Abstract
Objective:
Patients with chronic obstructive pulmonary disease (COPD) and comorbid mental disorders are known to have worse health status. The association between these variables remains complex and poorly understood. We sought to better understand the association between COPD severity, mental disorders (depression/anxiety), and health status.
Method:
This cross-sectional study compared participants without COPD or with mild COPD (n = 162) to those with moderate (n = 25), severe (n = 38), and very severe (n = 26) COPD. We recruited participants from a primary care and a pulmonary clinic at a veterans affairs medical center between July 2001 until September 2002. We used the Patient Health Questionnaire to screen for depression and anxiety and the Posttraumatic Stress Disorder Checklist to screen for posttraumatic stress disorder. Health status was assessed with the veteran's version of the Medical Outcomes Study 36-item Short-Form Health Survey (SF-36) and the Shortness of Breath Questionnaire (SOBQ).
Results:
COPD severity was associated with worse physical status and dyspnea as measured by the SF-36 physical component summary and the SOBQ but was not associated with worse mental status as measured by the SF-36 mental component summary. At each level of COPD severity, participants with mental disorders had worse health status and dyspnea as measured by the SF-36 physical component summary, mental component summary, and SOBQ. Significant linear trends with COPD severity were associated with increased prevalence of any depressive disorder, major depressive disorder, and nonpanic/non-PTSD anxiety disorders (all tests for linear trend, P < .01).
Conclusions:
Independent of COPD severity, comorbid mental disorders were associated with worse health status and dyspnea. Studies are needed to determine whether patients with comorbid mental disorders may have more significant improvement in physical symptoms and functioning if providers focus more on psychiatric conditions.
Chronic obstructive pulmonary disease (COPD) is a highly prevalent condition among veteran populations and is associated with significant impairments in health-related quality of life (HRQOL).1–12 The prevalence of mental disorders, such as depressive and anxiety disorders, has been reported to be higher among patients with COPD than among those patients without COPD. Depending on how mental health disorders are defined, the prevalence of depressive disorders has ranged between 6%–42%, and prevalence of anxiety disorders has ranged between 1%–32%.13–26 The individual effects of depression, anxiety, and COPD on HRQOL have been examined in prior studies and suggest HRQOL is worse among patients with both COPD and depressive or anxiety disorders.2,3,7–10,27–29
Clinical Points
♦Regardless of the severity of chronic obstructive pulmonary disease (COPD), patients with COPD and comorbid depressive/anxiety disorder have worse perceived dyspnea and physical health-related quality of life than patients with COPD alone.
♦Worsening mental health status is not associated with worsening severity of COPD.
There are limited data about the complex relationship between anxiety and/or depressive symptoms and their association with generic and condition-specific HRQOL in a single outpatient population. Recent work reported that anxiety and depressive symptoms in patients with COPD contributed more to the variance in function of patients with COPD than symptoms contributed by medical burden and COPD severity alone.8,10 We sought to further explore the influence of depressive and anxiety symptoms on functional status of patients with a range of COPD severity. We hypothesized that participants with COPD and comorbid mental disorders would report greater impairment in general and condition-specific HRQOL and that COPD severity would be associated with a higher prevalence of depressive and anxiety disorders.
METHOD
This cross-sectional study compared participants without COPD or mild COPD to those participants with COPD who had moderate, severe, and very severe airflow obstruction with regard to variables related to health status and the prevalence of comorbid mental disorders. Participants were enrolled between July 2001 until September 2002. Institutional Review Board approval was granted through the Human Subjects Division of the University of Washington and Veterans Affairs (VA) Puget Sound Health Care System (VAPSHCS), Seattle, Washington.
Setting and Participants
Veterans who received outpatient care from either the Chest Clinic or the General Internal Medicine Clinic (GIMC) at the VAPSHCS, Seattle Division, were enrolled. Participants with a known clinician diagnosis of COPD who presented for routine appointments in the Chest Clinic were consecutively approached by trained research assistants and invited to participate in the study. Using a random number generator, GIMC patients were selected from a list of patients to be seen that day. After the informed consent process with a trained research assistant, spirometry was collected on participants from both the Chest Clinic and GIMC using a hand-held device (Sensormedics Spiropro30). The Global Initiative for Chronic Obstructive Lung Disease (GOLD) was used to determine the presence of airflow limitation and the severity of COPD.31
A total of 568 participants were invited to participate from both the GIMC (n = 418, 74%) and the Chest Clinic (n = 150, 26%). Informed consent and spirometry were obtained from 228 GIMC patients (55% of those approached) and from 117 Chest Clinic patients (78% of those approached). Consenting participants with spirometry data were excluded for the following reasons: diagnosis of asthma (n = 34), did not complete the self-report assessment (n = 32), younger than age 45 years (n = 16), diagnosis of lung cancer (n = 9), or being female (n = 3).
