Abstract
Both clinical and experimental data have linked acute ethanol exposure to increased susceptibility to infection as well as increased morbidity and mortality after injury. Macrophages play an integral role in the innate immune system and are important in priming the adaptive immune system. In this study, we investigated the effect of a single in vivo exposure of macrophages to physiologically relevant levels of ethanol (1.2 and 2.9 g/kg) followed by ex vivo stimulation with lipopolysaccharide (LPS) or bacteria. Our study confirms the work of others showing that a single administration of ethanol suppresses the production of tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and IL-12 in response to LPS. There was no effect of ethanol on LPS induction of cytokine production at 30 min after treatment. In contrast, at 3 h, both doses of ethanol exposure decreased ex vivo TNF-α production by splenic and alveolar macrophages. Interestingly, the higher dose of ethanol resulted in sustained suppression of LPS-induced TNF-α production at 3 and 6 h after ethanol administration, as well as decreased IL-6 and IL-12 production after 6 h, as compared to control (saline-treated groups). Alveolar macrophages behaved similarly at 3 h after ethanol treatment. LPS-stimulated production of TNF-α and IL-6 was reduced at 3 h after ethanol administration, when compared with the saline-treated animals. Alveolar macrophages stimulated for 3 h with bacteria also showed decreased TNF-α and IL-6 production after harvested from mice given 2.9 g/kg ethanol for 3 h. This time point and high dose of ethanol also resulted in decreased Pseudomonas aeruginosa phagocytosis by alveolar macrophages. Taken together, we conclude that the effects of physiological levels of ethanol are dose dependent, have effects that last after ethanol is cleared from the circulation, and can affect multiple macrophage functions.
Introduction
Acute and chronic alcohol (ethanol) consumption has been associated with a weakened immune response often resulting in increased susceptibility to bacterial or viral infection (Cook 1998; Nelson and Kolls 2002). Though independent of the duration of alcohol consumed, evidence has shown that there are immunomodulatory effects seen in response to alcohol (Szabo 1999; Nelson and Kolls 2002). Both acute and chronic ethanol exposures have been linked to increased complications in trauma and burn patients (Faunce and others 1997; Germann and others 1997; Messingham and others 2002), and greater morbidity and mortality following infections (Nolan 1965; Ruiz and others 1999; Khan and Yatsuhashi 2000). Interestingly, the effects of ethanol are known to occur even after it has cleared the circulatory system (Wiese and others 2000).
Chronic ethanol exposure has been associated with modifying cells linked with the adaptive arm of the immune system, including T cell and B cell (Cook and others 1995; Cook 1998; Song and others 2001). Increased proinflammatory cytokine levels in the liver and circulation have also been measured in subjects with chronic ethanol exposure (Deviere and others 1989; Khoruts and others 1991; Cook 1998; Kishore and others 2002). In contrast, acute ethanol exposure reduces proinflammatory cytokine synthesis in response to a pathogenic stimulus and is often studied for its effects on the innate immune system (Nelson and others 1989b; Verma and others 1993; Szabo and others 1996; Szabo 1998; Boe and others 2001). This can result in decreased activation of macrophages and other antigen-presenting cells by suppressing their response to a pathogen, antigen presentation, along with additional functions, such as phagocytosis (Waltenbaugh and Peterson 1997; Girouard and others 1998; Peterson and others 1998; Szabo 1998; Boe and others 2001). Evidence suggest that acute ethanol exposure exhibits the suppressive effects of ethanol by abrogating mitogen-activated protein (MAP) kinase activation, specifically p38 and ERK1/2 phosphorylation (Goral and others 2004; Goral and Kovacs 2005; Drechsler and others 2006). Because MAP kinases are involved in multiple cellular functions, one could hypothesize that multiple functions are affected by acute ethanol exposure.
