Abstract
Attention deficit hyperactivity disorder (ADHD) is a common neuropsychiatric disorder. Genetics has an important role in the aetiology of this disease. In this study, we describe the clinical findings in a Dutch family with eight patients suffering from ADHD, in whom five had at least one other psychiatric disorder. We performed a genome-wide (parametric and nonparametric) affected-only linkage analysis. Two genomic regions on chromosomes 7 and 14 showed an excess of allele sharing among the definitely affected members of the family with suggestive LOD scores (2.1 and 2.08). Nonparametric linkage analyses (NPL) yielded a maxNPL of 2.92 (P=0.001) for marker D7S502 and a maxNPL score of 2.56 (P=0.003) for marker D14S275. We confirmed that all patients share the same haplotype in each region of 7p15.1–q31.33 and 14q11.2–q22.3. Interestingly, both loci have been reported before in Dutch (affected sib pairs) and German (extended families) ADHD linkage studies. Hopefully, the genome-wide association studies in ADHD will help to highlight specific polymorphisms and genes within the broad areas detected by our, as well as other, linkage studies.
Keywords: attention deficit hyperactivity disorder, genome-wide linkage analysis
Introduction
Attention deficit hyperactivity disorder (ADHD) is a pervasive neuropsychiatric disorder affecting 4–5% of children and 0.5–2% of adults.1 Genetics has an important role in the aetiology of the disorder. Data from clinical studies support the familial nature of ADHD.2 Twin studies of categorically defined ADHD estimated heritability to be 60–90%.3 Smalley4 and Faraone et al5 reported sibling relative-risk ratios (λs) of 4.0–8.0. Adoption studies report an increased frequency of ADHD in biological relatives of probands.6, 7, 8 Smalley4 proposed a genetic model for ADHD with an involvement of multiple genes with minor-to-moderate effect sizes interacting in an additive manner. Genome-wide exclusion mapping9 and molecular studies of candidate genes10 support this theory. However, the exact aetiology of ADHD is still unknown.
The search for susceptibility genes involved in the development of ADHD has focused mostly on the dopaminergic system, largely because of the therapeutic effects of methylphenidate hydrochloride, which increases extracellular dopamine levels by inhibiting re-uptake from the synaptic cleft. Many association studies on genes such as the dopamine D4 receptor gene (DRD4), the dopamine D5 receptor gene (DRD5), dopamine beta hydroxylase (DBH), dopamine transporter (DAT1 or SLC6A3) and the synaptosomal-associated protein of 25 kDa (SNAP25) provide further support for the involvement of the dopaminergic pathway.11, 12, 13
Several studies have also implicated the serotonergic and noradrenergic neurotransmitter systems as being involved in the pathophysiology of the disorder.14 The observation that methylphenidate decreases hyperactivity in DAT1 knockout mice by increasing 5-HT transmission could mean the involvement of the serotonin system in the aetiology of ADHD.15 In addition, low platelet and whole-blood 5-HT levels have been reported in ADHD probands.16 There is evidence of the involvement of serotonin transporter (5-HTT) and receptor (HTR2A and HTR1B) genes.17 The involvement of the noradrenergic system, the alpha 1C, 2A and 2C adrenergic receptor (ADRA1C, 2A, 2C) genes, is equivocal and further study is needed.17
Most replicated polymorphism studies showed negative as well as positive findings, and conclusive evidence of the involvement of any specific gene has not yet been presented.13, 17
Since recently, genome-wide association studies (GWA) are becoming available for ADHD.18, 19, 20 Eventually, they will lead to the identification of novel genes or pathways, as genome-wide studies do not rely on current biological knowledge. To date, eight genome-wide linkage analyses (GWLA) have been performed in ADHD. These studies have been conducted mainly in affected sib pairs (5),9, 21, 22, 23, 24, 25 in isolated populations (2)26, 27 and in extended pedigrees (1).28
We describe the clinical findings of a Dutch family with several members suffering from ADHD and the results from the second GWLA that applies the extended pedigree strategy in ADHD.
