Abstract
Objectives
The aim of this study was to examine the accuracy of doctors at diagnosing co-morbid psychiatric disorders in patients with chronic fatigue syndrome (CFS).
Design
Case series comparing clinical diagnoses with a standardized structured psychiatric interview.
Setting
Secondary care specialist chronic fatigue syndrome clinic.
Participants
One hundred and thirty-five participants of a randomized controlled trial of non-pharmacological treatments at one centre in the PACE trial.
Main outcome measures
Current psychiatric diagnoses made by CFS specialist doctors, compared with current psychiatric diagnoses made independently using a structured psychiatric interview.
Results
Clinicians identified 59 (44%, 95% CI 39–56%) of patients as suffering from a co-morbid psychiatric disorder compared to 76 (56%, CI 53–69%) by structured interview. Depressive and anxiety disorders were most common. Clinicians were twice as likely to miss diagnoses (30 patients, 22%) than misdiagnose them (13, 10%). Psychiatrists were less likely to miss diagnoses than other clinicians, but were as likely to misdiagnose them.
Conclusions
Doctors assessing patients in a chronic fatigue syndrome clinic miss psychiatric diagnoses more often than misdiagnosing them. Missed diagnoses are common. CFS clinic doctors should be trained to diagnose psychiatric disorders.
Background
Despite the prevalence of chronic fatigue syndrome (CFS), also known as myalgic encephalomyelitis (ME), much controversy surrounds aetiology, treatment options, and expected long-term outcomes.1 An overlap exists between many of the symptoms of CFS/ME and psychiatric disorders, in particular anxiety and depressive disorders.2 This can make deciphering the difference between CFS/ME alone, CFS/ME with psychiatric co-morbidity and a primary psychiatric disorder difficult. Misdiagnosis occurs commonly.2 Correct diagnosis is important, to ensure that patients receive the optimum treatment. Research suggests that misdiagnosis may result from the review of patients with CFS/ME by a wide variety of medical subspecialties, where diagnoses are often made by clinicians not trained in psychiatry or psychology.2,3
The aim of this study was to quantify the number and nature of current co-morbid psychiatric diagnoses in CFS/ME patients using a standardized psychiatric interview. We compared the proportion of diagnoses missed (where the clinician has not recorded a diagnosis which is present) or misdiagnosed (where the clinician has made a diagnosis not present) in a clinic staffed by specialist CFS/ME clinicians. Then finally we compared diagnostic errors made by psychiatrists with non-psychiatrists. The study concentrated specifically on those psychiatric diagnoses which do not exclude a diagnosis of CFS/ME: namely depressive disorders, generalized anxiety disorder, post-traumatic stress disorder, obsessive compulsive disorder, social phobia and specific phobias. Certain diagnoses (schizophrenia, bipolar disorder, substance misuse, eating disorder or proven organic brain disease) were excluded due to their likely ability to be the explanation for a complaint of chronic disabling fatigue.4 This study may support or refute the use of standardized tools for assessing psychiatric conditions at clinical evaluation and may give support to the argument that patient with CFS/ME should be seen by doctors trained to provide psychiatric assessments prior to final diagnosis.3
Methods
Participants
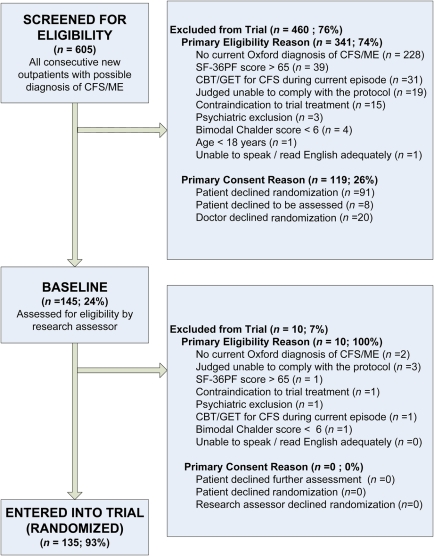
This was an ancillary study of the PACE trial; a multicentre randomized controlled trial of non-pharmacological interventions for patients diagnosed with CFS/ME.5 Participants (n = 135) were all those recruited into the trial from one of the PACE trial participating centres. All 135 patients had a diagnoses of CFS, using the Oxford criteria for CFS,6 made by a doctor in a specialist clinic, and had been referred to, consented to, and been randomized into the PACE trial at St Bartholomew's Hospital, London. All participants were aged 18 years and over. The screening breakdown is summarized in Figure 1.
