Abstract
The nosology of major psychoses is challenged by the findings that schizophrenia (SZ) and bipolar disorder (BP) share several neurobiological, neuropsychological and clinical phenotypic characteristics. Moreover, several vulnerability loci or genes may be common to the two DSM disorders. We previously reported, in a sample of 21 kindreds (sample 1), a genome-wide suggestive linkage in 13q13–q14 with a common locus (CL) phenotype that crossed the diagnostic boundaries by combining SZ, BP and schizoaffective disorders. Our objectives were to test phenotype specificity in a separate sample (sample 2) of 27 kindreds from Eastern Quebec and to also analyze the combined sample of 48 kindreds (1274 family members). We performed nonparametric and parametric analyses and tested as phenotypes: SZ alone, BP alone, and a CL phenotype. We replicated in sample 2 our initial finding with CL with a maximum NPLpair score of 3.36 at D13S1272 (44 Mb), only 2.1 Mb telomeric to our previous maximum result. In the combined sample, the peak with CL was at marker D13S1297 (42.1 Mb) with a NPLpair score reaching 5.21, exceeding that obtained in each sample and indicating consistency across the two samples. Our data suggest a susceptibility locus in 13q13–q14 that is shared by schizophrenia and mood disorder. That locus would be additional to another well documented and more distal 13q locus where the G72/G30 gene is mapped.
Keywords: schizophrenia, bipolar disorder, genetic linkage, 13q, G72/G30, genome scan
Introduction
In the last decade, converging genetic linkage results for schizophrenia (SZ) and bipolar disorder (BP) have accumulated despite the complexities of the two disorders. Although family studies suggest little co-aggregation of SZ and BP,1 an observable trend is that many of the genetic vulnerability loci may be shared by SZ and BP, which challenges the traditional Kraepelinian dichotomy and current nosology.2, 3, 4, 5, 6, 7, 8 This trend is congruent with the observations that BP and SZ share early in life,9, 10 and later on,11, 12 several phenotypic features encompassing the neurobiological, neuropsychological and clinical domains.
Seemingly in contrast with the evidence of genetic influences crossing the SZ and BP DSM boundaries, a second emerging pattern of findings suggests distinct subgroups within the SZ or within the BP diagnosis, such as the negative symptoms and of SZ found associated with a 6p locus,13, 14 or the psychotic BP subtype with a 16p locus or 13q21–q33.15, 16, 17 Research may have to reconcile these apparently contrasting bodies of data, one toward commonality and the other toward specificity.
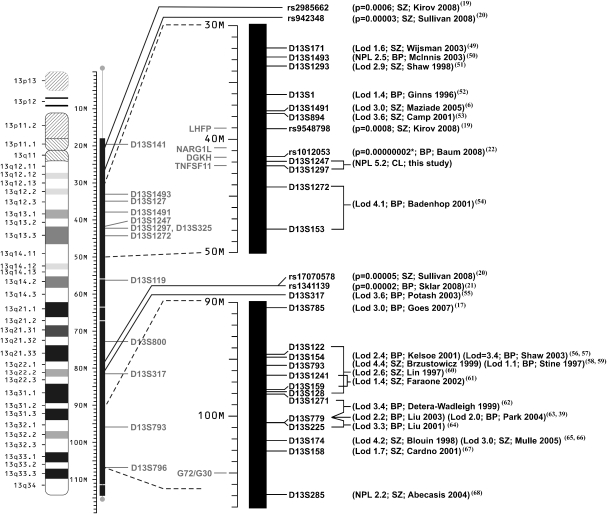
We have already reported genome-wide significant linkage findings pertaining to both SZ and BP6 and the commonality of some of these loci has been replicated in other populations such as in 15q26.18 Chromosome 13q is a good candidate for possible commonalities. First, as shown in Figure 1, 11 linkage and two genome-wide association studies (GWA) provided linkage and association signals for SZ19, 20 on this chromosome, and 12 linkage and two GWA studies for BP.21, 22 One meta-analysis3 confirmed linkage for SZ although another did not.23 Concerning BP, one meta-analysis confirmed linkage in 13q3 but two others did not.24, 25 Studying concurrently SZ and BP kindreds12, 26 permits to test directly for loci shared by the two disorders and we formerly reported a genome-wide suggestive linkage in 13q13–q14 for both SZ and BP.6 Second, the sites of maximum linkage from the different studies span more than 70 Mb on 13q, raising the possibility that 13q may contain more than one susceptibility gene, such as one in 13q13–q14 and another in 13q21–q33. Third, a meta-analysis of 10 association studies (seven in SZ, two in BP, one in both) of the G72-DAOA/G30 complex, mapped telomeric on 13q33, yielded a significant association of G72/G30 with SZ and a suggestive evidence for BP.27 Fourth, the NIMH BP Collaborative cohort provided a lod score of 2.99 with BP having mood-incongruent symptoms in a long region from 50 to 100 Mb on 13q21–q33, a zone also including the G72/G30 gene complex.17
Figure 1.
Linkage and genome-wide association findings in chromosome 13q for schizophrenia (SZ) and bipolar disorder (BP). Linkage and genome-wide association results from different studies are in dark black at the right. The markers analyzed in both samples and candidate genes are indicated in light gray at the left. Lod: parametric lod score; NPL: nonparametric lod score; NARG1L: NMDA receptor regulated 1-like; TNFSF11: tumor necrosis factor (ligand) superfamily, member 11; DGKH: diacylglycerol kinase, eta; LHFP: lipoma HMGIC fusion partner; G72/G30: -amino acid oxidase activator (DAOA).
Therefore, further genetic studies of chromosome 13q are warranted to elucidate the exact location of a single susceptibility locus that could be shared by the two major psychoses, or the presence of two loci that could be specific to each. In the current study, we took advantage of investigating both disorders within a single study using homogeneous diagnostic, statistical and genotyping methods, which, to our knowledge, has rarely been attempted.