Materials and methods
Subjects
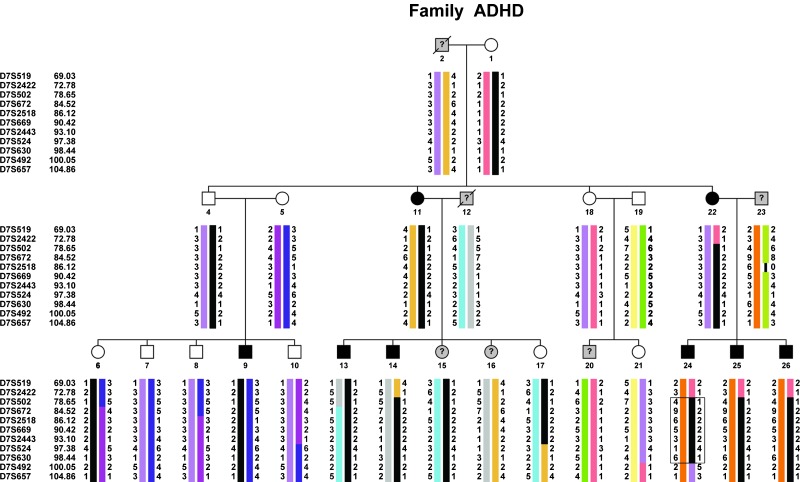
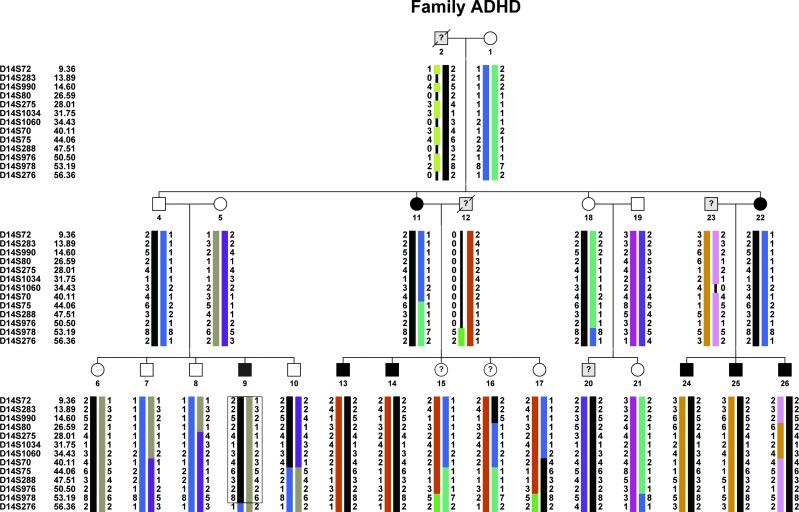
The family (as shown in Figures 1 and 2) consisted of 37 persons in three generations, of which 24 participated in the study. In total, six individuals died before the start of this research. A total of five persons refused to participate and two did not fulfil our age inclusion criterion (>12 years).
Figure 1.
: Family tree showing microsatellite haplotypes corresponding to the 7p15.1–q31.33 region. Marker order is according to the sex-averaged Marshfield map. A black bar represents the haplotype segregating with the disease. The minimum candidate region determined by recombinations is boxed (person III-24). Clinical phenotypes are as follows: blackened symbol ‘ADHD definitely affected', (?) ‘ADHD possibly affected' or not examined (deceased) and white symbol ‘likely not affected'. For linkage analysis, individuals classified as ‘possibly affected' and ‘likely not affected' were coded as ‘diagnosis unknown'. Haplotypes from persons I-2 and II-12 (both deceased) are inferred.
Figure 2.
Family tree showing microsatellite haplotypes corresponding to the 14q11.2–q22.3 region. See legend of Figure 1. The minimum candidate region for chromosome 14 is boxed (person III-9).
A total of 10 female (41.7%) and 14 male (age range: 13–83 years) were included in the study. Four children were between 13 and 16 years of age. One older family member (brother of I-2, not displayed in figures) participated in the research by donating a blood sample, but he refused to be interviewed or examined.
Signed informed consent, as approved by the Medical Ethics Committee of the Erasmus Medical Centre and the Dutch Central Committee on Human-related Research (CCMO), was obtained during the first visit. In the case of children between 12 and 18 years of age, both parents co-signed the consent form.
Diagnostic assessment
Clinical evaluation
During home visits, all participating family members underwent a semi-structured interview (MV) to assess the presence of ADHD symptoms on the basis of DSM-IV criteria (American Psychiatric Association29), the history or presence of other psychiatric or somatic disorders and the use of medication. If possible, parents were interviewed regarding ADHD symptoms during the school age period of their children. Each subject also filled in a self-report questionnaire regarding the presence of ADHD symptoms according to the DSM-IV criteria in childhood and adulthood.
