Abstract
Background
Postoperative adhesions are the most frequent complication of abdominal surgery, leading to high morbidity, mortality, and costs. However, the problem seems to be neglected by surgeons for largely unknown reasons.
Methods
A survey assessing knowledge and personal opinion about the extent and impact of adhesions was sent to all Dutch surgeons and surgical trainees. The informed-consent process and application of antiadhesive agents were questioned in addition.
Results
The response rate was 34.4%. Two thirds of all respondents (67.7%) agreed that adhesions exert a clinically relevant, negative effect. A negative perception of adhesions correlated with a positive attitude regarding adhesion prevention (ρ = 0.182, p < 0.001). However, underestimation of the extent and impact of adhesions resulted in low knowledge scores (mean test score 37.6%). Lower scores correlated with more uncertainty about indications for antiadhesive agents which, in turn, correlated with never having used any of these agents (ρ = 0.140, p = 0.002; ρ = 0.095, p = 0.035; respectively). Four in 10 respondents (40.9%) indicated that they never inform patients on adhesions and only 9.8% informed patients routinely. A majority of surgeons (55.9%) used antiadhesive agents in the past, but only a minority (13.4%) did in the previous year. Of trainees, 82.1% foresaw an increase in the use of antiadhesive agents compared to 64.5% of surgeons (p < 0.001).
Conclusions
The magnitude of the problem of postoperative adhesions is underestimated and informed consent is provided inadequately by Dutch surgeons. Exerting adhesion prevention is related to the perception of and knowledge about adhesions.
Introduction
Postoperative adhesions occur in about 90% of all patients undergoing abdominal surgery and lead to at least one readmission for a third of these patients in the following 10 years [1, 2]. Adhesions become clinically apparent in the form of chronic abdominal pain, female infertility, and small-bowel obstruction [3, 4]. Furthermore, adhesions can seriously complicate subsequent surgery [5, 6]. Therefore, postoperative adhesions should not merely be regarded as a side effect of abdominal surgery but as the most common complication caused by abdominal surgery.
Regardless of an open or a laparoscopic approach, the surgical treatment of adhesions induces the reformation as well as new formation of adhesions [7, 8]. Hence, adhesion prevention is of key importance. For obvious reasons, reducing surgical trauma by meticulous surgical technique is the primary step that needs to be exerted at all times. However, performing surgery implies surgical trauma to some extent but it can be further reduced by other means, e.g., using powder-free gloves, wetting tissues, and reducing operative time [9]. The use of adhesion barriers seems inevitable to obtain further adhesion prevention. A local barrier composed of hyaluronic acid and carboxymethylcellulose (Seprafilm®, Genzyme, Cambridge, MA, USA) has proven effective in reducing adhesions in various open general surgery studies [10]. Previous reviews have also shown significant benefit with the use of Interceed® membrane (Ethicon 360, Johnson & Johnson, New Brunswick, NJ, USA), composed of oxidized regenerated cellulose, in open gynecologic surgery [11]. Administration of an icodextrin solution (Adept®, Baxter Healthcare Corp., Deerfield, IL, USA) that spreads throughout the peritoneal cavity has shown adhesion reductive capacity in benign laparoscopic gynecologic surgery [12].
In contrast to most surgical complications, the risk of adhesion-related morbidity remains for many years and complications are often not followed up by the primary surgeon. In addition, symptoms of adhesion-related complications vary and a fully effective remedy has not yet been discovered. All these factors have probably resulted in an undervaluation of postoperative adhesions by surgeons. This in turn explains why adhesions are mentioned only sporadically during the informed-consent process [13, 14]. Nevertheless, failure to do so can be regarded as an omission of the doctor’s duty of care and has already resulted in successful negligence claims [15].
In spite of the extent and impact of postoperative adhesions, we are under the impression that surgeons lack sufficient awareness about this most common complication. Moreover, they seem to provide inadequate informed consent on and take insufficient preventive actions against adhesions. However, until now, no data has been available to substantiate these assumptions. Therefore, we conducted a nationwide survey assessing the awareness of and behavior toward adhesions among Dutch surgeons and surgical trainees.
Materials and methods
Design of the survey
A steering group of 11 general and gynecologic surgeons with a special interest in adhesions and its associated morbidity (Dutch Adhesion Group) conceived a first set of survey questions. These questions were edited by two independent researchers, both experts in survey and multiple-choice test construction. Subsequently, five surgeons and three surgical trainees tested the survey for indistinctness and leading questions. After making adjustments, the survey was reviewed again and consecutively approved by the steering group, the independent researchers, and the test group of surgeons and trainees. The survey consisted of 55 multiple-choice questions, four open-ended questions, and four optional questions with a total word count of 716. In its final layout, both an electronic online version (six web pages) and a printed version (three pages) were available in Dutch (see the Appendix for a translated version).