This study investigated multiple resident macrophage populations and their ability to respond to pattern recognition receptor (PRR) stimulation after acute ethanol exposure. PRRs are immune receptors that recognize microbe-specific pathogen-associated molecular patterns (PAMPs). Commonly studied examples of PRRs on macrophages includes the Toll-like receptors (TLRs). These receptors, such as the activation of TLR4 by lipopolysaccharide (LPS), activate MAP kinases and ultimately a proinflammatory response. Specifically, we show that acute ethanol exposure inhibits both splenic and alveolar macrophage proinflammatory cytokine release in response to LPS stimulation. Acute ethanol exposure also decreased alveolar macrophage cytokine production after stimulation with Escherichia coli, and phagocytosis of Pseudomonas aeruginosa. We conclude that acute ethanol exposure can suppress multiple macrophage functions and these effects are dose dependent.
Materials and Methods
Animals
Eight- to 10-week-old male C57BL/6 mice (Harlan, Indianapolis, IN) were used for all experiments. Mice were acclimated for 1 week upon arrival at the animal facilities of Loyola University Medical Center (Maywood, IL). The studies described were performed in accordance with the guidelines established by the Loyola University Chicago Institutional Animal Care and Use Committee.
Ethanol administration
Mice were randomly divided into two groups. One group, the control group, was given either 100 μL or 300 μL saline intraperitoneally (i.p.). The second group, the experimental group, was given a single i.p. injection of 1.2 or 2.9 g/kg body weight ethanol (100 or 300 μL of 20% v/v ethanol in saline). These doses are equivalent to two drinks for the moderate dose and three to four drinks at the higher dose; quantities of alcohol that are commonly consumed in humans. As described previously, these doses resulted in blood ethanol levels of ∼100 or ∼300 mg/dL at 30 min after administration, respectively (Messingham and others 2000). This was the peak blood alcohol concentration observed for these animals. At this time point, mice were lethargic and displayed poor balance and motor coordination at the higher dose but not at the moderate dose. Three hours after exposure to ethanol, the behavior of ethanol-treated mice returned to normal, and ethanol was no longer present in their circulation. Ethanol levels were measured in blood plasma with NAD–alcohol dehydrogenase assay (Sigma-Aldrich, St. Louis, MO), as described previously (Seitz and Stickel 2007). In the blood ethanol assay, nonspecific background values in the saline-treated mice were subtracted from the values determined in the ethanol-treated mice. Previous studies demonstrated that the i.p. administration of ethanol did not result in the local inflammation because the percentages of macrophages and neutrophils, collected by peritoneal lavage 3 h after the treatment, were similar between control and ethanol-treated mice (Deviere and others 1989).
Cell isolation and culture
Mice were killed at 0.5, 1, 1.5, 3, and 6 h after ethanol or saline exposure. Purified splenic macrophages were obtained from spleen cell suspensions by plastic adherence, as described previously (Goral and others 2004). Briefly, spleen cells were plated in 200 μL RPMI 1640 medium supplemented with 5% FBS, 2 mM glutamine, 100 U/mL penicillin, and 100 μg/mL streptomycin (Invitrogen Life Technologies, San Diego, CA). After 2-h incubation, nonadherent cells were removed by washing three times with warm medium. This method resulted in a cell preparation, which was ∼98% positive for Mac-3 and di-I-acetylated low-density lipoprotein uptake, as shown previously (Goral and others 2004). Alveolar macrophages were isolated by eight sequential 800 μL bronchoalveolar lavages (BAL). Roughly 600 μL of collected BAL fluid and cell suspension was isolated per lavage, for a total of ∼5 ml total BAL fluid. The total BAL fluid was then spun down and characterized as >98% alveolar macrophage by using F4/80 staining and flow cytometry (data not shown). 2 × 105 Cells were plated in 200 μL RPMI 1640 medium supplemented with 5% FBS, 2 mM glutamine, 100 U/mL penicillin, and 100 μg/mL streptomycin. Similar to the splenic macrophage plating protocol, alveolar macrophages were incubated for 2 h and nonadherent cells were removed by washing three times with warm medium. Purified macrophages were cultured for 16 h in RPMI 1640 supplemented with 5% FBS overnight with or without endotoxin (100 ng/mL LPS; E. coli O111:B4; Sigma-Aldrich, St. Louis, MO). In the absence of stimulation, macrophage cytokine levels were undetectable (data not shown). Bacterial activation of alveolar macrophages was accomplished by incubating the macrophages for 3 h with E. coli (K12 strain kindly provided by Dr. Shankar, Burn Shock Trauma Institute, Loyola University Medical Center, Chicago, IL) in RPMI 1640 medium supplemented with 5% FBS. Supernatants were collected after 3 or 16 h, prior to cytokine analysis, and stored at −80°C.
