Abstract
If orthodontists and restorative dentists establish the interdisciplinary approach to esthetic dentistry, the esthetic and functional outcome of their combined efforts will be greatly enhanced. This article describes satisfying esthetic results obtained by the distribution of space for restoration by orthodontic treatment and porcelain laminate veneers in uneven space between maxillary anterior teeth. It is proposed that the use of orthodontic treatment for re-distribution of the space and the use of porcelain laminate veneers to alter crown anatomy provide maximum esthetic and functional correction for patients with irregular interdental spacing.
Keywords: Interdental spacing, Orthodontic treatment, Porcelain laminate veneers, Interdisciplinary approach
INTRODUCTION
Nowadays, there are many patients who want to restore their teeth more esthetically not only for the origin such as dental caries or tooth fracture but also for diastema. As the interests of patients in esthetics increased, a number of reports over the porcelain laminate veneer increased.1,2
Interdental spacing in the anterior region of the mouth presents a challenge for correction that has been traditionally difficult to resolve with conventional full-veneer crown treatment alternatives due to imbalanced tooth proportion. In such instances, an interdisciplinary approach, which is composed of orthodontics, periodontology and prosthodontics, is necessary to evaluate, diagnose, and resolve esthetic.3 When a comprehensive approach is necessary, communication among the disciplines is critical in achieving improved esthetic outcomes in the anterior maxilla. Uneven space between maxillary anterior teeth can be treated orthodontically. After the rearrangement of the teeth, the anterior maxillary esthetics can be restored with porcelain laminate veneers for minimal teeth preparations, which can preserve sound tooth structure and prevent pulp-irritation, with the least possible irritation of marginal gingiva around the restored teeth.4,5
This clinical report describes a patient with uneven interdental space between anterior maxillary teeth, improper clinical crown lengths, tooth size discrepancies, and malocclusion. The patient's esthetic demands were met through an interdisciplinary treatment approach consisting of orthodontic movement and porcelain laminate veneers.
CASE REPORT
A 50-year-old woman visited Seoul National University Dental Hospital, with a chief complaint of "desire to improve esthetics" because of the existing space between anterior maxillary teeth. The patient had uneven space between anterior maxillary teeth and showed deep bite Angle class II malocclusion. The problem list of patient's anterior maxillary part was as followed: asymmetrical zenith lines, abnormal incisal profile with disharmonious tooth axes and imbalances in tooth positions (Fig. 1). The midline was deviated and the maxilla was canted to the right. The proportion of tooth size was asymmetrical and there was wide diastema between central incisors, approximately 2 mm. On the first visit, irreversible hydrocolloid impressions of both maxillary and mandibular arches were taken, and diagnostic wax up was performed. To produce the most esthetic result, recurring esthetic dental (RED) proportion was used to establish the widths of the anterior six teeth as viewed from the frontal.6 The author has defined the RED proportion as the proportion of successive widths of the teeth viewed from the frontal, remaining constant as one moves distally. As it is well known, the golden proportion is limited to 62%, however, the RED proportion gives greater flexibility, as the dentist can define desired RED proportion, and an approximate 70% is preferred. Based on the RED proportion of 70%, diagnostic wax-up was performed, and the favorable results were predicted by space redistribution. If the right central incisor would be moved toward mesial and incisal directions 1 mm respectively, the left lateral incisor would be moved toward incisal direction 1 mm (Fig. 2).
Fig. 1.
Pretreatment intra-oral photograph. Look at the wide diastema between #11 and #21.
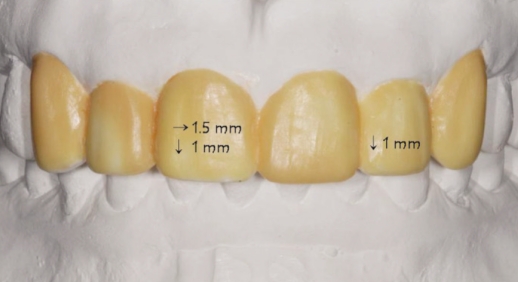
Fig. 2.
Diagnostic wax-up was performed on the supposition that #11 and #22 moved as mentioned.
Deciding as for the treatment option, the MBT brackets (3M Unitek, Monrovia, CA, USA) were bonded to the anterior maxillary teeth according to their related positions, and the brackets of the right central incisor and the left lateral incisor were bonded in slightly cervical positions for extrusion. Then open coil spring (3M Unitek, Monrovia, CA, USA) was inserted between the right central incisor and the right lateral incisor in order to move the right central incisor in mesial direction. On the other hand, closed coil springs (3M Unitek, Monrovia, CA, USA) were inserted between the right central incisor and the left central incisor and between the right lateral incisor and the right canine, with keeping in mind not to overclose of the diastema and not to take the wrong distal direction for the right lateral incisor. After the spring and wire were inserted, all of the brackets and 016 stainless-steel round wire (Jin-Sung Industrial Co., Seoul, Korea) were ligated tightly and activation of teeth movements had begun (Fig. 3). The recall checks were carried out with two weeks intervals. The careful observation of teeth movements was fulfilled and open coil spring had been changed, if necessary. The occlusal adjustment of extruded right central incisor and the palatal surface of the left lateral incisor was carried out to remove occlusal interferences. The minute examination was performed for evaluating favorable teeth movements 6 weeks after brackets bonding procedure. Because the teeth were in proper positions in the maxillary dentition, all brackets and wire were removed, and the teeth surfaces were cleaned and polished. The fixed retainer was bonded to avoid the relapse of the moved teeth.