Participants were considered to have COPD only if they had a clinician-documented diagnosis of COPD along with spirometric values as defined by GOLD criteria.31 Participants recruited from the GIMC who were not found to have COPD were included to be part of the non-COPD comparison group. On the basis of previous work showing minimal clinical difference and association with HRQOL between the absence of COPD and mild COPD, we chose to pool those subjects with mild COPD in the control group without COPD so that we could focus our analyses on those participants with moderate to very severe COPD.8,10,32–36
Hence, we compared those with moderate, severe, and very severe COPD to the comparison group that consisted of those participants with no or mild COPD as defined by GOLD criteria.31 Participants in the COPD categories included moderate (n = 25), severe (n = 38), and very severe (n = 26) COPD. The 162 participants who did not have a diagnosis of COPD or who had mild COPD served as the comparison group.
Data and Instruments
All questionnaires were self-administered. Research assistants were available to assist with clarifications. We assessed sociodemographic information including race and income, as well as past and current smoking status and body mass index (BMI [kg/m2]). We used the previously validated Patient Health Questionnaire (PHQ)37 to assess major depressive disorders, other depressive disorders, panic disorders, and other anxiety disorders. PHQ criteria for the diagnosis of major depressive disorder are consistent with that of the DSM-IV.38
The “other depressive disorder” category is consistent with DSM-IV criteria and requires 2 to 4 symptoms present “more than half the days” in the past 2 weeks with 1 of the symptoms being depressed mood or anhedonia. The PHQ diagnoses of panic disorder and other anxiety disorders are consistent with DSM-IV diagnostic criteria.38 As the PHQ does not assess for posttraumatic stress disorder (PTSD), which is prevalent in the veteran population, we used the Posttraumatic Stress Disorder Checklist (PCL),39 a 17-item validated screen for PTSD. A cutoff score of ≥ 50 was used to identify those participants who likely had PTSD.39 Given the high rate of alcohol misuse disorders and their potential impact on HRQOL, we used the Alcohol Use Disorders Identification Test (AUDIT),40 a 10-item validated screen for hazardous alcohol use or alcohol abuse or dependence. An AUDIT score > 8 indicates significant risk of alcohol use disorders.
General HRQOL was assessed by the veteran's version of the Medical Outcomes Study 36-item Short-Form Health Survey (SF-36).41 The SF-36 has been validated among patients with COPD.42,43 The SF-36 evaluates general HRQOL on 8 scales related to the participant's mental and physical health status. The SF-36 also generates 2 summary scales: the mental component summary (MCS) and the physical component summary (PCS).41 The Shortness of Breath Questionnaire (SOBQ) is a validated, disease-specific scale that measures the influence of dyspnea on HRQOL.44 Participants provided informed consent and were paid $5 for completing the assessment.
Data Analysis
We tested for differences between COPD severity groups and depressive/anxiety disorders (present/absent) using 2-way analysis of variance (ANOVA) with quality of life measures as the dependent variable. Separate models were run adjusting for potential confounders. Differences in demographics by COPD severity were assessed using ANOVA (for age and BMI) and χ2 tests (all other variables). Those variables that had differences by COPD severity were considered potential confounders and were included as covariates in subsequent models. Logistic regression was used to detect associations between COPD severity and presence/absence of depressive/anxiety disorders.
We were interested not only in whether there were differences across groups, but also, more specifically, if the proportion of patients with depressive/anxiety disorders was progressively higher in groups with greater severity of COPD. Thus, we assessed linear trends in proportions with depressive/anxiety disorders using polynomial contrasts for the 4-category COPD severity variable.
All data analyses were conducted using the Statistical Package for the Social Sciences for Windows Version 11,45 MS Access,46 and R 2.4.1.47
RESULTS
Table 1 summarizes the sociodemographic information of the participants. COPD severity was strongly related to BMI, with mean BMI tending to be lower in participants with moderate to very severe COPD when compared to participants with no COPD (Table 1). History of smoking in the past year was found more frequently in the moderate COPD category than in the other categories. There were also smaller proportions of married participants in the moderate and very severe categories than in the other 2 categories.
Table 1.
Demographics by Chronic Obstructive Pulmonary Disease (COPD) Severity
| Demographics | Mild or No COPD (n = 162) | Moderate COPD (n = 25) | Severe COPD (n = 38) | Very Severe COPD (n = 26) | P Value |
| Age, mean ± SD, y | 64.8 ± 11.3 | 68.0 ± 10.6 | 66.9 ± 8.9 | 67.5 ± 8.9 | .3 |
| Nonwhite, %a | 14 | 12 | 11 | 12 | 1.0 |
| Married, % | 63 | 40 | 66 | 42 | .045 |
| Some college or more, %b | 50 | 60 | 58 | 64 | .5 |
| Income > $25,000/y, % | 43 | 35 | 45 | 42 | .9 |
| Body mass index (kg/m2), mean ± SDc | 29.9 ± 5.3 | 27.3 ± 5.6 | 28.1 ± 6.5 | 25.1 ± 6.7 | .0003 |
| Smoked in the past year, %c | 24 | 52 | 32 | 35 | .023 |
| Alcohol Use Disorders Identification Test score ≥ 8, %a | 8 | 12 | 11 | 15 | .5 |
Four subjects with missing data.
Ten subjects with missing data.
Two subjects with missing data.
Table 2.
