Abstract
Objectives
To assess the impact of an information poster on rate and accuracy of referrals of abnormal red reflex from general practioners (GP) and hospital doctors involved in the care of children.
Design
A retrospective audit of all referrals for abnormal red reflex received between the periods September 2005 to September 2006 was carried out. Posters were sent to 200 GP practices in East London as well as our local hospital. Pathways for referrals were given, and a prospective re-audit was conducted from October 2006 to March 2008.
Setting
The Royal London Hospital and practices serving the East End of London.
Participants
GPs serving the East End of London and hospital doctors involved in child care.
Main outcome measures
(1) Increase in the referral rate for abnormal red reflex finding; and (2) accuracy of referral for abnormal red reflex.
Results
Prior to posters being sent, there were no referrals of abnormal red reflexes to our department. Following the posters being sent, 21 abnormal red reflex referrals were made over a period of 18 months; 18 from GPs and three from neonatologists. Thirteen were detected at 6 weeks of age (routine screening). Three patients had a positive finding (two with bilateral cataracts and one with hypermetropic astigmatism).
Conclusions
Although an increase in referrals suggests that the assessment of the red reflex is being performed and public awareness has increased, the sensitivity of this test remains low. Management strategies need to be in place to deal with an influx of patients who may have normal assessments and a strategy in East London will be discussed.
Introduction
The assessment of the red reflex is an essential part of a child's examination, and it is commonly performed by general practitioners (GPs) and paediatricians, though some clinicians can be unaware of its continued importance.1 An abnormal test can be associated with many conditions, including life-threatening diseases such as retinoblastoma. Hence, awareness of this examination technique and its correct performance is an important skill for healthcare professionals involved in child care.
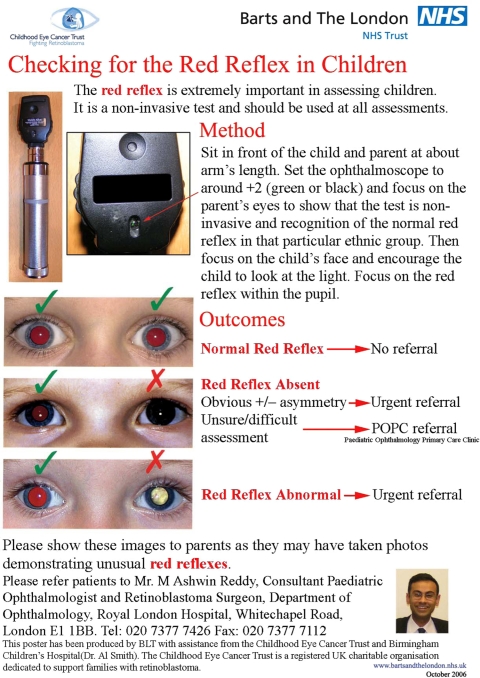
This test is simple, non-invasive and can be performed quickly by the trained examiner. Early diagnosis is extremely important for vision and life-threatening conditions that can cause an abnormal red reflex. We, therefore, designed an information poster (Figure 1) which was sent to all GP practices in north-east London, as well as our paediatric and neonatology departments. Our aim was to improve awareness and promote early referral.
Figure 1.
Abnormal red reflex information poster
Methods
Our department serves a large proportion of the East London community, and it is also a tertiary referral centre for retinoblastoma and other posterior segment disorders of children. During a retrospective audit from September 2005 to September 2006 there were no referrals for abnormal red reflex by GPs or paediatricians, though 557 new paediatric ophthalmology referrals were received.
We designed an information poster which detailed a correct method of assessment, together with colour photographic examples and pathways for onward referral (Figure 1). The examiner was asked to perform the test by sitting in front of the child at approximately an arm's length, then set the ophthalmoscope to +2 diopters, and focus the light on the parents' eyes to show that it is a non-invasive and painless test thus acquiring the child's confidence. This also gives an opportunity to appreciate the red reflex in the particular ethnic group of the child. In the author's opinion this is a common cause of misdiagnosis as darkly-pigmented races often have a duller red reflex due to the increased amount of melanin pigment in their fundus. Then the examiner is asked to focus the light on the child's face and assess the red reflex in both pupils.
The poster was sent to 200 GP practices in East London as well as our hospital paediatric and neonatology units. Practices and departments were asked to display the poster in a public place in order to make parents aware, in case they have noticed an abnormal red reflex in any of their child's photographs.
The examiner was required to refer any white, absent or asymmetric reflexes to the ophthalmologist. If they were unsure then they may refer to the paediatric ophthalmology primary care clinics (POPC) where further assessment will be carried out by qualified optometrists and orthoptists. The staff in these clinics are members of the retinoblastoma team at Barts and the London NHS Trust, and children who are found to have a true red reflex abnormality will be able to see a consultant ophthalmologist within 24 hours.
