Abstract
Associations between body mass index (BMI) and attempted (nonfatal) suicide have recently been reported. However, the few existing studies are relatively small in scale, the majority cross-sectional, and results contradictory. The authors have explored BMI–attempted suicide associations in a large cohort of 1,133,019 Swedish men born between 1950 and 1976, with BMI measured in early adulthood. During a mean follow-up of 23.9 years, a total of 18,277 (1.6%) men had at least 1 hospital admission for attempted suicide. After adjustment for confounding factors, there was a stepwise, linear decrease in attempted suicide with increasing BMI across the full BMI range (per standard deviation increase in BMI, hazard ratio = 0.93, 95% confidence interval: 0.91, 0.94). Analyses excluding men with depression at baseline were essentially identical to those based on the complete cohort. In men free from depression at baseline, controlling for subsequent depression slightly attenuated the raised risk of attempted suicide, particularly in lower weight men. This study suggests that lower weight men have an increased risk of attempted suicide and that associations may extend into the “normal” BMI range.
Keywords: body mass index; cohort studies; depression; social class; suicide, attempted
The prevalences of obesity and overweight are increasing worldwide (1). Increased body mass index (BMI) is a recognized risk factor for many chronic somatic conditions, such as cardiovascular disease, diabetes, and some cancers (2–8). There is also emerging evidence of BMI associations with mental health outcomes, such as depression, although findings are inconsistent, with higher depression rates reported in individuals with higher BMI (9, 10), lower BMI (11, 12), or both (13, 14). Suicide has also recently been linked with obesity. Results from studies of completed suicide, including an analysis of the current cohort (15), generally suggest that increasing BMI is associated with decreasing suicide risk (9, 15–20), although a recent study, based on relatively small numbers of deaths, reported an excess suicide risk among obese men (21). Results from studies of attempted (nonfatal) suicide have been markedly less consistent (12, 19, 22–28). Although attempted suicide is the strongest predictor of completed suicide (29), they do not necessarily share a common etiology; for example, completed suicide is more common in men, while nonfatal suicidal behaviors are more common in women and younger individuals (30). There is, therefore, a need for evidence from high-quality studies that specifically consider attempted suicide.
Attempted suicide risk has variously been reported as not associated with BMI (22, 27), greater in heavier individuals (25, 28), greater in lighter individuals (12, 19, 22), or greater in lighter and heavier individuals (23, 24, 26). However, the majority of studies (12, 23–26, 28) are cross-sectional, many focus on adolescents, and the role of psychiatric illness, particularly depression, has not been widely explored. Depression, in addition to being an important risk factor for suicidal behavior (31), is associated with both increases and decreases in appetite and may subsequently influence BMI. It is impossible, by using a cross-sectional design, to establish whether BMI directly influences attempted suicide risk or whether comorbidity, particularly with depression, impacts on both BMI and attempted suicide risk. Evidence from prospective studies is therefore needed to establish the temporal association between BMI and attempted suicide. Moreover, the majority of existing studies did not adjust for socioeconomic status (SES), an important candidate confounder given its strong associations with both BMI (32) and attempted suicide (33).
The present analyses explore associations between BMI measured in early adulthood (before the onset of most chronic somatic disease) and subsequent hospital admissions for attempted suicide in a cohort of over 1 million Swedish men. This cohort is considerably larger than any previous study in this context. In addition to offering greater statistical power, this has allowed 1) investigation of long-term associations of BMI with attempted suicide risk, 2) further exploration of the role of depression, 3) adjustment for SES at 2 points of the life course, and 4) insight into BMI–attempted suicide associations in the “normal” BMI range (BMI, 18.50–24.99 kg/m2).
MATERIALS AND METHODS
The record linkage used to generate this cohort has been reported previously (34, 35). In brief, all nonadopted men born in Sweden from 1950 to 1976 with both biologic parents identified in the Multi-Generation Register were identified and linked to the Population and Housing Census records (1960 and 1970) and Military Service Conscription, Cause of Death, and National Hospital Discharge registers, resulting in 1,379,531 successful matches. Study approval was obtained from the Regional Ethics Committee, Stockholm.
The military service conscription examination involves structured, standard medical assessment of physical and mental health. During the years covered by this study, the law required this examination; only men of foreign citizenship or with severe disability were excused. This data set covers examinations from September 15, 1969, to December 31, 1994. The average age at examination was 18 (range, 16–25) years. Height, weight, and blood pressure were measured by medical personnel using standard protocols. BMI was derived in the usual way (weight (kg)/height (m)2), and men were classified 1) according to World Health Organization (WHO) guidelines (36) as underweight (BMI, <18.5), normal weight (BMI, 18.5–24.9), overweight (BMI, 25.0–29.9), or obese (BMI, ≥30.0) and 2) in deciles of BMI (first decile: BMI, 14.0–18.6; second decile: BMI, >18.6–19.5; third: >19.5–20.1; fourth: >20.1–20.7; fifth: >20.7–21.2; sixth: >21.2–21.9; seventh: >21.9–22.5; eighth: >22.5–23.5; ninth: >23.5–25.0; and tenth: >25.0–54.7). Depression (International Classification of Diseases (ICD), Eighth and Ninth Revisions, codes 300, 308, 309, 311) at conscription was identified from physician interviews or from preconscription hospital admissions.
Childhood SES was based on the highest occupation of either parent from the Population and Housing Census records of 1960/1970. These same census records from 1990 were used to ascertain adult SES, based on own occupation for men who had an occupational code and otherwise on household SES. Highest educational achievement was obtained from Statistics Sweden's longitudinal integration database for health insurance and labor market studies of 1990–2004.