Following our results in 13q in a first kindred sample,6 we recruited a second sample of kindreds from the same population to seek replication and also to use the increased statistical power of the combined kindred samples to test for the phenotypic specificity of linkage. The objectives were (i) to replicate our 13q13–q14 suggestive linkage with a primary attention to our common locus (CL) phenotype, (ii) to look at the results in the combined sample, (iii) to assess whether linkage would cross the boundaries between SZ and BP.
Methods
Sample
Our first sample of 21 kindreds (sample 1) comprised 643 family members of whom 480 provided DNA sample and is described in Maziade et al. 2005.6 We collected a second sample (sample 2) from Eastern Quebec that consisted of 27 other multigenerational families of which 15 were mainly affected by BP (<15% of the affected family members had SZ), eight mainly affected by an SZ spectrum disorder (<15% had BP) and four were mixed pedigrees, that is, affected almost equally by SZ and BP. Sample 2 included 631 family members; 490 provided DNA samples and 210 were affected with a BP or an SZ spectrum disorder. The combined sample included 48 kindreds (15 SZ, 21 BP and 12 mixed kindreds) comprising 1274 family members of whom 970 provided DNA sample. The study was explained to each family member and the signed consent was reviewed by our University Ethics Committee.
Phenotype definition
A best-estimate lifetime DSM-IV diagnosis was made in sample 2 with the same stringent procedure outlined in previous reports.12, 26, 28.In brief, all available information across lifetime from different sources (all medical records, family informant interviews, personal structured interview) was reviewed blindly by four research diagnosticians. The board of diagnosticians also specified the presence or absence of psychotic features in BP patients according to DSM-IV. To test our hypothesis, we defined a narrow and broad ‘common locus' (CL) phenotype. The narrow CL phenotype included BP narrow (see later), SZ narrow and schizoaffective disorder (SAD). The broad CL definition included the broad definitions of BP and SZ, in addition to SAD. Our SZ narrow definition was restricted to SZ and the broad definition included SZ narrow plus schizophreniform disorder and schizotypal personality. The BP narrow phenotype was restricted to BP I and the broad definition included BP I, BP II, and recurrent major depression. Table 1 provides the number of affected subjects for each phenotype definition.
Table 1. Number of affected subjects for each phenotype definition.
| Phenotypes | ||||||
|---|---|---|---|---|---|---|
| CL | SZ | BP | ||||
| Narrow | Broad | Narrow | Broad | Narrow | Broad | |
| Sample 1 | 133 | 168 | 71 | 81 | 48 | 72 |
| Sample 2 | 148 | 210 | 54 | 55 | 72 | 133 |
| Combined | 281 | 378 | 125 | 136 | 120 | 205 |
Abbreviations: SZ, schizophrenia; BP, bipolar; CL refers to the ‘common locus' phenotype as defined in the Methods section. As regards the secondary analysis with a BP-Psychotic narrow definition, 32 and 49 subjects were found affected in samples 1 and 2, respectively. The BP-Psychotic broad definition included 40 and 59 subjects in samples 1 and 2, respectively. These subjects were added to the SZ and SAD subjects to create a new CL (BP-psychotic) narrow and broad definition including 117 and 125 affected subjects in samples 1 and 2, respectively.
As a secondary analysis, to test sub-phenotypes previously found associated with 13q (see Goes et al.17), we defined a phenotype restricted to the BP subjects presenting psychotic symptoms without discriminating mood-congruent or mood-incongruent symptoms, as we did not have this distinction available.
Genotyping
From whole-blood cell or cultured immortalized lymphocytes, we extracted DNA using an affinity column (Blood and cell culture DNA maxi kit; Qiagen). The location of markers in megabases (Mb) was defined according to NCBI human genome resource maps (Human Genome Build 36.3; http://www.ncbi.nlm.nih.gov/). We genotyped, in sample 2, the same set of 13 microsatellite markers originally genotyped in sample 1. These markers are detailed in Figure 2. A semi-automated high-throughput genotyping procedure using laser infrared automatic DNA sequencers (Li-Cor, Lincoln, NE, USA) was used. PCR primers were synthesized (Alpha DNA, Montreal, Canada) after adding an M13 tail to the forward primer. Microsatellite genotypes were called automatically using the software SAGA (LICOR). After automatic genotyping, which was read blind to the phenotypes, manual editing of the results was performed if needed. Mendelian inheritance was checked using the computer software PedCheck.29 Subjects who failed the Mendelian test were reanalyzed completely, that is, from the PCR to the genotyping. When Mendelian errors persisted, these genotypes were discarded. Missing genotypes plus those discarded reached less than 1% of the total sample for all markers. Some 10% of blind replicates were also included randomly among the DNAs for genotyping quality control: the replication rate was 95%.
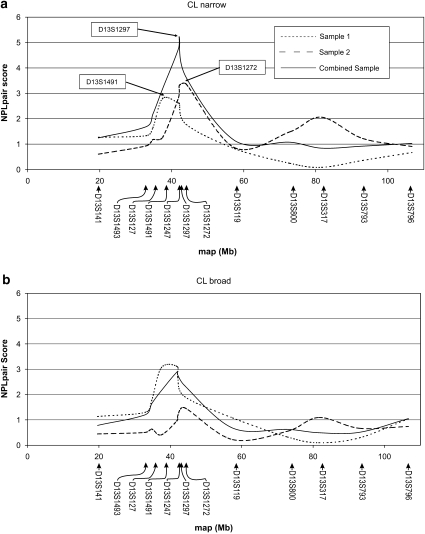
Figure 2.
NPLpair scores for the Common Locus (CL) phenotype on chromosome 13q from the nonparametric analyses using the Mega2 program with the Merlin/SimWalk2-NPL option. The value reported on the y axis is the NPLpair score corresponding to −log10(P), where P is the P-value based on 700 000 unconditional simulations (25). Markers identified in boxes are those at which linkage peaks were observed for each of the samples (Sample 1, Sample 2 and the Combined Sample). All the markers analyzed are indicated along the x axis, which uses an Mb scale. Marker D13S325 could not be analyzed with the Simwalk2 program because of the small distance between D13S325 and D13S1297 (less than 0.1 cM;31). All 48 families of our total sample were found informative (ie, containing at least two affected subjects) for linkage under the CL phenotype definitions and the number of affected subjects per family ranged from 2 to 17 and 2 to 26 for the narrow and broad definitions, respectively.
