Abstract
Objectives
There is no international consensus on the components of anaphylaxis management plans and responsibility for their design and delivery is contested. We set out to establish consensus among relevant specialist and generalist clinicians on this issue to inform future randomized controlled trials.
Design
A two-round electronic Delphi study completed by a 25-person, multidisciplinary expert panel. Participants scored the importance of a range of statements on anaphylaxis management, identified from a systematic review of the literature, on a five-point scale ranging from ‘very important’ to ‘irrelevant’. Consensus was defined a priori as being achieved if 80% or more of panel members rated a statement as ‘important’ or ‘very important’ after Round 2.
Setting
Primary and secondary care and academic settings in the UK and Ireland.
Participants
Twenty-five medical, nursing and allied health professionals.
Main outcome measures
Consensus on the key components of anaphylaxis management plans.
Results
The response rate was 84% (n = 21) for Round 1 and 96% (n = 24) for Round 2. The key components of emergency care on which consensus was achieved included: awareness of trigger factors (100%); recognition and emergency management of reactions of different severity (100%); and clear information on adrenaline (epinephrine) use (100%). Consensus on longer-term management issues included: clear written guidelines on anaphylaxis management (96%); annual review of plans (87%); and plans that were tailored to individual needs (82%).
Conclusions
This national consensus-building exercise generated widespread agreement that emergency plans need to be simple, clear and generic, making them easy to implement in a crisis. In contrast, long-term plans need to be negotiated between patient/carers and professionals, and tailored to individual needs. The effectiveness of this expert-agreed long-term plan now needs to be evaluated rigorously.
Introduction
Anaphylaxis is a rapid onset and potentially life-threatening condition with many possible triggers.1,2 The true frequency of anaphylactic reactions is unknown, but a recent epidemiological review indicated that the incidence of anaphylaxis is approximately 50–2000 episodes per 100,000 person years, with a lifetime prevalence of 0.05–2.0%.3 UK data suggest that the incidence of anaphylaxis may be increasing.4,5 Annually, it results in approximately 150 deaths in the US and 20–30 reported deaths in the UK.6,7 Most cases of anaphylaxis occur unpredictably in community settings, in the absence of a healthcare professional.2,8 Management of anaphylaxis typically focuses mostly on emergency treatment, specifically how to recognize reactions and the prompt administration of intramuscular adrenaline (epinephrine).1,2 Risk assessment and long-term, individualized risk reduction and education along with more effective self-management strategies are, however, potentially crucial in preventing severe and fatal anaphylactic episodes.2,6,7,9
Anaphylaxis management plans are increasingly advocated internationally to improve outcomes and reduce risk of recurrent reactions in people with a history of anaphylaxis.2,10,11 Where patients have access to allergy specialists, evidence suggests that long-term management plans may have successfully reduced the frequency and severity of further reactions in children and adults. One longitudinal case control study, for example, reported an eight-fold reduction in frequency of reactions and 60-fold reduction in frequency of severe reactions in peanut-allergic children following delivery of a written anaphylaxis management plan.12 Allergy clinic-based multidisciplinary team assessment, training and management have also been associated with significant improvements in food avoidance techniques, managing reactions, and the use of adrenaline auto-injectors in children with anaphylaxis.13 These are encouraging data, but the lack of control groups and potential for selection and information biases means that these findings need to be interpreted with caution.14,15
Other than the importance of adrenaline injection, there is no consensus on what should be included in an anaphylaxis management plan.15 Moreover, the responsibility for design and delivery of anaphylaxis management plans is contested. It can be argued that the responsibility lies appropriately with allergy specialists,16,17 but given their paucity in many parts of the world, such an approach may leave most patients with severe allergies receiving minimal support in managing their condition and experiencing significant psychosocial consequences.6,18–20 Even in healthcare systems where allergy specialists are available, referrals for long-term management advice are not routine,2 suggesting that clearer guidelines on remits and responsibilities of specialist and non-specialist staff are needed.