Hospital admissions data from 1969 to 2006 were based on the Swedish Hospital Discharge Register, which covered around a third of the Swedish population in 1970, rising to 71% in 1977 and 100% in 1987. The shortfall in the 1970s/1980s occurred in counties of varying population density and socioeconomic composition, and there were no systematic differences in BMI–attempted suicide associations in counties included and not included in the register during these early years. We identified attempted suicides from injuries coded as intentional (ICD, Eighth and Ninth Revisions, codes E950–E959; ICD, Tenth Revision, codes X60–X64) or undetermined (ICD, Eighth and Ninth Revisions, codes E980–E989; ICD, Tenth Revision, codes Y10–Y34). Analyses excluding undetermined injuries were very similar to those based on intentional and undetermined injuries combined. Our follow-up period covered 3 successive ICD revisions, and we identified 7 specific methods that were coded consistently across revisions (37, 38) (Table 1): poisoning by solid or liquid; other poisoning; hanging, strangulation, and suffocation; drowning; firearms and explosives; jumping or falling from a high place; and sharp object injuries. Analyses were restricted to attempted suicide admissions occurring after conscription. Hospital admissions for depression (ICD, Eighth and Ninth Revisions, codes 300, 308, 309, 311; ICD, Tenth Revision, codes F32–34, F40–43) occurring prior to any suicide attempts were also identified. As the purpose was to identify men with preexisting depression, those whose first depression admission coincided with a suicide attempt were not identified as previously depressed.
Table 1.
Number of Swedish Men Born Between 1950 and 1976 With 1 or More Hospital Admissions for Attempted Suicidea During Follow-up (N = 1,133,019)
| ICD-8/9 Codes | ICD-10 Codes | No.b | |
| All suicides | E950–E959, E980–E989 | X60–X64, Y10–Y34 | 18,277 |
| Poisoning by solid or liquid substances | E950, E980 | X60–X65, X68, X69, Y10–Y15, Y18, Y19 | 14,489 |
| Sharp object | E956, E986 | X78, Y28 | 1,700 |
| Other poisoning | E951, E952, E981, E982 | X66, X67, Y16, Y17 | 466 |
| Hanging, strangulation, and suffocation | E953, E983 | X70, Y20 | 438 |
| Jumping from a high place | E957, E987 | X80, Y30 | 389 |
| Firearms and explosives | E955, E985 | X72–X75, Y22–Y25 | 222 |
| Drowning and submersion | E954, E984 | X71, Y21 | 110 |
Abbreviations: ICD-8/9, International Classification of Diseases, Eighth Revision/Ninth Revision; ICD-10, International Classification of Diseases, Tenth Revision.
Includes undetermined injuries.
Men could have more than 1 type of suicide attempt.
We used Cox proportional hazards regression (39) to explore BMI–attempted suicide associations, having first checked that proportional hazards assumptions were not violated. As all hospital admissions were included, men could have more than 1 suicide attempt recorded. The main analyses were based on the first attempt by any means or by any specific methods. Thus, a man with 2 admissions for jumping and 1 for hanging would contribute to 1) all attempted suicides (first event), 2) jumping (first jump), and 3) hanging (only hanging). Follow-up began on the date of conscription and ended on the earliest of the following: date of attempted suicide, death, emigration, or December 31, 2006. Hazard ratios and 95% confidence intervals for attempted suicide were computed for underweight, overweight, and obese men relative to those of normal weight, according to WHO classifications. Hazard ratios and 95% confidence intervals were also calculated for attempted suicide by any means for deciles of BMI relative to the modal decile (decile 6). All analyses were adjusted for age at conscription, conscription center, and year of birth. Separate models controlled for childhood SES, adult SES, educational attainment, and blood pressure, which previously had been associated with both BMI (2) and suicide risk (40). Analyses are based on men with complete data for all variables.
We explored the role of depression in 2 ways. First, analyses were repeated excluding men with a diagnosis of depression at conscription and whose BMI might therefore be affected by related over- or undereating. Second, in men free from depression at conscription, we adjusted for depression during follow-up to explore the possibility that poor body image arising from high or low BMI leads to depression and therefore increases attempted suicide risk. We also carried out a series of sensitivity analyses. Specifically, we repeated the main analyses 1) excluding attempted suicides in the first 2 years of follow-up, 2) stratified by year of birth, 3) using age as the time scale rather than years since conscription, and 4) in the subgroup (3%) with data, adjusting for smoking and alcohol consumption.
RESULTS
The original cohort consisted of 1,379,531 men of whom 234,000 (17.0%) had missing conscription data and 12,512 (0.9%) had missing data on SES and education in 1990–2004. Analyses are based on 1,133,019 (82.1%) men with complete data on BMI and all covariates. Men with missing data tended to have lower SES. Men were followed up for an average of 23.9 years during which 18,277 (1.6%) had at least 1 admission for attempted suicide (Table 1) compared with 2,020 (0.8%) men excluded from analyses. The most common method was poisoning by solid or liquid (1.3% of the analytical sample), followed by sharp object injury (0.2%), other poisoning (0.04%), hanging, strangulation, or suffocation (0.04%), jumping or falling (0.03%), firearms or explosives injury (0.02%), and drowning or submersion (0.01%).
Characteristics of men according to baseline BMI are shown in Table 2. The majority (81.2%) were of normal weight at conscription. Similar numbers were under- and overweight (8.8% vs. 8.4%), and only 1.6% were obese. As expected, systolic blood pressure at conscription increased with increasing BMI. Men who were heavier at conscription were less likely to be in nonmanual occupations in 1990, less likely to be university educated, and less likely to have parents in nonmanual occupations. There was also a suggestion that those who were lighter at conscription had marginally lower educational attainment and childhood SES. Altogether, 34,319 (3.0%) men were identified as having depression at conscription, and a further 20,888 (1.9%) men without depression at conscription had at least 1 subsequent admission for depression during follow-up. Depression at conscription was more common in men who were underweight or obese; in contrast, there were an excess of postconscription hospital admissions for depression only among underweight men and little difference between men who were normal or overweight/obese. Attempted suicide admissions were higher among men at the extremes of the BMI distribution. Within the “normal” BMI range, men with increasing BMI tended to have 1) steadily increasing systolic blood pressure, 2) decreasing nonmanual SES (in childhood and adulthood), depression, and attempted suicide, and 3) a slight rise and then fall in university education (not shown).