Phagocytosis and microscopy
Macrophage phagocytosis was measured by incubating enhanced green fluorescent protein (EGFP) expressing P. aeruginosa (plasmid pUCP24-EGFP was donated by Dr. John C. Alverdy, University of Chicago, IL) at 20 bacteria per cell for 30 min. Alveolar macrophages were isolated as described above and incubated with the bacteria in RPMI plus 5% FBS and 2 mM glutamine. After 30 min, cells were washed three times with ice-cold phosphate buffered saline (PBS) to arrest the phagocytosis and fixed in 4% paraformaldehyde for 15 min. Cells were then permeabilized with 0.1% Triton X-100 in PBS for 5 min, blocked with 2% bovine serum albumin in PBS for 1 h, and stained with rhodamine phalloidin (Invitrogen, Eugene, OR), according to the manufacturer's specifications. Fluorescent images of the EGFP–P. aeruginosa were captured using a Zeiss Axiovert 200 microscope (Zeiss, Germany). Phagocytosis was measured by calculating the phagocytic index, which is the product of the mean fluorescent intensity of bacteria expressing EGFP per macrophages multiplied by the percent of cells phagocytosing bacteria (Phagocytic index = Mean fluorescent intensity × Percent of phagocytic cells). Image capture and mean fluorescent intensity measurements were done using AxioVision Rel. 4.5 (Zeiss, Germany).
Measurement of TNF-α, IL-6, and IL-12
The concentrations of tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and IL-12 in macrophage supernatants were measured by commercially available OptEIA™ ELISA kits (BD Pharmingen, San Diego, CA), according to the manufacturer's instructions, as described previously (Corinti and others 2003). The lowest detectable limit of these kits are 15.6 pg/mL. Data are expressed as pg/mL.
Statistical analysis
Data are expressed as mean ± SEM of each group. Data were analyzed by t test or analysis of variance (ANOVA), followed by post hoc testing with Fisher's protected least significant difference test using Graphpad Instat 3 (San Diego, CA). A value of p ≤ 0.05 was considered significant.
Results
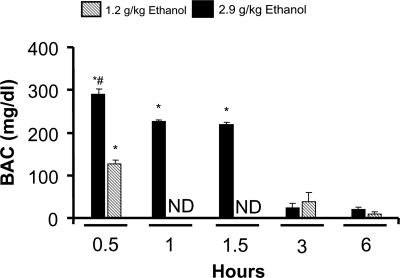
Blood alcohol concentration of mice given a single ethanol dose
Our laboratory has previously performed studies utilizing an acute treatment of 2.9 g/kg ethanol intoxication to show attenuated proinflammatory responses to various TLR activators after 3 h (Goral and others 2004; Goral and Kovacs 2005). In the present study, our initial experiments began by exposing mice to 2.9 g/kg ethanol and measuring their blood alcohol content (BAC) at 0.5, 1, 1.5, 3, and 6 h after treatment. BAC peaked, in our studies, at 0.5 h after treatment reaching levels of 300 mg/dL. Thirty minutes to an 1 h later, the BAC dropped to about 250 mg/dL, but was still five times above the saline control levels (p < 0.05). BAC reached baseline levels after 3 h (Fig. 1). Using a lower dose of ethanol (1.2 g/kg), we noted a BAC peak at 30 min of 150 mg/dL, and returned to control levels by 3 h.
FIG. 1.
Blood alcohol concentration (BAC) was measured 0.5, 3, or 6 h after 1.2 g/kg ethanol (striped bars), or 0.5, 1, 1.5, 3, and 6 h after 2.9 g/kg ethanol (filled bars) intraperitoneal injection. Mice injected with saline for all time points were used as control. ND = not determined. Data are shown as mean BAC ± SEM. N = 3–6 animals. *p < 0.001 from saline control, #p < 0.05 from all other groups.
