Abstract
Objectives
To describe the plans of English NHS hospitals to implement ePrescribing systems.
Design and setting
Questionnaire-based survey of attendees of the National ePrescribing Forum.
Participants
A piloted questionnaire was distributed to all NHS and non-NHS hospital-based attendees. The questionnaire enquired about any completed or planned implementation of ePrescribing systems, the specific systems of interest, and functionality they offered.
Main outcome measures
Estimate of the number of NHS Trusts planning to implement ePrescribing systems.
Results
Ninety-one of the 166 questionnaires distributed to NHS hospital-based staff were completed and returned. Of those, six were incomplete, resulting in a total usable response rate of 51% (n = 85). Eighty-two percent (n = 46) of the 56 Trusts represented at the Forum were either ‘thinking of implementing’ or ‘currently implementing’ an ePrescribing system, such as Ascribe (13%, n = 7) and JAC (20%, n = 11). Forty percent (n = 22) of respondents specified other systems, including those procured by NHS Connecting for Health e.g. RiO, Lorenzo and Cerner. Knowledge support, decision support and computerized links to other elements of patients’ individual care records were the functionalities of greatest interest.
Conclusion
There is considerable reported interest and activity in implementing ePrescribing systems in hospitals across England. Whether such developments have the desired impact on improving the safety of prescribing is however, yet to be determined.
Introduction
Given the ever increasing array of medicines now available, clinicians may find daily prescribing, dispensing and administering of drugs somewhat challenging. Electronic prescribing (ePrescribing) systems can help support clinicians in this important task by both assisting in the identification of appropriate treatments and dosages, and highlighting possible drug-history related contraindications and drug-drug interactions. ePrescribing has the potential to improve patient safety by mitigating the possibility of such drug errors.1–4 NHS Connecting for Health (NHS CfH), the ‘Arm's Length Body’ charged with commissioning and implementing the National Programme for Information Technology in England, has defined ePrescribing as ‘the utilisation of electronic systems to facilitate and enhance the communication of a prescription or medicine order, aiding the choice, administration and supply of a medicine through knowledge and decision support and providing a robust audit trail for the entire medicines use process’.5 Referred to as computerized provider (prescriber or physician) order entry (CPOE) systems in different contexts, ePrescribing applications can also incorporate computerized decision support (CDS) systems functionality with varying degrees of sophistication. CDS systems are active knowledge systems, which use real-time patient-specific information to generate individualized prescribing advice. CDS systems range from commercially available off-the-shelf systems – as have, for example, been procured by NHS CfH – to more tailored home-grown applications.
With virtually all UK primary care employing some form of ePrescribing system,6 NHS CfH has concentrated on the development of ePrescribing functionality in secondary care.7 In order to inform a planned programme of work studying the implementation of ePrescribing systems into hospitals, we undertook a descriptive study aiming to provide an overview of the landscape in relation to ePrescribing implementations in English hospitals. This is, as far as we are aware, the first study of its kind anywhere in the UK.
Materials and methods
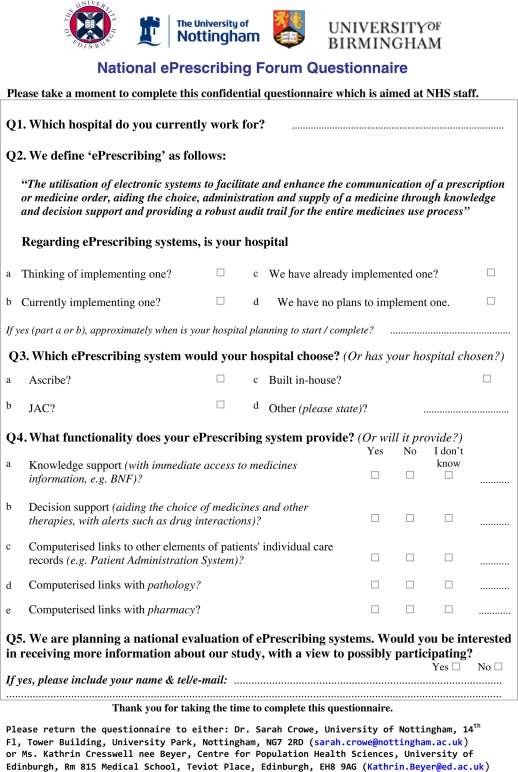
Questionnaire development and distribution
Informed by reading the literature and our previous experiences of undertaking related work on prescribing safety and IT implementation in healthcare,8–13 we developed a semi-structured questionnaire to describe what is currently happening and/or planned to happen in relation to the implementation of hospital ePrescribing systems (Appendix 1). It started by asking NHS staff to identify the hospital which they currently worked for. Respondents were then provided with the NHS CfH's definition for ePrescribing (as stated above) and asked whether their hospital had already implemented, or had plans to implement, such a system. If they indicated that their hospital is ‘currently implementing’ or ‘thinking of implementing’ an ePrescribing system, respondents were asked approximately when their Trust was planning to start/complete this process. The remaining sections inquired about the type of ePrescribing system that is of interest and the functionality this would provide.
