Central serous chorioretinopathy (CSCR) is often self-limiting but can have serious ocular complications. We present a case of severe visual loss secondary to chronic CSCR in a renal transplant patient on long-term corticosteriods.
Case history
A 50-year-old man presented to the eye clinic with a 12-month history of a gradual loss of vision in the right eye. He had no significant past ocular history but had been diagnosed at the age of 10 years with Henoch-Schonlein nephritis. He had a renal transplant in 1997 and had been taking oral prednisolone for the past 12 years as part of his immunosuppression regime. He also suffered from hyperparathyroidism and had recently been diagnosed with type 2 diabetes. At the time of presentation his medication included immunosuppression with cyclosporin 50 mg twice daily, azothiaprine 100 mg and prednisolone 7.5 mg. He was also on candesartan, atenolol, furosemide, simvastatin, alfacalcidol, darbepoetin alfa and cinacalcet.
On examination his visual acuities were 2/60 in the right eye and 6/4 in the left eye. The anterior segments, intraocular pressures and crystalline lenses were normal in both eyes. A dilated ophthalmic examination revealed diffuse non-specific retinal pigment epithelial (RPE) changes in both eyes. There were no clinical signs of subretinal fluid or neurosensory or pigment epithelial retinal detachments in either eye although the ocular coherence tomogram (OCT) detected shallow extrafoveal subretinal fluid in the left eye. The OCT, fundus autofluorescence (FA) and fundus fluorescein angiogram (FFA) findings are shown in Figure 1. The optic discs were healthy.
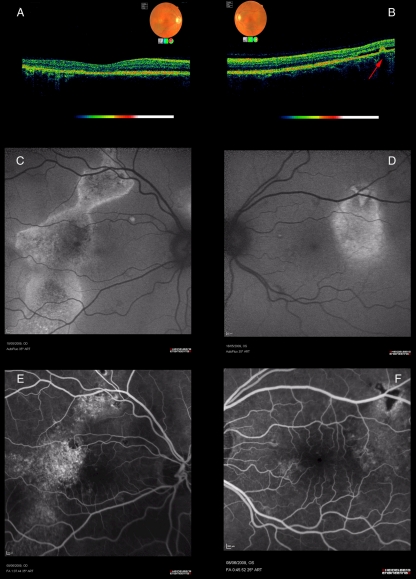
Figure 1.
Showing the OCT, fundus autofluorescence and angiographic findings in the right and left eyes at presentation. A and B: OCT images captured on the Topcon 3D OCT 1000. No subretinal fluid seen in the right eye (1A). Left eye shows disruption of the retinal pigment epithelium associated with shallow subretinal fluid localized to the superotemporal macular area (red arrow) (1B). C and D: Fundus autofluorescence images captured on the Heidelberg retina angiograph 2 (HRA 2). There is an area of mottled reduced autofluorescence with bright margins, a gravitational distribution and extensive foveal involvement in the right eye (1C). The left eye shows a localized and relatively uniform area of increased autofluorescence, sparing the macula (1D). E and F: Fundus fluorescein angiogram images captured on HRA 2. There is mottled hyperfluorescence in the right eye at 1 minute corresponding to the area of abnormal fundus autofluorescence (1E). The left eye at 45 seconds shows a triangular area of hypofluorescence (corresponding to a similar shaped area of increased fundus autofluorescence) surrounded by mottled hyperfluorescence (1F). Neither eye showed any area of focal hyperfluorescence or choroidal neovascularization
A diagnosis of steroid-induced chronic central serous retinopathy was made. The right eye had inactive end-stage disease. However, the presence of shallow subretinal fluid in the left eye indicated residual disease activity in this eye. If left untreated there remained the threat of foveal involvement and loss of vision. After discussion with the treating renal physician and the patient it was decided to reduce the oral prednisolone while jointly monitoring both the renal function and the ophthalmic condition. His oral prednisolone has been gradually reduced over three months from 7.5 mg to 2 mg. Both his transplant function and ocular status remain stable on this reduced dose.
Discussion
Central serous chorioretinopathy (CSCR) is an ocular disease that typically presents with blurred vision and a neurosensory detachment of the central macula.1 While most cases are self- limiting and recover good visual acuity, the severe variants of CSCR are less likely to resolve with one study showing only 52% of eyes regaining 6/6 vision.2
The cause of CSCR is unknown and the majority are considered to be idiopathic.3 However, several studies have shown an association between corticosteroid use and CSCR.1–4
Multiple routes of steroid administration have been implicated including oral, intravenous, inhaled, intranasal, epidural and intra-articular forms.5 The underlying pathogenesis of CSCR secondary to steroid therapy has been attributed to disruption of the blood retinal barrier, hyperpermeability of the choriocapillaris and damage to the retinal pigment epithelial pump.1
There are several published reports describing the development of CSCR in renal transplant patients.6,7 This case is challenging because when the patient first presented to the eye clinic, he had already developed irreversible sight loss in one eye and had an active sight-threatening disease in the other. The immune suppression with low dose prednisolone, however, was considered necessary to prevent renal graft failure. The patient had to make a difficult decision between continuing the steroids and risk losing his sight entirely, or reducing his steroids and risking loss of the transplant. After careful consideration he chose to try to preserve his vision and reduce the steroids as far as possible, knowing that if the transplant were to fail he could revert to haemodialysis to replace his renal function.