Current knowledge suggests that anaphylaxis management plans may have substantial clinical benefits for patients.12 A more robust methodological approach – ideally a randomized controlled trial – would provide stronger evidence of effectiveness and safety and is increasingly seen as a needed piece of evidence prior to routine implementation of anaphylaxis management plans in national and international policies. This does, however, also throw into sharp focus the need to identify and develop agreement on the key components of such plans. In the short term, professional consensus on the components of anaphylaxis management plans is useful, in the absence of definitive evidence, for developing clinical practice.21 In the longer term, randomized controlled trials – which will, given the relative infrequency of anaphylaxis, inevitably need to be very large – will require professional agreement on the utility and acceptability of the proposed intervention. Regional consensus of expert opinion on the key components of anaphylaxis management plans is, therefore, an essential pre-requisite for such future trials. With this in mind, we aimed to identify and reach clinician consensus on the most important and useful components of anaphylaxis management plans for use in future UK trials.
Methods
Initially, we conducted a systematic review of the randomized controlled trial, and then other potentially relevant experimental, epidemiological and qualitative literature on anaphylaxis management. We also contacted a panel of international anaphylaxis experts to identify anaphylaxis management plans in use worldwide and evaluate the evidence for their effectiveness. The findings from these reviews have recently been reported.14,15 These literature reviews enabled us to identify the core issues concerning anaphylaxis management to inform the consensus-seeking process.
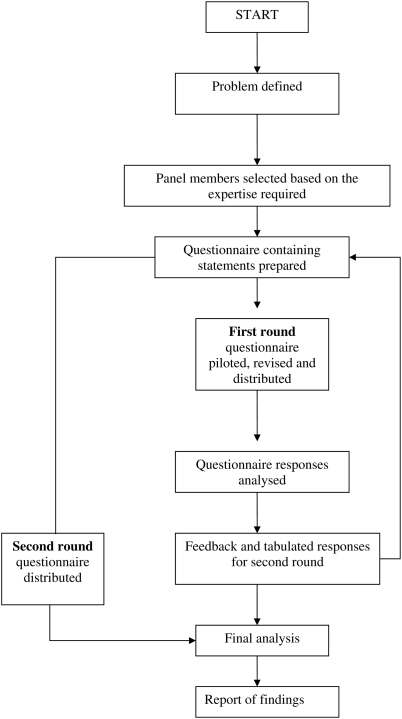
In order to establish professional consensus on the most relevant criteria of anaphylaxis management plans, we used an adaptation of the Delphi technique. This is a method of reaching consensus on a particular research question and has been widely used in healthcare research.22,23 It involves circulating a set of statements, assumptions, solutions or options to be anonymously scored by participants, thereby minimizing the risk of actual or perceived peer pressure influencing participants' responses. Median scores and percentage agreements on the statements are then circulated to the participants who re-score them in the light of other participants' responses. Our adaptation involved undertaking this consensus-building work through e-mail rounds rather than face-to-face meetings, thereby allowing us to engage with our geographically dispersed expert panel in an efficient and cost-effective way. Figure 1 shows the e-Delphi process as used in this study.
Figure 1.
Flow chart for e-Delphi study
The first stage of the e-Delphi process was to identify the panel of experts to participate in the study. To reflect an adequate breadth of expertise and perspectives we purposively selected an expert panel of 26 members with direct experience of anaphylaxis management, drawn from those in clinical and academic healthcare settings in the UK and Ireland. An invitation to participate in the study, sent jointly from the research team and the Anaphylaxis Campaign, was e-mailed to an expert panel of allergy specialists/practitioners with a particular interest in allergy drawn from internal medicine, nursing and allied health professionals, family physicians and school nurses (Table 1).
Table 1.