Statistical analysis
We performed nonparametric (or model-free) linkage analyses, which do not require specifying a mode of inheritance for the disease nor genetic parameters such as the disease allele frequency and penetrances. Nonparametric analysis consists of quantifying the extent of identity by descent allele sharing among family members and testing if it exceeds the expectation under the null hypothesis of no linkage between the disorder and the locus under analysis. NPLpairs and NPLall are two commonly used nonparametric linkage (NPL) statistics. The NPLpairs statistics is roughly the sum of conditional kinship coefficients for all affected pairs, whereas the NPLall statistics is a measure of whether a few founder alleles are overly represented in all affected subjects. Both NPL statistics are implemented in the Merlin30 (Multipoint Engine for Rapid Likelihood Inference) and SimWalk231 packages, the latter being optimized to be able to estimate multipoint scores in large pedigrees by employing a Markov Chain Monte Carlo (MCMC) algorithm.
We used the Mega2 program32 (Manipulation Environment for Genetic Analyses) with the Merlin/SimWalk2-NPL option. This permits to combine the exact NPL statistics calculated by Merlin in the smaller pedigrees with the statistics approximated by Simwalk2 on large pedigrees, to produce an overall NPL statistics. We herein report NPL scores defined as the −log10(P) of this NPL statistic, where P is the P-value.
Even with its efficient MCMC estimation algorithm, the analysis with SimWalk2 of a few of our extended pedigrees (involving more than 20 affected subjects) turned out to consume excessive time if analyzed with the entire set of 13 markers on chromosome 13. So we created two ‘windows' of 8 and 7 markers, respectively, with two overlapping markers.
Parametric (or model-based) linkage analyses were also performed using both a dominant and a recessive mode of inheritance with the age-dependent penetrance values used in sample 1.6 The exact parameter values were provided in Maziade et al. 2002.33 Both models took into account the uncertainty of diagnosis by increasing the phenocopy rate in liability classes corresponding to ‘probable' or ‘possible' diagnoses (see Ott34). For each mode of inheritance, the analysis was first carried out with affected and unaffected subjects and then repeated by considering only the affected family members to allow for the presence of a few disease gene carriers who had not yet expressed the disorder (referred to as the ‘affected-only' affection-status type). Hence, for each phenotype definition, four models were tested resulting from the combination of the two modes of inheritance and affection-status types. Multipoint parametric lod scores were calculated using the FASTLINK version35 of the LINKAGE programs.36 Given the large size of our pedigrees, four-point analyses were performed (one disease gene plus three markers), each marker being analyzed with its telomeric and centromeric adjacent markers.
Statistical thresholds
We reported the results separately for sample 1 and sample 2, and also in the combined sample merging samples 1 and 2, in which we optimally expected an increase in linkage evidence. This allowed us to evaluate the contribution of each sample to the linkage evidence provided by the combined sample. We referred to the conventional criterion of a P-value of 0.01 for claiming a replication in sample 2.37 This corresponds to a NPL value of 2.0 [ie, –log10 (.01)] and to a parametric lod score of approximately 1.18, which represents a likelihood ratio of 15.0 leading to a one-sided χ2 statistics of 5.42=2 ln (15.0)=χ21,0.99. Given that two and four analyses were performed for the nonparametric (NPLpairs and NPLall) and parametric analysis, respectively, the conventional criterion (P-value of 0.01) was divided by the number of analyses to adjust for multiple testing. For nonparametric analyses, this raised the threshold for replication to a NPL of 2.30 [ie, –log10 (.005)]. For the parametric threshold, this raised the lod score to 1.71, that is, a likelihood ratio of 51.4 leading to a one-sided χ2 statistics of 7.88=χ21,0.9975.
Results
The most significant results from the nonparametric analysis (Merlin-SimWalk2 analysis) are presented in Table 2 and illustrated in Figure 2. We clearly reproduced our initial finding, as indicated by the maximum NPLpair score with CL narrow in sample 2, of 3.36 (Table 2, Figure 2a) at D13S1272 (44.0 Mb), a marker only 2.1 Mb distal to marker D13S1247, which had formerly provided a genome-wide suggestive signal in sample 1.6 Marker D13S1247 yielded a NPLpair score of 2.62 in sample 1 and again an evidence for replication in sample 2 with an NPLpair score of 2.83. In the combined sample, the peak was at marker D13S1297 (42.1 Mb) with an NPLpair score reaching 5.21. Moreover, this score exceeded the NPL score obtained in the individual samples (NPLpair=2.80 in sample 1 at D13S1491, 37.5 Mb; NPLpair=3.36 in sample 2, as mentioned above) thus increasing the overall linkage signal and indicating a level of consistency across the two samples. Overall, four markers spanning 6.5 Mb showed NPLpair scores over three in the combined sample (Table 2). When we used a 1-point drop in NPL score to define the boundaries of the support region,34 we obtained a region of about 3 Mb between 40.3 Mb and 43.3 Mb.