Knowledge test
Eight multiple-choice questions concerning the prevalence and morbidity of adhesions were formulated based on up-to-date and best-available evidence. The following statements were considered correct:
Approximately 70% of small-bowel obstructions are due to postoperative adhesions [16–18].
The 5-year readmission rate after operative procedures of the colon or rectum directly related to postoperative adhesions is approximately 5% [19–21].
The 10-year readmission rate after any abdominal surgery probably or directly related to postoperative adhesions is approximately 30% [1, 2].
Inadvertent enterotomy during adhesiolysis occurs in 20% of patients with a history of abdominal surgery [5, 6].
A total colonic resection has the highest risk of adhesion-related morbidity compared with a partial small-bowel resection, an appendectomy, or a resection of the rectum [2, 21].
Age above 60 years is associated with fewer adhesions, a history of abdominal surgery with more adhesions, and a history of Crohn’s disease with no difference in adhesion formation [2, 21].
Survey distribution
We aimed to distribute the survey among all officially registered Dutch surgeons and trainees (n = 1,282 and 432, respectively). Contact details were retrieved from the 2008 annual report of the Dutch Association for Surgery from the section of regular members (n = 1,009) and members of the association of surgical trainees (n = 446). We approached the surgeons and trainees by electronic mail (e-mail) or by postal mail when no or no valid e-mail address was available. A personalized mail was sent on Tuesday (at 6:00 a.m. in case of e-mail) and a reminder sent the next Tuesday (at 7:00 p.m. in case of e-mail) when no response was recorded yet. As an incentive, five portable audio players and 40 pens with inbuilt laser pointer and USB stick were raffled among all respondents. The survey closed 3 weeks after the first mailing.
Data analysis
Only surveys more than 80% complete, excluding optional questions, were included. We defined subgroups of respondents as trainees, general surgeons, gastrointestinal surgeons, or other surgeons. Proportions were compared using χ2 tests. Comparisons between groups were performed using the Mann–Whitney U test, the Wilcoxon signed-rank test, or the Kruskal–Wallis test with post-hoc Bonferroni correction. Knowledge test scores were compared with Student’s t tests and ANOVA with post-hoc Bonferroni correction. Correlations were calculated using Spearman’s rank correlation and a p < 0.050 was considered significant. Statistics were performed using SPSS® version 15.0 (SPSS, Inc., Chicago, IL, USA).
Results
A total of 1,455 surgeons and trainees were contacted by e-mail (83.8%) or postal mail (16.2%). Twenty-three physicians indicated not to participate. After 1 week, 352 surveys were collected, and there were 523 surveys at close of the survey. Of these, 22 incomplete surveys (4.2%) were rejected, resulting in a response rate of 34.4% (501 surveys, 98% complete) representing 90.7% of all Dutch surgical departments (98.3% of all teaching and 81.3% of all nonteaching departments). Response rates were comparable for e-mail and postal mail (35.3 vs. 29.8%, respectively, p = 0.102), but higher for surgeons than for trainees (Table 1). The survey was completed by a comparable number of trainees (n = 131), general surgeons (n = 130), gastrointestinal surgeons (n = 116), and other surgeons (n = 124) (p = 0.767).
Table 1.
Respondents (n = 501)
| Trainees | Surgeons | p Value | |
|---|---|---|---|
| Response rate (%) (n) | 29.4% (131 of 446) | 36.7% (370 of 1,009) | 0.007 |
| Experience, mean (SD) (years) | 4.3 (1.6) | 13.2 (9.6) | n.a. |
| Full-time employment (%) (n) | 89.9% (116) | 88.8% (316) | 0.718 |
| Academic hospital employment (%) (n) | 33.6% (44) | 25.8% (95) | 0.088 |
SD standard deviation; n.a. not applicable
All χ2 tests
Opinion on adhesions
About two thirds (67.7%) of all respondents agreed that adhesions exert a clinically relevant and predominantly negative effect. The proportion was significantly higher for trainees than for surgeons (75.6 vs. 64.9%, respectively, p = 0.025). A small group (6.0%) indicated that adhesions exert a clinically relevant and predominantly positive effect. Half of all respondents (50.6%) considered adhesiolysis for treating pain not effective, whereas 26.2% considered it effective.