A prospective audit was conducted for 18 months after these posters were sent out. Data were collected on all new patients referred with an abnormal red reflex as their main diagnosis. The patient underwent a red reflex test as well as a complete ocular examination, including dilated fundoscopy and refraction. The data collected included age, race, the red reflex finding and the final diagnosis. In addition all referrers were contacted via telephone and asked if they had seen the poster, and whether it prompted them to refer.
Results
Twenty-one referrals were received with the main complaint of abnormal red reflex. A total of 1588 new referrals were received during that period. The average age at referral was 23.7 weeks (range 6–130). The ethnic origin of the patients referred is shown in Table 1; this shows a large proportion of children from the South Asian community reflecting the population of the East End of London.
Table 1.
The ethnic origin of patients referred with abnormal red reflexes
| Race | n |
|---|---|
| South Asian | 10 (47.6%) |
| White | 2 (9.5%) |
| Chinese | 2 (9.5%) |
| Afro-Carribean | 2 (9.5%) |
| Black | 1 (4.8%) |
| Not stated | 4 (19%) |
Eighteen of these referrals were from GPs and three from neonatologists. Thirteen (72%) GPs responded to our follow-up by telephone. Six (46%) admitted seeing the poster and confirmed it was a prompt for referral. Interestingly, one of these patients was referred because the mother had noticed an abnormal reflex in one of the photographs. It was not ascertained whether she had learnt of this abnormality from our poster or due to general awareness in the media.
Of all the referrals, 18 (86%) were judged to have a normal red reflex, and this was also confirmed by further dilated fundus examination. Two had bilateral cataracts and one had high astigmatism; the overall sensitivity was 14.3%.
Discussion
In our study we initially received no referrals for abnormal red reflexes from our audit of September 2005 to 2006. Our information campaign with distribution of posters in a hospital department and the local GP practices resulted in an increased number of referrals. Six of the local GP referrals responding said they had seen our poster, and it prompted them to refer. In our study we have described an appropriate method for performing the red reflex test, and in particular to use the red reflex of parents in order to gain an impression of what is normal for a particular ethnic group. Our study shows that this test continues to be an important tool in detecting sight-threatening conditions. There were still a relatively high number of normal reflexes, which were identified by our specialist optometrists. The study raises awareness of this important clinical test, however, it remains the responsibility of the clinician to be well familiarized with performing the test and to gain appropriate practice in the clinical setting. The red reflex tests was first described by Bruckner in 1962,1 and has proven to be a very effective test in detecting ocular pathology of children and adults. Gole and Douglas2 have shown that this test can be performed by non-ophthalmologists with a high sensitivity for detecting different causes of amblyopia. Some clinicians continue to remain unaware of the usefulness of this simple test.3 Our study appears to show that once clinicians were reminded of the test, important pathologies were detected and appropriately referred. It is recommended that all newborn babies should undergo this test before discharge from hospital, and at six weeks.
It would be prudent to assess the red reflex whenever a child has an ocular problem, such as a squint or reduced vision. From the referrals we received, three important diagnoses were made and the appropriate management instigated. Visually-threatening disorders such as high hypermetropia and astigmatism may present as abnormal red reflex. It is essential that such children are refracted and placed in glasses promptly in order to prevent amblyopia. Many information campaigns now encourage families and friends to report abnormal red reflexes seen on photographs or other multimedia images.4 This has also been highlighted recently by national media organizations, and so GPs need to know of the growing public awareness and possible increased referrals to their surgeries. If an abnormal finding is detected, or the examiner is not sure, then onward referral to a specialist centre is necessary.
Our referral pathway provided an efficient system for examiners to refer patients that they were concerned about to be further assessed by our allied healthcare professionals. It is customary for these patients to be seen by consultant ophthalmologists but our audit has shown that it is safe for such patients to be seen by appropriately trained ancillary staff.
Continued awareness by healthcare professionals involved in dealing with children is important in the early detection of such sight- and life-threatening conditions. Ophthalmologists involved in the care of children may need to instigate appropriate referral pathways to facilitate early referrals utilizing allied healthcare workers. They should also make sure that all healthcare professionals are made aware of the technique.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Not applicable
Guarantor
MAR
Contributorship
All authors contributed equally
Acknowledgements
None
Reviewer
Jaya Chidambaram
References
- 1.Roe LD, Guyton DL The light that leaks: Bruckner and the red reflex. Surv Ophthalmol 1984;28:665–70 [DOI] [PubMed] [Google Scholar]
- 2.Gole GA, Douglas LM Validity of the Bruckner reflex in the detection of amblyopia. Aust N Z J Ophthalmol 1995;23:281–5 [DOI] [PubMed] [Google Scholar]
- 3.Sotomi O, Ryan CA, O'Connor G, Murphy BP Have we stopped looking for a red reflex in newborn screening? Ir Med J 2007;100:398–400 [PubMed] [Google Scholar]
- 4.Childhood Eye Cancer Trust Information Awareness Campaign. See www.chect.org.uk