Management of idiopathic CSCR is reassurance and observation unless it develops into chronic or recurrent disease. Second-line treatment may include photodynamic therapy, anti-vascular endothelial growth factors (anti- VEGF) or non-visible subthreshold micropulse diode laser.8,9 Verteporfin photodynamic therapy has shown promising results but complications such as choroid neovasuclarization and damage to the choroidal circulation are limitations to its use.9,10 A recent prospective trial using low fluence rate photodynamic therapy demonstrated improved subretinal fluid and visual acuity while inducing less damage to the choroidal circulation than normal fluence photodynamic therapy, however, this study excluded patients who were taking corticosteriods.10 Intravitreal anti-VEGF agents have also been used in the management of chronic CSCR and a recent study suggests it may be an alternative treatment option.11 Non-visible subthreshold micropulse diode laser has shown promising results in smaller studies with short-term follow-up.9
For CSCR secondary to steroid use, however, the first line of management would be to remove the underlying cause by taking the patient off the drug. The important management issues to consider in this case would be: (1) the morbidity of renal graft failure versus the possibility of bilateral and irreversible loss of vision; (2) whether a reduced steroid dose would be sufficient to halt the disease as opposed to complete withdrawal; and (3) the effectiveness of second-line ophthalmic treatments for CSCR if the patient remained on low-dose prednisolone. Close liaisons with the treating renal physician and active patient involvement in the decision-making processes are the key to managing this complex case.
DECLARATIONS
Competing interests
None declared
Funding
The funding of this case report was supported by an educational grant provided by the Ophthalmic Department of Novartis Pharmaceuticals UK Ltd
Ethical approval
Written informed consent to publication has been obtained from the patient or next of kin
Guarantor
SP
Contributorship
SP and AH wrote the case report. SP was the patient's ophthalmic consultant and obtained the images. KA was the renal consultant involved in the patient's care and editor the report prior to submission. SP was the supervising author for the paper
Acknowledgements
None
Reviewer
Balini Balasubramaniam
References
- 1.Loo J-L, Lee S-Y, Ang C-L Can long-term corticosteroids lead to blindness? A case series of central serous chorioretinopathy induced by corticosteroids. Ann Acad Med Singapore 2006;35:496–9 [PubMed] [Google Scholar]
- 2.Otsuka S, Ohba N, Nakao K A long-term follow-up study of severe variant of central serous chorioretinopathy. Retina 2002;22:25–32 [DOI] [PubMed] [Google Scholar]
- 3.Levy J, Marcus M, Belfair N, Klemperer, Lifshitz T Central serous chorioretinopathy in patients receiving systemic corticosteroid therapy. Can J Opthalmol 2005;40:217–21 [DOI] [PubMed] [Google Scholar]
- 4.Wakakura M, Song E, Ishikawa S Corticosteroid-induced central serous chorioretinopathy. Jpn J Ophthalmol 1997;41:180–5 [DOI] [PubMed] [Google Scholar]
- 5.Bouzas EA, Karadimas P, Pournaras CJ Central serous chorioretinopathy and glucocorticoid. Survey of Ophthalmology 2002;47:431–48 [DOI] [PubMed] [Google Scholar]
- 6.Kian-Ersi F, Taheri S, Akhlaghi MR Ocular disorders in renal transplant patients. Saudi J Kidney Dis Transpl 2008;19:751–5 [PubMed] [Google Scholar]
- 7.Oliaei F, Rasoulinejad SB An ophthalmological complication: central serous chorioretinopathy in a renal transplant recipient. Transplantation Proceedings 2007;39:1134–5 [DOI] [PubMed] [Google Scholar]
- 8.Chan WM, Lam DSC, Lai TY, et al. Choroidal vascular remodelling in central serous chorioretinopathy after indocyanine green guided photodynamic therapy with verteporfin: a novel treatment at the primary disease level. Br J Ophthalmol 2003;87:1453–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lanzetta P, Furlan F, Morgante L, Veritti D, Bandello F Nonvisible subthreshold micropulse diode laser (810 nm) treatment of central serous chorioretinopathy. A pilot study. Eur J Opthalmol 2008;18:934–40 [DOI] [PubMed] [Google Scholar]
- 10.Reibaidi M, Cardascia N, Longo A, et al. Standard-fluence versus low-fluence photodynamic therapy in chronic central serous chorioretinopathy: a nonrandomized clinical trial. Am J Opthalmology 2010;149:307–15 [DOI] [PubMed] [Google Scholar]
- 11.Artunay O, Yuzbasioglu E, Rasier R, Sengul A, Bahcecioglu H Intravitreal bevacizumab in treatment of idiopathic persistent central serous chorioretinopathy: a prospective, controlled clinical study. Curr Eye Res 2010;35:91–8 [DOI] [PubMed] [Google Scholar]