Awareness of adhesions and their associated morbidity
Respondents scored a mean of 37.6% correct answers on the knowledge test, with trainees scoring slightly but significantly higher than general surgeons (39.9 vs. 34.6%, p = 0.032). Only 6.9% of respondents reported a correct 10-year readmission rate after abdominal surgery probably or directly related to adhesions (30%), whereas 69.0% thought it was 10% or lower. Also, 62.9% underestimated the percentage of small-bowel obstructions caused by adhesions, reporting a percentage of 50% or lower. On the other hand, a vast majority of respondents (87.6%) correctly indicated that a history of abdominal operations is associated with increased adhesion-related morbidity. The knowledge test score did not correlate with respondents’ opinion on adhesions (ρ = 0.010, p = 0.830).
Informed consent
One in 10 respondents (9.8%) reported that they routinely include adhesions or related morbidity in the informed consent information for both laparotomies and laparoscopies. Yet, 40.9% of all respondents reported that they never mention it at all (Fig. 1). No correlation was observed with opinion on adhesions or knowledge test score (ρ = 0.031, p = 0.497; ρ = 0.016, p = 0.730; respectively). Trainees and nonacademic surgeons provided adhesion information during informed consent less often than surgeons and academic surgeons, respectively (both p = 0.002). Furthermore, providing information on adhesions before a laparoscopic procedure was done less often in comparison with laparotomy (p < 0.001). Informing fewer patients before a laparoscopy correlated with a greater belief that laparoscopy is a means to limit adhesion formation (ρ = 0.186, p < 0.001).
Fig. 1.
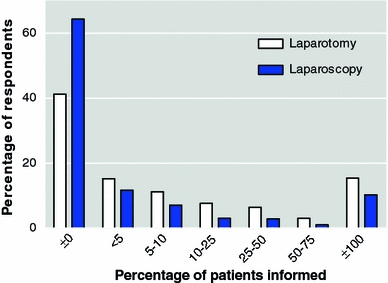
Informed consent
Adhesion prevention
Four in 10 respondents (39.1%) expressed a positive opinion on adhesion prevention, 22.4% expressed a negative one. In addition, a positive opinion correlated with a negative view of adhesions (ρ = 0.182, p < 0.001). All respondents, except gastrointestinal surgeons, believed more strongly in adhesion prevention for specific indications than for all abdominal surgery (p < 0.001). Significantly more surgeons than trainees believed that a meticulous surgical technique minimizes adhesions (83.5 vs. 65.6%, p < 0.001). Similarly, significantly more gastrointestinal than nongastrointestinal surgeons believed that laparoscopy reduces adhesion formation (90.5 vs. 72.0%, p < 0.001) (Fig. 2).
Fig. 2.
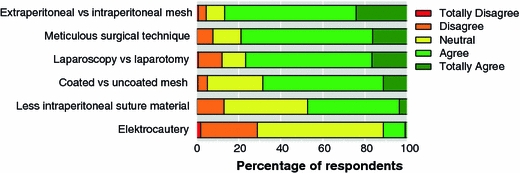
Techniques to minimize adhesions
Antiadhesive agents
Of all respondents, 26.5% expressed a positive attitude toward antiadhesive agents and 29.1% expressed a negative one (Fig. 3). Although a majority of surgeons (55.9%) had used at least one of these agents, only a minority did in the previous year (13.4%). Significantly higher proportions of gastrointestinal and academic surgeons used an antiadhesive agent in the previous year compared to general and nonacademic surgeons, respectively (23.0 vs. 9.0%, p = 0.001; 23.9 vs. 10.5%, p < 0.0001; respectively). Not using antiadhesive agents any longer showed no significant associations with knowledge test score, opinion on adhesions, adhesion prevention, or antiadhesive agents (p = 0.622, p = 0.431, p = 0.283, p = 0.209, respectively). Most surgeons used Adept® (8.9% ever, 8.5% last year) and Seprafilm® (33.7% ever, 5.4% last year). In the group of surgeons who used antiadhesive agents, 78.8% did so in adhesion-related laparotomies, 29.2% in abdominal wall surgery, and 21.8% in (sub)total colectomies. In general, use of products for high-risk operations regarding adhesion formation was higher than for low-risk operations (p < 0.001). Uncertainty about when to use these products correlated with never having used any products (ρ = 0.095, p = 0.035) and lower knowledge test scores (ρ = 0.140, p = 0.002).
Fig. 3.