Demographic and professional characteristics of Delphi expert panel
| Panellist no. | Gender | Professional background | Professional role |
|---|---|---|---|
| 1 | F | Medicine-allergy specialist | Clinical |
| 2 | M | Medicine-allergy specialist | Clinical |
| 3 | M | Medicine | Academic/Clinical |
| 4 | M | Paediatrician | Academic/Clinical |
| 5 | M | Immunologist | Clinical |
| 6 | M | Medicine-allergy specialist | Clinical |
| 7 | F | Nursing | Nurse Advisor |
| 8 | M | Immunologist | Clinical |
| 9 | M | GP | Academic/Clinical |
| 10 | M | GP | Academic/Clinical |
| 11 | F | Nursing | Policy/Research |
| 12 | M | GP | Academic/Clinical |
| 13 | F | Dietician | Academic/Clinical |
| 14 | M | Medicine | Hospital consultant |
| 15*† | M | GP | Clinical |
| 16* | F | Paediatrician | Clinical |
| 17‡ | F | Pharmacy | Academic |
| 18* | M | Paediatrician | Academic/Clinical |
| 19 | F | Nursing | Policy/Academic |
| 20 | F | Nursing | Academic/Clinical |
| 21 | M | Medicine | Academic/Clinical |
| 22 | M | Paediatrician | Clinical |
| 23 | F | Nursing | Academic/Clinical |
| 24 | M | Medicine | Academic/Clinical |
| 25 | F | Nursing | Academic/Clinical |
| 26 | F | Nursing | Academic/Clinical |
*Non-responders Round 1
†Non-responders Round 2
‡Not available: excluded
The e-Delphi questionnaire was designed by identifying, through the systematic literature review,15 key potential issues in emergency and long-term anaphylaxis management for patients, families and professionals. The issues were formalized into 34 statements, which were presented in the questionnaire in two sections: components of anaphylaxis management plans and general issues identified from the literature as contentious. Participants were asked to score the importance of each statement on a five-point Likert scale ranging from ‘very important’ to ‘irrelevant’. Free text comments were encouraged in order to capture the reasons for participants' opinions. The questionnaire was piloted with five professionals.
Following Round 1, we calculated the median score and the percentage agreement for each item using SPSS (v14.0). These values were incorporated into the Round 2 questionnaire and panel members were asked to re-score each item with knowledge of what other panel members had overall scored each item in Round 1. An additional question (Q 35) was added to the Round 2 questionnaire, in response to strongly-expressed views from a number of panel members in Round 1 that emergency and long-term management issues should be considered separately.
All information was then collated and assessed for consensus. Consensus was defined a priori as having been achieved if 80% or more of the panel members rated a statement as ‘very important/strongly agree’ or ‘important/agree’ after Round 2.
Free text comments were collated and content analysis undertaken to capture the range and strength of opinions expressed.
Results
Twenty-five of the 26 experts initially approached agreed to participate. We achieved a response rate of 84% (n = 21) to Round 1 and 96% (n = 24) to Round 2. There was over 80% agreement of importance on 20 of the 35 statements after Round 2, this including the need separately to consider emergency and long-term management considerations.
The items which it was agreed should form part of an emergency anaphylaxis management plan are shown in Table 2. Overall, our findings revealed strong support for a short simple emergency plan focused on recognition of severity of the reaction (100% agreement), prompt and appropriate treatment with adrenaline (100%), and summoning of emergency services (100%).
Table 2.
Consensus on the components of emergency anaphylaxis management plans in rank order
| Components | % |
|---|---|
| Contact details – names and numbers – for emergencies, including family members to be contacted in an emergency | 100 |
| Details of the individual's allergies/known trigger factors | 100 |
| Generic and proprietary names of drugs and possible cross-sensitivities to drugs, if relevant | 100 |
| How to recognize the signs and symptoms of mild, moderate and severe allergic reactions and how to act in each case | 100 |
| Medication prescribed and when it should be used | 100 |
| Management of emergencies: actions to be taken and medications to be used | 100 |
| Clear statement of the need to administer adrenaline without hesitation | 100 |
| When to call emergency services | 100 |
| Where medication is stored at home, in school, or workplace | 96 |
| Review dates for prescribed medication if appropriate, e.g. when child reaches 30 kg in weight, importance of checking expiry dates | 87 |
| Number of injectable adrenaline devices (e.g. Epipens) required | 83 |
| Who is trained to administer medication in home, school, workplace | 80 |
Consensus was achieved on certain principles of long-term management (Table 3), these including the need for clear guidelines in healthcare, school and work settings (96%), the need for regular review of plans (87%) and the need for personalized plans tailored to the individual's particular circumstances (82%). Other aspects of long-term management were contentious and there were some differences which appeared to reflect the professional role of the respondent and whether allergy specialist services were available locally. Aspects of long-term anaphylaxis management on which consensus was not attained (Table 4) included whether non-specialists in allergy can diagnose anaphylaxis (70%), and design and deliver anaphylaxis management plans (78%). There was little support for written advice on the social management of risk (46%) and documentation of patients' concerns about the impact of anaphylaxis on their lives (12%).