Six or more of the inattentive and/or hyperactive/impulsive criteria in childhood had to be present in order to be diagnosed as ADHD. A second psychiatrist (MvdL), experienced in diagnosing ADHD in adults, performed a clinical assessment of the family members. The final diagnosis of ADHD was based on a consensus between the two psychiatrists. In addition, school reports, medical and psychological reports, if present, were studied for clues for ADHD.
Questionnaires
All subjects were administered the Structured Clinical Interview for DSM-IV Axis I disorders30 (validated Dutch version: Groenestijn et al31) and Axis II Personality Disorders32 (validated Dutch version: Weertman et al33), from which we only evaluated the presence of borderline and antisocial personality disorder.
Phenotyping
Our behavioural phenotypes consisted of ‘ADHD definitely affected', in which subjects met the full childhood DSM-IV ADHD criteria with onset of symptoms before the age of 7 years and with persistence of clearly impairing symptoms in more than one setting, and ‘ADHD possibly affected' if they failed to meet the DSM-IV ADHD criteria, particularly with respect to impairment or by meeting only five instead of the six criteria of the inattentive and/or hyperactive subtype in childhood. Individuals who did not meet a minimum of five out of six criteria of the inattentive and/or hyperactive subtype in childhood (DSM-IV ADHD criteria) were classified as ‘likely unaffected'.
Laboratory analysis
Blood samples were collected from 24 available family members. Genomic DNA was extracted from peripheral blood using the Puregene DNA purification kit from Gentra Systems (Minneapolis, MN, USA).
A genome-wide screen was carried out with 382 fluorescently labelled markers from the ABI PRISM MD-10 Linkage v. 2.5 Mapping Set (Applied Biosystems, Foster City, CA, USA), covering all autosomes with an average spacing of 10 cM. Additional markers from the Marshfield integrated genetic map (available online at http://research.marshfieldclinic.org/genetics/GeneticResearch/compMaps.asp) were genotyped for fine mapping of ‘positive' regions. PCR products were pooled and loaded onto an ABI 3100 automatic DNA sequencer (Foster City, CA, USA); data were analysed using GeneMapper v.2 (Applied Biosystems). Mega234 was used to process the genetic data into the appropriate format.
Linkage analysis
Owing to the uncertainties related to the correct genetic model in ADHD, parametric and nonparametric linkage analyses (NPL) were performed using Simwalk2 software (version 2.9, Eric Sobel, University of California, Los Angeles (UCLA), CA, USA).35 For parametric analysis, we specified an autosomal dominant mode of inheritance, a mutant allele frequency of 1 in 1000 and equal marker allele frequencies. Marker order and genetic distances were based on the Marshfield integrated linkage map. For some markers with an unresolved order, the Icelandic (deCODE) genetic map was used. A phenocopy rate of 1 in 1000 and a reduced penetrance of 80% were applied. A conservative affected-only design was used, thus all individuals in whom ADHD was not clinically proven (ADHD possibly affected and likely unaffected) were classified as ‘diagnosis unknown'.
A total of 1000 simulations (SLINK and MSIM programs, Jurg Ott, Rockefeller University New York, NY, USA)36 were performed using the genetic model specified above. To evaluate the use of a more conservative (and less powerful) ‘affected only' design, two simulation analyses were performed. The first considered an ‘affected only' disease status definition and the second design included all clinical information available.
Pedigree location scores (directly comparable with multipoint LOD scores) were calculated.
For nonparametric analysis, the maximum-tree statistic (max-tree, the largest number of affected members inheriting an allele from one founder allele)37 is reported. This statistic was designed for traits best modelled by dominant inheritance. The NPL-All statistic, a measure of whether a few founder alleles are overly present in affected members, is reported as well (designed for traits best modelled by additive inheritance).37 Empirical P-values (10 000 simulations) were also obtained. This P-value is the probability of obtaining a value for that statistic that is equal to or greater than the observed value, if the traits were not linked to markers.
For positive regions, haplotypes were constructed using Simwalk2 and were subsequently checked manually on the basis of the minimal number of recombinations. To display haplotypes, the programme HaploPainter38 (Holger Thiele, Gene Mapping Center, Max Delbrueck Center for Molecular Medicine, and Cologne Center for Genomics, University of Cologne, Germany) was used.