Fig. 3.
The brackets were bonded as considered the teeth movements.
On the next visit, porcelain laminate preparation was performed with the silicone index (Exafine Putty Type; GC Corporation, Tokyo, Japan) attained from the diagnostic wax-up cast. Immediate dentin sealing (Adper Scotchbond Multi-purpose Adhesive; 3M ESPE, St. Paul, MN, USA) was carried out for achieving improved bond strength, fewer gap formations, decreasing bacterial leakage, and reducing dentin sensitivity (Fig. 4).7-9 The final impression was taken with polyvinyl siloxane impression material (Express; 3M ESPE, St. Paul, MN, USA) using 1-step technique. Shade was carefully decided considering the prepared teeth and opposite mandibular incisors with shade guide (VITA System 3D-Master; VITA Zahnfabrik, Säckingen, Germany). The provisional restorations (Luxatemp; DMG, Hamburg, Germany) were fabricated directly with premade silicone index (Exafine Putty Type; GC Corporation, Tokyo, Japan) attained from the diagnostic wax-up cast.
Fig. 4.
Porcelain laminate veneer preparation was done and immediate dentin sealing was performed.
After 2 weeks, the final restorations was completed and tried in the mouth, all margins, contacts were verified (Fig. 5). The final restorations were bonded using resin cement (Variolink II; Ivoclar vivadent, Schaan, Liechtenstein). After delivery, as shown in Fig. 5, the gingiva was healthy and showed harmonious shapes and contours. The proper esthetics was obtained that the shade of surrounding tissues was stable and shown balanced properties, the proportion of tooth size was favorable and satisfied. The retainer was bonded for maximum retention of new teeth positions. The following check-ups of the patient were performed for 3 months after placement of the definitive prosthesis, and oral hygiene was maintained in excellent state and tooth alignment was stable. The patient was very satisfied with the appearance and the function.
Fig. 5.
Frontal view of definitive porcelain laminate veneers.
CONCLUSION
This clinical report describes an interdisciplinary approach where communication and coordination were the key for an improved esthetic result in the anterior maxilla. Coordinated treatment with careful consideration of patient expectations and requests were critical for successful outcome and patient's satisfaction.
References
- 1.Banker CA, Berlocher WC, Mueller BH. Alternative methods for the management of persistent maxillary central diastema. Gen Dent. 1982;30:136–139. [PubMed] [Google Scholar]
- 2.Rakow B, Light EI, Condello P. Enamel bonded mechanically retained laminate veneer. Gen Dent. 1978;26:47–48. [PubMed] [Google Scholar]
- 3.Kokich VG, Spear FM. Guidelines for managing the orthodontic-restorative patient. Semin Orthod. 1997;3:3–20. doi: 10.1016/s1073-8746(97)80036-9. [DOI] [PubMed] [Google Scholar]
- 4.Claman L, Alfaro MA, Mercado A. An interdisciplinary approach for improved esthetic results in the anterior maxilla. J Prosthet Dent. 2003;89:1–5. doi: 10.1067/mpr.2003.5. [DOI] [PubMed] [Google Scholar]
- 5.Heymann HO, Hershey HG. Use of composite resin for restorative and orthodontic correction of anterior interdental spacing. J Prosthet Dent. 1985;53:766–771. doi: 10.1016/0022-3913(85)90153-2. [DOI] [PubMed] [Google Scholar]
- 6.Ward DH. Proportional smile design using the recurring esthetic dental (red) proportion. Dent Clin North Am. 2001;45:143–154. [PubMed] [Google Scholar]
- 7.Magne P. Immediate dentin sealing: a fundamental procedure for indirect bonded restorations. J Esthet Restor Dent. 2005;17:144–154. doi: 10.1111/j.1708-8240.2005.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 8.Magne P, Kim TH, Cascione D, Donovan TE. Immediate dentin sealing improves bond strength of indirect restorations. J Prosthet Dent. 2005;94:511–519. doi: 10.1016/j.prosdent.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Magne P, So WS, Cascione D. Immediate dentin sealing supports delayed restoration placement. J Prosthet Dent. 2007;98:166–174. doi: 10.1016/S0022-3913(07)60052-3. [DOI] [PubMed] [Google Scholar]