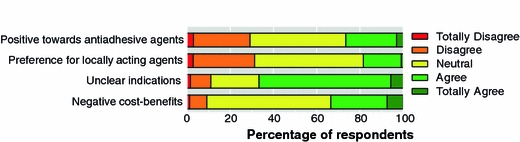
Opinion on antiadhesive agents
Of all trainees, 82.1% predicted that the use of antiadhesive agents will increase compared with 64.5% of all surgeons (p < 0.001). Such opinion correlated with a negative view of adhesions (ρ = 0.141, p = 0.002) and with a more positive view in terms of cost–benefits (ρ = 0.148, p = 0.001). Most respondents anticipated that new antiadhesive agents would come to the market and that the evidence either for or against adhesion prevention would increase.
Discussion
Adhesions and related complications lead to substantial morbidity and mortality, with increased medical costs [22, 23]. This nationwide survey shows that two of three Dutch surgeons recognize adhesions as a clinically relevant and negative entity. However, readmission rates and small-bowel obstructions caused by adhesions are heavily underestimated. Moreover, the informed-consent process and application of antiadhesive agents are not in line with the extent and impact of postoperative adhesions. Therefore, it can be concluded that the knowledge and awareness of and the behavior toward adhesions is limited among Dutch surgeons and surgical trainees.
At least 40% of respondents did not inform any patients about postoperative adhesions or related morbidity and only very few informed patients routinely. This corresponds with the recent finding that more than 90% of consent forms lack this information [13]. In contrast, the risks for hemorrhage and infection after abdominal surgery are almost invariably discussed during the informed-consent process. Adhesion-related complications share nearly all features of these complications, including the risk of death, but may occur many years after the operation. Thus, it is essential to discuss adhesions as a possible complication during the informed-consent process. In addition, in case of any reoperation, a high risk of inadvertent organ damage exists and should be discussed prior to surgery as well. These recommendations apply also for laparoscopic procedures since laparoscopy has not been proven to reduce adhesion-related morbidity compared with laparotomy, though definite studies are lacking [24].
Current surgical trainees consider adhesions a negative drawback of surgery more often, have a slightly better understanding of the extent of the problem, rely less on surgical technique to reduce adhesions, and have a higher belief in an increasing use of antiadhesive agents, compared to surgeons. In contrast, they seem to inform fewer patients about adhesions or adhesion-related morbidity compared to current surgeons. The reason for this is unclear, but this behavior may change when they have more responsibilities and follow-up their own patients more closely. The finding is of interest for the future and might mandate (educational) interventions with this group of young surgeons before they face legal claims. The significantly lower response rate of surgical trainees compared to surgeons can be explained by the higher number of trainees’ contact details than the number of officially registered trainees for general surgery. This is probably due to the fact that plastic and orthopedic surgery trainees share the first 2 years of training.
The current study is the first to evaluate awareness and behavior of surgeons regarding adhesions. Recently, two similar studies reported on adhesion awareness among gynecologic surgeons in the United Kingdom and Germany [14, 25]. Little over half of those respondents agreed that adhesions are the most common complication after abdominal surgery. This is in line with our finding that the impact of adhesions is underestimated. Yet, around three in four gynecologic surgeons indicated that they inform patients routinely about adhesions and about half of the respondents stated that they use antiadhesive agents regularly. This clearly surpasses the current behavior of Dutch surgeons and reflects a higher awareness of adhesions among gynecologic surgeons. Nevertheless, the 8.8% response rate of the British gynecologists and the 33.5% response rate of German gynecologic departments might reflect a selection bias.
Approximately 80% of respondents agreed that an extraperitoneal mesh, meticulous surgical technique, and laparoscopy reduce adhesions. Only a quarter of surgeons expressed a positive opinion toward antiadhesive agents. In addition, only one in 10 surgeons used an agent in the past year, with Adept® taking a small lead over Seprafilm®. Adept® is a liquid acting throughout the whole abdomen; Seprafilm® is a site-specific barrier film. The efficacy of Seprafilm® has already been evidenced in general surgery, whereas for Adept® efficacy has been shown in laparoscopic gynecologic surgery and results in general surgery are awaited [10, 12]. Both agents have been shown to be safe in general abdominal surgery, though application of Seprafilm® on bowel anastomoses should be avoided [10, 26, 27]. Although current agents do not provide complete prevention of postoperative adhesions, it is worth considering their use in high-risk surgery such as colorectal procedures. Even a relative decrease in adhesions might entail benefits for the patient and the surgeon. Interestingly, uncertainty about indications for antiadhesive agents was correlated with never having used any agents and with lower knowledge scores.