Percentage of Subjects With Depressive or Anxiety Disorders by Chronic Obstructive Pulmonary Disease (COPD) Status
| Variable | Mild or No COPD (n = 162) | Moderate COPD (n = 25) | Severe COPD (n = 38) | Very Severe COPD (n = 26) | P Valuea |
| Any depressive or anxiety disorderb | 23 | 28 | 34 | 50 | .044* |
| Any depressive disorder | 19 | 20 | 21 | 50 | .018* |
| Major depressive disorder | 9 | 12 | 11 | 31 | .020* |
| Other depressive disorder | 10 | 8 | 11 | 19 | .6 |
| Any anxiety disorder | 15 | 16 | 16 | 27 | .4 |
| Panic disorder | 10 | 8 | 8 | 4 | 1.0 |
| Other anxiety disorder | 8 | 4 | 6 | 27 | .036 |
| PTSD (PTSD Checklist score ≥ 50) | 10 | 12 | 11 | 12 | .9 |
Logistic regression of depression/anxiety outcome on COPD severity adjusted for age, body mass index, marital status, and smoking history.
Depressive and anxiety disorders defined by the Patient Health Questionnaire.
*A significant linear trend (P < .01).
Abbreviation: PTSD = posttraumatic stress disorder.
Presence of any depressive or anxiety disorder increased significantly with COPD severity (Table 2). In comparison to the no or mild COPD group, the unadjusted odds (95% confidence intervals) of any depressive or anxiety disorder were 1.4 (0.5–3.9) for moderate COPD, 2.1 (0.9–4.5) for severe COPD, and 3.6 (1.4–9.3) for very severe COPD. Large absolute differences were observed between severe (34%) and very severe categories (50%). Among subcategories of depression/anxiety disorders, the significant linear associations with COPD were any depressive disorders and major depressive disorders (all tests for linear trend, P < .01). Again, the largest absolute differences across successive COPD categories occurred between the severe and very severe categories (Table 2). Models adjusted for BMI, age, marital status, and smoking history yielded similar results.
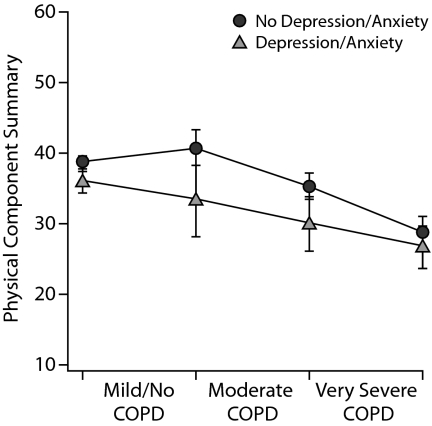
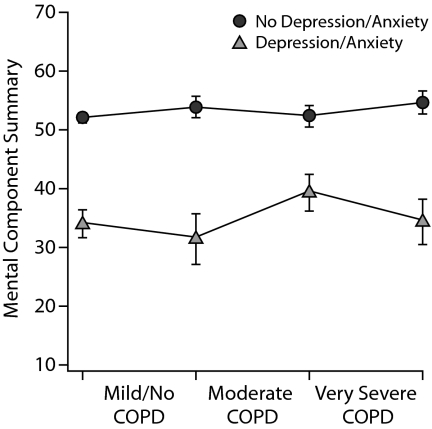
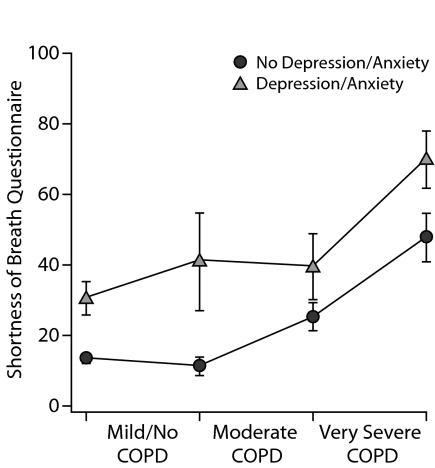
COPD severity was significantly and linearly associated with lower HRQOL as measured by mean SF-36 PCS and SOBQ scores (Table 3 and Figure 1). There was also a significant quadratic component with the most impaired mean SOBQ score seen in the very severe COPD category. There was no significant association between COPD severity and the SF-36 MCS. There were no significant interactions between COPD severity and presence of depressive/anxiety disorder in the 2-way ANOVA models of the 3 HRQOL measures, ie, the association of HRQOL with COPD severity was consistent regardless of the presence of depressive/anxiety disorders. Similarly, compared to participants without depressive/anxiety disorders, those with depressive/anxiety disorders had significantly worse mean HRQOL scores across all COPD categories. Thus, COPD severity (in particular, severe and very severe COPD) and presence of depressive/anxiety disorder were independently associated with significantly worse HRQOL as measured by the PCS and the SOBQ. In summary, the clinical effects of depression and anxiety as reflected by scores on the PCS, MCS, and SOBQ were substantial. This patient-reported burden (as measured by these instruments) was differential across disease severity.
Table 3.