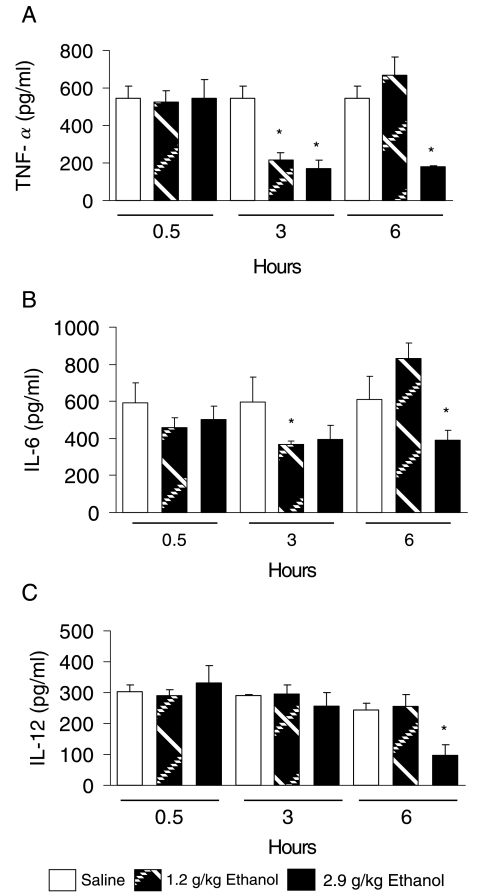
Time course of impaired proinflammatory response after acute ethanol treatment
To understand the temporal effects of two physiologic doses of ethanol on macrophage production of proinflammatory cytokines, we treated mice with either 1.2 or 2.9 g/kg ethanol or saline control, and obtained splenic macrophages at 0.5, 3, and 6 h after treatment. Macrophages were stimulated with 100 ng/mL LPS for 16 h in vitro, after which supernatants were collected for cytokine assay (Fig. 2). After 30 min of ethanol exposure, splenic macrophages isolated from either the moderate (1.2 g/kg) or the high (2.9 g/kg) dose of ethanol showed no differences in TNF-α, IL-6, or IL-12 production, compared to saline controls (Fig. 2A). Three hours after ethanol exposure, both the moderate and the high dose of ethanol caused decreases in ex vivo LPS induction of TNF-α production, compared to control levels (p < 0.05). LPS stimulation of TNF-α production by macrophages isolated from the moderate dose group returned to normal levels by 6 h. This was in contrast to the high dose group, in which LPS activation of TNF-α was still suppressed after 6 h (p < 0.05). LPS induction of IL-6 production showed patterns similar to TNF-α (Fig. 2B). In vivo exposure to the moderate dose of ethanol did not show any effect on splenic macrophage production IL-12 following in vitro stimulation at 30 min, 3 h, or 6 h after ethanol administration (Fig. 2C). The high dose of ethanol did not alter LPS stimulation of IL-12 production at either of the early time points examined, but did show a decrease after 6 h (p < 0.05). In the present study, we did not continue to monitor cytokine production 6 h after treatment, but there is evidence from previous work that the effect seen with the higher dose is present up to 24 h after treatment (Goral and others 2004; Goral and Kovacs 2005).
FIG. 2.
Proinflammatory cytokine production was measured after LPS stimulation of splenic macrophages. Spleens were harvested at 0.5, 3, and 6 h after a single dose of ethanol at 1.2 g/kg (striped bars), or 2.9 g/kg (filled bars), or saline (open bars) as a control. Splenic macrophages were purified as described in Materials and Methods, and stimulated with 100 ng/mL LPS for 16 h. (A) TNF-α, (B) IL-6, and (C) IL-12 were measured by ELISA. Open bars represent saline group, shaded bars represent group treated with 1.2 g/kg ethanol, and filled bars represent group treated with 2.9 g/kg ethanol. Data are shown as mean ± SEM. N = 3–6 animals. *p < 0.05 from saline control group.