Table 2. NPLpair scores above 1.5 in the combined sample (48 families) and the corresponding scores in each individual sample (Samples 1 and 2) for the CL narrow, SZ broad and BP narrow phenotype definitions.
| NPLpair scores | |||||
|---|---|---|---|---|---|
| Sample | |||||
| Phenotype | Marker | Map (Mb) | 1 | 2 | Combined |
| CL narrow | |||||
| D13S1493 | 32.91 | 1.33 | 0.93 | 1.69 | |
| D13S127 | 34.76 | 1.64 | 1.18 | 2.18 | |
| D13S1491 | 37.46 | 2.80 | 1.27 | 3.18 | |
| D13S1247 | 41.86 | 2.62 | 2.83 | 4.76 | |
| D13S1297 | 42.09 | 2.61 | 3.31 | 5.21 | |
| D13S1272 | 43.98 | 1.78 | 3.36 | 3.63 | |
| SZ broad | |||||
| D13S1491 | 37.46 | 2.50 | 0.82 | 2.62 | |
| D13S1247 | 41.86 | 2.14 | 2.07 | 3.46 | |
| D13S1297 | 42.09 | 1.53 | 2.53 | 2.98 | |
| D13S1272 | 43.98 | 1.96 | 1.67 | 2.93 | |
| D13S119 | 57.45 | 1.36 | 0.83 | 1.61 | |
| BP narrow | |||||
| D13S1491 | 37.46 | 1.35 | 1.05 | 1.74 | |
| D13S1247 | 41.86 | 0.89 | 1.48 | 1.74 | |
| D13S1297 | 42.09 | 2.14 | 1.23 | 2.53 | |
| D13S1272 | 43.98 | 1.41 | 2.23 | 2.19 | |
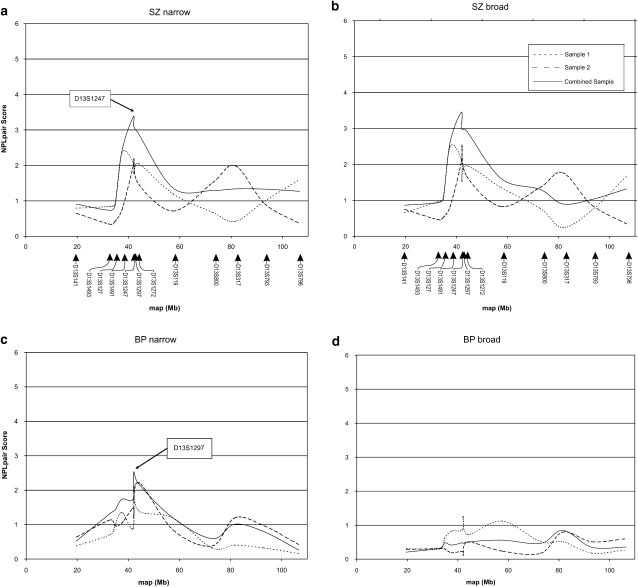
The broad CL phenotype (Figure 2b) provided weaker results than narrow CL. The SZ and the BP narrow phenotypes (Figures 3a and c) provided NPLpair scores above 2.5 in the combined sample, suggesting that the results with the CL phenotypes described above truly reflect the contribution of both disorders. The results obtained with the NPLall analysis also reached the replication criterion: the maximum NPLall score was 2.47 in sample 2 and 3.09 in the combined sample.
Figure 3.
NPLpair scores for the SZ and BP phenotypes on chromosome 13q from the nonparametric analyses using the Mega2 program with the Merlin/SimWalk2-NPL option. The value reported on the y axis is the NPLpair score corresponding to −log10(P), where P is the P-value based on 700 000 unconditional simulations (25). Markers identified in boxes are those at which linkage peaks were observed in the combined samples. Marker D13S325 could not be analyzed with the Simwalk2 program because of the small distance between D13S325 and D13S1297 (less than 0.1 cM;31). The same map scale in Mb is used in all the sub-figures and the location of the markers is indicated for the SZ figures (a and b). For the SZ narrow and SZ broad phenotypes, the number of informative families was, respectively, 33 and 35 and the number of affected subjects per family ranged from 2 to 11 for both phenotypes. For the (c) BP narrow and the (d) BP broad phenotypes, the number of informative families was, respectively, 26 and 28 and the number of affected subjects per pedigree ranged, respectively, from 2 to 14 and from 2 to 25.
As a follow-up analysis, we tested a secondary phenotype that was closer to that used in the NIMH cohort, along their hypothesis that BP with mood-incongruent psychosis might be underlain by genes shared by SZ and BP. We thus excluded BP without psychosis and analyzed a phenotype combining the SZ+SAD+BP with psychosis. This did not provide a better linkage signal as the maximum NPLpair obtained in the combined sample at the same locus (D13S1297) was only 2.7, a lower value than that obtained before excluding BP without psychosis (not shown in the figures).
The parametric analysis yielded results that were congruent with the nonparametric ones. In summary, a four-point maximum lod score (Zmax) of 3.09 was obtained in sample 2 with CL narrow (D13S1247-0.059-D13S325-0.029-D13S1297-0.150-CL), thus exceeding our replication criterion of 1.71. In the combined sample, the CL phenotype yielded a four-point lod score of 3.12 (D13S1247-0.059-D13S325-0.029-D13S1297-0.200-CL). Both results were obtained with the recessive model and affected-only affection status. Although the initial finding in sample 1 was also obtained under the affected-only analysis, the maximum had been observed with a dominant mode of inheritance. Hence, given that the two samples differed in their transmission model, misspecification probably explains the observed stronger nonparametric results.
Discussion
We had formerly reported a genome-wide suggestive linkage in 13q13–q14 with our CL phenotype, combining SZ+BP+SAD, in an initial sample of 21 kindreds. 6 We now report that our CL phenotype was amenable to replication in a separate sample of 27 kindreds. The present findings of an NPL of 5.21 clearly suggest that 13q13–q14, near the D13S1247–D13S1297 locus, contains one or several genes underlying both mood disorders and schizophrenia. Such level of evidence has rarely been reported for a complex disorder and the enhancement of the linkage signal provided by pooling samples 1 and 2 is also unprecedented, as discussed in Mérette et al.15 Our findings also suggest that extended families remain a powerful tool for identifying chromosomal regions harboring susceptibility loci for complex disorders. Moreover, our study design, which consisted of ascertaining a second sample of extended kindreds within the same population and assessed with similar procedures has proved to be a successful and powerful strategy for replicating previous findings.