Mean ± SD for SF-36 Physical Function and Mental Function Component Scores and the Summary SOBQ Score by Chronic Obstructive Pulmonary Disease (COPD) Severity and Presence of Depressive or Anxiety Disorders
| Mild or No COPD (n = 162) | Moderate COPD (n = 25) | Severe COPD (n = 38) | Very Severe COPD (n = 26) |
P Valuea |
||
| Variable | COPD | Depression/ Anxiety | ||||
| SF-36 physical component summaryb | ||||||
| No depression/anxietycd | 38.7 ± 10.5 | 40.8 ± 10.6 | 35.3 ± 9.3 | 28.9 ± 7.6 | ||
| Depression/anxietyce | 35.9 ± 9.3 | 33.3 ± 13.4 | 29.9 ± 14.0 | 26.7 ± 10.7 | .0002 (L) | .0034 |
| SF-36 mental component summaryb | ||||||
| No depression/anxiety | 52.1 ± 8.9 | 53.9 ± 8.0 | 52.4 ± 8.5 | 54.7 ± 6.9 | ||
| Depression/anxiety | 34.2 ± 13.2 | 31.6 ± 11.4 | 39.4 ± 11.3 | 34.5 ± 13.9 | .7 | < .0001 |
| Shortness of Breath Questionnairecf | ||||||
| No depression/anxiety | 13.2 ± 15.2 | 10.9 ± 9.8 | 25.0 ± 18.9 | 47.5 ± 24.8 | ||
| Depression/anxiety | 30.1 ± 28.4 | 40.7 ± 34.0 | 39.1 ± 30.8 | 69.6 ± 28.9 | < .0001 (LQ) | < .0001 |
Two-way analysis of variance on COPD severity and depression/anxiety outcome. “L” and “LQ” indicate significant linear and quadratic trends (p < .01) across COPD severity adjusted for age, body mass index, marital status, and smoking history.
Higher score associated with better function; 14 participants with missing scores.
Depression/anxiety represents depressive and anxiety disorders as defined by the Patient Health Questionnaire.
n = 180.
n = 71.
Lower score associated with better function; 11 participants had missing scores; there were no significant COPD × depression/anxiety interactions (P > .3).
Abbreviation: SF-36 = Medical Outcomes Study 36-item Short-Form Health Survey.
Figure 1.
General and Condition-Specific Health-Related Quality of Life (mean ± SD) by Chronic Obstructive Pulmonary Disease (COPD) Severitya
aCOPD vs physical component summary: P = .0002, COPD vs mental component summary: P = .7, COPD vs Shortness of Breath Questionnaire: P < .0001.
DISCUSSION
In this sample of older male veteran outpatients, those with COPD and a comorbid depressive/anxiety disorder reported worse physical HRQOL as measured by the PCS, worse perceived dyspnea and function as measured by the SOBQ, and worse mental HRQOL as measured by the MCS than those patients with COPD and without a comorbid depressive/anxiety disorder. The clinical effects of depression/anxiety disorders on PCS, MCS, and SOBQ were substantial. These results are important in that the patient's reported burden (as measured by these instruments) was differential across disease severity. Once stratified by the presence of depressive/anxiety disorder, mental HRQOL as measured by the MCS was not associated with severity of COPD.
There were no significant interactions between COPD severity and the presence of a depressive/anxiety disorder. Hence, the association of HRQOL with COPD severity was consistent regardless of the presence of a depressive/anxiety disorder. In addition, COPD severity and the presence of a depressive/anxiety disorder were independently associated with HRQOL on the PCS and SOBQ outcome measures that focus more on physical function. The differences between those participants with and without comorbid depressive/anxiety disorders are considered to be clinically relevant and statistically significant for all participants except for those with very severe COPD as measured on the PCS (Figure 1).48 As COPD severity increased, there was a significant linear trend for increasing rates of any depressive/anxiety disorder.
The literature is clear that patients with COPD are well known to have impaired HRQOL on scales that measure both disease-specific and general HRQOL.2–5,48,49 Patients with COPD and comorbid anxiety and depressive symptoms have also been shown to have lower HRQOL as measured by general and disease-specific HRQOL scales.9,10,14,15,29 As COPD severity worsens or as mental disorder comorbidity is added, one would expect HRQOL to worsen. However, understanding the interactions and associations of these variables has been complicated. Previous studies on the association between HRQOL and COPD severity have focused on the correlation with spirometry; however, this correlation has been weak to moderate.5,15,29,49 Thus, it appears that factors other than spirometry influence HRQOL in patients with COPD.