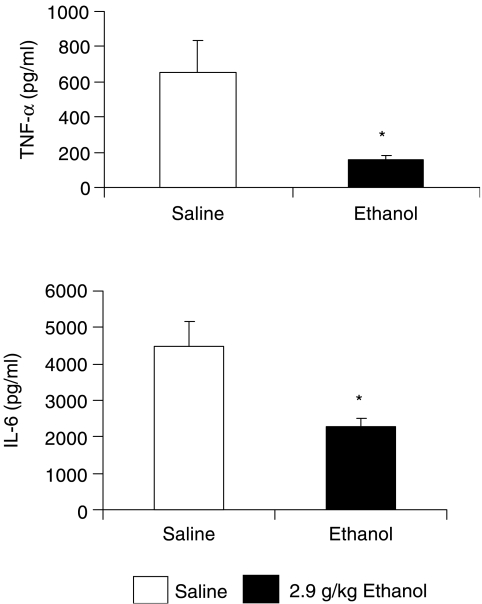
Alveolar macrophage cytokine suppression by acute in vivo ethanol exposure
Pulmonary infection exacerbated by ethanol exposure is a serious clinical problem. Therefore, to test macrophages from a tissue that is more clinically susceptible to repeated infection, we measured proinflammatory cytokine production by alveolar macrophages isolated from the lung. As described above, alveolar macrophages were isolated by BAL from ethanol-exposed and saline-exposed mice. Cells were stimulated with 100 ng/mL LPS for 16 h (Fig. 3). LPS stimulation of alveolar macrophages resulted in robust proinflammatory cytokine production after 16 h, whereas in the absence of stimulation, cytokine concentrations were below the level of detection of the assay kit (data not shown). LPS-induced production of both TNF-α and IL-6 by alveolar macrophages isolated from mice 3 h after they received a single administration of 2.9 g/kg ethanol was attenuated compared to the cytokine production from the macrophages of saline-treated mice. The ethanol-mediated suppression of cytokine production observed with the alveolar macrophages parallel the results found in the splenic macrophages isolated from ethanol-treated mice.
FIG. 3.
TNF-α and IL-6 production by alveolar macrophages stimulated with 100 ng/mL LPS for 16 h. Macrophages were obtained from mice treated with either 2.9 g/kg ethanol (filled bars) or saline control (open bars). Alveolar macrophages were obtained by bronchoalveolar lavage as described in Materials and Methods, 3 h after ethanol exposure. Cells were cultured with LPS for 16 h and supernatant cytokines were measured by ELISA. Data are shown as mean ± SEM. N = 3–4 animals. *p < 0.05.
Cytokine release after exposure to bacteria is reduced following acute ethanol exposure
LPS is a single PAMP that activates a unique receptor, TLR4. Bacterial surfaces, on the other hand, have numerous PAMPs that can stimulate multiple PRRs. Therefore, in order to model a typical interaction between an alveolar macrophage and invading bacterium, we stimulated alveolar macrophages with E. coli at the ratio of 10 bacteria per cell. We also chose E. coli as the bacteria, because the LPS used above was purified from E. coli. Again, alveolar macrophages were obtained by BAL of mice given either saline or 2.9 g/kg ethanol 3 h prior to isolation. Cells were cultured with bacteria for 3 h, and supernatants were collected for TNF-α and IL-6 by ELISA (Table 1). As expected, bacterial stimulation of the alveolar macrophages from the saline group of mice resulted in a robust TNF-α and IL-6 production. Macrophages obtained from the lungs of ethanol-treated mice produced lower levels of these cytokines relative to the macrophages isolated from the saline-exposed groups. Both TNF-α and IL-6 levels measured in the supernatants of these bacteria-stimulated macrophages were reduced by 21% and 26%, respectively, at this early time point (p < 0.05). Longer exposure to the bacteria was not measured due to overproliferation of bacteria in the culture dishes.
Table 1.
Cytokine Production of E. Coli–Stimulated Alveolar Macrophages
| Treatmenta | Cytokine concentration (pg/mL) |
|---|---|
| TNF-α | |
| Saline | 1089.1 ± 49.4 |
| Ethanol | 859.1 ± 61.9* |
| IL-6 | |
| Saline | 226.1 ± 46.8 |
| Ethanol | 168.0 ± 12.5* |
Alveolar macrophages obtained from mice after 3 h of 2.9 g/kg ethanol or saline exposure. Cells were stimulated with 10 E. coli per cell for 3 h in vitro. Supernatants were collected and measured for TNF-α and IL-6 by ELISA. Data are shown as mean ± SEM. N = 3–4 animals. *p < 0.05 from saline control group.