Figure 1.
Derivation of study sample
Measures
We first examined the clinical diagnoses of trial participants made by the assessing doctor who had confirmed a diagnosis of CFS and then referred the patient to the PACE trial.5 We did this by reading the initial assessment letter and the first follow-up clinic letter following randomization. All details which could identify either the patient or the assessing doctor was removed from these letters. The clinic letters were examined to obtain: patient demographics (age and gender) and the doctor's final clinical assessment. Two investigators, both psychiatric trainees, examined the letters separately and recorded whether they believed a clinical diagnosis of a psychiatric disorder was made. The diagnoses recorded in the clinic letters included depressive illness, dysthymia, anxiety disorder (which included panic disorder with or without agoraphobia and generalized anxiety disorder), obsessive compulsive disorder, post-traumatic disorder, social phobia and specific phobia. Investigators disagreed on whether a particular diagnosis was made by the assessing doctor in six sets of notes. The consultant liaison psychiatrist (PDW) was consulted for a final decision.
After the initial assessment, but prior to randomization, all patients had a semi-structured psychiatric diagnostic interview, the ‘Structured Clinical Interview for DSM-IV Disorders’ (SCID; patient edition with psychotic screen), administered to them by a research nurse (Registered Mental Nurse) appropriately trained to administer the SCID and supervised by a consultant psychiatrist.7 For the purposes of this study, we regarded this as the most valid test for the presence or absence of a psychiatric disorder as the SCID has been shown to produce greater reliability and validity than clinicians, most of whom in this study were not psychiatrists or, if psychiatrists, were not fully trained. The SCID results for each participant were recorded. The research nurse also confirmed that all participants met the Oxford criteria for CFS, which included laboratory tests to exclude those with alternative diagnoses, as recommended by the National Institute for Health and Clinical Excellence.6,8 The Oxford criteria allow for certain mental disorders to be co-morbidly and concurrently present (e.g. minor depressive episode). We also used the SCID before recruitment into this study to ensure that no case had an exclusionary mental disorder (e.g. schizophrenia).
The investigators also had access to records of any medication participants were taking at baseline, 12 weeks and 24 weeks after randomization. Any antidepressant medication being taken at these points was noted, as was the indication for its use. We included the use of St John's wort. These data were collected in order to analyse whether there was a change in prescribing after the SCID was administered. Notably, if the research nurse diagnosed a psychiatric disorder, using the SCID, the treating doctor was informed shortly after the diagnosis was made. The interval between clinical assessment and the SCID being administered was also recorded.
The doctors who had done the initial assessment all had experience in treating CFS but came from a variety of backgrounds. The non-psychiatrists were either physicians or general practitioners with a special interest; the psychiatrists were at both consultant and trainee level. The doctors' specialty and grade were coded by the research nurse and the two investigators were blinded to this.
Analysis
Descriptive statistics used were mean and standard deviation or median and interquartile range, depending on the distribution of the values. The frequency and proportions of false positive and false negative diagnoses are presented, with 95% confidence intervals, for all psychiatric diagnoses and then subgroups by depressive and anxiety disorders, providing sensitivity and specificity measures.9 Comparisons were made between psychiatrists versus non-psychiatrists and consultants versus non-consultants. Comparative statistics included the kappa statistic (with 95% confidence intervals) for total agreement between clinicians and the SCID diagnoses. Direct comparisons of proportions were made using the Chi square test with McNemar tests for the probability of a statistical significant difference between the proportions of patients with missed diagnoses and those misdiagnosed. We also calculated sensitivity and specificity values.10
Results
The participants' median age was 35 years (interquartile range 29–43). One hundred and two (76%) participants were women. Seventy-six (56%) participants had a co-morbid psychiatric diagnosis, confirmed by the SCID. Of these, 42 (31%) had a major or minor depressive episode, 15 (11%) dysthymia, 47 (35%) an anxiety disorder, three (2%) obsessive compulsive disorder, eight (6%) post-traumatic stress disorder, 11 (8%) social phobia and 20 (15%) a specific phobia. Several patients had more than one co-morbid psychiatric diagnosis. At baseline, 40 (30%) participants were taking an antidepressant and three (2%) were taking St John's wort. One patient was taking both an antidepressant and St John's wort.