Table 2.
Characteristics of Study Members According to Baseline Body Mass Index (N = 1,133,019), Swedish Men Born Between 1950 and 1976
| Body Mass Index, kg/m2 |
||||||||||||
| Underweight (<18.5) |
Normal Weight (18.5–24.9) |
Overweight (25.0–29.9) |
Obese (≥30.0) |
|||||||||
| No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | No. | % | Mean (SD) | |
| No. | 99,772 | 919,465 | 95,602 | 18,180 | ||||||||
| Age, years | 18.3 (0.6) | 18.3 (0.6) | 18.3 (0.6) | 18.3 (0.6) | ||||||||
| Systolic blood pressure, mm Hg | 125.7 (10.7) | 128.3 (10.8) | 131.8 (10.8) | 134.7 (11.1) | ||||||||
| Parents in nonmanual occupation | 42,646 | 42.7 | 401,883 | 43.7 | 34,306 | 35.9 | 5,235 | 28.8 | ||||
| Subject in nonmanual occupation | 27,915 | 28.0 | 239,072 | 26.0 | 16,729 | 17.5 | 2,211 | 12.2 | ||||
| University educated | 31,160 | 31.2 | 319,745 | 34.8 | 22,554 | 23.6 | 2,802 | 15.4 | ||||
| Depression at conscription | 4,927 | 4.9 | 25,752 | 2.8 | 2,866 | 3.0 | 774 | 4.3 | ||||
| Depression after conscriptiona | 2,443 | 2.6 | 16,565 | 1.9 | 1,563 | 1.7 | 317 | 1.8 | ||||
| Hospital admission for attempted suicide | 2,018 | 2.0 | 14,493 | 1.6 | 1,461 | 1.5 | 305 | 1.7 | ||||
Abbreviation: SD, standard deviation.
In 1,098,700 men with no depression identified at conscription.
Hazard ratios and 95% confidence intervals for attempted suicide by any means by WHO BMI classifications are presented in Table 3. In analyses adjusted for age, center, and year of birth, there were raised risks of attempted suicide in men who were underweight or obese when compared with normal-weight men. However, controlling for childhood SES, adult SES, and, particularly, educational attainment substantially reduced the raised risk in obese men and, to a lesser extent, in those who were underweight. Adjustment for blood pressure had no impact on the associations. In multiply-adjusted models, there was evidence of a raised risk in underweight men (hazard ratio (HR) = 1.12, 95% confidence interval (CI): 1.07, 1.18), and there was a correspondingly reduced risk in overweight (HR = 0.88, 95% CI: 0.83, 0.93) and obese (HR = 0.88, 95% CI: 0.78, 0.98) men.
Table 3.
Hazard Ratios and 95% Confidence Intervals for the Relation of Baseline Body Mass Index With Future Attempted Suicide by Any Means (N = 1,133,019), Swedish Men Born Between 1950 and 1976
| Body Mass Index | Suicide/No Suicide, nos. | Adjusted for Age, Center, and Birth Year |
Adjusted for Age, Center, Birth Year, and Childhood SES |
Adjusted for Age, Center, Birth Year, and Adult SES |
Adjusted for Age, Center, Birth Year, and Educational Attainment |
Multiple Adjustmenta |
|||||
| Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | ||
| Underweight | 2,018/97,754 | 1.22 | 1.16, 1.28 | 1.21 | 1.15, 1.26 | 1.17 | 1.11, 1.22 | 1.18 | 1.13, 1.24 | 1.12 | 1.07, 1.18 |
| Normal | 14,493/904,972 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Overweight | 1,461/94,141 | 1.02 | 0.96, 1.07 | 0.97 | 0.92, 1.02 | 0.98 | 0.93, 1.04 | 0.89 | 0.84, 0.94 | 0.88 | 0.83, 0.93 |
| Obese | 305/17,875 | 1.17 | 1.04, 1.31 | 1.07 | 0.96, 1.20 | 1.08 | 0.96, 1.21 | 0.94 | 0.84, 1.05 | 0.88 | 0.78, 0.98 |
| Pheterogeneityb | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||||||
Abbreviations: CI, confidence interval; SES, socioeconomic status.
Adjusted for age, conscription center, year of birth, childhood SES, adult SES, and educational attainment.
Pheterogeneity across categories of body mass index.
Figure 1A shows multiply-adjusted associations with BMI deciles. The first decile (BMI = 14.0–18.6) is composed almost entirely of men who were underweight according to WHO guidelines, while the tenth decile (BMI, >25.0) represents men who were overweight or obese. The remaining 8 deciles, therefore, span almost the entire WHO “normal” weight range. The magnitude of individual hazard ratios is relatively modest, and several 95% confidence intervals include 1. However, it is striking that the trend of decreasing hazard with increasing BMI identified in Table 3 is consistently stepwise across all 10 deciles and extends throughout the “normal” BMI range. In multiply-adjusted analyses that included BMI as a continuous variable, there was a linear trend of decreasing attempted suicide with increasing BMI (for a 1-standard deviation (SD) (2.8-kg/m2) increase in BMI, HR = 0.93, 95% CI: 0.91, 0.94).
Figure 1.
