Oncol. 2004;22:4202–4208. doi: 10.1200/JCO.2004.11.102. [DOI] [PubMed] [Google Scholar]
- 23.Hulscher JB, Tijssen JG, Obertop H, et al. Transthoracic versus transhiatal resection for carcinoma of the esophagus: a meta-analysis. Ann Thorac Surg. 2001;72:306–313. doi: 10.1016/S0003-4975(00)02570-4. [DOI] [PubMed] [Google Scholar]
- 24.Hulscher JB, van Sandick JW, de Boer AG, et al. Extended transthoracic resection compared with limited transhiatal resection for adenocarcinoma of the esophagus. N Engl J Med. 2002;347:1662–1669. doi: 10.1056/NEJMoa022343. [DOI] [PubMed] [Google Scholar]
- 25.Cense HA, Visser MR, van Sandick JW, et al. Quality of life after colon interposition by necessity for esophageal cancer replacement. J Surg Oncol. 2004;88:32–38. doi: 10.1002/jso.20132. [DOI] [PubMed] [Google Scholar]
- 26.Hölscher AH, Voit H, Buttermann G, et al. Function of the intrathoracic stomach as esophageal replacement. World J Surg. 1988;12:835–844. doi: 10.1007/BF01655491. [DOI] [PubMed] [Google Scholar]
- 27.Viklund P, Lindblad M, Lagergren J. Influence of surgery-related factors on quality of life after esophageal or cardia cancer resection. World J Surg. 2005;29:841–848. doi: 10.1007/s00268-005-7887-9. [DOI] [PubMed] [Google Scholar]
- 28.van Knippenberg FC, Out JJ, Tilanus HW, et al. Quality of life in patients with resected oesophageal cancer. Soc Sci Med. 1992;35:139–145. doi: 10.1016/0277-9536(92)90161-I. [DOI] [PubMed] [Google Scholar]
- 29.Nakamura M, Kido Y, Hosoya Y, et al. Postoperative gastrointestinal dysfunction after 2-field versus 3-field lymph node dissection in patients with esophageal cancer. Surg Today. 2007;37:379–382. doi: 10.1007/s00595-006-3413-4. [DOI] [PubMed] [Google Scholar]
- 30.Stratton RJ, Stubbs RJ, Elia M. Short-term continuous enteral tube feeding schedules did not suppress appetite and food intake in healthy men in a placebo-controlled trial. J Nutr. 2003;133:2570–2576. doi: 10.1093/jn/133.8.2570. [DOI] [PubMed] [Google Scholar]
- 31.Steyn RS, Grenier I, Darnton SJ, et al. Weight gain as an indicator of response to chemotherapy for oesophageal carcinoma. Clin Oncol (R Coll Radiol) 1995;7:382–384. doi: 10.1016/s0936-6555(05)80010-x. [DOI] [PubMed] [Google Scholar]
- 32.Nishihira T, Watanabe T, Ohmori N, et al. Long-term evaluation of patients treated by radical operation for carcinoma of the esophagus. World J Surg. 1984;8:778–785. doi: 10.1007/BF01655780. [DOI] [PubMed] [Google Scholar]