Our data in 13q13–q14 are compatible with two possibilities: (i) there might be at that locus one gene shared by SZ and BP, that imputes susceptibility to either SZ or BP according, for instance, to a pleiotropic mechanism, or (ii) two genes that is, one for SZ and one for BP. The present susceptibility locus on 13q13–q14 is unlikely to be the G72/G30 gene complex mapped about 60 Mb distally on 13q21.33.27 This is congruent with Detera-Wadleigh et al.'s review27 of 25 linkage studies of SZ or BP indicating two potential zones of maximal linkage in 13q for either disorder: one on 13q13–q14 (≈40 Mb) and another on 13q21–q33 (≈95 Mb). Over 45 genes of interest lie within 2 Mb of our peak region at D13S1247 and D13S1297, among them the TNFSF11 and NARGIL genes. But most relevant is the report of a recent GWA study of BP22 yielding its strongest and genome-wide significant result with an SNP in the gene DGKH mapped exactly within the present support linkage region (Figure 1). DGKH encodes a key protein in the lithium-sensitive phosphatidyl inositol pathway. Besides, it is also noteworthy that the suggestive linkage signal obtained in 13q21–q33 in sample 2 (Figure 2) may sustain the presence of another locus in that region.
Our data raise the question as to the exact phenotype linked to 13q13–q14. Given that our CL phenotype offered the best fit with the genotype, this suggested that a single CL gene in 13q13–q14 imputes susceptibility to SZ or BP according to, for instance, a pleiotropic mechanism. Nevertheless, it remains possible that two genes lie within 13q13–q14, one for SZ and one for BP. Also, Goes et al. 200717 had a linkage signal with D13S785 located more telomeric at 92 Mb, with a 2-LOD support interval spanning 46 Mb, using BP with mood-incongruent psychotic symptoms. When BP without psychosis was included, the linkage signal disappeared, which led Goes et al.17 to the interpretation of a ‘psychosis gene'. By contrast, when we excluded BP without psychosis, our linkage signal decreased although the NPL remained at 2.7, which does not exactly support Goes et al.'s17 formulation. At least two explanations may be offered for this difference in results: (i) we did not distinguish mood-congruent and mood-incongruent symptoms in our sample, whereas Goes et al.17 used mood-incongruent psychosis only; and (ii) Goes et al.'s17 findings may pertain to a different susceptibility locus located more telomeric around 13q33 where the G72 (DAOA)/G30 gene is mapped.
The nature of our findings supports the presence of a gene in 13q13–q14 that underlies schizophrenia, mood disorder with and without psychosis. Hence, three patterns of evidence seem to emerge from our studies and from others, which may help to guide the genetic dissection of major psychiatric disorders. A first group of genes would be specific to subsets of SZ13, 14, 38 or BP15, 39, 40, 41 patients. A second group of genes, among them the G72/G30 gene,27 may be related to psychosis either present in the BP or the SZ categories. A third group of genes (eg, the present 13q13–q14 locus or the 15q26 locus18) would overlap mood disorders (with and without psychosis) and schizophrenia. These three patterns could help integrate the concepts of commonality with that of heterogeneity in the two DSM disorders and then help deciphering distinct homogeneous subforms within the current nosological entities.
Our data also call for further study of the exact endophenotype, pertaining to both SZ and BP that would underlie the present linkage on 13q13–q14 and increase our genetic understanding of the disease.42, 43 In that respect, in five SZ kindreds of Celtic origin that were affected with language impairment or dyslexia, Bartlett et al.44 observed a parametric multipoint lod score of 3.92 with that cognitive impairment in a region of 13q that may overlap the present findings. As neurocognitive impairments have been shown to be shared by patients with SZ or BP,45 and their unaffected relatives,46, 47 cognitive intermediate phenotypes might help to investigate further the mechanisms involved in chromosome 13q.42 Also, the concurrent investigation of SZ and BP within the same study may bring advantages to modeling the disease, having in mind the probable joint implications of several susceptibility genes and of epigenetic effects involving environmental factors the nature and timing of which may contribute to explain commonalities as well as specificities in mechanisms underlying psychiatric disorders.10, 48
Acknowledgments
We are grateful to our professional research assistants: Louise Bélanger, Linda René, Lisette Gagnon, Claudie Poirier, Nicole Leclerc, Julie Lamarche, Pierrette Boutin, David Demers, Lise St-Germain, Anne-Marie Simard and to the family members, adults and children, who participated in this study. We also thank IREP for their collaboration regarding the BALSAC database. This research was supported in part by a group Grant (no. MGC-14501) from the Canadian Institutes of Health Research (CIHR) and another individual CIHR Grant (no. MT-12854), and also by a Canada Research Chair (no. 950-200810) in the genetics of neuropsychiatric disorders of which Maziade is the Chair. Bureau is supported by a fellowship from the Fonds de la recherche en santé du Québec (FRSQ).