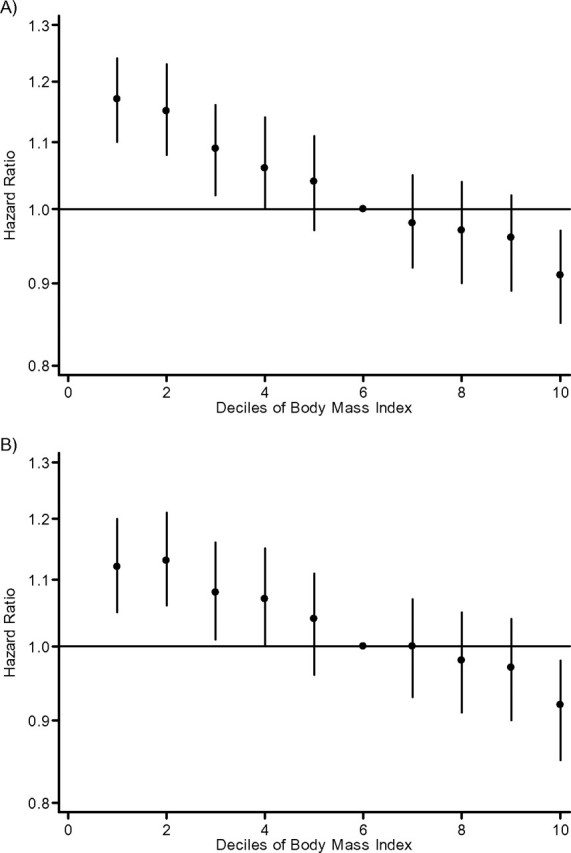
Hazard ratio and 95% confidence interval for the relation of baseline body mass index with future attempted suicide in 1,133,019 men with complete data (A) and in 1,098,700 men with complete data, free from depression at conscription, and additionally adjusted for depression during follow-up (B), for Swedish men born between 1950 and 1976. All hazard ratios are adjusted for age, conscription center, year of birth, childhood socioeconomic status, adult socioeconomic status, and educational attainment.
Age, center, and year of birth, as well as multiply-adjusted hazard ratios, are presented for method-specific attempted suicides in Table 4. Associations of BMI with the 2 most common attempted suicide methods (poisonings with solid/liquid or sharp object injuries) were broadly similar to those with attempted suicide by any means. Analyses of other method-specific attempted suicides were based on relatively small numbers of events, and confidence intervals are correspondingly wider. However, there was a suggestion that increasing BMI was associated with a steadily decreasing risk of other attempted poisoning, attempted hanging, and attempted jumping. Conversely, attempted firearms injuries were most common in men who were obese at conscription, although there were only 7 events in this group.
Table 4.
Hazard Ratios and 95% Confidence Intervals for Method-specific Attempted Suicidea by Body Mass Index, Swedish Men Born Between 1950 and 1976
| Suicide/No Suicide, nos. | Adjusted for Age, Center, and Birth Year |
Multiple Adjustmentb |
|||
| Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | ||
| Attempted poisoning (solid or liquid) | |||||
| Underweight | 1,601/98,171 | 1.22 | 1.15, 1.28 | 1.12 | 1.06, 1.18 |
| Normal | 1,485/907,980 | 1.00 | 1.00 | ||
| Overweight | 1,162/94,440 | 1.02 | 0.96, 1.09 | 0.88 | 0.83, 0.93 |
| Obese | 241/17,939 | 1.17 | 1.03, 1.33 | 0.87 | 0.76, 0.99 |
| Pheterogeneityc | <0.001 | <0.001 | |||
| Attempted sharp object injury | |||||
| Underweight | 179/99,593 | 1.16 | 1.00, 1.36 | 1.06 | 0.91, 1.24 |
| Normal | 1,344/918,121 | 1.00 | 1.00 | ||
| Overweight | 147/95,455 | 1.10 | 0.93, 1.30 | 0.96 | 0.81, 1.13 |
| Obese | 30/18,150 | 1.23 | 0.86, 1.77 | 0.93 | 0.65, 1.34 |
| Pheterogeneity | 0.15 | 0.78 | |||
| Other attempted poisoning | |||||
| Underweight | 61/99,711 | 1.43 | 1.09, 1.88 | 1.35 | 1.03, 1.78 |
| Normal | 363/919,102 | 1.00 | 1.00 | ||
| Overweight | 36/95,566 | 1.01 | 0.72, 1.43 | 0.88 | 0.62, 1.24 |
| Obese | 6/18,174 | 0.94 | 0.42, 2.10 | 0.72 | 0.32, 1.62 |
| Pheterogeneity | 0.10 | 0.11 | |||
| Attempted hanging | |||||
| Underweight | 46/99,726 | 1.16 | 0.85, 1.57 | 1.09 | 0.80, 1.49 |
| Normal | 358/919,107 | 1.00 | 1.00 | ||
| Overweight | 30/95,572 | 0.82 | 0.56, 1.19 | 0.72 | 0.49, 1.04 |
| Obese | 4/18,176 | 0.59 | 0.22, 1.57 | 0.46 | 0.17, 1.23 |
| Pheterogeneity | 0.32 | 0.08 | |||
| Attempted jumping | |||||
| Underweight | 43/99,729 | 1.20 | 0.87, 1.65 | 1.09 | 0.79, 1.50 |
| Normal | 320/919,145 | 1.00 | 1.00 | ||
| Overweight | 23/95,579 | 0.71 | 0.47, 1.09 | 0.65 | 0.42, 0.99 |
| Obese | 3/18,177 | 0.51 | 0.16, 1.59 | 0.41 | 0.13, 1.27 |
| Pheterogeneity | 0.12 | 0.08 | |||
| Attempted firearms injury | |||||
| Underweight | 23/99,749 | 1.13 | 0.73, 1.75 | 1.06 | 0.68, 1.63 |
| Normal | 174/919,291 | 1.00 | 1.00 | ||
| Overweight | 18/95,584 | 1.06 | 0.65, 1.72 | 0.89 | 0.55, 1.45 |
| Obese | 7/18,173 | 2.29 | 1.07, 4.88 | 1.66 | 0.76, 3.54 |
| Pheterogeneity | 0.28 | 0.41 | |||
| Attempted drowning | |||||
| Underweight | 14/99,758 | 1.38 | 0.78, 2.43 | 1.29 | 0.73, 2.28 |
| Normal | 85/919,380 | 1.00 | 1.00 | ||
| Overweight | 10/95,592 | 1.23 | 0.64, 2.38 | 1.17 | 0.61, 2.26 |
| Obese | 1/18,179 | 0.70 | 0.10, 5.03 | 0.62 | 0.09, 4.43 |
| Pheterogeneity | 0.66 | 0.75 | |||
Abbreviations: CI, confidence interval; SES, socioeconomic status.