Results
Psychiatric diagnosis
A total of 8 out of 24 family members (33%) were diagnosed as ADHD ‘definitely affected' (three had ADHD of the combined type, four had the inattentive type and one had the hyperactive/impulsive type). ADHD ‘possibly affected' was diagnosed in four members (17%) (See Figure 1).
Comorbidity
Except for tic disorders (more frequent in the unaffected or possibly affected group) and nicotine use disorder (equally present in both groups), we found more comorbidity in the ADHD-diagnosed group than in the unaffected or possibly affected group (ie, obsessive compulsive disorder was found in 38% of the ADHD group compared with 19% in the unaffected or probably affected group, Table 1). The average number of comorbidities per patient was higher in the ADHD-diagnosed group as compared with that in the unaffected or possibly affected group (3.4 versus 2.3, respectively). The percentage of patients having one or more comorbid disorders was 63% in the ADHD group versus 69% in the unaffected and possibly affected group (Table 1). We did not diagnose the presence of a borderline or antisocial personality disorder in any member of this family. The majority (75%) of ADHD patients were male (six out of eight). In the group diagnosed as unaffected or possibly affected, the male–female ratio was 1:1.
Table 1. Lifetime psychiatric comorbidity in a Dutch family with ADHD (N (%)).
| DSM-IV axis I | ADHD N=8 | ADHD LU/PA, N=16 |
|---|---|---|
| Alcohol-use disordera | 2 (25) | 2 (13) |
| Cannabis-use disorderb | 1 (13) | 1 (6) |
| Nicotine-use disorderc | 4 (50) | 8 (50) |
| Depressive disorderd | 3 (38) | 4 (25) |
| Anxiety disorder | 3 (38) | 2 (13) |
| Tic disorder | 1 (13) | 5 (31) |
| Obsessive compulsive disorder | 3 (38) | 3 (19) |
| Comorbid disorder(s)e | 5 (63) | 11 (69) |
Abbrevations: ADHD: attention deficit/hyperactivity disorder; LU/PA: likely unaffected and possibly affected; NOS, not otherwise specified.
Dependence or abuse.
Dependence or abuse.
Dependence or abuse.
Major depressive disorder, single or recurrent episode, Dysthymic disorder, depressive disorder NOS.
One or more comorbid disorder.
Genetic studies
At least one individual of the family is an ‘obligate carrier' (Figure 1 and 2, individual II-4); this person transmits the disease gene but the phenotype description and anamnesis were normal. As male-to-male transmission was observed, a causal gene located on the X chromosome was excluded.
Simulation analysis to estimate the probability of detecting genetic linkage, given the pedigree structure (statistical power), was performed. An average LOD score of 1.7 with a maxLOD of 3.3 was obtained when all clinical information was included. A conservative ‘affected only' approach yielded an average LOD score of 1.3 and a maxLOD of 2.1.
Despite the loss in statistical power, we decided to use the ‘affected only' design owing to reduced gene penetrance (a clinically unaffected person could be carrying the disease gene, which could lead to false linkage results).
We performed parametric and NPL for all autosomes. Four regions on chromosomes 3, 7, 14 and 21 showed an excess of allele sharing among the patients of the family. Two of these regions, on chromosomes 7 and 14, showed suggestive LOD scores39 2.1 and 2.08, respectively (Table 2) , very close to the maxLOD predicted by the simulation studies (2.1).
Table 2. Summary of the linkage analysis results.