Of the 14 assessing doctors, 10 were psychiatrists (one consultant and nine trainees). One was a consultant physician and three were general practitioners with a special interest in CFS. Fifty-three (39%) of participants were seen by a psychiatrist and 82 (61%) were seen by a non-psychiatrist. Sixty-nine (51%) patients were seen by a consultant and 66 (49%) were seen by a non-consultant.
Seventy-six (56%) participants had at least one co-morbid psychiatric diagnosis, as measured by the SCID, but only 59 (44%) had a psychiatric diagnosis made by clinicians at clinical assessment. Forty-three (32%) of the clinicians' psychiatric diagnoses were categorically wrong in comparison to the SCID. Thirty (22%) clinicians' diagnoses were falsely negative (i.e. the clinician made no diagnosis, but the SCID did) and 13 (10%) clinicians' diagnoses were falsely positive (i.e. the clinician made a diagnosis, but the SCID did not) (Table 1). Therefore, clinicians missed diagnoses more than twice as frequently as making misdiagnoses; a statistically significant difference (p < 0.01), particularly for anxiety disorders (p < 0.04). This is reflected in the sensitivity being less than the specificity for all comparisons.
Table 1.
Misdiagnoses and missed diagnoses (n = 135)
| Any psychiatric co-morbidity | Depression | Depression and dysthymia combined | All anxiety disorders combined | |
|---|---|---|---|---|
| False positive n (%) (CI) | 13 (10%) (6–16%) |
15 (11%) (7–17%) |
11 (8%) (5–14%) |
14 (10%) (6–17%) |
| False negative n (%) (CI) | 30 (22%) (16–30%) |
19 (14%) (9–21%) |
20 (15%) (10–22%) |
28 (21%) (15–28%) |
| P value | 0.01 | 0.61 | 0.15 | 0.04 |
| Total disagreement (CI) | 43 (32%) (25–40%) |
34 (25%) (19–33%) |
31 (23%) (17–31%) |
42 (31%) (CI 24–39%) |
| Kappa value (CI) | 0.37 (0.33–0.41) |
0.40 (0.37–0.43) |
0.47 (0.44–0.50) |
0.36 (0.32–0.40) |
| Sensitivity (CI) | 46/76 = 61% (49–71%) | 23/42 = 55% (40–69%) | 27/47 = 57% (43–70%) | 32/60 = 53% (41–65%) |
| Specificity (CI) | 46/59 = 78% (66–87%) | 78/93 = 84% (75–90%) | 77/88 = 88% (79–93%) | 61/75 = 81% (71–88%) |
P values are the probabilities that false positive and negative proportions are different. All kappa values, which measure level of agreement, were significant at p < 0.01
CI = 95% confidence interval
When comparing the subgroups: depressive episodes on their own, combined depressive episode and dysthymia, and anxiety disorders, the proportions for each class of diagnosis were very similar to the overall results. In other words, clinicians were no better at diagnosing specific psychiatric disorders compared to the total (Table 1).
When analysing the effectiveness of different specialties and grades of doctors, psychiatrists made errors in 26% of participants (15% missed, 11% misdiagnosis) and non-psychiatrists in 34% (27% missed and 7% misdiagnosis) (Table 2). Psychiatrists made errors of misdiagnosis as much as missing diagnoses, whereas non-psychiatrists were statistically more likely to miss diagnoses than misdiagnose patients (p < 0.01).
Table 2.
Comparison between specialties and level of training
| Psychiatrists | Non-psychiatrists | Consultants | Non- consultants | |
|---|---|---|---|---|
| False positive n (%) (CI) | 6 (11% ) (5–22%) |
7 (9%) (4–17%) |
9 (13%) (7–28%) |
4 (6%) (2–15%) |
| False negative n (%) (CI) | 8 (15%) (8–27%) |
22 (27%) (18–37%) |
14 (20%) (12–31%) |
16 (24%) (16–36%) |
| P value | 0.79 | 0.01 | 0.41 | 0.01 |
| Total disagreement (CI) | 14 (26%) (16–40%) |
29 (36%) (26–46%) |
23 (33%) (23–45%) |
20 (30%) (21–42%) |
| Kappa value (CI) | 0.47 (0.41–0.53) |
0.31 (0.26–0.36) |
0.34 (0.28–0.40) |
0.41 (0.35–0.47) |
| Sensitivity (CI) | 22/28 = 79% (60–90%) | 24/31 = 77% (60–89%) | 24/33 = 73% (56–85%) | 22/26 = 85% (66–94%) |
| Specificity (CI) | 17/25 = 68% (48–83%) | 29/51 = 57% (43–69%) | 22/36 = 61% (45–75%) | 24/40 = 60% (45–74%) |
P values are the probabilities that false positive and negative proportions are different. All kappa values, which measure level of agreement, were significant at p < 0.01
CI = 95% confidence interval
Non-consultant grade doctors of all disciplines made errors in 33% of participants in comparison to 30% by consultants (Table 2) (not statistically significant). There was no statistically significant difference in missed diagnoses and misdiagnoses by consultants, but non-consultants were significantly more likely to miss diagnoses than misdiagnose patients (p = 0.01) (Table 2). There were no individual outliers within doctors, so these findings were generalized across all doctors.