This study demonstrates that a change in behavior is needed among surgeons and trainees. Patients have to be informed of the risks of adhesions routinely and the application of clinically available antiadhesive agents should at least be considered in specific abdominal surgery [28]. However, to obtain changes in behavior, both knowledge and attitudes have to be addressed [29]. Barriers for improving knowledge include accessibility and volume of information; attitudes can be affected by a lack of agreement or poor methodology in evidence, but also by personal beliefs and experiences. Therefore, attempts to obtain sustainable changes in behavior have to target multiple aspects. Moreover, breakthrough results from basic research should be translated to clinically applicable agents [30].
Some limitations of this study should be noted. First of all, the 34.4% response rate might reflect a selection bias, possibly providing more positive results. Furthermore, no elaborate nonresponse analysis could be performed due to the lack of any central database comprising detailed information on Dutch surgeons. On the other hand, responses were recorded from 90.7% of all Dutch surgical departments. In addition, response rates were markedly higher than in the recent survey among gynecologic surgeons in the UK and a survey in the USA on work, stress, and research among academic surgeons (8.8 and 22.7%, respectively) [14, 31]. Our relatively high response rate might be due to the raffle, which is known to increase response rates without affecting response quality [32, 33].
The knowledge test was based on up-to-date and best-available evidence selected by the steering group of general and gynecologic surgeons. Several rounds of pilot testing were conducted to ensure comprehensibility and face and content validity of the survey. However, although most of the knowledge questions were based on very large cohort studies, some still consider the consistently found high morbidity controversial. Yet, even if the true morbidity would be lower, many of the respondents would still underestimate the magnitude of the problem.
Finally, this study surveyed only Dutch surgeons and surgical trainees, but results are likely to be generalizable to surgeons worldwide; adhesions are encountered after all abdominal surgeries and the associated morbidity, mortality, and costs are comparably high in different countries [23, 34, 35].
As for the future, action must be taken to improve knowledge, attitude, and behavior concerning adhesions among Dutch surgeons and surgical trainees. Specialty courses could be developed and rewarded credits; compulsory classes on adhesions and antiadhesive agents should be embedded in the surgical training program. Nonetheless, surgeons represent only one of the many parties involved in adhesion awareness. Attention must also be given to the other specialists operating in the abdominal cavity, patients, hospitals, antiadhesive agents manufacturers, and health insurance companies in order to improve awareness of and behavior toward adhesions. In order to follow-up on the actions, the results of this survey can serve as a benchmark for later research.
Acknowledgments
The Dutch Adhesion Group consists of Mrs. E. A. Bakkum (gynecologic surgeon, Amsterdam), Mrs. N. D. Bouvy (surgeon, Maastricht), F. P. Dijkhuizen (gynecologic surgeon, Arnhem), H. van Goor (surgeon, Nijmegen), F. W. Jansen (gynecologic surgeon, Leiden), J. Jeekel (surgeon, Rotterdam), R. F. Kruitwagen (gynecologic surgeon, Maastricht), M. M. Reijnen (surgeon, Arnhem), E. J. van Santbrink (gynecologic surgeon, Rotterdam), D. J. Swank (surgeon, Gouda), and Mrs. G. C. Trimbos-Kemper (gynecologic surgeon, Leiden).