References
- Kendler KS, Gardner CO. The risk for psychiatric disorders in relatives of schizophrenic and control probands: a comparison of three independent studies. Psychol Med. 1997;27:411–419. doi: 10.1017/s003329179600445x. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Carpenter WT., Jr Diagnosis and classification of schizophrenia. Schizophr Bull. 1993;19:199–214. doi: 10.1093/schbul/19.2.199. [DOI] [PubMed] [Google Scholar]
- Badner JA, Gershon ES. Meta-analysis of whole-genome linkage scans of bipolar disorder and schizophrenia. Mol Psychiatry. 2002;7:405–411. doi: 10.1038/sj.mp.4001012. [DOI] [PubMed] [Google Scholar]
- Berrettini W. Evidence for shared susceptibility in bipolar disorder and schizophrenia. Am J Med Genet (Seminars in Medical Genetics) 2003;123C:59–64. doi: 10.1002/ajmg.c.20014. [DOI] [PubMed] [Google Scholar]
- Craddock N, O′Donovan MC, Owen MJ. Genes for schizophrenia and bipolar disorder? Implications for psychiatric nosology. Schizophr Bull. 2006;32:9–16. doi: 10.1093/schbul/sbj033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziade M, Roy M-A, Chagnon Y, et al. Shared and specific susceptibility loci for schizophrenia and bipolar disorder: a dense genome scan in Eastern Quebec families. Mol Psychiatry. 2005;10:486–499. doi: 10.1038/sj.mp.4001594. [DOI] [PubMed] [Google Scholar]
- Carpenter WT. Deconstructing and reconstructing illness syndromes associated with psychosis. World Psychiatry. 2007;6:92–93. [PMC free article] [PubMed] [Google Scholar]
- Owen MJ, Craddock N, Jablensky A. The genetic deconstruction of psychosis. Schizophr Bull. 2007;33:905–911. doi: 10.1093/schbul/sbm053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziade M, Gingras N, Rouleau N, et al. Clinical Diagnoses in Offspring from Eastern Québec Multigenerational Families Densely Affected by Schizophrenia or Bipolar Disorder. Acta Psychiatrica Scandinavica. 2008;117:118–126. doi: 10.1111/j.1600-0447.2007.01125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray RM, Sham P, Van Os J, Zanelli J, Cannon M, McDonald C. A developmental model for similarities and dissimilarities between schizophrenia and bipolar disorder. Schizophrenia Res. 2004;71:405–416. doi: 10.1016/j.schres.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Maier W, Zobel A, Wagner M. Schizophrenia and bipolar disorder: Differences and overlaps. Curr opin psychiatry. 2006;19:165–170. doi: 10.1097/01.yco.0000214342.52249.82. [DOI] [PubMed] [Google Scholar]
- Maziade M, Roy M-A, Martinez M, et al. Negative, psychoticism, and the disorganized dimensions in patients with familial schizophrenia or bipolar disorder: Continuity and discontinuity between the major psychoses. Am J Psychiatry. 1995;152:1458–1463. doi: 10.1176/ajp.152.10.1458. [DOI] [PubMed] [Google Scholar]
- Hallmayer JF, Kalaydjieva L, Badcock J, et al. Genetic evidence for a distinct subtype of schizophrenia characterized by pervasive cognitive deficit. Am J Hum Genet. 2005;77:468–476. doi: 10.1086/432816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanous AH, Van der Oord EJ, Riley BP, et al. Relationship between a high-risk haplotype in the DTNBP1 (Dysbidin) gene and clinical features of schizophrenia. Am J Psychiatry. 2005;162:1824–1832. doi: 10.1176/appi.ajp.162.10.1824. [DOI] [PubMed] [Google Scholar]
- Merette C, Roy MA, Bureau A, et al. Replication of linkage with bipolar disorder on chromosome 16p in the Eastern Quebec population. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:737–744. doi: 10.1002/ajmg.b.30673. [DOI] [PubMed] [Google Scholar]
- Schulze TG, Ohlraun S, Czerski PM, et al. Genotype-phenotype studies in bipolar disorder showing association between the DAOA/G30 locus and persecutory delusions: a first step toward a molecular genetic classification of psychiatric phenotypes. Am J Psychiatry. 2005;162:2101–2108. doi: 10.1176/appi.ajp.162.11.2101. [DOI] [PubMed] [Google Scholar]
- Goes FS, Zandi PP, Kuangyi M, et al. Mood-incongruent psychotic features in bipolar disorder: familial aggregation and suggestive linkage to 2p11-q14 and 13q21-33. Am J Psychiatry. 2007;164:236–247. doi: 10.1176/ajp.2007.164.2.236. [DOI] [PubMed] [Google Scholar]
- Vazza G, Bertolin C, Scudellaro E, et al. Genome-wide scan supports the existence of a susceptibility locus for schizophrenia and bipolar disorder on chromosome 15q26. Mol Psychiatry. 2007;12:87–93. doi: 10.1038/sj.mp.4001895. [DOI] [PubMed] [Google Scholar]
- Kirov G, Zaharieva I, Georgieva L, et al. A genome-wide association study in 574 schizophrenia trios using DNA pooling Mol Psychiatry 2008. available online 11 March 2008 [e-pub ahead of print]. [DOI] [PubMed]
- Sullivan PF, Lin D, Tzeng JY, et al. Genomewide association for schizophrenia in the CATIE study: results of stage 1. Mol Psychiatry. 2008;13:570–584. doi: 10.1038/mp.2008.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sklar P, Smoller JW, Fan J, et al. Whole-genome association study of bipolar disorder. Mol Psychiatry. 2008;13:558–569. doi: 10.1038/sj.mp.4002151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum AE, Akula N, Cabanero M, et al. A genome-wide association study implicates diacylglycerol kinase eta (DGKH) and several other genes in the etiology of bipolar disorder. Mol Psychiatry. 2008;13:197–207. doi: 10.1038/sj.mp.4002012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis CM, Levinson DF, Wise LH, et al. Genome scan meta-analysis of schizophrenia and bipolar disorder, Part II: Schizophrenia. Am J Hum Genet. 2003;73:34–48. doi: 10.1086/376549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQueen MB, Devlin B, Faraone SV, et al. Combined analysis from eleven linkage studies of bipolar disorder provides strong evidence of susceptibility loci on chromosomes 6q and 8q. Am J Hum Genet. 2005;77:582–595. doi: 10.1086/491603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segurado R, Detera-Wadleigh SD, Levinson DF, et al. Genome scan meta-analysis of schizophrenia and bipolar disorder, Part III: Bipolar disorder. Am J Hum Genet. 2003;73:49–62. doi: 10.1086/376547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziade M, Roy MA, Fournier J-P, et al. Reliability of best-estimate diagnosis in genetic linkage studies of major psychoses: Results from the Québec pedigree studies. Am J Psychiatry. 1992;149:1674–1686. doi: 10.1176/ajp.149.12.1674. [DOI] [PubMed] [Google Scholar]