Table 3.
Consensus on the principles of long-term anaphylaxis management in rank order
| Principles | % |
|---|---|
| Clear, written guidelines on anaphylaxis management, including referral pathways, should be in place in all healthcare, work and school settings | 96 |
| Plans should be reviewed if a severe allergic reaction occurs | 96 |
| Oral antihistamines, inhalers and/or injectable adrenaline (e.g. Epipen), if prescribed, should be accompanied by information on their use | 91 |
| Anaphylaxis management plans should be reviewed annually including reassessment of patient/parent knowledge of anaphylaxis management and emergency treatment | 87 |
| Quality Outcome Framework (QOF) targets for anaphylaxis reviews in primary care would improve standards of care | 86 |
| Plans should be reviewed when a child starts nursery or a new school | 83 |
| Anaphylaxis management plans should be personalized to the patient's circumstances and tailored to age | 82 |
| Anaphylaxis management plans should focus on emergency care. Long-term management plans should be addressed in a separate document | 80 |
Table 4.
Statements on which consensus was not attained in rank order
| Statements | % |
|---|---|
| For each patient, there should be a named clinician responsible for planning, coordinating and managing care for people with a history of anaphylaxis | 78 |
| GPs, school nurses and/or practice nurses, if trained, can safely design and deliver anaphylaxis management plans | 78 |
| The diagnosis of anaphylaxis should be confirmed by an allergy specialist | 70 |
| Written advice on dietary management, if relevant | 67 |
| An indemnity statement for school and workplace staff involved in administering adrenaline | 65 |
| Injectable adrenaline (e.g. Epipen) should only be prescribed when there is increased risk, such as known airway involvement in previous reaction, history of asthma or reaction to even a trace of nut | 61 |
| Signatures of patient/parent, clinical staff, head teacher, workplace staff as relevant | 58 |
| Contact details for information, advice and support, including the Anaphylaxis Campaign | 54 |
| Written advice on minimizing exposure to bees and wasps, if relevant | 50 |
| Statement that anaphylaxis can be fatal | 50 |
| Written advice on managing specific social situations, e.g. eating out, parties, school trips, travel abroad, if relevant | 46 |
| An allergy specialist should design and deliver anaphylaxis management plans | 35 |
| GPs should not prescribe injectable adrenaline without referral to a specialist | 26 |
| Written advice on interpreting food labels, if relevant | 25 |
| Record of discussion about particular concerns the patient may have about impact on lifestyle | 12 |
Free text comments by panel members explained the scores given, raised uncertainties and highlighted a number of contentious issues in anaphylaxis management where views were polarized.
Emergency anaphylaxis management plans
Panel members indicated that clarity, simplicity and brevity are the cornerstones of an emergency anaphylaxis management plan. Clear advice about recognizing the symptoms of mild, moderate and severe reactions and how to respond was viewed as crucial.