Disclosures
Portable audio players and pens with built-in laser pointer and USB stick were supplied unconditionally and free from any imprints by Johnson & Johnson Medical, Amersfoort, The Netherlands. None of the authors holds any financial interest in Johnson & Johnson Medical nor in any of the companies whose products are mentioned in this study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Appendix: Adhesions survey
Personal data
You are a (multiple responses possible): trainee, general surgeon, oncologic surgeon, vascular surgeon, gastrointestinal surgeon, pediatric surgeon, trauma surgeon, other…
How many years of work experience (as a trainee or as a surgeon) do you have?…
Do you currently work in an academic or nonacademic hospital? Yes/No
Do you currently work full-time or part-time? Yes/No
Prevalence and morbidity of adhesions
Adhesions are not of clinical interest. Totally disagree/Disagree/Neutral/Agree/Totally agree
Adhesions have more beneficial than detrimental effects. Totally disagree/Disagree/Neutral/Agree/Totally agree
Adhesiolysis for complaints of pain is not effective. Totally disagree/Disagree/Neutral/Agree/Totally agree
A proportion of all small-bowel obstructions is caused by postoperative adhesions. This proportion is closest to: 30%/50%/70%/90%
Within 5 years after an operation on the colon or rectum a certain percentage of patients will be readmitted because of morbidity directly related to adhesions. This percentage is closest to: 2%/5%/10%/20%
Within 10 years after an abdominal operation a certain percentage of patients will be readmitted because of morbidity possibly related to adhesions. This percentage is closest to: 5%/10%/20%/30%
Inadvertent bowel lesions caused by adhesiolysis occur in a certain percentage of patients with a history of an abdominal operation. This percentage is closest to: 5%/10%/20%/30%
Which of the following procedures carries with it the highest risk for adhesion-related morbidity? Partial small-bowel resection/appendectomy/total (procto)colectomy/proctectomy
- Some patient characteristics have been proven to influence adhesion formation. What do you think is the influence of:
- Age above 60 years: less adhesions/no effect/more adhesions
- History of abdominal operations: less adhesions/no effect/more adhesions
- Crohn’s disease: less adhesions/no effect/more adhesions
Informed consent
- How many patients do you inform about adhesions or adhesion-related morbidity as a possible complication after
- laparotomy? virtually none/<5%/5–10%/10–25%/25–50%/50–75%/virtually all
- laparoscopy? virtually none/<5%/5–10%/10–25%/25–50%/50–75%/virtually all
Opinion on adhesion prevention
You do not believe in adhesion prevention. Totally disagree/Disagree/Neutral/Agree/Totally agree
You would like to apply adhesion prevention in all abdominal operations. Totally disagree/Disagree/Neutral/Agree/Totally agree
You would like to apply adhesion prevention only in certain indications. Totally disagree/Disagree/Neutral/Agree/Totally agree
Laparoscopic surgery causes fewer adhesions than open surgery. Totally disagree/Disagree/Neutral/Agree/Totally agree
Meticulous surgical technique (tissue handling, avoiding gauzes) reduces adhesions. Totally disagree/Disagree/Neutral/Agree/Totally agree
Extraperitoneal mesh position causes fewer adhesions than the intraperitoneal mesh position. Totally disagree/Disagree/Neutral/Agree/Totally agree
A coated mesh causes fewer adhesions than an uncoated mesh. Totally disagree/Disagree/Neutral/Agree/Totally agree
Electrocautery causes fewer adhesions. Totally disagree/Disagree/Neutral/Agree/Totally agree
Less intraperitoneal suture material reduces adhesions. Totally disagree/Disagree/Neutral/Agree/Totally agree
Opinion on antiadhesive agents
You don’t believe in antiadhesive agents. Totally disagree/Disagree/Neutral/Agree/Totally agree
You experience a lack of clarity about when to use an antiadhesive agent. Totally disagree/Disagree/Neutral/Agree/Totally agree
You prefer using a locally acting antiadhesive agent over an agent that acts throughout the whole abdomen. Totally disagree/Disagree/Neutral/Agree/Totally agree
You think the costs do not outweigh the possible benefits of antiadhesive agents. Totally disagree/Disagree/Neutral/Agree/Totally agree
Which factors influence your belief in adhesion prevention?…
Using antiadhesive agents
Have you ever used:
Interceed, Seprafilm, Adept, Spraygel, Hyalobarrier, Prevadh, Ringers lactate (not regarded an antiadhesive agent), Intercoat, Other… For all agents: Never used, but would like to/Never used/Used in the past year/Ever used
With which operation have you ever used antiadhesive agents? Never/Seldom/Regularly/Often/Very often
Relaparotomy because of adhesion-related morbidity, Pancreatic or duodenal surgery, Partial small-bowel resection, Ileostomy creation, Appendectomy, Partial colectomy, Panproctocolectomy, Laparoscopic colon surgery, Rectal operation, Abdominal wall surgery, Aortic bifurcation prosthesis, Other…
- How many times are antiadhesive agents used by you and your colleagues in your hospital?