The questionnaire had several rounds of development before being piloted within our research team, which consisted both of academics and clinicians with established interests and expertise in relation to ePrescribing systems. Because of the difficulties of singling out NHS staff, one questionnaire (containing a unique reference number) was placed in each delegate pack and distributed to all attendees at the NHS CfH-organized one-day ‘National ePrescribing Forum’ (February 2010, Birmingham, UK). This Forum attracted a mix of healthcare professionals (mainly hospital-based clinicians, pharmacists or IT programme managers/leads) from different NHS Trusts, particularly those who were considering ePrescribing, or were already doing so. There were also a limited number of attendees from commercial organizations, universities, Strategic Health Authorities, Primary Care Trusts and other professional societies and agencies who were also given the questionnaire; however, any data provided by these respondents who were not working in acute hospital or mental health settings and, therefore, not the focus of our enquiry, were omitted. Delegates were reminded by the first speaker to complete the questionnaire and hand it to a member of the research team when leaving the first session. Respondents from the same acute or mental health Trust were identified from the delegate list to avoid double counting. If discrepancies were found to exist in the answers of two respondents from the same Trust, the category 'Don't know' was assigned. If discrepancies existed in the answers of three or more respondents from the same Trust, the most common answer was chosen. Should all answers differ, the category 'Don't know' was assigned. NHS non-respondents (identified from the delegate list) were sent an e-mail reminder approximately four weeks after the forum inviting them to complete an electronic version of the questionnaire.
Data handling and analysis
Data were entered into Excel before being imported into SPSS v17.00 for analysis. Descriptive statistical testing was performed, with percentages of categorical variables calculated.
Results
Response rate and population demographics
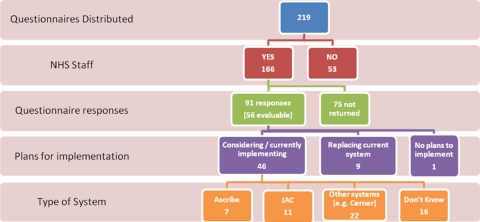
Of the 219 Forum delegates to whom questionnaires were distributed, 53 were identified as non-NHS hospital-based staff. Ninety-one of the 166 questionnaires distributed to NHS hospital-based staff were returned. A further six questionnaires were excluded because Questions 1 or 2 were found to be incomplete, resulting in a total usable response rate of 51% (n = 85). Thirty-two ‘duplicate’ responses were received from staff working in the same hospital; thus 56 hospital Trusts (89% Acute, n = 50 and 11% Mental Health, n = 6) were represented (Figure 1).
Figure 1.
Flowchart depicting the number of Trusts planning to implement ePrescribing systems and the type of system chosen
System implementation
Eighty-two percent (n = 46) of Trusts were either ‘thinking of implementing’ or ‘currently implementing’ an ePrescribing system. Fifty-two percent (n = 24) of these also specified a start or completion date for implementation. Of those who had already implemented an ePrescribing system (16%, n = 9), two respondents were either ‘thinking of implementing’ or ‘currently implementing’ a replacement system. Only one Trust had no plans to implement such a system.
Type of system
Thirteen percent (n = 7) and 20% (n = 11) of respondents indicated that their hospital is currently implementing or in the future likely to implement the Ascribe and JAC systems, respectively. Forty percent (n = 22) of respondents specified other systems, including those procured by NHS CfH, i.e. RiO, Lorenzo and Cerner. No respondents' hospital chose to build their own system in-house. Twelve respondents were unsure what system their hospital would pick and were included in the ‘don't know’ category; respondents (n = 3) who left the answer blank or choose more than one system (n = 1) were also included in this category.