| Chromosome | Physical map (Mb)a | Genetic map (cM)b | Marker namec | NPL-ALL | P-value | LOD score |
|---|---|---|---|---|---|---|
| 7 | 66 | 78.6 | D7S502 | 2.92 | 0.001 | 2.1 |
| 7 | 71.5 | 84.5 | D7S672 | 2.8 | 0.002 | 2.1 |
| 7 | 75.2 | 86.1 | D7S2518 | 2.74 | 0.002 | 2.1 |
| 7 | 77.7 | 90.4 | D7S669 | 2.8 | 0.002 | 2.1 |
| 7 | 79.7 | 93.1 | D7S2443 | 2.7 | 0.002 | 2.08 |
| 7 | 84.5 | 97.4 | D7S524 | 1.72 | 0.02 | 1.64 |
| 7 | 88.3 | 98.4 | D7S630 | 1.65 | 0.03 | 1.73 |
| 14 | 20.4 | 9.4 | D14S72 | 1.48 | 0.03 | 2.04 |
| 14 | 21.7 | 13.9 | D14S283 | 1.88 | 0.01 | 2.07 |
| 14 | 22.6 | 14.6 | D14S990 | 1.92 | 0.01 | 2.07 |
| 14 | 25.8 | 28 | D14S275 | 2.56 | 0.003 | 2.08 |
| 14 | 26.8 | 26.6 | D14S80 | 2.5 | 0.003 | 2.08 |
| 14 | 32.5 | 34.4 | D14S1060 | 2.54 | 0.003 | 2.08 |
| 14 | 33.5 | 40.1 | D14S70 | 2.45 | 0.003 | 2.08 |
| 14 | 36.5 | 44.1 | D14S75 | 2.17 | 0.007 | 2.08 |
| 14 | 43.2 | 47.5 | D14S288 | 2.17 | 0.007 | 2.08 |
| 14 | 47.6 | 50.5 | D14S976 | 2.22 | 0.006 | 2.08 |
| 14 | 49.2 | 52.5 | D14S984 | 2.2 | 0.006 | 2.08 |
| 14 | 51 | 53.2 | D14S978 | 1.74 | 0.018 | 1.95 |
| 14 | 52.9 | 55.3 | D14S989 | 1.2 | 0.06 | −0.42 |
According to NCBI build 36.3.
According to the sex-averaged Marshfield map.
Markers displayed in italic were tested during the fine mapping phase.
By haplotype analysis, we could exclude the regions on chromosomes 3 and 21, as one patient (III-14) was not sharing the ‘affected' haplotype (data not shown). We then refined the regions on chromosomes 7 and 14 by testing 17 extra markers. Parametric linkage analysis again yielded suggestive LOD scores: 2.1 for markers D7S502, D7S672, D7S2518 and D7S669 (at 0 recombination fraction). The maximum NPL (2.92) in the region was observed for marker D7S502 (P=0.001), followed by markers D7S672 and D7S669 (NPL=2.8, P=0.002).
By haplotype analysis on 7p15.1–q31.33 (Figure 1), we observed that all eight patients share the same haplotype extending from D7S2422 (72.8 cM, 51.1 Mb) to D7S492 (100.1 cM, 89.2 Mb). Recombination events occurring in patients II-22, III-14 and III-24 determined the upper (p-arm) and lower (q-arm) border. The minimum region extended 20 cM (D7S502–D7S630, 78.7–98.4 cM, 66.7–88.3 Mb), containing 161 genes (NCBI build 36.3).
For chromosome 14, the maxLOD score (2.08) was obtained for markers D14S80–D14S984 (Table 2), with a maxNPL score of 2.56 for marker D14S275 (P=0.003). Haplotype analysis on 14q11.2–q22.3 showed a common haplotype shared by all patients extending from the centromere to 14q (D14S72–D14S276), comprising at least 47 cM. A recombination event observed in patient III-9 delimited the lower border of this large region (Figure 2).
We also observed the presence of the ‘disease haplotype' in individuals free of symptoms: II-4 (carrier) and III-6 for chromosome 7, and II-4, II-18 and III-6 for the chromosome 14 region.
Discussion
We clinically characterized a family with more than 30% of the participating members diagnosed with ADHD. The overall frequency of DSM-IV Axis I comorbidity in the definitely affected group (63%) is lower than the frequencies found in most studies among adults with ADHD (75%).2, 40 The frequency of tic disorder was high, particularly in the ‘possibly affected' and ‘likely unaffected' group (31%). A total of 25% (6 out of 24) of the investigated relatives had a tic disorder.
Owing to the scarceness of families with a sufficient number of patients allowing a powerful linkage analysis, most GWLA in ADHD were limited to sib pair cohorts9, 21, 22, 23, 24, 25 and to isolated populations in the region of Antioquia, Colombia26 and the southwest of The Netherlands.27 Recently, Romanos et al28 published the only GWLA performed in unrelated extended pedigrees. Factors complicating linkage analysis, such as reduced penetrance and bilinear inheritance, were present in several families.