- % of all laparotomies…
- % of all laparoscopies…
Do you think this percentage will increase? Yes/No
Why?…
References
- 1.Ellis H, Moran BJ, Thompson JN, et al. Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet. 1999;353:1476–1480. doi: 10.1016/S0140-6736(98)09337-4. [DOI] [PubMed] [Google Scholar]
- 2.Parker MC, Ellis H, Moran BJ, et al. Postoperative adhesions: ten-year follow-up of 12, 584 patients undergoing lower abdominal surgery. Dis Colon Rectum. 2001;44:822–829. doi: 10.1007/BF02234701. [DOI] [PubMed] [Google Scholar]
- 3.Sulaiman H, Gabella G, Davis MC, et al. Presence and distribution of sensory nerve fibers in human peritoneal adhesions. Ann Surg. 2001;234:256–261. doi: 10.1097/00000658-200108000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vrijland WW, Jeekel J, van Geldorp HJ, et al. Abdominal adhesions: intestinal obstruction, pain, and infertility. Surg Endosc. 2003;17:1017–1022. doi: 10.1007/s00464-002-9208-9. [DOI] [PubMed] [Google Scholar]
- 5.Van Der Krabben AA, Dijkstra FR, Nieuwenhuijzen M, et al. Morbidity and mortality of inadvertent enterotomy during adhesiotomy. Br J Surg. 2000;87:467–471. doi: 10.1046/j.1365-2168.2000.01394.x. [DOI] [PubMed] [Google Scholar]
- 6.Wullstein C, Gross E. Laparoscopic compared with conventional treatment of acute adhesive small bowel obstruction. Br J Surg. 2003;90:1147–1151. doi: 10.1002/bjs.4177. [DOI] [PubMed] [Google Scholar]
- 7.Szomstein S, Lo Menzo E, Simpfendorfer C, et al. Laparoscopic lysis of adhesions. World J Surg. 2006;30:535–540. doi: 10.1007/s00268-005-7778-0. [DOI] [PubMed] [Google Scholar]
- 8.Wiseman DM, Trout JR, Diamond MP. The rates of adhesion development and the effects of crystalloid solutions on adhesion development in pelvic surgery. Fertil Steril. 1998;70:702–711. doi: 10.1016/S0015-0282(98)00270-2. [DOI] [PubMed] [Google Scholar]
- 9.van den Tol MP, Haverlag R, van Rossen ME, et al. Glove powder promotes adhesion formation and facilitates tumour cell adhesion and growth. Br J Surg. 2001;88:1258–1263. doi: 10.1046/j.0007-1323.2001.01846.x. [DOI] [PubMed] [Google Scholar]
- 10.Kumar S, Wong PF, Leaper DJ (2009) Intra-peritoneal prophylactic agents for preventing adhesions and adhesive intestinal obstruction after non-gynaecological abdominal surgery. Cochrane Database Syst Rev 1:CD005080 [DOI] [PubMed]
- 11.Wiseman DM, Trout JR, Franklin RR, et al. Meta-analysis of the safety and efficacy of an adhesion barrier (Interceed TC7) in laparotomy. J Reprod Med. 1999;44:325–331. [PubMed] [Google Scholar]
- 12.Brown CB, Luciano AA, Martin D, et al. Adept (icodextrin 4% solution) reduces adhesions after laparoscopic surgery for adhesiolysis: a double-blind, randomized, controlled study. Fertil Steril. 2007;88:1413–1426. doi: 10.1016/j.fertnstert.2006.12.084. [DOI] [PubMed] [Google Scholar]
- 13.Rajab TK, Wallwiener M, Talukdar S, et al. Adhesion-related complications are common, but rarely discussed in preoperative consent: a multicenter study. World J Surg. 2009;33:748–750. doi: 10.1007/s00268-008-9917-x. [DOI] [PubMed] [Google Scholar]
- 14.Trew G, Cooke I, Lower A, et al. Post-operative abdominal adhesions—awareness of UK gynaecologists—a survey of members of the Royal College of Obstetricians and Gynaecologists. J Gynecol Surg. 2009;6:25–37. doi: 10.1007/s10397-008-0409-7. [DOI] [Google Scholar]
- 15.Ellis H, Crowe A. Medico-legal consequences of post-operative intra-abdominal adhesions. Int J Surg. 2009;7:187–191. doi: 10.1016/j.ijsu.2009.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Miller G, Boman J, Shrier I, et al. Etiology of small bowel obstruction. Am J Surg. 2000;180:33–36. doi: 10.1016/S0002-9610(00)00407-4. [DOI] [PubMed] [Google Scholar]
- 17.Miller G, Boman J, Shrier I, et al. Natural history of patients with adhesive small bowel obstruction. Br J Surg. 2000;87:1240–1247. doi: 10.1046/j.1365-2168.2000.01530.x. [DOI] [PubMed] [Google Scholar]