Type of system functionality specified
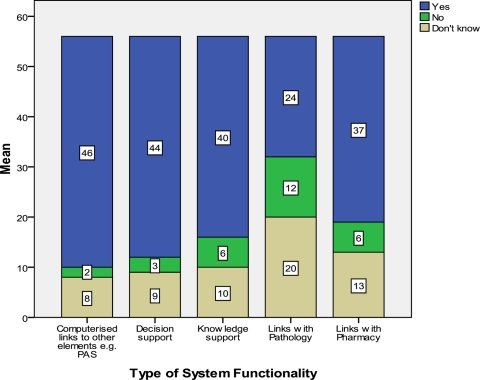
Eighty-two percent (n = 46) of respondents indicated that their hospital is planning to implement ePrescribing systems which provides or will provide knowledge support functionality. Respondents indicated that 79% (n = 44) and 71% (n = 40) of chosen systems would also provide decision support functionality and computerized links to other elements of the patient record such as the Patient Administration Systems (PAS). A higher proportion of respondents were unsure whether their ePrescribing system would provide links with pathology 36% (n = 20) and pharmacy 23% (n = 13) services, respectively. Two respondents left the answer completely or partially blank and were included in the ‘don't know’ category (Figure 2).
Figure 2.
Graphical representations of the type of system functionality provided by ePrescribing systems that are currently being (or planned to be) implemented
Ninety-three percent (n = 52) of respondents requested more information on the national evaluation of ePrescribing systems study which our team is planning to conduct.
Discussion
Statement of principal findings
Our findings indicate that there is considerable interest from Acute and Mental Health Trusts in England to embrace technological advances in information delivery and implement ePrescribing systems in England. The majority of respondents indicated that their Trusts were either actively considering or already implementing an ePrescribing system. No Trust chose to develop their ePrescribing systems in-house, perhaps wishing to avoid the time and expense required.14 National products with innate ePrescribing functionality (like iSOFT Lorenzo and Cerner Millennium, delivered as part of the National Programme for IT) were among the examples of systems respondents' hospitals had chosen. Given the reported delays and political uncertainty surrounding the delivery of these national software products,15 respondents may have been encouraged to choose products outside the Programme, such as Theriak from CIS Healthcare Limited and Soarian from Siemens.
Knowledge support, decision support and computerized links to other elements of patients' individual care records were the most popular functionalities identified as being necessary in ePrescribing systems. Knowledge support provides links to a repository of clinical information and can give details of all items ordered electronically, including costs. As such, knowledge bases can supplement gaps in clinicians' knowledge and help inform their decision-making. Decision support applications provide computerized advice on drug doses, routes and frequencies, and perform checks for drug-allergy or drug-drug interactions. With advanced decision support functionality, information is obtained from the wider patient record and dosages adjusted in light of patient characteristics and other medications currently being taken. By improving clinical decision-making, these applications have the potential to impact on the quality and perhaps most importantly the safety of healthcare.
Strengths and weaknesses of the study
Data were obtained from 50 of the 76 (66%) acute hospitals and six of the 14 (43%) mental health Trusts represented at this National ePrescribing Forum. While these data obtained from key staff working in a large number of Trusts from across England provide a useful snapshot of the current picture with respect to the implementation of ePrescribing systems in these settings, care must be taken when attempting to extrapolate from these findings both to non-responders and the 92 hospital and 59 mental health Trusts in England that were not represented at this Forum. This is because those attending and/or responding are likely to have an established interest in ePrescribing. As mentioned earlier, the category 'Don't know' was also assigned if discrepancies were found to exist in the answers of two respondents from the same Trust. These summary statistics are, therefore, likely to over-estimate the true proportion of Trusts implementing ePrescribing nationally. Care should also be taken in interpreting the summary measures as, given the convenience nature of the sample, we did not calculate confidence intervals. Despite these limitations, however, there is clear evidence of the considerable interest and activity in relation to ePrescribing implementation in the acute and mental health NHS settings in England.