We performed a GWLA in a Dutch family using parametric and nonparametric affected-only analysis designs. With both analyses, two regions on chromosomes 7 (72.8–100.1 cM) and 14 (9–56.36 cM) yielded suggestive LOD scores on the basis of Lander and Kruglyak's established criteria.39
From the nonparametric analysis, two statistics were examined: the max-tree (dominant model) and the NPL-All (additive model). For both regions, the NPL-All statistic performed better (ie, for D7S502 max-tree NPL 2.2, P=0.007 and for NPL-All 2.9, P=0.001), suggesting that an additive disease model better fits the genetic data than a dominant model.
Interestingly, both loci have been reported before. In view of the complexity of a psychiatric disorder such as ADHD, it is likely that multiple genes with a limited effect size are involved in disease aetiology even in single multigeneration families. The alternative hypothesis is that only one region represents a true linkage finding.
A Dutch sib-pairs study (117 ASPs with ADHD, strict diagnosis criteria, DSM-IV) identified suggestive linkage in a region on chromosome 7p13 (MLS 3.04 for markers D7S1818, 69.9 cM and for D7S2422, 72.8 cM).21 In addition, in a 155 German ADHD sib-pairs study, both regions (D7S2490, 88 cM and D14S306, 46 cM)22 showed (nominal) linkage signals. Furthermore, in eight extended families with ADHD of German origin, GWLA revealed linkage signals at 7q21.11 (LOD 3.14, 84–89 cM) and 14q12 (LOD 4.17, 16 cM), when analysing families together under a narrow diagnostic criteria.28 However, when the families were analysed independently, other chromosomal regions were highlighted. Recently, a meta-analysis of seven GWLA in ADHD (five affected sib pairs and two multigenerational pedigrees studies) identified a significant linkage signal on chromosome 16 and several regions with nominal linkage signals on chromosomes 5, 6, 7, 8, 9, 15 and 17.41 The region on chromosome 7 (60–91 cM) overlaps the region detected in our family (72.8–100.1 cM).
A recent study converged evidence from their GWA (500K SNP arrays) and from extended pedigrees GWLA (50K), and found several common candidate loci that overlapped across the studies.42 They reported the locus on 14q11.2–12, which overlaps with the region found in our family. With the GWA analysis, two genes from the area were highlighted: SLC7A8 and NOVA1.42
It is remarkable that in a clinically and genetically heterogeneous disorder such as ADHD, overlapping genomic regions are reported by studies conducted in different populations, using different assessment, genotyping and analysis strategies. Hopefully, the ongoing GWA studies18, 19, 20 will help to highlight specific SNPs and genes within the broad areas detected by our, as well as other, linkage studies. In conclusion, we performed a GWLA in a relatively large Dutch family with eight ADHD patients and found two (replicated) loci showing suggestive evidence of linkage on chromosomes 7p and 14q.
Acknowledgments
The authors thank the family for their cooperation. This research was partially funded by the Center for Biomedical Genetics (CBG), The Netherlands.
References
- Buitelaar JK. Epidemiology: What Have We Learned Over The Last Decade? Cambridge: Cambridge University Press; 2002. [Google Scholar]
- Biederman J, Faraone SV, Keenan K, et al. Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder. Patterns of comorbidity in probands and relatives psychiatrically and pediatrically referred samples. Arch Gen Psychiatry. 1992;49:728–738. doi: 10.1001/archpsyc.1992.01820090056010. [DOI] [PubMed] [Google Scholar]
- Levy F, Hay DA, McStephen M, Wood C, Waldman I. Attention-deficit hyperactivity disorder: a category or a continuum? Genetic analysis of a large-scale twin study. J Am Acad Child Adolesc Psychiatry. 1997;36:737–744. doi: 10.1097/00004583-199706000-00009. [DOI] [PubMed] [Google Scholar]