The number of patients prescribed antidepressants was 41 (30%, 95% CI 23–38%) at baseline, increasing to 49 (36%, 29–45%) at 12 weeks and 51 (38%, 30–46%) at 24 weeks follow-up, but these differences were not statistically significant. Knowledge of a SCID diagnosis of a depressive illness made no significant difference in prescription rates for antidepressants.
The median (interquartile range) interval between clinical assessment and SCID interview was 3 (1–7) weeks. Neither this interval, age, nor gender made a statistically significant difference to the results (data not shown).
Discussion
The rates of psychiatric co-morbidity in patients with CFS were high with over a half of patients having at least one psychiatric diagnosis confirmed by the SCID. Overall the doctors missed a psychiatric diagnosis in 22% of participants and diagnosed a psychiatric illness which was not present in 10%. The only significant difference between doctors was that psychiatrists missed fewer psychiatric diagnoses than non-psychiatrists, but they were equally likely to make a misdiagnosis. Informing doctors of SCID diagnoses made no significant difference to the prescriptions of antidepressants, which generally occurred more commonly with time. Prescribing rates of antidepressants were high (30%) although not always for a recorded indication of a depressive illness. Many patients were prescribed them for anxiety disorders or were given low dose tricyclics as hypnotics for insomnia.
The strengths of this study include: the comparison of different specialty doctors, different levels of training, the initial confirmation of the diagnosis of chronic fatigue syndrome using the standardized criteria, and the independent and blind assessment of clinical diagnoses. The limitations of the study include the selection bias of participation in a clinical trial and the involvement of only one specialist service. The psychiatric SCID interview was given by a research nurse, rather than a psychiatrist.
How representative are these findings of other CFS services and previous research? The demographics of our sample are similar to those found in other CFS services.2,11,13 The study sample (Figure 1) shows that the commonest reason for exclusion from this study was the absence of a diagnosis of CFS, with only a minority declining consent for the trial, which suggests the data are comparable to our overall clinic population of those with confirmed CFS. We cannot directly compare our data with those of Deale and Wessely,2 since they compared standardized psychiatric diagnoses made in clinic to diagnoses made before attending. Their reported prevalence of current psychiatric co-morbidity of 34% was lower than our finding of 56% but no details were reported of which psychiatric diagnoses were assessed, so our ability to compare is limited. The prevalence of co-morbid psychiatric disorders in patients attending other CFS clinics, measured by standardized interviews, varies from 21% to 77%, with most studies finding about 45% prevalence.12 We cannot suggest that our data are compatible with primary care, since the prevalence of psychiatric co-morbidity is likely to be different,12,13 although an American population study recently found a very similar prevalence of current co-morbid psychiatric disorders (57%) using the same standardized interview.14
What are the clinical implications of this study? Diagnosing co-morbid psychiatric disorders, particularly depressive disorders, is important because they negatively affect prognosis if not treated.1,15 Clinicians more frequently missed diagnoses but were better at avoiding misdiagnoses in this study. Psychiatrists are understandably better at not missing diagnoses. Doctors often mentioned symptoms consistent with a depressive or anxiety disorder, but did not make a formal diagnosis. This may reflect either reluctance to ‘label’ patients with a stigmatized diagnosis, the assumption that these symptoms were due to or a part of CFS, or different training backgrounds. Even when doctors were informed of a missed diagnosis of depressive illness, this did not influence prescriptions of antidepressants. This may be due to patients already receiving appropriate treatment (e.g. an antidepressant or cognitive behaviour therapy), patients declining medication, or doctors preferring to trust their own clinical judgement.
