This report highlights the difficulty for both patient and physician of the diagnosis and management of this rare disease.
Case report
A 48-year-old woman presented to the Accident and Emergency department (A&E) with a two-day history of swelling and pain in the left buttock. She had a past history of hypothyroidism, depression and a hysterectomy for menorrhagia. Clinically there was a soft, diffuse, tender mass in the left buttock, with no evidence of abscess or cellulitis. Blood tests including inflammatory markers were normal. The surgical team suspected a diagnosis of a lipoma and discharged the patient with an outpatient ultrasound scan (USS).
The patient re-attended A&E three weeks later with increased buttock swelling and discomfort. The USS reported an irregular hypoechoic mass 6.9 × 4.5 × 3.2 cm in size situated 2 cm deep to the skin and extending towards the medial aspect of the left buttock, suggestive of an abscess. However, the clinical examination did not correlate with the radiological diagnosis and the patient was discharged following a brief admission for analgesia. An outpatient magnetic resonance imaging (MRI) scan was arranged.
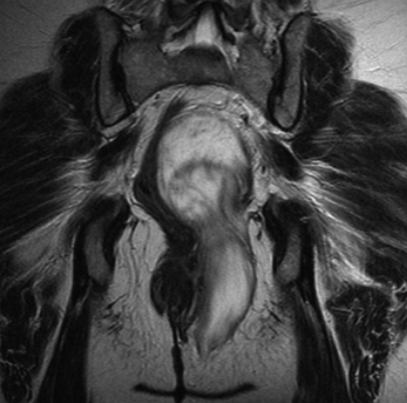
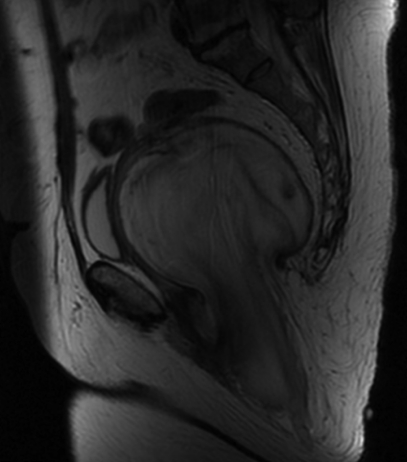
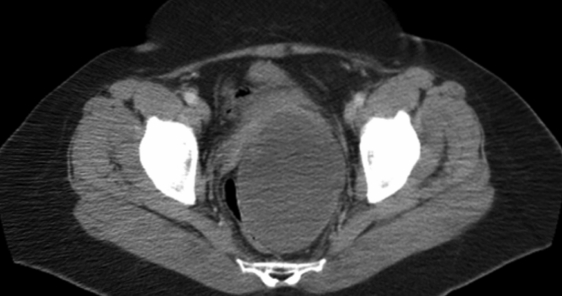
The MRI suggested a large pelvic liposarcoma and hence a staging CT scan was done (Figures 1, 2 and 3). This reported the soft tissue mass displacing the bladder and rectum as it extends from the level of sacroiliac joints and through the greater sciatic notch into the buttock. The CT concludes that a sarcoma is less likely a diagnosis than a cystic neoplasm. The patient was referred to a consultant surgeon at a regional Sarcoma Unit for treatment.
Figure 1.
Coronal section MRI scan showing tumour extending from pelvis into left buttock
Figure 2.
Sagittal section MRI scan of pelvis and perineum showing mass extending into buttock
Figure 3.
CT scan of pelvis showing tumour mass displacing bladder and rectum
An elective admission was arranged for full excision of the tumour via an incision into the buttock, and the patient was discharged at day 10. The main complications postoperatively were pain and a haematoma which discharged spontaneously. Histology confirmed an aggressive pelvic angiomyxoma. The patient is currently under follow-up with repeat MRI scans to assess for local recurrence and is awaiting further investigation of a suspicious lesion seen at her most recent scan, only 12 months post-primary resection.
Discussion
Buttock and perineal swellings are common presentations to both the general surgeon and gynaecologist, either on call or in clinic. Aggressive angiomyxoma is a very rare differential diagnosis for such cases.
Aggressive angiomyxoma was first described in 1983 by Steeper and Rosai1 and, according to literature, there have been fewer than 250 reported cases worldwide.2 It is a slow-growing benign mesenchymal neoplasm which is characterized by its tendency for local tissue infiltration and recurrence, even many years after resection. Metastases are very rare with only two reported cases in world literature where multiple metastases led to the death of both patients.3
It more commonly presents as a vulval or perineal tumour, although there are reports of its manifestation at other sites outside the pelvis.4 These tumours are almost always seen in women in their third and fourth decades of life but cases in men have also been reported, having presented as scrotal swellings and been mistaken for hernias or hydroceles.5 Presentation is generally as an asymptomatic soft tissue tumour often slow-growing over many years, making our case unusual in that the patient complained of a short history of a painful buttock lump.