- Smalley SL. Genetic influences in childhood-onset psychiatric disorders: autism and attention-deficit/hyperactivity disorder. Am J Hum Genet. 1997;60:1276–1282. doi: 10.1086/515485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Monuteaux MC. Toward guidelines for pedigree selection in genetic studies of attention deficit hyperactivity disorder. Genet Epidemiol. 2000;18:1–16. doi: 10.1002/(SICI)1098-2272(200001)18:1<1::AID-GEPI1>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- Morrison JR, Stewart MA. The psychiatric status of the legal families of adopted hyperactive children. Arch Gen Psychiatry. 1973;28:888–891. doi: 10.1001/archpsyc.1973.01750360098015. [DOI] [PubMed] [Google Scholar]
- Cantwell DP. Genetics of hyperactivity. J Child Psychol Psychiatry. 1975;16:261–264. doi: 10.1111/j.1469-7610.1975.tb01275.x. [DOI] [PubMed] [Google Scholar]
- van den Oord EJ, Boomsma DI, Verhulst FC. A study of problem behaviours in 10- to 15-year-old biologically related and unrelated international adoptees. Behav Genet. 1994;24:193–205. doi: 10.1007/BF01067187. [DOI] [PubMed] [Google Scholar]
- Fisher SE, Francks C, McCracken JT, et al. A genomewide scan for loci involved in attention-deficit/hyperactivity disorder. Am J Hum Genet. 2002;70:1183–1196. doi: 10.1086/340112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Doyle AE, Mick E, Biederman J. Meta-analysis of the association between the 7-repeat allele of the dopamine D(4) receptor gene and attention deficit hyperactivity disorder. Am J Psychiatry. 2001;158:1052–1057. doi: 10.1176/appi.ajp.158.7.1052. [DOI] [PubMed] [Google Scholar]
- Kirley A, Hawi Z, Daly G, et al. Dopaminergic system genes in ADHD: toward a biological hypothesis. Neuropsychopharmacology. 2002;27:607–619. doi: 10.1016/S0893-133X(02)00315-9. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Khan SA. Candidate gene studies of attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006;67 Suppl 8:13–20. [PubMed] [Google Scholar]
- Gizer IR, Ficks C, Waldman ID. Candidate gene studies of ADHD: a meta-analytic review. Hum Genet. 2009;9:9. doi: 10.1007/s00439-009-0694-x. [DOI] [PubMed] [Google Scholar]
- Hawi Z, Lowe N, Kirley A, et al. Linkage disequilibrium mapping at DAT1, DRD5 and DBH narrows the search for ADHD susceptibility alleles at these loci. Mol Psychiatry. 2003;8:299–308. doi: 10.1038/sj.mp.4001290. [DOI] [PubMed] [Google Scholar]
- Gainetdinov RR, Wetsel WC, Jones SR, Levin ED, Jaber M, Caron MG. Role of serotonin in the paradoxical calming effect of psychostimulants on hyperactivity. Science. 1999;283:397–401. doi: 10.1126/science.283.5400.397. [DOI] [PubMed] [Google Scholar]
- Bhagavan HN, Coleman M, Coursin DB. The effect of pyridoxine hydrochloride on blood serotonin and pyridoxal phosphate contents in hyperactive children. Pediatrics. 1975;55:437–441. [PubMed] [Google Scholar]
- Bobb AJ, Castellanos FX, Addington AM, Rapoport JL. Molecular genetic studies of ADHD: 1991–2004. Am J Med Genet B Neuropsychiatr Genet. 2005;132B:109–125. [PubMed] [Google Scholar]
- Rommelse NN, Arias-Vasquez A, Altink ME, et al. Neuropsychological endophenotype approach to genome-wide linkage analysis identifies susceptibility loci for ADHD on 2q21.1 and 13q12.11. Am J Hum Genet. 2008;83:99–105. doi: 10.1016/j.ajhg.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasky-Su J, Neale BM, Franke B, et al. Genome-wide association scan of quantitative traits for attention deficit hyperactivity disorder identifies novel associations and confirms candidate gene associations. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1345–1354. doi: 10.1002/ajmg.b.30867. [DOI] [PubMed] [Google Scholar]
- Neale BM, Lasky-Su J, Anney R, et al. Genome-wide association scan of attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1337–1344. doi: 10.1002/ajmg.b.30866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakker SC, van der Meulen EM, Buitelaar JK, et al. A whole-genome scan in 164 Dutch sib pairs with attention-deficit/hyperactivity disorder: suggestive evidence for linkage on chromosomes 7p and 15q. Am J Hum Genet. 2003;72:1251–1260. doi: 10.1086/375143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebebrand J, Dempfle A, Saar K, et al. A genome-wide scan for attention-deficit/hyperactivity disorder in 155 German sib-pairs. Mol Psychiatry. 2006;11:196–205. doi: 10.1038/sj.mp.4001761. [DOI] [PubMed] [Google Scholar]