- 18.Bizer LS, Liebling RW, Delany HM, et al. Small bowel obstruction: the role of nonoperative treatment in simple intestinal obstruction and predictive criteria for strangulation obstruction. Surgery. 1981;89:407–413. [PubMed] [Google Scholar]
- 19.Edna TH, Bjerkeset T. Small bowel obstruction in patients previously operated on for colorectal cancer. Eur J Surg. 1998;164:587–592. doi: 10.1080/110241598750005688. [DOI] [PubMed] [Google Scholar]
- 20.Beck DE, Opelka FG, Bailey HR, et al. Incidence of small-bowel obstruction and adhesiolysis after open colorectal and general surgery. Dis Colon Rectum. 1999;42:241–248. doi: 10.1007/BF02237135. [DOI] [PubMed] [Google Scholar]
- 21.Parker MC, Wilson MS, Menzies D, et al. The SCAR-3 study: 5-year adhesion-related readmission risk following lower abdominal surgical procedures. Colorectal Dis. 2005;7:551–558. doi: 10.1111/j.1463-1318.2005.00857.x. [DOI] [PubMed] [Google Scholar]
- 22.Stanciu D, Menzies D. The magnitude of adhesion-related problems. Colorectal Dis. 2007;9(Suppl 2):35–38. doi: 10.1111/j.1463-1318.2007.01346.x. [DOI] [PubMed] [Google Scholar]
- 23.Wilson MS. Practicalities and costs of adhesions. Colorectal Dis. 2007;9(Suppl 2):60–65. doi: 10.1111/j.1463-1318.2007.01360.x. [DOI] [PubMed] [Google Scholar]
- 24.Lower AM, Hawthorn RJ, Clark D, et al. Adhesion-related readmissions following gynaecological laparoscopy or laparotomy in Scotland: an epidemiological study of 24 046 patients. Hum Reprod. 2004;19:1877–1885. doi: 10.1093/humrep/deh321. [DOI] [PubMed] [Google Scholar]
- 25.Hackethal A, Sick C, Brueggmann D, et al. Awareness and perception of intra-abdominal adhesions and related consequences: survey of gynaecologists in German hospitals. Eur J Obstet Gynecol Reprod Biol. 2010;150(2):180–189. doi: 10.1016/j.ejogrb.2010.02.017. [DOI] [PubMed] [Google Scholar]
- 26.Beck DE, Cohen Z, Fleshman JW, et al. A prospective, randomized, multicenter, controlled study of the safety of Seprafilm adhesion barrier in abdominopelvic surgery of the intestine. Dis Colon Rectum. 2003;46:1310–1319. doi: 10.1007/s10350-004-6739-2. [DOI] [PubMed] [Google Scholar]
- 27.Menzies D, Pascual MH, Walz MK, et al. Use of icodextrin 4% solution in the prevention of adhesion formation following general surgery: from the multicentre ARIEL Registry. Ann R Coll Surg Engl. 2006;88:375–382. doi: 10.1308/003588406X114730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Parker MC, Wilson MS, van Goor H, et al. Adhesions and colorectal surgery—call for action. Colorectal Dis. 2007;9(Suppl 2):66–72. doi: 10.1111/j.1463-1318.2007.01342.x. [DOI] [PubMed] [Google Scholar]
- 29.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 30.Kosaka H, Yoshimoto T, Yoshimoto T, et al. Interferon-gamma is a therapeutic target molecule for prevention of postoperative adhesion formation. Nat Med. 2008;14:437–441. doi: 10.1038/nm1733. [DOI] [PubMed] [Google Scholar]
- 31.Chokshi NK, Simeone DM, Chari RS, et al. A survey of academic surgeons: work, stress, and research. Surgery. 2009;146:462–468. doi: 10.1016/j.surg.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 32.Dirmaier J, Harfst T, Koch U, et al. Incentives increased return rates but did not influence partial nonresponse or treatment outcome in a randomized trial. J Clin Epidemiol. 2007;60:1263–1270. doi: 10.1016/j.jclinepi.2007.04.006. [DOI] [PubMed] [Google Scholar]
- 33.Edwards PJ, Roberts I, Clarke MJ et al (2009) Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 3:MR000008 [DOI] [PMC free article] [PubMed]
- 34.Jeekel H. Cost implications of adhesions as highlighted in a European study. Eur J Surg. 1997;163(Suppl 579):43–45. [PubMed] [Google Scholar]
- 35.Tingstedt B, Isaksson J, Andersson R. Long-term follow-up and cost analysis following surgery for small bowel obstruction caused by intra-abdominal adhesions. Br J Surg. 2007;94:743–748. doi: 10.1002/bjs.5634. [DOI] [PubMed] [Google Scholar]