Given the rarity of the condition and its relatively non-descript clinical presentation, it is almost impossible to suspect the diagnosis at first encounter.6 This explains the high rate of initial mis-diagnosis, and hence delayed treatment, of such tumours.
Surgery is the mainstay of treatment for aggressive angiomyxoma. Adequate surgical clearance is important in reducing recurrence rates but such wide excision of these usually large tumours carries a high morbidity. More recently, authors are describing a less radical approach to surgical excision with the aid of adjuvant therapy. Other treatment modalities have been used to treat both the primary and recurrent disease and these include chemotherapy, radiotherapy, vessel embolization and hormone suppression. Chemotherapy and radiotherapy are unlikely to be of certain benefit due to the low mitotic activity of the tumour cells. Preoperative vessel embolization is generally used to aid identifying the abnormal tissue at the time of resection and is also reported to shrink the tumour in some cases.7 The majority, but not all, of aggressive angiomyxomas are oestrogen and progesterone receptor positive which has lead to the use of gonadotropin-releasing hormone (GnRH) agonists in their treatment.8,9 GnRH agonists bind to receptors and initially increase the release of FSH and LH, and hence oestrogen and progesterone. However, after approximately 10 days of treatment, down-regulation of receptors is achieved by their internalization and a decrease in hormone levels results. Indeed, some reports have shown full radiological resolution of tumour with the use of GnRH agonists in cases of both primary and recurrent tumours. For this reason, it is suggested by some authors that GnRH agonists should form part of the treatment protocol in order to obviate the need for radical pelvic surgery in hormone receptor positive patients. More recently, one report of the successful use of an aromatase inhibitor in the treatment of angiomyxoma has been published, describing its use to shrink the tumour prior to resection.10 This treatment modality works by blocking the enzyme aromatase from synthesizing oestrogen.
Recurrence rates ranging between 9–72% have been reported from various case series, the spectrum being wide due to the low incidence of the disease and the variations in length of follow-up as well as the fact that many recurrences develop several years following the primary tumour. This emphasizes the need for long-term surveillance and follow-up of these patients.
In summary, although a rare and benign tumour, aggressive angiomyxoma may cause significant symptoms if large and surgical resection carries a high morbidity. Adjuvant medical therapies should be discussed and follow-up must be long-term with repeat MRI or CT scanning.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Written informed consent to publication has been obtained from the patient or next of kin
Guarantor
MAR
Contributorship
HA is the main author, AP performed literature search for discussion, MAR is a consultant surgeon involved in this patient's management and approved the report content
Acknowledgements
None
Reviewer
Sudha Sundar
References
- 1.Steeper TA, Rosai J Aggressive angiomyxoma of the female pelvis and perineum. Report of nine cases of a distinctive type of gynecologic soft-tissue neoplasm. Am J Surg Pathol 1983;7:463–75 [DOI] [PubMed] [Google Scholar]
- 2.Haldar K, Martinek IE, Kehoe S Aggressive angiomyxoma: A case series and literature review. Eur J Surg Oncol 2010;36:335–9 [DOI] [PubMed] [Google Scholar]
- 3.Blandamura S, Cruz J, Faure Vergara L, et al. Aggressive angiomyxoma: a second case of metastasis with patient's death. Hum Pathol 2003;34:1072–4 [DOI] [PubMed] [Google Scholar]
- 4.Chuang FP, Wu ST, Lee SS, et al. Aggressive angiomyxoma of the scrotum. Arch Androl 2002;48:101–6 [DOI] [PubMed] [Google Scholar]
- 5.Hong RD, Outwater E, Gomella LG Aggressive angiomyxoma of the perineum in a man. J Urol 1997;157:959–60 [PubMed] [Google Scholar]
- 6.Jingping Z, Chunfu Z Clinical experiences on aggressive angiomyxoma in China (report of 93 cases). Int J Gynecol Cancer 2010;20:303–7 [DOI] [PubMed] [Google Scholar]
- 7.Corson SL, Rosato EL, Rosato FE, et al. Aggressive angiomyxoma of the pelvis: case report and review. Int J Fertil Womens Med 2002;47:248–52 [PubMed] [Google Scholar]
- 8.Fine BA, Munoz AK, Litz CE, et al. Primary medical management of recurrent aggressive angiomyxoma of the vulva with a gonadotropin-releasing hormone agonist. Gynecologic Oncology 2001;81:120–2 [DOI] [PubMed] [Google Scholar]
- 9.Poirier M, Fraser R, Meterissian S Case 1. Aggressive angiomyxoma of the pelvis: response to luteinizing hormone-releasing hormone agonist. J Clin Oncol 2003;21:3535–6 [DOI] [PubMed] [Google Scholar]
- 10.Giles DL, Liu PT, Lidner TK, et al. Treatment of aggressive angiomyxoma with aromatase inhibitor prior to surgical resection. Int J Gynecol Cancer 2008;18:375–9 [DOI] [PubMed] [Google Scholar]