One study examined the amount of variance that depressive symptoms accounted for on scales related to HRQOL.29 As expected, the greatest amount of variance was found on scales that measured mental health (32%–52%). However, on those scales that focus on physical symptom factors, 11%–18% of the variance could be attributed to depressive symptoms.29 However, this study did not consider COPD severity or the role of comorbid anxiety disorders.29 Another study did explore the role of anxiety as well as depressive disorders and, though the sample size was low, similarly reported that depression and anxiety significantly contributed to the overall variance in functional status beyond that attributed to the medical burden of COPD severity.8
In a larger study, Cully et al10 evaluated 179 subjects from a randomized controlled trial of cognitive-behavioral therapy in patients with COPD. Patients stratified by moderate to very severe COPD were evaluated and the association with depressive/anxiety disorders with regard to health status was explored. Cully et al reported that in a sample of patients with COPD, mental health distress accounts for a significant amount of variance in quality of life above and beyond the contribution of COPD severity, medical comorbidity, and patient demographic factors.10 It was also reported that the role of anxiety and depression symptoms had a role in mental health outcomes, but only anxiety symptoms had an association with physical functioning, general health, and disease-specific outcomes. Cully et al called for further studies to better understand the relationship between COPD depression and anxiety.10
The results reported here support these previous findings related to the association between COPD severity, depression, and anxiety symptoms while further clarifying the complicated interactions between these variables. We found in this population that the presence of comorbid depressive/anxiety disorders was associated with impairments in HRQOL on scales that measure both general and disease-specific HRQOL. This association was consistent across all COPD categories. As expected, the greatest impact of the comorbid depressive/anxiety disorders was seen on the MCS of the SF-36. One would suspect that as severity of COPD worsened, mental health function would also significantly worsen. Interestingly, mental health status was not associated with worsening severity of COPD. It is not clear why mental health status did not worsen with COPD severity. Perhaps participants became more focused on their perceived physical symptoms and functional status related to these physical symptoms. When one considers those with COPD and comorbid depressive/anxiety disorders, there was a marked reduction in HRQOL on the PCS of the SF-36 and the SOBQ, a disease-specific measure of HRQOL. Items from the SOBQ focus on perceived shortness of breath while participating in activities of daily living. These findings suggest that the presence of comorbid depressive or anxiety disorders might influence one's subjective perception of physical health. This finding might help to explain why patients with COPD and comorbid depressive symptoms have been associated with poorer survival, longer hospital stays, persistent smoking, increased symptom burden, and worse physical and social function.50
As noted in the introduction, the prevalence of depressive and anxiety disorders in patients with COPD is high. However, the range of reported prevalence rates is large. This is likely related to the use of different diagnostic scales in different clinical populations. However, in further understanding the prevalence of comorbid depressive and anxiety disorders in patients with COPD, stratifying the severity of the COPD may be important. One study examined the prevalence of depression in subjects with COPD.21 It was reported that although patients with mild to moderate COPD (forced expiratory volume in 1 second [FEV1] 50%–80%) were not at greater risk for depression than controls, patients with severe COPD (FEV1 < 50%) were 2.5 times more likely to suffer from depression than controls.21 Our results were similar to these reports. Among participants with moderate, severe, and very severe COPD, compared to those participants with no or mild COPD, we did find a significant trend toward increasing rates of depressive/anxiety disorders. Among the subcategories of depressive/anxiety disorders, significant linear trends with COPD severity were observed for any depressive disorder, major depressive disorder, and nonpanic/non-PTSD anxiety disorders.
Limitations of this study include inclusion of a population of older veteran outpatients. In addition, this study did not include any women, who are known to suffer from higher rates of anxiety and/or depressive disorders. Therefore, these findings may not generalize to the general population. Another limitation includes the cross-sectional design. Therefore, we are unable to draw conclusions about causation between independent and dependent variables. In addition, the scales used for this study (though all validated) were all self-report and can be influenced by other patient factors. In this study, we did not evaluate subjects with regard to the presence of psychotropic medications. Subjects may have been treated or partially treated for depressive and anxiety disorders, and these potential treatments could influence prevalence rates for these disorders and HRQOL. We also did not control for medications or comorbid medical disorders that may have influenced the prevalence of depressive and anxiety disorders in this population. Finally, the sample sizes for the moderate and very severe COPD categories were relatively small, thus limiting the power to detect differences, especially in the logistic regression analyses of depression/anxiety and in detecting interactions between COPD and depression/anxiety in the ANOVA models on the HRQOL measures. Lack of significance in these analyses should be interpreted with caution.
In this sample of outpatient male veterans, those patients with COPD and comorbid depressive/anxiety disorders had worse general and disease-specific HRQOL for both physical function and mental health function regardless of the severity of COPD. This finding may imply that treatment based on guidelines may need to be modified in 2 ways: (1) there may need to be greater emphasis on detecting these conditions and (2) it is likely that pharmacologic therapy for those with mental health disorders is likely to be less effective for dyspnea. This finding further suggests that interventions should be designed to test the effects of treating the patient more broadly (such as comprehensive pulmonary rehabilitation programs) or that mental health should be integrated into such programs. These findings are also important in that organized treatment approaches for COPD that take into account depressive and anxiety symptoms may improve function and quality of life.7,29,51–54
Disclosure of off-label usage: The authors have determined that, to the best of their knowledge, no investigational information about pharmaceutical agents that is outside US Food and Drug Administration−approved labeling has been presented in this article.
Financial disclosure: Dr Au is a consultant for Nexus. Drs Felker, Harel, and Shores and Mss Bush and Shofer have no personal affiliations or financial relationships with any commercial interest to disclose relative to the article.