- Ogdie MN, Bakker SC, Fisher SE, et al. Pooled genome-wide linkage data on 424 ADHD ASPs suggests genetic heterogeneity and a common risk locus at 5p13. Mol Psychiatry. 2006;11:5–8. doi: 10.1038/sj.mp.4001760. [DOI] [PubMed] [Google Scholar]
- Asherson P, Zhou K, Anney RJ, et al. A high-density SNP linkage scan with 142 combined subtype ADHD sib pairs identifies linkage regions on chromosomes 9 and 16. Mol Psychiatry. 2008;13:514–521. doi: 10.1038/sj.mp.4002140. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Doyle AE, Lasky-Su J, et al. Linkage analysis of attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1387–1391. doi: 10.1002/ajmg.b.30631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcos-Burgos M, Castellanos FX, Pineda D, et al. Attention-deficit/hyperactivity disorder in a population isolate: linkage to loci at 4q13.2, 5q33.3, 11q22, and 17p11. Am J Hum Genet. 2004;75:998–1014. doi: 10.1086/426154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amin N, Aulchenko YS, Dekker MC, et al. Suggestive linkage of ADHD to chromosome 18q22 in a young genetically isolated Dutch population. Eur J Hum Genet. 2009;21:21. doi: 10.1038/ejhg.2008.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romanos M, Freitag C, Jacob C, et al. Genome-wide linkage analysis of ADHD using high-density SNP arrays: novel loci at 5q13.1 and 14q12. Mol Psychiatry. 2008;13:522–530. doi: 10.1038/mp.2008.12. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Washington, D.C: American Psychiatric Press; 1994. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) Washington D.C.: American Psychiatric Press; 1997. [Google Scholar]
- Groenestijn vMAC, Akkerhuis GW, Kupka RW, Schneider N, Nolen WA. Gestructureerd Klinisch Interview Voor De Vaststelling Van DSM-IV As I Stoornissen. Lisse, The Netherlands: Swets & Zeitlinger BV; 1999. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin L. Structured Clinical Interview for DSM-IV Axis II Personality Disorder (SCID II) Washington D.C.: American Psychiatric Press; 1997. [Google Scholar]
- Weertman A, Arntz A, Kerhos MLM. Gestructureerd Klinisch Interview Voor De Vaststelling Van DSM-IV As II Stoornissen. Lisse, The Netherlands: Swets & Zeitlinger BV; 1999. [Google Scholar]
- Mukhopadhyay N, Almasy L, Schroeder M, Mulvihill WP, Weeks DE. Mega2: data-handling for facilitating genetic linkage and association analyses. Bioinformatics. 2005;21:2556–2557. doi: 10.1093/bioinformatics/bti364. [DOI] [PubMed] [Google Scholar]
- Sobel E, Lange K. Descent graphs in pedigree analysis: applications to haplotyping, location scores, and marker-sharing statistics. Am J Hum Genet. 1996;58:1323–1337. [PMC free article] [PubMed] [Google Scholar]
- Ott J. Computer-simulation methods in human linkage analysis. Proc Natl Acad Sci USA. 1989;86:4175–4178. doi: 10.1073/pnas.86.11.4175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange EM, Lange K. Powerful allele sharing statistics for nonparametric linkage analysis. Hum Hered. 2004;57:49–58. doi: 10.1159/000077389. [DOI] [PubMed] [Google Scholar]
- Thiele H, Nurnberg P. HaploPainter: a tool for drawing pedigrees with complex haplotypes. Bioinformatics. 2005;21:1730–1732. doi: 10.1093/bioinformatics/bth488. [DOI] [PubMed] [Google Scholar]
- Lander E, Kruglyak L. Genetic dissection of complex traits: guidelines for interpreting and reporting linkage results. Nat Genet. 1995;11:541–547. doi: 10.1038/ng1195-241. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Kwon A, Tanguay S, et al. Characteristics of adults with attention deficit hyperactivity disorder plus substance use disorder: the role of psychiatric comorbidity. Am J Addict. 2005;14:319–327. doi: 10.1080/10550490591003639. [DOI] [PubMed] [Google Scholar]
- Zhou K, Dempfle A, Arcos-Burgos M, et al. Meta-analysis of genome-wide linkage scans of attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2008;147B:1392–1398. doi: 10.1002/ajmg.b.30878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesch KP, Timmesfeld N, Renner TJ, et al. Molecular genetics of adult ADHD: converging evidence from genome-wide association and extended pedigree linkage studies. J Neural Transm. 2008;115:1573–1585. doi: 10.1007/s00702-008-0119-3. [DOI] [PubMed] [Google Scholar]