Includes undetermined injuries.
Adjusted for age, conscription center, year of birth, childhood SES, adult SES, and educational attainment.
Pheterogeneity across categories of body mass index.
Of 34,319 men identified as depressed at conscription, 1,909 (5.6%) had a subsequent hospital admission for attempted suicide compared with 1.5% of men without depression. BMI–attempted suicide associations based on 1,098,700 men without depression at conscription were almost identical to those based on the full cohort (for a 1-SD increase in BMI, multiply-adjusted HR = 0.93, 95% CI: 0.91, 0.94). Additional adjustment for depression during follow-up led to a slight attenuation of the association, particularly among lower-weight men (Figure 1B), but a modest inverse linear trend remained across the full BMI range (for a 1-SD increase in BMI, multiply-adjusted HR = 0.94, 95% CI: 0.92, 0.95). Results from analyses restricted to attempted suicides more than 2 years after conscription, stratified by birth year, using age as the time scale, or adjusted for smoking and alcohol consumption were very similar to those presented in Table 3 (results not shown).
DISCUSSION
We have explored BMI–attempted suicide associations in a large-scale, prospective cohort study. In multiply-adjusted models, we observed a consistent, stepwise linear decrease in attempted suicide risk across the full BMI range. This association was evident in men without depression at baseline and was only slightly attenuated by adjustment for depression during follow-up.
Because of our large study population and lengthy follow-up, we were able, for the first time to our knowledge, to examine BMI associations with method-specific attempted suicides. Multiply-adjusted associations with most method-specific suicides were similar to those for all attempted suicides combined, with decreasing attempted suicide risk associated with greater BMI. It is, perhaps, of note that, in spite of relatively small numbers of events, the strongest associations were those with methods likely to require the greatest degree of physical effort and agility, namely, hanging and jumping. Alternatively, these may be methods that are most likely to require hospitalization and are therefore less prone to misclassification using our definition of attempted suicide. If this is the case, then our main results may, to some extent, be biased toward the null by other methods that are more variable in their likelihood of hospitalization. Finally, the most common attempted suicide method was self-poisoning; in this case, it may be that greater BMI is protective on the basis of body size and volume of distribution, leading to fewer attempted poisonings actually resulting in hospitalization.
Strengths and limitations
The majority of existing evidence on BMI-attempted suicide associations is based on cross-sectional data (12, 23–26, 28). In contrast, the current analyses utilize an almost complete birth cohort of over 1 million men, well defined for SES in childhood and adulthood, and followed up for an average of almost 24 years. This study is considerably larger than others in the field and, in addition to providing superior statistical power, this has allowed a more detailed exploration of associations within the “normal” BMI range. BMI was measured once, at the beginning of follow-up when men were aged between 16 and 25 (median age, 18) years and were likely to be free from chronic diseases, such as malignancies, that might influence both BMI and attempted suicide risk. BMI is known to demonstrate a high degree of tracking from adolescence and throughout adulthood (41, 42), and the long follow-up period therefore provides a unique insight into longer-term adult associations between BMI and attempted suicide risk. Attempted suicides were identified from records of hospital admissions and, as hospital treatment in Sweden is free, we have no reason to suppose there was any systematic bias resulting from this approach. We had data on depression at baseline and subsequently during follow-up, allowing further exploration of the role, particularly temporally, of depression in BMI–attempted suicide associations.
However, there are also a number of limitations. Analyses were based on 82.1% of men with complete data, which could potentially lead to bias if BMI–attempted suicide associations differ in those with missing data (including 0.4% of the cohort who died prior to data collection in 1990–2004); however, it is reassuring that analyses adjusted for age, center, and year of birth in men with complete data for all variables other than BMI and age at conscription were almost identical to those presented in Table 3. Our analyses do not include cases of self-harm not requiring hospital treatment, which may be important in identifying individuals at future risk of attempted or completed suicide. Additionally, our analyses are limited to attempted suicide admissions in men aged 16–57 years. Younger people have been identified as a priority in terms of suicide prevention, and our results provide an insight into this particularly vulnerable group but do not add information on BMI–attempted suicide associations in women or older men. Finally, depression during follow-up was based on hospital discharge data and is therefore restricted to episodes severe enough to warrant hospital admission. Previous studies of attempted suicide that consider the role of depression (12, 25, 27, 28) have been based on self-report and therefore include less severe morbidity. However, there are also issues around the validity of self-reported depression. In addition, studies were either cross-sectional (12, 25, 28) or only measured depression at one time point (27) and therefore provide no information on the temporal effects. Furthermore, evidence from previous studies (43, 44) indicates that rates of suicide in depressed individuals are greater in those who are hospitalized for depression, and the men identified in this way in our study were therefore likely to be those most at risk of future suicidal behavior.
Possible explanations for associations
Although BMI–attempted suicide associations were strong, they may not be causal, and BMI may be a marker for other factors involved in the etiology of attempted suicide. BMI is greater in lower SES individuals (32) and in those with lower intelligence (45) or educational attainment (46). Moreover, results from a large cohort (47) suggest that men who were obese at age 18 had lower educational attainment than their normal-weight peers, even after adjustment for intelligence and parental SES. Obesity and underweight in late adolescence have also been associated with increased disability pension for any cause and for psychiatric illness (48), which may lead to low SES, unemployment, and lack of social support from workmates. Increased suicide risks have been reported in individuals with lower SES (49), intelligence quotient (IQ) (19, 34), or education (19) who may have poorer problem-solving abilities, social support, and financial resources when affected by serious life events such as unemployment. In the current analyses, heavier men tended to have lower childhood and adult SES and educational attainment. Separate adjustment for these factors, particularly the potential mediators adult SES and education, markedly attenuated the raised risk of attempted suicide in heavier men (adjusted for age, center, and year of birth), including those at the upper end of the “normal” range, and, in multiply-adjusted models, there were clear linear trends of decreasing attempted suicide with increasing BMI, suggesting that attempted suicide associations with higher BMIs may be at least partially confounded/mediated by poor socioeconomic circumstances from across the life course.