‘The management plan, I believe, should be very simple and easy to read in a crisis.’ (Participant 7)
‘The anaphylaxis management plan should focus on crisis avoidance and crisis response.’ (Participant 24)
‘Differentiation of grades of reaction of prime importance in determining appropriate self-treatment. V[ery] important.’ (Participant 8)
The statements on medications attained a high level of consensus, but revealed some variations in practice, particularly in the number of adrenaline auto-injectors prescribed, with participants reporting a range of preferences from one to four. Factors which contributed to more adrenaline auto-injectors being prescribed included parental anxiety, geographical distance from emergency services and individual patient circumstances. The importance of all relevant parties taking responsibility for prescribing and administering adrenaline was stressed:
‘Failure to take responsibility could lead to unnecessary death.’ (Participant 9)
Long-term anaphylaxis management plans
Long-term advice and management concerning factors such as minimizing exposure to risk and management of social situations was seen as important, but part of a separate package of care:
‘It is good advice, but will dilute the action plan.’ (Participant 24)
Clear distinctions were made between acute and long-term management:
‘Acute management should be simple, didactic and generic and NOT tailor-made. Preventive plans absolutely important to individualize with a generic component and specific tailor-made aspects.’ (Participant 3)
There were diverse views about the level of detail required in long-term plans. Some expressed doubt about the value of written advice on avoidance, describing it as ‘common sense surely’ (Participant 9), or not useful. Written advice on dietary management, interpreting food labels and management of social situations was not well-supported. A wide range of views was also expressed on the regularity of which an anaphylaxis management plan should be reviewed, from two- to three-monthly to three-yearly, but overall the importance of regular reviews was stressed:
‘It is an under-appreciated reason why allergy services need support as the ongoing needs of families after diagnosis are almost as great as the need for a diagnosis in the first place. This review is in the remit of an experienced practice nurse or specialist hospital nurse.’ (Participant 24)
Consensus was attained on the separation of emergency and long-term anaphylaxis management plans (80%).
‘Absolutely. Anaphylaxis plans should be very short and easy to read. Patients and carers cannot read detailed documents in an emergency.’ (Participant 7)
‘There could be a separate area within the document to detail specifics for that individual… Preventative issues might be recorded in an area of this document. Long-term management and emergency care should in some ways cross over and be thought about together as one component in the care.’ (Participant 19)
‘No need for second document – over-bureaucratic. Plan needs to fit into Epipen box, purse or wallet if what to do in emergency is to make any sense at all.’ (Participant 25)
Specialist and generalist roles in anaphylaxis management
Many respondents drew a distinction between the ‘ideal world’, where ‘everyone with anaphylaxis should see a specialist’ (Participant 1), and reality, where there are ‘too few allergists to go round’ (Participant 3), where specialist clinics may have long waiting lists and there are major geographical gaps in provision of specialist services. Some participants indicated that allergy specialists should have the major responsibility for design and delivery of anaphylaxis management plans, due to their ability to make an accurate diagnosis and give expert advice. The lack of access for many patients to such specialists led most participants to suggest that primary care will play a key role:
‘In the UK with poor access to allergists the primary care team must be able to form an initial management plan including instruction in the use of EpiPens and when to use prior to being seen by an allergist.’ (Participant 9)
Concerns were expressed that GPs and school nurses may lack sufficient understanding of anaphylaxis and consequently provide inadequate information and training for patients/parents in anaphylaxis management and the use of injectable self-administered adrenaline. The key to effective management was, therefore, seen as: clear delineation of roles and responsibilities; adequate training for primary care and education staff in anaphylaxis management; defined competencies; clearer guidelines; an integrated, cross-sector, multidisciplinary approach to anaphylaxis management; sufficient resources to support specialist services and increase capacity in primary care. These were, however, considered by participants to be largely lacking in current practice.
The components of emergency and long-term anaphylaxis management plans
Based on the UK professional consensus attained in this study, we can recommend the components of emergency anaphylaxis management plans (Table 5). Consensus on the underpinning principles of long-term anaphylaxis management on which plans should be based included:
Anaphylaxis management plans should be personalized to the patient's circumstances and tailored to age;
Clear, written guidelines on anaphylaxis management, including referral pathways, should be in place in all healthcare, work and school settings;
Plans should be reviewed regularly and also if a severe allergic reaction occurs and at significant times such as when a child starts nursery or a new school;
Oral antihistamines, inhalers and/or injectable adrenaline, if prescribed, should be accompanied by clear information on their use.