Specialist doctors in CFS clinics, particularly non-psychiatrists, need training to be able to diagnose co-morbid psychiatric disorders in order to offer treatment either themselves or referral onwards. Such training should include how to take a psychiatric history and how to do a mental state examination. Since the only significantly increased cause of death in this clinic population of patients is through suicide,16 which is most likely to occur when associated with depressive illness and those of less certain diagnosis,16 this training should include risk assessment. Such a programme might improve the care provided to patients attending such clinics.
DECLARATIONS
Competing interests
PDW has done independent consultancy work for the Department for Work and Pensions and a re-insurance company. MS has done independent consultancy work for insurance companies and lawyers. No other authors had competing interests
Funding
This project was supported by East London Foundation Trust, Queen Mary University of London, and the Medical Research Council
Ethical approval
Ethical approval for this study was provided by the West Midlands Research Ethics Committee as a substantial amendment to ethical approval given for the PACE trial (02/7/089)
Guarantor
PDW
Contributorship
BK and PDW conceived the idea and BK wrote the protocol. TL and PK collected the data. TL, PK and PDW analysed the data. All authors wrote and approved the final version of the paper
Acknowledgements
The authors thank Julie Richards, Research Nurse, for her contribution
Reviewer
Hugh Rickards
References
- 1.Prins JB, Van Der Meer JWM, Bleijenberg G Chronic fatigue syndrome. Lancet 2006;367:346–55 [DOI] [PubMed] [Google Scholar]
- 2.Deale A, Wessely S Diagnosis of psychiatric disorder in clinical evaluation of chronic fatigue syndrome. J R Soc Med 2000;93:310–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prins JB, Bleijenberg G, Bazelmans E, et al. Cognitive behaviour therapy for chronic fatigue syndrome: a multicentre randomised controlled trial. Lancet 2001;357:841–7 [DOI] [PubMed] [Google Scholar]
- 4.Reeves WC, Lloyd A, Vernon SD, et al. Identification of ambiguities in the 1994 chronic fatigue syndrome research case definition and recommendations for resolution. BMC Health Serv Res 2003;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.White P, Sharpe M, Chalder T, DeCesare J, Walwyn R; PACE trial group Protocol for the PACE trial: A randomised controlled trial of adaptive pacing, cognitive behaviour therapy, and graded exercise as supplements to standardised specialist medical care alone for patients with the chronic fatigue syndrome/myalgic encephalomyelitis or encephalopathy. BMC Neurology 2007;7:6 See http://www.biomedcentral.com/1471-2377/7/6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharpe MC, Archard LC, Banatvala JE, et al. A report – chronic fatigue syndrome. J R Soc Med 1991;84:118–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.First MB, Spitzer RL, Gibbon M, Williams JBW Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen (SCID-I/P W/ PSY SCREEN). New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. See http://cpmcnet.columbia.edu/dept/scid/ [Google Scholar]
- 8.National Institute for Health and Clinical Excellence Clinical guideline CG53. Chronic fatigue syndrome/myalgic encephalomyelitis (or encephalopathy): diagnosis and management. London: NICE; 2007 [Google Scholar]
- 9.Altman D, Bland J Statistical Notes: Diagnostic tests 1: sensitivity and specificity. BMJ 1994;308:1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Altman D, Bland J Statistical Notes: Diagnostic tests 2: predictive values. BMJ 1994;309:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White PD, Pinching AJ, Rakib A, Castle M, Hedge B, Priebe S A comparison of patients with chronic fatigue syndrome attending separate fatigue clinics based in immunology and psychiatry. J R Soc Med 2002;95:440–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wessely S, Hotopf M, Sharpe M Chronic fatigue and its syndromes. Oxford: Oxford University Press; 1998 [Google Scholar]
- 13.Euba R, Chalder T, Deale A, Wessely S A comparison of the characteristics of chronic fatigue syndrome in primary and tertiary care. Br J Psychiatry 1996;168:121–6 [DOI] [PubMed] [Google Scholar]
- 14.Nater UM, Lin J-MS, Maloney EM, et al. Psychiatric comorbidity in persons with chronic fatigue syndrome identified from the Georgia population. Psychosom Med 2010;72:506–7 [DOI] [PubMed] [Google Scholar]
- 15.Bombardier CH, Buchwald D Outcome and prognosis of patients with chronic fatigue vs chronic fatigue syndrome. Arch Intern Med 1995;155:2105–10 [PubMed] [Google Scholar]
- 16.Smith WR, Noonan C, Buchwald D Mortality in a cohort of chronically fatigued patients. Psychol Med 2006;36:1301–6 [DOI] [PubMed] [Google Scholar]