- Detera-Wadleigh S, McMahon FJ. G72/G30 in schizophrenia and bipolar disorder: review and meta-analysis. Biol Psychiatry. 2006;60:106–114. doi: 10.1016/j.biopsych.2006.01.019. [DOI] [PubMed] [Google Scholar]
- Roy M-A, Lanctôt G, Mérette C, et al. Clinical and methodological factors related to reliability of the best-estimate diagnostic procedure. Am J Psychiatry. 1997;154:1726–1733. doi: 10.1176/ajp.154.12.1726. [DOI] [PubMed] [Google Scholar]
- O'Connell JR, Weeks DE. PedCheck: A Program for Identification of Genotype Incompatibilities in Linkage Analysis. Am J Hum Genet. 1998;63:259–266. doi: 10.1086/301904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abecasis GR, Cherny SS, Cookson WO, Cardon LR. Merlin—rapid analysis of dense genetic maps using sparse gene flow trees. Nat Genet. 2002;30:97–101. doi: 10.1038/ng786. [DOI] [PubMed] [Google Scholar]
- Sobel E, Sengul H, Weeks DE. Multipoint estimation of identity-by-descent probabilities at arbitrary positions among marker loci on general pedigrees. Hum Hered. 2001;52:121–131. doi: 10.1159/000053366. [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay N, Almasy L, Schroeder M, Mulvihill WP, Weeks DE. Mega2: data-handling for facilitating genetic linkage and association analyses. Bioinformatics. 2005;21:2556–2557. doi: 10.1093/bioinformatics/bti364. [DOI] [PubMed] [Google Scholar]
- Maziade M, Fournier A, Phaneuf D, et al. Chromosome 1q12-q22 linkage results in Eastern Québec families affected by schizophrenia. Am J Med Genet (Neuropsychiatric Genetics) 2002;114:51–55. doi: 10.1002/ajmg.1616. [DOI] [PubMed] [Google Scholar]
- Ott J. Analysis of human genetic linkage. Baltimore: Johns Hopkins University Press; 1999. [Google Scholar]
- Schaffer AA. Faster linkage analysis computations for pedigrees with loops or unused alleles. Human Heredity. 1996;46:226–235. doi: 10.1159/000154358. [DOI] [PubMed] [Google Scholar]
- Lathrop GM, Lalouel JM, Julier C, Ott J. Strategies for multilocus linkage analysis in humans. Proc Natl Acad Sci USA. 1984;81:3443–3446. doi: 10.1073/pnas.81.11.3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lander E, Kruglyak L. Genetic dissection of complex traits: guidelines for interpreting and reporting linkage results. Nat Genet. 1995;11:241–247. doi: 10.1038/ng1195-241. [DOI] [PubMed] [Google Scholar]
- Stöber G, Saar K, Rüschendorf F, et al. Splitting schizophrenia: periodic catatonia-susceptibility locus on chromosome 15q15. Am J Hum Genet. 2000;67:1201–1207. doi: 10.1016/s0002-9297(07)62950-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park N, Juo SH, Cheng R, et al. Linkage analysis of psychosis in bipolar pedigrees suggests novel putative loci for bipolar disorder and shared susceptibility with schizophrenia. Mol Psychiatry. 2004;9:1091–1099. doi: 10.1038/sj.mp.4001541. [DOI] [PubMed] [Google Scholar]
- Etain B, Mathieu F, Rietschel M, et al. Genome-wide scan for genes involved in bipolar affective disorder in 70 European families ascertained through a bipolar type I early-onset proband: supportive evidence for linkage at 3p14. Mol Psychiatry. 2006;11:685–694. doi: 10.1038/sj.mp.4001815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Glatt SJ, Su J, Tsuang MT. Three potential susceptibility loci shown by a genome-wide scan for regions influencing the age at onset of mania. Am J Psychiatry. 2004;161:625–630. doi: 10.1176/appi.ajp.161.4.625. [DOI] [PubMed] [Google Scholar]
- Szatmari P, Maziade M, Zwaigenbaum LZ, et al. Informative phenotypes for genetic studies of psychiatric disorders. Am J Med Genet B Neuropsychiatr Genet. 2007;144:581–588. doi: 10.1002/ajmg.b.30426. [DOI] [PubMed] [Google Scholar]
- Braff DL, Freedman R, Schork NJ, Gottesman I. Deconstructing schizophrenia: an overview of the use of endophenotypes in order to understand a complex disorder. Schizophr Bull. 2007;33:21–32. doi: 10.1093/schbul/sbl049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett CW, Flax JF, Logue MW, et al. A major susceptibility locus for specific language impairment is located on 13q21. Am J Hum Genet. 2002;71:45–55. doi: 10.1086/341095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schretlen DJ, Cascella NG, Meyer SM, et al. Neuropsychological functioning in bipolar disorder and schizophrenia. Biol Psychiatry. 2007;62:179–186. doi: 10.1016/j.biopsych.2006.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziade M, Rouleau N, Gingras N, et al. Shared Neurocognitive Dysfunctions in Young Offspring at Extreme Risk for Schizophrenia or Bipolar Disorder in Eastern Quebec Multigenerational Families Schizophr Bull 2008. available online 11 June 2008 [e-pub ahead of print]. [DOI] [PMC free article] [PubMed]
- Snitz BE, Macdonald AW, III, Carter CS. Cognitive deficits in unaffected first-degree relatives of schizophrenia patients: a meta-analytic review of putative endophenotypes. Schizophr Bull. 2006;32:179–194. doi: 10.1093/schbul/sbi048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maziade M, Rouleau N, Marino C, et al. Early Exposure to Numerous Parental Hospitalizations: Relationship with IQ and Memory in Young Offspring at Extreme Genetic Risk of Schizophrenia and Bipolar DisorderSubmitted.