Table 5.
Recommended components of a plan for managing anaphylactic emergencies
| Recommended components |
|---|
| Contact details – names and numbers – for emergencies, including family members to be contacted in an emergency |
| Details of the individual's allergies/known trigger factors |
| Generic and proprietary names of drugs and possible cross-sensitivities to drugs, if relevant |
| How to recognize the signs and symptoms of mild, moderate and severe allergic reactions and how to act in each case |
| Medication prescribed and when it should be used |
| Management of emergencies: actions to be taken and medications to be used |
| Clear statement of the need to administer adrenaline without hesitation |
| When to call emergency services |
| Where medication is stored at home, in school, or workplace |
| Review dates for prescribed medication if appropriate, e.g. when child reaches 30 kg in weight, importance of checking expiry dates |
| Number of injectable adrenaline devices (e.g. Epipens) required |
| Who is trained to administer medication in home, school, workplace |
Discussion
Our study has highlighted the view that emergency and long-term anaphylaxis management plans should be stand-alone documents. The greatest consensus was around the components of an emergency anaphylaxis management plan, which participants indicated should be a simple, clear and brief, generic and easy to implement in a crisis situation. Responsibility for long-term management plans, particularly where specialist services are unavailable, was more controversial. Long-term anaphylaxis management plans need to be negotiated between patient/family and professionals and tailored to individual needs.
This study supports the view that long-term management of anaphylaxis is in the main inadequately addressed.2,24,25 Ideally, all patients with anaphylaxis should have a comprehensive assessment which covers issues relating to emergency management and discussion of ways of minimizing further reactions, with appropriate written information, access to expert advice and follow-up review and retraining if necessary.2,7,10,12,26 Our study suggests, however, that policy and practice in anaphylaxis management are fragmented, with much local variation in care provision.
Allergy patients are often managed by non-specialists, but clearly defined referral pathways to specialists for patients with severe disease are required. Specialists may in particular need to see children at key transition points, such as starting a new school (nursery, primary or secondary) or leaving home. More effective long-term anaphylaxis management requires education for non-specialists to enhance their skills and confidence. The lack of specialist services in many countries means that non-specialist healthcare and school staff have little access to such training and support from specialists, therefore establishing competencies in anaphylaxis management at all clinical levels is essential for effective long-term management and review for children and adults.27 The low numbers of patients with anaphylaxis means that experience of anaphylaxis management is hard to come by for generalist staff and integrated cross-sector working in allergy is uncommon. There appears to be a danger that no-one, in the absence of an allergy specialist clinic or a dedicated school nurse or a community-based practitioner with a special interest in allergy, takes responsibility for long-term management of anaphylaxis. This mirrors parents' experiences in previous studies.18,19,28
Professional consensus on the key aspects of anaphylaxis management does not necessarily coincide with the views of patients and families. The panel of experts did not identify psychosocial support, such as specific advice on managing social situations, as important, although parents have identified this as a major concern in risk management with adolescents.18,29 Support and advice to enable those affected by anaphylaxis to live a normal social and family life through effective risk management could potentially improve quality of life and reduce morbidity and mortality.10,30
Strengths and limitations
It is vital to ensure that any proposed intervention is acceptable to the academics and professionals in the areas in which evaluative studies are likely to be conducted and, furthermore, that any future change in clinical practice is relevant and acceptable to clinicians. The e-Delphi process was highly effective in engaging a diverse group of academics and professionals as evidenced by the very high response rates. This process enabled a structured, systematic approach to be taken to developing consensus from experts in the field and allowing all voices to be heard equally, thereby resulting in a clinically-relevant strategy for anaphylaxis management, while also recognizing divergent views. Despite assurances of confidentiality, however, some contributors may still have had doubts about whether or not others might have been able to identify them and this may have influenced their responses. Consensus between clinicians and patients/families also needs to be established before anaphylaxis management plans can be successfully implemented.