Meaning of the study
ePrescribing has the potential to substantially improve patient safety by reducing medication errors.16–18 Such systems are highly variable in functionality and also in the extent to which they integrate with other clinical systems. Our study showed a high number of Trusts were either ‘thinking of implementing’ or ‘currently implementing’ ePrescribing systems, choosing commercially available or NHS CfH-produced systems. Kuperman et al. recommend that organizations should review the suitability of medication-related decision support functionality compared to developing their own locally (when appropriate expertise exists).19 Customizing commercial knowledge bases to more suit the local hospital environment was also considered necessary to realize the benefits.20
Unanswered questions and future research
As far as we are aware, this is the first investigation to provide a useful snapshot of the current picture with respect to the implementation of ePrescribing systems in acute and mental health NHS settings anywhere in the UK. Our findings suggest that a number of Trusts in England have either already implemented or are at some stage of the process of implementing ePrescribing systems. Given this activity and the reported interest in evaluating the success or otherwise of such implementations, there is both the need and opportunity for well-designed prospective evaluations.21
DECLARATIONS
Competing interests
None declared
Funding
This work received no direct funding. SC and KC are supported by a grant from the NHS Connecting for Health Evaluation Programme (NHS CFHEP 005). KC is also supported by a MRC Doctoral Studentship
Ethical approval
Not applicable
Guarantor
SC
Contributorship
SC and KC conducted the questionnaire survey. SC led the writing of this paper with KC, TA, AS, JC and AS all commenting on various drafts
Acknowledgements
None
Reviewer
Jasdeep Gill
Appendix 1
References
- 1.Leape LL A systems analysis approach to medical error. J Eval Clin Pract 1997;3:213–22 [DOI] [PubMed] [Google Scholar]
- 2.Leape LL, Berwick DM, Bates DW What practices will most improve safety? Evidence-based medicine meets patient safety. JAMA 2002;288:501–7 [DOI] [PubMed] [Google Scholar]
- 3.Bates DW, Cohen M, Leape LL, et al. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc 2001;8:299–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bates DW Preventing medication errors: a summary. Am J Health Syst Pharm 2007;64:S3–S9 [DOI] [PubMed] [Google Scholar]
- 5.NHS Connecting for Health Electronic Prescribing in Hospitals - Challenges and Lessons Learned. London: NHS Connecting for Health, 2009 [Google Scholar]
- 6.Car J, Black A, Anandan C, et al. A Systematic Overview & Synthesis of the Literature. Report for the NHS Connecting for Health Evaluation Programme,2008
- 7.NHS Connecting for Health. ePrescribing Functional Specification for NHS Trusts. See http://www.connectingforhealth.nhs.uk/systemsandservices/eprescribing/baselinefunctspec.pdf .
- 8.Cresswell K, Sheikh A The NHS Care Record Service (NHS CRS): recommendations from the literature on successful implementation and adoption. Inform Prim Care 2009;17:1–8 [DOI] [PubMed] [Google Scholar]
- 9.Catwell L, Sheikh A Information Technology (IT) system users must be allowed to decide on the future direction of major national IT initiatives. But the task of redistributing power equally amongst stakeholders will not be an easy one. Inform Prim Care 2009;17:1–4 [DOI] [PubMed] [Google Scholar]
- 10.Avery AJ, Savelyich BS, Sheikh A, et al. Improving general practice computer systems for patient safety: qualitative study of key stakeholders. Qual Saf Health Care 2007;16:28–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cresswell K, Fernando B, McKinstry B, Sheikh A Adverse drug events in the elderly. British Medical Bulletin 2007;83:1–16 [DOI] [PubMed] [Google Scholar]
- 12.Avery AJ, Rogers S, Cantrill JA, et al. Protocol for the PINCER trial: a cluster randomised trial comparing the effectiveness of a pharmacist-led IT-based intervention with simple feedback in reducing rates of clinically important errors in medicines management in general practices. Trials 2009;10:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris CJ, Savelyich BS, Avery AJ, Cantrill J, Sheikh A Patient safety features of clinical computer systems: questionnaire survey of GP views. Qual Saf Health Care 2005;14:164–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Field TS, Rochon P, Lee M, et al. Costs associated with developing and implementing a computerized clinical decision support system for medication dosing for patients with renal insufficiency in the long-term care setting. J Am Med Inform Assoc 2008;15:466–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.eHealth Insider See http://www.e-health-insider.com/news/5959/isoft_hit_by_'political_uncertainty' (last checked 10 July 2010)
- 16.Bates DW, Cohen M, Leape LL, et al. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc 2001;8:299–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kohn LT, Corrigan JM, Donaldson MS To Err is Human, Building a Safer Health System. Washington, DC: National Academy Press, 2000 [PubMed] [Google Scholar]
- 18.Rind DM, Safran C, Phillips RS, et al. Effect of computer-based alerts on the treatment and outcomes of hospitalized patients. Arch Intern Med 1994;154:1511–17 [PubMed] [Google Scholar]
- 19.Kuperman GJ, Bobb A, Payne TH, et al. Medication-related clinical decision support in computerized provider order entry systems: a review. J Am Med Inform Assoc 2007;14:29–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuperman GJ, Reichley RM, Bailey TC Using commercial knowledge bases for clinical decision support: opportunities, hurdles, and recommendations. J Am Med Inform Assoc 2006;13:369–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Catwell L, Sheikh A Evaluating eHealth interventions: the need for continuous systemic evaluation. PLoS Med 2009;6:e1000126. [DOI] [PMC free article] [PubMed] [Google Scholar]