Funding/support: Dr Au was funded by a VA Health Services Research and Development Career Development Award. A Department of Veteran Affairs Epidemiologic Research Information Center Grant EPC 97-010 supported this work. This material is based upon work supported by the Health Services R&D Service, the VA Puget Sound Mental Illness Research and Education Clinical Center, and the Center of Excellence in Substance Abuse Treatment and Education, VA Puget Sound Health Care System, VA Puget Sound Geriatric Research, Education and Clinical Center, Seattle, Washington.
Disclaimer: All work was performed at the Department of Veterans Affairs, Puget Sound Health Care System, Seattle, Washington.
Footnotes
CME Background
Articles are selected for credit designation based on an assessment of the educational needs of CME participants, with the purpose of providing readers with a curriculum of CME articles on a variety of topics throughout each volume. Activities are planned using a process that links identified needs with desired results.
To obtain credit, read the material and go to PSYCHIATRIST.COM to complete the Posttest and Evaluation online.
CME Objective
- Recognize that depressive and anxiety disorders are potential mediators of dyspnea and health status in patients with chronic obstructive pulmonary disease (COPD)
Accreditation Statement
The CME Institute of Physicians Postgraduate Press, Inc., is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Credit Designation
The CME Institute of Physicians Postgraduate Press, Inc., designates this educational activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Date of Original Release/Review
This educational activity is eligible for AMA PRA Category 1 Credit through August 31, 2013. The latest review of this material was June 2010.
Financial Disclosure
The faculty for this CME activity and CME Institute staff were asked to complete a statement regarding all relevant personal financial relationships between themselves or their spouse/partner and any commercial interest. The CME Institute has resolved any conflicts of interest that were identified. No member of the CME Institute staff reported any relevant personal financial relationships. Faculty financial disclosure appears at the end of the article.
REFERENCES
- 1.Washington DC: COPD/Asthma Working Group with support from the Office of Performance Management; 1997. Clinical Practice Guideline for the Management of Persons With Chronic Obstructive Pulmonary Disease and Asthma. VHA Headquarters version 1. [Google Scholar]
- 2.Jones P. Issues concerning health-related quality of life in COPD. Chest. 1995;107(suppl 5):187s–193s. doi: 10.1378/chest.107.5_supplement.187s. [DOI] [PubMed] [Google Scholar]
- 3.Curtis JR, Deyo RA, Hudson LD. Pulmonary rehabilitation in chronic respiratory insufficiency, 7: health-related quality of life among patients with chronic obstructive pulmonary disease. Thorax. 1994;49(2):162–170. doi: 10.1136/thx.49.2.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsukino M, Nishimura K, Ikeda A, et al. Physiologic factors that determine the health-related quality of life in patients with COPD. Chest. 1996;110(4):896–903. doi: 10.1378/chest.110.4.896. [DOI] [PubMed] [Google Scholar]
- 5.Ferrer M, Alonso J, Morera J, et al. The Quality of Life of Chronic Obstructive Pulmonary Disease Study Group. Chronic obstructive pulmonary disease stage and health-related quality of life. Ann Intern Med. 1997;127(12):1072–1079. doi: 10.7326/0003-4819-127-12-199712150-00003. [DOI] [PubMed] [Google Scholar]
- 6.Viramontes JL, O'Brien B. Relationship between symptoms and health-related quality of life in chronic lung disease. J Gen Intern Med. 1994;9(1):46–48. doi: 10.1007/BF02599142. [DOI] [PubMed] [Google Scholar]
- 7.Brenes GA. Anxiety and chronic obstructive pulmonary disease: prevalence, impact, and treatment. Psychosom Med. 2003;65(6):963–970. doi: 10.1097/01.psy.0000097339.75789.81. [DOI] [PubMed] [Google Scholar]
- 8.Kim HF, Kunik ME, Molinari VA, et al. Functional impairment in COPD patients: the impact of anxiety and depression. Psychosomatics. 2000;41(6):465–471. doi: 10.1176/appi.psy.41.6.465. [DOI] [PubMed] [Google Scholar]
- 9.Cleland JA, Lee AJ, Hall S. Associations of depression and anxiety with gender, age, health-related quality of life and symptoms in primary care COPD patients. Fam Pract. 2007;24(3):217–223. doi: 10.1093/fampra/cmm009. [DOI] [PubMed] [Google Scholar]
- 10.Cully JA, Graham DP, Stanley MA, et al. Quality of life in patients with chronic obstructive pulmonary disease and comorbid anxiety or depression. Psychosomatics. 2006;47(4):312–319. doi: 10.1176/appi.psy.47.4.312. [DOI] [PubMed] [Google Scholar]