Implications for practice, policy and research
Consensus on the core components of emergency anaphylaxis management plans exists and the evidence base for their implementation is probably adequate to inform policy decisions, given the challenges inherent in conducting research in the context of a relatively uncommon, acute and short-lived emergency. The emergency component of anaphylaxis management plans should, therefore, be implemented nationally. There is less agreement, however, on aspects of long-term management and the evidence-base for the effectiveness of strategies to reduce risk and severity of recurrence requires further development. Tailored plans, individualized to the patient's age, underlying triggers and circumstances, are required, but currently not routinely used in practice and the agreed components of anaphylaxis management plans identified in this study should now be evaluated. Protocols for use in schools and workplaces and referral pathways should also be developed and will require robust evaluation of impact, including cost–benefit analysis, when they are implemented.
DECLARATIONS
Competing interests
None declared
Funding
Chief Scientist Office, Scottish Government Health Department
Ethical approval
Not applicable
Guarantor
AS
Contributorship
AS conceived the study; UN conducted the study, supervised by AW and AS; AW drafted the paper; AS and AW revised the paper; all authors have read successive drafts and approved the final paper
Acknowledgements
The research team is extremely grateful to members of the e-Delphi panel for their time and substantial contribution to the study. We are also grateful to David Reading, Director of the Anaphylaxis Campaign, for joining us in inviting participants to contribute to the e-Delphi study
Reviewer
M Hazel Gowland
References
- 1.Worth A, Soar J, Sheikh A Management of anaphylaxis in the emergency setting. Expert Rev Clin Immunol 2010;6:89–100 [DOI] [PubMed] [Google Scholar]
- 2.Simons FER Anaphylaxis, killer allergy: Long-term management in the community. J Allergy Clin Immunol 2006;117:367–77 [DOI] [PubMed] [Google Scholar]
- 3.Lieberman P, Camargo CA, Bohlke K, et al. Epidemiology of anaphylaxis: findings of the American College of Allergy, Asthma and Immunology Epidemiology of Anaphylaxis Working Group. Ann Allergy Asthma Immunol 2006;97:596–602 [DOI] [PubMed] [Google Scholar]
- 4.Simpson CR, Newton J, Hippisley-Cox J, Sheikh A Incidence and prevalence of multiple allergic disorders recorded in a national primary care database. J R Soc Med 2008;101:558–63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta R, Sheikh A, Strachan DP, Anderson HR Time trends in allergic disorders in the UK. Thorax 2007;62:91–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pumphrey R, Gowland H Further fatal allergic reactions to food in the United Kingdom, 1999–2006. J Allergy Clin Immunol 2007;119:1018–19 [DOI] [PubMed] [Google Scholar]
- 7.Bock SA, Munoz-Furlong A, Sampson HA Further fatalities caused by anaphylactic reactions to food, 2001–2006. J Allergy Clin Immunol 2007;119:1016–18 [DOI] [PubMed] [Google Scholar]
- 8.Simons FER, Sheikh A Evidence-based management of anaphylaxis. Allergy 2007;62:827–9 [DOI] [PubMed] [Google Scholar]
- 9.Simons FER, Frew AJ, Ansotegui IJ, et al. Risk assessment in anaphylaxis: current and future approaches. J Allergy Clin Immunol 2007;120(Suppl. 1):S2–24 [DOI] [PubMed] [Google Scholar]
- 10.Hourihane JO Community management of severe allergies must be integrated and comprehensive, and must consist of more than just epinephrine. Allergy 2001;56:1023–5 [DOI] [PubMed] [Google Scholar]
- 11.Ewan PW, Clark AT Efficacy of a management plan based on severity assessment in longitudinal and case-controlled studies of 747 children with nut allergy: proposal for good practice. Clin Exp Allergy 2005;35:751–6 [DOI] [PubMed] [Google Scholar]