- Wijsman EM, Rosenthal EA, Hall D, et al. Genome-wide scan in a large complex pedigree with predominantly male schizophrenics from the island of Kosrae: evidence for linkage to chromosome 2q Mol Psychiatry 20038695–705.643. [DOI] [PubMed] [Google Scholar]
- McInnis MG, Lan TH, Willour VL, et al. Genome-wide scan of bipolar disorder in 65 pedigrees: supportive evidence for linkage at 8q24, 18q22, 4q32, 2p12, and 13q12. Mol Psychiatry. 2003;8:288–298. doi: 10.1038/sj.mp.4001277. [DOI] [PubMed] [Google Scholar]
- Shaw SH, Kelly M, Smith AB, et al. A genome-wide search for schizophrenia susceptibility genes. Am J Med Genet (Neuropsychiatric Genetics) 1998;81:364–376. doi: 10.1002/(sici)1096-8628(19980907)81:5<364::aid-ajmg4>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Ginns EI, Ott J, Egeland JA, et al. A genome-wide search for chromosomal loci linked to bipolar affective disorder in the Old Order Amish. Nat Genet. 1996;12:431–435. doi: 10.1038/ng0496-431. [DOI] [PubMed] [Google Scholar]
- Camp NJ, Neuhausen SL, Tiobech J, Polloi A, Coon H, Myles-Worsley M. Genomewide multipoint linkage analysis of seven extended Palauan pedigrees with schizophrenia, by a Markov-chain Monte Carlo method. Am J Hum Genet. 2001;69:1278–1289. doi: 10.1086/324590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badenhop RF, Moses MJ, Scimone A, et al. A genome screen of a large bipolar affective disorder pedigree supports evidence for a susceptibility locus on chromosome 13q. Mol Psychiatry. 2001;6:396–403. doi: 10.1038/sj.mp.4000887. [DOI] [PubMed] [Google Scholar]
- Potash JB, Zandi PP, Wilmour VL, et al. Suggestive linkage to chromosomal regions 13q31 and 22q12 in families with psychotic bipolar disorder. Am J Psychiatry. 2003;160:680–686. doi: 10.1176/appi.ajp.160.4.680. [DOI] [PubMed] [Google Scholar]
- Kelsoe JR, Spence MA, Loetscher E, et al. A genome survey indicates a possible susceptibility locus for bipolar disorder on chromosome 22. Proc Natl Acad Sci USA. 2001;98:585–590. doi: 10.1073/pnas.011358498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw SH, Mroczkowski-Parker Z, Shekhtman T, et al. Linkage of a bipolar disorder susceptibility locus to human chromosome 13q32 in a new pedigree series. Mol Psychiatry. 2003;8:558–564. doi: 10.1038/sj.mp.4001267. [DOI] [PubMed] [Google Scholar]
- Brzustowicz LM, Honer WG, Chow EWC, et al. Linkage of Familial Schizophrenia to Chromosome 13q32. Am J Hum Genet. 1999;65:1096–1103. doi: 10.1086/302579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stine OC, McMahon FJ, Chen L-S, et al. Initial genome screen for bipolar disorder in the NIMH genetics initiative pedigrees: Chromosomes 2. 11. 13. 14. and X. Am J Med Genet(Neuropsychiatric Genetics) 1997;74:263–269. [PubMed] [Google Scholar]
- Lin MW, Sham P, Hwu HG, Collier D, Murray R, Powell JF. Suggestive evidence for linkage of schizophrenia to markers on chromosome 13 in Caucasian but not Oriental populations. Hum Genet. 1997;99:417–420. doi: 10.1007/s004390050382. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Skol AD, Tsuang DW, et al. Linkage of chromosome 13q32 to schizophrenia in a large veterans affairs cooperative study sample. Am J Med Genet. 2002;114:598–604. doi: 10.1002/ajmg.10601. [DOI] [PubMed] [Google Scholar]
- Detera-Wadleigh S, Badner JA, Berrettini WH, et al. A high-density genome scan detects evidence for a bipolar disorder susceptibility locus on 13q32 and other potential loci on 1q32 and 18p11.2. Proc Natl Acad Sci USA. 1999;96:5604–5609. doi: 10.1073/pnas.96.10.5604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J, Juo SH, Dewan A, et al. Evidence for a putative bipolar disorder locus on 2p13-16 and other potential loci on 4q31, 7q34, 8q13, 9q31, 10q21-24, 13q32, 14q21 and 17q11-12. Mol Psychiatry. 2003;8:333–342. doi: 10.1038/sj.mp.4001254. [DOI] [PubMed] [Google Scholar]
- Liu C, Badner JA, Christian SL, Guroff JJ, Detera-Wadleigh SD, Gershon ES. Fine mapping supports previous linkage evidence for a bipolar disorder susceptibility locus on 13q32. Am J Med Genet. 2001;105:375–380. doi: 10.1002/ajmg.1358. [DOI] [PubMed] [Google Scholar]
- Blouin J-L, Dombroski BA, Nath SK, et al. Schizophrenia susceptibility loci on chromosomes 13q32 and 8p21. Nat Genet. 1998;20:70–73. doi: 10.1038/1734. [DOI] [PubMed] [Google Scholar]
- Mulle JG, McDonough JA, Chowdari KV, Nimgaonkar V, Chakravarti A. Evidence for linkage to chromosome 13q32 in an independent sample of schizophrenia families. Mol Psychiatry. 2005;10:429–431. doi: 10.1038/sj.mp.4001639. [DOI] [PubMed] [Google Scholar]
- Cardno AG, Holmans PA, Rees MI, et al. A genomewide linkage study of age at onset in schizophrenia. Am J Med Genet (Neuropsychiatric Genetics) 2001;105:439–445. doi: 10.1002/ajmg.1404. [DOI] [PubMed] [Google Scholar]
- Abecasis GR, Burt RA, Hall D, et al. Genomewide scan in families with schizophrenia from the founder population of Afrikaners reveals evidence for linkage and uniparental disomy on chromosome 1. Am J Psychiatry. 2004;74:403–417. doi: 10.1086/381713. [DOI] [PMC free article] [PubMed] [Google Scholar]