- 11.Adams SG, Smith PK, Allan PF, et al. Systematic review of the chronic care model in chronic obstructive pulmonary disease prevention and management. Arch Intern Med. 2007;167(6):551–561. doi: 10.1001/archinte.167.6.551. [DOI] [PubMed] [Google Scholar]
- 12.Engström CP, Persson LO, Larsson S, et al. Functional status and well being in chronic obstructive pulmonary disease with regard to clinical parameters and smoking: a descriptive and comparative study. Thorax. 1996;51(8):825–830. doi: 10.1136/thx.51.8.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Isoaho R, Keistinen T, Laippala P, et al. Chronic obstructive pulmonary disease and symptoms related to depression in elderly persons. Psychol Rep. 1995;76(1):287–297. doi: 10.2466/pr0.1995.76.1.287. [DOI] [PubMed] [Google Scholar]
- 14.McSweeny AJ, Grant I, Heaton RK, et al. Life quality of patients with chronic obstructive pulmonary disease. Arch Intern Med. 1982;142(3):473–478. [PubMed] [Google Scholar]
- 15.Prigatano GP, Wright EC, Levin D. Quality of life and its predictors in patients with mild hypoxemia and chronic obstructive pulmonary disease. Arch Intern Med. 1984;144(8):1613–1619. [PubMed] [Google Scholar]
- 16.Toshima M, Blumberg E, Ries A, et al. Does rehabilitation reduce depression in patients with chronic obstructive pulmonary disease? J Cardiopulm Rehabil. 1992;12(4):261–269. [Google Scholar]
- 17.Light RW, Merrill EJ, Despars JA, et al. Prevalence of depression and anxiety in patients with COPD: relationship to functional capacity. Chest. 1985;87(1):35–38. doi: 10.1378/chest.87.1.35. [DOI] [PubMed] [Google Scholar]
- 18.Yellowlees PM. The treatment of psychiatric disorders in patients with chronic airways obstruction. Med J Aust. 1987;147(7):349–352. [PubMed] [Google Scholar]
- 19.Jones PW, Baveystock CM, Littlejohns P. Relationships between general health measured with the sickness impact profile and respiratory symptoms, physiological measures, and mood in patients with chronic airflow limitation. Am Rev Respir Dis. 1989;140(6):1538–1543. doi: 10.1164/ajrccm/140.6.1538. [DOI] [PubMed] [Google Scholar]
- 20.van Ede L, Yzermans CJ, Brouwer HJ. Prevalence of depression in patients with chronic obstructive pulmonary disease: a systematic review. Thorax. 1999;54(8):688–692. doi: 10.1136/thx.54.8.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Manen JG, Bindels PJ, Dekker FW, et al. Risk of depression in patients with chronic obstructive pulmonary disease and its determinants. Thorax. 2002;57(5):412–416. doi: 10.1136/thorax.57.5.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karajgi B, Rifkin A, Doddi S, et al. The prevalence of anxiety disorders in patients with chronic obstructive pulmonary disease. Am J Psychiatry. 1990;147(2):200–201. doi: 10.1176/ajp.147.2.200. [DOI] [PubMed] [Google Scholar]
- 23.Pollack MH, Kradin R, Otto MW, et al. Prevalence of panic in patients referred for pulmonary function testing at a major medical center. Am J Psychiatry. 1996;153(1):110–113. doi: 10.1176/ajp.153.1.110. [DOI] [PubMed] [Google Scholar]
- 24.Goodwin RD, Pine DS. Respiratory disease and panic attacks among adults in the United States. Chest. 2002;122(2):645–650. doi: 10.1378/chest.122.2.645. [DOI] [PubMed] [Google Scholar]
- 25.Aghanwa HS, Erhabor GE. Specific psychiatric morbidity among patients with chronic obstructive pulmonary disease in a Nigerian general hospital. J Psychosom Res. 2001;50(4):179–183. doi: 10.1016/s0022-3999(00)00206-3. [DOI] [PubMed] [Google Scholar]
- 26.Aydin IO. Uluşahin A. Depression, anxiety comorbidity, and disability in tuberculosis and chronic obstructive pulmonary disease patients: applicability of GHQ-12. Gen Hosp Psychiatry. 2001;23(2):77–83. doi: 10.1016/s0163-8343(01)00116-5. [DOI] [PubMed] [Google Scholar]
- 27.Moore MC, Zebb BJ. The catastrophic misinterpretation of physiological distress. Behav Res Ther. 1999;37(11):1105–1118. doi: 10.1016/s0005-7967(98)00197-1. [DOI] [PubMed] [Google Scholar]
- 28.Kunik ME, Veazey C, Cully JA, et al. COPD education and cognitive behavioral therapy group treatment for clinically significant symptoms of depression and anxiety in COPD patients: a randomized controlled trial. Psychol Med. 2008;38(3):385–396. doi: 10.1017/S0033291707001687. [DOI] [PubMed] [Google Scholar]
- 29.Felker B, Katon W, Hedrick SC, et al. The association between depressive symptoms and health status in patients with chronic pulmonary disease. Gen Hosp Psychiatry. 2001;23(2):56–61. doi: 10.1016/s0163-8343(01)00127-x. [DOI] [PubMed] [Google Scholar]
- 30.SprioPro SMC. Yorba Linda, CA: SensorMedics; 2010. [Google Scholar]