Another possible mechanism is comorbidity, particularly at baseline, as existing disease may impact on both BMI and attempted suicide risk. Recent evidence (21) suggests that unexplained weight loss, possibly due to psychiatric illness, is more strongly associated with completed suicide risk than BMI per se. In the current analyses, men were examined as young adults, and the impact of chronic somatic diseases is likely to have been minimal. In contrast, 3.0% of men were identified as depressed at baseline and, in addition to influencing attempted suicide risk, depression can be associated with both increased and decreased appetite. However, results from analyses excluding these men were almost identical to those based on the whole cohort, suggesting that baseline comorbidity did not have a significant role, and that attempted suicide associations with BMI measured early in adulthood extend into later life.
One possible biologic mechanism that has been suggested involves insulin resistance. Individuals with high levels of insulin resistance have been shown to have a greater prevalence of depression (50), possibly due to increased serotonin concentrations. In addition, suicide risk has been shown to increase with increasing numbers of insulin sensitivity markers (51), including low BMI. The multiply-adjusted association of decreasing attempted suicide with increasing BMI presented here would certainly be consistent with this hypothesis. However, we had no information on insulin resistance and were unable to examine this mechanism directly.
Finally, the possibility of a psychological association should not be discounted. Studies of adolescents suggest that body dissatisfaction is an important predictor of suicidal behaviors (24, 28) and that associations with perceived weight are stronger than those with actual weight. Similarly, “body uneasiness” has been associated with increased suicide risk in young adults (52). Although women generally favor a lower body weight, perceptions in men may differ. A recent review (53) suggests that, while many adult men would prefer a slimmer body, a similar number would prefer a larger, more muscular shape. Although speculative, the consistently raised risk of attempted suicide in lower-weight men presented here is consistent with dissatisfaction with body sizes below the norm. Furthermore, the extension of this association into a BMI range usually regarded as “normal” in terms of general health suggests that the definition of “ideal” BMI may be even narrower. We had no information on body satisfaction and were unable to examine this hypothesis directly. However, adjustment for depression during follow-up slightly attenuated attempted suicide risk in lower weight men, and the longitudinal nature of the data makes reverse causality (e.g., low BMI caused by loss of appetite in depressed men) unlikely.
In conclusion, we observed stepwise inverse associations of decreasing attempted suicide with increasing BMI. Of note is the observation that this association was apparent in the “normal” BMI range. Evidence from the current analyses and wider literature suggests that BMI–attempted suicide associations are complex and that there is a need for more prospective evidence across the full BMI range to confirm long-term associations and to disentangle the interdependent effects of confounding/mediating variables and the role of depression.
Acknowledgments
Author affiliations: Medical Research Council Social and Public Health Sciences Unit, Glasgow, United Kingdom (G. David Batty, Elise Whitley); Centre for Cognitive Ageing and Cognitive Epidemiology, Department of Psychology, University of Edinburgh, Edinburgh, United Kingdom (G. David Batty); The George Institute for International Health, University of Sydney, Sydney, Australia (G. David Batty); Department of Epidemiology and Public Health, University College London, London, United Kingdom (Mika Kivimaki); and Department of Public Health Sciences, Karolinska Institute, Stockholm, Sweden (Per Tynelius, Finn Rasmussen).
G. D. B. is a Wellcome Trust Fellow (WBS U.1300.00.006.00012.01) the funds from which also support E. W. The Medical Research Council Social and Public Health Sciences Unit receives funding from the United Kingdom Medical Research Council and the Chief Scientist Office at the Scottish Government Health Directorates. The Centre for Cognitive Ageing and Cognitive Epidemiology is supported by the Biotechnology and Biological Sciences Research Council, the Engineering and Physical Sciences Research Council, the Economic and Social Research Council, the Medical Research Council, and the University of Edinburgh as part of the cross-council Lifelong Health and Wellbeing initiative. M. K. is supported by the Academy of Finland; the BUPA Foundation, United Kingdom; and the National Heart, Lung, and Blood Institute (R01HL036310-20A2) and the National Institute on Aging (R01AG034454), US National Institutes of Health. F. R. is supported by the Swedish Research Council, Labour Market Insurance, Ltd., and the Swedish Council for Working Life and Social Research.
Conflict of interest: none declared.