- 12.Ewan PW, Clark AT Long-term prospective observational study of patients with peanut and nut allergy after participation in a management plan. Lancet 2001;357:111–15 [DOI] [PubMed] [Google Scholar]
- 13.Kapoor S, Roberts G, Bynoe Y, Gaughan M, Habibi P, Lack G Influence of a multidisciplinary paediatric allergy clinic on parental knowledge and rate of subsequent allergic reactions. Allergy 2004;59:185–91 [DOI] [PubMed] [Google Scholar]
- 14.Choo K, Sheikh A Action plans for the long-term management of anaphylaxis: systematic review of effectiveness. Clin Exp Allergy 2007;37:1090–4 [DOI] [PubMed] [Google Scholar]
- 15.Nurmatov U, Worth A, Sheikh A Anaphylaxis management plans for the acute and long term management of anaphylaxis: a systematic review J Allergy Clin Immunol 2008;122:353–61 [DOI] [PubMed] [Google Scholar]
- 16.Ewan PW, Durham SR NHS allergy services in the UK: proposals to improve allergy care. Clin Med 2002;2:122–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soar J, Pumphrey R, Cant A, et al. Emergency treatment of anaphylactic reactions-guidelines for healthcare providers. Resuscitation 2008;77:157–69 [DOI] [PubMed] [Google Scholar]
- 18.Akeson N, Worth A, Sheikh A The psychological impact of anaphylaxis on young people and their parents. Clin Exp Allergy 2007;37:1213–20 [DOI] [PubMed] [Google Scholar]
- 19.Primeau M-N, Kagan R, Joseph L, et al. The psychological burden of peanut allergy as perceived by adults with peanut allergy and the parents of peanut-allergic children. Clin Exp Allergy 2000;30:1135–43 [DOI] [PubMed] [Google Scholar]
- 20.Levy M, Sheikh A, Walker S, Woods A Should UK allergy services focus on primary care? BMJ 2006;332:1347–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hourihane JO, Beirne P Evidence of effectiveness of anaphylaxis management plans: are we waiting for godot? Clin Exp Allergy 2007;37:967–9 [DOI] [PubMed] [Google Scholar]
- 22.Jones J, Hunter D Qualitative research: Consensus methods for medical and health services research. BMJ 1995;311:376–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Avery AJ, Savelyich BSP, Sheikh A, et al. Identifying and establishing consensus on the most important safety features of GP computer systems: e-Delphi study. Inform Prim Care 2005;3:3–11 [DOI] [PubMed] [Google Scholar]
- 24.Department of Health A review of services for allergy – the epidemiology, demand for and provision of treatment and effectiveness of clinical interventions. London: DH Allergy Services Review Team, 2006 [Google Scholar]
- 25.House of Lords Science and Technology Committee Allergy. 6th report of session 2006–2007. London: The Stationery Office, 2007 [Google Scholar]
- 26.Vickers DW, Maynard L, Ewan PW Management of children with potential anaphylactic reactions in the community: a training package and proposal for good practice. Clin Exp Allergy 1997;27:898–903 [PubMed] [Google Scholar]
- 27.Kaliner MA, Del Giacco S, Crisci CD, et al. Requirements for physician training in allergy. Key clinical competencies appropriate for the care of patients with allergic or immunologic diseases – a provisional position statement of the World Allergy Organization. Allergy Clin Immunol Int – J World Allergy Org 2006;18:92–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sicherer SH, Noone SA, Munoz-Furlong A The impact of childhood food allergy on quality of life. Ann Allergy Asthma Immunol 2001;87:461–4 [DOI] [PubMed] [Google Scholar]
- 29.Sampson MA, Munoz-Furlong A, Sicherer SH Risk-taking and coping strategies of adolescents and young adults with food allergy. J Allergy Clin Immunol 2006;117:1440–5 [DOI] [PubMed] [Google Scholar]
- 30.Muraro A, Roberts G, Clark A, et al. The management of anaphylaxis in childhood: position paper of the European academy of allergology and clinical immunology. Allergy 2007;62:857–71 [DOI] [PubMed] [Google Scholar]