- 31.Pauwels RA, Buist AS, Calverley PM, et al. GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–1276. doi: 10.1164/ajrccm.163.5.2101039. [DOI] [PubMed] [Google Scholar]
- 32.Hardie JA, Buist AS, Vollmer WM, et al. Risk of over-diagnosis of COPD in asymptomatic elderly never-smokers. Eur Respir J. 2002;20(5):1117–1122. doi: 10.1183/09031936.02.00023202. [DOI] [PubMed] [Google Scholar]
- 33.Enright P, Quanjer P. Don't diagnose mild COPD without confirming airway obstruction after an inhaled bronchodilator. COPD. 2007;4(2):89–90. doi: 10.1080/15412550701341509. [DOI] [PubMed] [Google Scholar]
- 34.Enright P. Does screening for COPD by primary care physicians have the potential to cause more harm than good? Chest. 2006;129(4):833–835. doi: 10.1378/chest.129.4.833. [DOI] [PubMed] [Google Scholar]
- 35.Celli BR, Halbert RJ, Isonaka S, et al. Population impact of different definitions of airway obstruction. Eur Respir J. 2003;22(2):268–273. doi: 10.1183/09031936.03.00075102. [DOI] [PubMed] [Google Scholar]
- 36.Scanlon PD, Connett JE, Waller LA, et al. Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease: The Lung Health Study. Am J Respir Crit Care Med. 2000;161(2 pt 1):381–390. doi: 10.1164/ajrccm.161.2.9901044. [DOI] [PubMed] [Google Scholar]
- 37.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 38.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 39.Blanchard EB, Jones-Alexander J, Buckley TC, et al. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 40.Saunders JB, Aasland OG, Babor TF, et al. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption, II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 41.Kazis LE, Ren XS, Lee A, et al. Health status in VA patients: results from the Veterans Health Study. Am J Med Qual. 1999;14(1):28–38. doi: 10.1177/106286069901400105. [DOI] [PubMed] [Google Scholar]
- 42.Mahler DA, Mackowiak JI. Evaluation of the short-form 36-item questionnaire to measure health-related quality of life in patients with COPD. Chest. 1995;107(6):1585–1589. doi: 10.1378/chest.107.6.1585. [DOI] [PubMed] [Google Scholar]
- 43.Alonso J, Prieto L, Ferrer M, et al. Quality of Life in COPD Study Group. Testing the measurement properties of the Spanish version of the SF-36 Health Survey among male patients with chronic obstructive pulmonary disease. J Clin Epidemiol. 1998;51(11):1087–1094. doi: 10.1016/s0895-4356(98)00100-0. [DOI] [PubMed] [Google Scholar]
- 44.Eakin EG, Resnikoff PM, Prewitt LM, et al. Validation of a new dyspnea measure: the UCSD Shortness of Breath Questionnaire. University of California, San Diego. Chest. 1998;113(3):619–624. doi: 10.1378/chest.113.3.619. [DOI] [PubMed] [Google Scholar]
- 45.Chicago, Illinois: SPSS Inc, an IBM Company; 2010. Statistical Package for the Social Sciences Windows Version 11.0.1. [Google Scholar]
- 46.Redmond, Washington: Microsoft Corporation; 1999. Microsoft Access 2000 (9.0.3821 SR-1) [Google Scholar]
- 47.R Development Core Team. The R Project for Statistical Computing. Available at: http://www.R-project.org.
- 48.Tu SP, McDonell MB, Spertus JA, et al. Ambulatory Care Quality Improvement Project (ACQUIP) Investigators. A new self-administered questionnaire to monitor health-related quality of life in patients with COPD. Chest. 1997;112(3):614–622. doi: 10.1378/chest.112.3.614. [DOI] [PubMed] [Google Scholar]
- 49.Jones PW, Quirk FH, Baveystock CM, et al. A self-complete measure of health status for chronic airflow limitation; the St. George's Respiratory Questionnaire. Am Rev Respir Dis. 1992;145(6):1321–1327. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 50.Ng TP, Niti M, Tan WC, et al. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007;167(1):60–67. doi: 10.1001/archinte.167.1.60. [DOI] [PubMed] [Google Scholar]
- 51.Sirey JA, Raue PJ, Alexopoulos GS. An intervention to improve depression care in older adults with COPD. Int J Geriatr Psychiatry. 2007;22(2):154–159. doi: 10.1002/gps.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Borson S, McDonald GJ, Gayle T, et al. Improvement in mood, physical symptoms, and function with nortriptyline for depression in patients with chronic obstructive pulmonary disease. Psychosomatics. 1992;33(2):190–201. doi: 10.1016/S0033-3182(92)71995-1. [DOI] [PubMed] [Google Scholar]
- 53.Smoller JW, Pollack MH, Systrom D, et al. Sertraline effects on dyspnea in patients with obstructive airways disease. Psychosomatics. 1998;39(1):24–29. doi: 10.1016/S0033-3182(98)71377-5. [DOI] [PubMed] [Google Scholar]
- 54.Paz-Díaz H, Montes de Oca M, López JM, et al. Pulmonary rehabilitation improves depression, anxiety, dyspnea and health status in patients with COPD. Am J Phys Med Rehabil. 2007;86(1):30–36. doi: 10.1097/phm.0b013e31802b8eca. [DOI] [PubMed] [Google Scholar]