Glossary
Abbreviations
- BMI
body mass index
- CI
confidence interval
- HR
hazard ratio
- ICD
International Classification of Diseases
- SD
standard deviation
- SES
socioeconomic status
- WHO
World Health Organization
References
- 1.World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Geneva, Switzerland: World Health Organization; 2000. [PubMed] [Google Scholar]
- 2.Jung RT. Obesity as a disease. Br Med Bull. 1997;53(2):307–321. doi: 10.1093/oxfordjournals.bmb.a011615. [DOI] [PubMed] [Google Scholar]
- 3.Lawlor DA, Hart CL, Hole DJ, et al. Reverse causality and confounding and the associations of overweight and obesity with mortality. Obesity (Silver Spring). 2006;14(12):2294–2304. doi: 10.1038/oby.2006.269. [DOI] [PubMed] [Google Scholar]
- 4.Solomon CG, Manson JE. Obesity and mortality: a review of the epidemiologic data. Am J Clin Nutr. 1997;66(4 suppl):1044S–1050S. doi: 10.1093/ajcn/66.4.1044S. [DOI] [PubMed] [Google Scholar]
- 5.Batty GD, Shipley MJ, Jarrett RJ, et al. Obesity and overweight in relation to organ-specific cancer mortality in London (UK): findings from the original Whitehall Study. Int J Obes (Lond). 2005;29(10):1267–1274. doi: 10.1038/sj.ijo.0803020. [DOI] [PubMed] [Google Scholar]
- 6.Batty GD, Shipley MJ, Jarrett RJ, et al. Obesity and overweight in relation to disease-specific mortality in men with and without existing coronary heart disease in London: the original Whitehall Study. Heart. 2006;92(7):886–892. doi: 10.1136/hrt.2005.072637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Batty GD, Kivimaki M, Smith GD, et al. Obesity and overweight in relation to mortality in men with and without type 2 diabetes/impaired glucose tolerance: the original Whitehall Study. Diabetes Care. 2007;30(9):2388–2391. doi: 10.2337/dc07-0294. [DOI] [PubMed] [Google Scholar]
- 8.Silventoinen K, Magnusson PK, Tynelius P, et al. Association of body size and muscle strength with incidence of coronary heart disease and cerebrovascular diseases: a population-based cohort study of one million Swedish men. Int J Epidemiol. 2009;38(1):110–118. doi: 10.1093/ije/dyn231. [DOI] [PubMed] [Google Scholar]
- 9.Bjerkeset O, Romundstad P, Evans J, et al. Association of adult body mass index and height with anxiety, depression, and suicide in the general population: the HUNT Study. Am J Epidemiol. 2008;167(2):193–202. doi: 10.1093/aje/kwm280. [DOI] [PubMed] [Google Scholar]
- 10.Simon GE, Von Korff M, Saunders K, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63(7):824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lawlor DA, Hart CL, Hole DJ, et al. Body mass index in middle life and future risk of hospital admission for psychoses or depression: findings from the Renfrew/Paisley study. Psychol Med. 2007;37(8):1151–1161. doi: 10.1017/S0033291707000384. [DOI] [PubMed] [Google Scholar]
- 12.Carpenter KM, Hasin DS, Allison DB, et al. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90(2):251–257. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kress AM, Peterson MR, Hartzell MC. Association between obesity and depressive symptoms among U.S. military active duty service personnel, 2002. J Psychosom Res. 2006;60(3):263–271. doi: 10.1016/j.jpsychores.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 14.Rivenes AC, Harvey SB, Mykletun A. The relationship between abdominal fat, obesity, and common mental disorders: results from the HUNT Study. J Psychosom Res. 2009;66(4):269–275. doi: 10.1016/j.jpsychores.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 15.Magnusson PK, Rasmussen F, Lawlor DA, et al. Association of body mass index with suicide mortality: a prospective cohort study of more than one million men. Am J Epidemiol. 2006;163(1):1–8. doi: 10.1093/aje/kwj002. [DOI] [PubMed] [Google Scholar]
- 16.Gasse C, Derby LE, Vasilakis C, et al. Risk of suicide among users of calcium channel blockers: population based, nested case-control study. BMJ. 2000;320(7244):1251. doi: 10.1136/bmj.320.7244.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaplan MS, McFarland BH, Huguet N. The relationship of body weight to suicide risk among men and women: results from the US National Health Interview Survey Linked Mortality File. J Nerv Ment Dis. 2007;195(11):948–951. doi: 10.1097/NMD.0b013e3181594833. [DOI] [PubMed] [Google Scholar]
- 18.Mukamal KJ, Kawachi I, Miller M, et al. Body mass index and risk of suicide among men. Arch Intern Med. 2007;167(5):468–475. doi: 10.1001/archinte.167.5.468. [DOI] [PubMed] [Google Scholar]
- 19.Osler M, Nybo Andersen AM, et al. Impaired childhood development and suicidal behaviour in a cohort of Danish men born in 1953. J Epidemiol Community Health. 2008;62(1):23–28. doi: 10.1136/jech.2006.053330. [DOI] [PubMed] [Google Scholar]
- 20.Mukamal KJ, Rimm EB, Kawachi I, et al. Body mass index and risk of suicide among one million US adults. Epidemiology. 2010;21(1):82–86. doi: 10.1097/EDE.0b013e3181c1fa2d. [DOI] [PubMed] [Google Scholar]
- 21.Elovainio M, Shipley MJ, Ferrie JE, et al. Obesity, unexplained weight loss and suicide: the original Whitehall Study. J Affect Disord. 2009;116(3):218–221. doi: 10.1016/j.jad.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jiang GX, Rasmussen F, Wasserman D. Short stature and poor psychological performance: risk factors for attempted suicide among Swedish male conscripts. Acta Psychiatr Scand. 1999;100(6):433–440. doi: 10.1111/j.1600-0447.1999.tb10893.x. [DOI] [PubMed] [Google Scholar]
- 23.Falkner NH, Neumark-Sztainer D, Story M, et al. Social, educational, and psychological correlates of weight status in adolescents. Obes Res. 2001;9(1):32–42. doi: 10.1038/oby.2001.5. [DOI] [PubMed] [Google Scholar]
- 24.Eaton DK, Lowry R, Brener ND, et al. Associations of body mass index and perceived weight with suicide ideation and suicide attempts among US high school students. Arch Pediatr Adolesc Med. 2005;159(6):513–519. doi: 10.1001/archpedi.159.6.513. [DOI] [PubMed] [Google Scholar]
- 25.Brunner J, Bronisch T, Pfister H, et al. High cholesterol, triglycerides, and body-mass index in suicide attempters. Arch Suicide Res. 2006;10(1):1–9. doi: 10.1080/13811110500318083. [DOI] [PubMed] [Google Scholar]
- 26.Dong C, Li WD, Li D, et al. Extreme obesity is associated with attempted suicides: results from a family study. Int J Obes (Lond). 2006;30(2):388–390. doi: 10.1038/sj.ijo.0803119. [DOI] [PubMed] [Google Scholar]
- 27.Crow S, Eisenberg ME, Story M, et al. Are body dissatisfaction, eating disturbance, and body mass index predictors of suicidal behavior in adolescents? A longitudinal study. J Consult Clin Psychol. 2008;76(5):887–892. doi: 10.1037/a0012783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dave D, Rashad I. Overweight status, self-perception, and suicidal behaviors among adolescents. Soc Sci Med. 2009;68(9):1685–1691. doi: 10.1016/j.socscimed.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 29.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry. 2002;181:193–199. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- 30.Nock MK, Borges G, Bromet EJ, et al. Impaired childhood development and suicidal behaviour in a cohort of Danish men born in 1953 Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–154. [Google Scholar]
- 31.Miles CP. Conditions predisposing to suicide: a review. J Nerv Ment Dis. 1977;164(4):231–246. doi: 10.1097/00005053-197704000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Clarke P, O'Malley PM, Johnston LD, et al. Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986–2004. Int J Epidemiol. 2009;38(2):499–509. doi: 10.1093/ije/dyn214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Platt S, Hawton K, Kreitman N, et al. Recent clinical and epidemiological trends in parasuicide in Edinburgh and Oxford: a tale of two cities. Psychol Med. 1988;18(2):405–418. doi: 10.1017/s0033291700007959. [DOI] [PubMed] [Google Scholar]
- 34.Gunnell D, Magnusson PK, Rasmussen F. Low intelligence test scores in 18 year old men and risk of suicide: cohort study. BMJ. 2005;330(7484):167–170. doi: 10.1136/bmj.38310.473565.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Batty GD, Wennerstad KM, Smith GD, et al. IQ in early adulthood and later cancer risk: cohort study of one million Swedish men. Ann Oncol. 2007;18(1):21–28. doi: 10.1093/annonc/mdl473. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. World Health Organization Consultation on Obesity. Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity, Geneva, 3–5 June 1997. Geneva, Switzerland: World Health Organization; 1998. [PubMed] [Google Scholar]
- 37.Biddle L, Brock A, Brookes ST, et al. Suicide rates in young men in England and Wales in the 21st century: time trend study. BMJ. 2008;336(7643):539–542. doi: 10.1136/bmj.39475.603935.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brock A, Griffiths C. Trends in suicide by method in England and Wales, 1979 to 2001. Health Stat Q. 2003;20:7–17. [Google Scholar]
- 39.Collett D. Modelling Survival Data in Medical Research. London, United Kingdom: Chapman & Hall; 1994. [Google Scholar]
- 40.Terry PD, Abramson JL, Neaton JD, et al. Blood pressure and risk of death from external causes among men screened for the Multiple Risk Factor Intervention Trial. Am J Epidemiol. 2007;165(3):294–301. doi: 10.1093/aje/kwk014. [DOI] [PubMed] [Google Scholar]
- 41.Wilsgaard T, Jacobsen BK, Schirmer H, et al. Tracking of cardiovascular risk factors: the Tromsø Study, 1979–1995. Am J Epidemiol. 2001;154(5):418–426. doi: 10.1093/aje/154.5.418. [DOI] [PubMed] [Google Scholar]
- 42.Ulmer H, Kelleher C, Diem G, et al. Long-term tracking of cardiovascular risk factors among men and women in a large population-based health system: the Vorarlberg Health Monitoring & Promotion Programme. Eur Heart J. 2003;24(11):1004–1013. doi: 10.1016/s0195-668x(03)00170-2. [DOI] [PubMed] [Google Scholar]
- 43.Simon GE, VonKorff M. Suicide mortality among patients treated for depression in an insured population. Am J Epidemiol. 1998;147(2):155–160. doi: 10.1093/oxfordjournals.aje.a009428. [DOI] [PubMed] [Google Scholar]
- 44.Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a reexamination. Am J Psychiatry. 2000;157(12):1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- 45.Chandola T, Deary IJ, Blane D, et al. Childhood IQ in relation to obesity and weight gain in adult life: the National Child Development (1958) Study. Int J Obes (Lond). 2006;30(9):1422–1432. doi: 10.1038/sj.ijo.0803279. [DOI] [PubMed] [Google Scholar]
- 46.Batty GD, Deary IJ, Schoon I, et al. Mental ability across childhood in relation to risk factors for premature mortality in adult life: the 1970 British Cohort Study. J Epidemiol Community Health. 2007;61(11):997–1003. doi: 10.1136/jech.2006.054494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Karnehed N, Rasmussen F, Hemmingsson T, et al. Obesity and attained education: cohort study of more than 700,000 Swedish men. Obesity (Silver Spring). 2006;14(8):1421–1428. doi: 10.1038/oby.2006.161. [DOI] [PubMed] [Google Scholar]
- 48.Neovius M, Kark M, Rasmussen F. Association between obesity status in young adulthood and disability pension. Int J Obes (Lond). 2008;32(8):1319–1326. doi: 10.1038/ijo.2008.70. [DOI] [PubMed] [Google Scholar]
- 49.Steenland K, Halperin W, Hu S, et al. Deaths due to injuries among employed adults: the effects of socioeconomic class. Epidemiology. 2003;14(1):74–79. doi: 10.1097/00001648-200301000-00017. [DOI] [PubMed] [Google Scholar]
- 50.Lawlor DA, Smith GD, Ebrahim S. Association of insulin resistance with depression: cross sectional findings from the British women's Heart and Health Study. BMJ. 2003;327(7428):1383–1384. doi: 10.1136/bmj.327.7428.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Golomb BA, Tenkanen L, Alikoski T, et al. Insulin sensitivity markers: predictors of accidents and suicides in Helsinki Heart Study screenees. J Clin Epidemiol. 2002;55(8):767–773. doi: 10.1016/s0895-4356(02)00407-9. [DOI] [PubMed] [Google Scholar]
- 52.Pompili M, Girardi P, Innamorati M, et al. Body uneasiness and suicide risk in a non-clinical sample of university students. Arch Suicide Res. 2007;11(2):193–202. doi: 10.1080/13811110600896392. [DOI] [PubMed] [Google Scholar]
- 53.McCabe MP, Ricciardelli LA. Body image dissatisfaction among males across the lifespan: a review of past literature. J Psychosom Res. 2004;56(6):675–685. doi: 10.1016/S0022-3999(03)00129-6. [DOI] [PubMed] [Google Scholar]