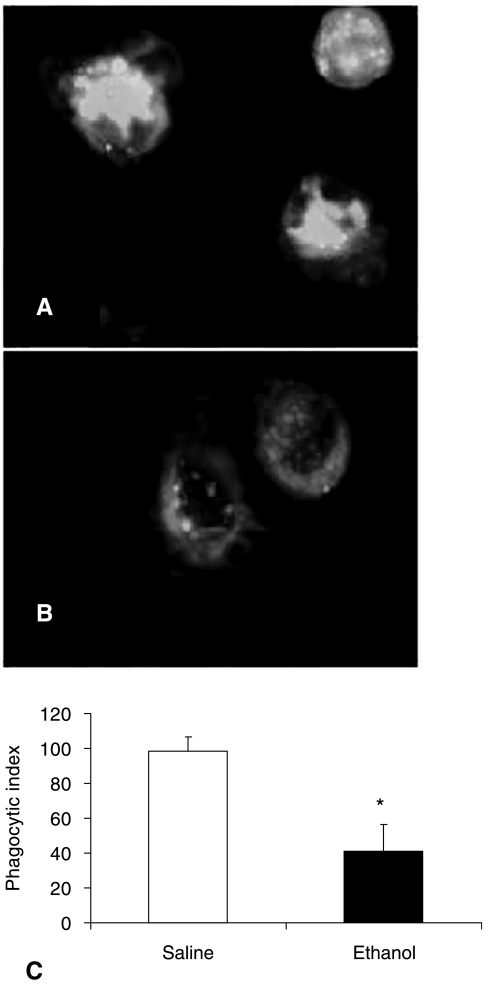
Acute ethanol exposure suppresses alveolar macrophage phagocytosis
To examine whether functions other than cytokine production are suppressed in alveolar macrophages from animals exposed to ethanol, the ability of these cells to phagocytose P. aeruginosa in vitro after in vivo ethanol exposure was measured. We decided to use P. aeruginosa because it is one of the most common gram-negative bacterial infections occurring in the lungs of immunocompromised subjects (Fagon and others 1996; Gaynes and others 1996). Three hours after mice were exposed to 2.9 g/kg ethanol, BAL was performed to obtain alveolar macrophages. The cells were cultured with EGFP–P. aeruginosa for 30 min, and phagocytosis was assessed. Twenty bacteria per cell were incubated with alveolar macrophages for 30 min, and were then fixed and stained with rhodamine phalloidin to observe cytoskeletal composition. Fluorescent microscopy shows the EGFP–P. aeruginosa (green) with actin staining of the macrophage with rhodamine phalloidin (red) (Fig. 4A and B). The alveolar macrophages isolated from the saline-treated mice showed fluorescence throughout the bulk of the cytoplasm, except in regions where the nucleus would be (shaded regions in cell). In contrast, alveolar macrophages from ethanol-treated mice showed diffuse bacterial fluorescence in the cytoplasm, compared to the saline-treated group.
FIG. 4.
Phagocytosis of enhanced green fluorescent protein (EGFP)–P. aeruginosa by alveolar macrophages was measured using fluorescence microscopy. Alveolar macrophages were incubated with EGFP–P. aeruginosa for 30 min after they were isolated from saline-treated or ethanol-treated (2.9 g/kg) mice. Cells were fixed, and the fluorescent intensity of EGFP–P. aeruginosa (green) was used to calculate phagocytosis after staining with rhodamine phalloidin (red). Figure shows representative images of alveolar macrophages isolated from (A) saline-treated and (B) ethanol-treated mice. Phagocytic index of alveolar macrophages isolated from (C) mice treated with saline or ethanol. Data are shown as mean ± SEM. N = 3–4 animals. *p < 0.05 from saline control group.
Quantification of phagocytosis was determined by calculating the phagocytic index (Fig. 4C). The phagocytic index is the product of the mean fluorescent intensity of the macrophages with EGFP–P. aeruginosa multiplied by the percent of macrophages phagocytosing bacteria. Alveolar macrophages isolated from ethanol-treated mice exhibited a 58% decrease in phagocytic index (p < 0.05), compared to macrophages isolated from saline-treated mice. It is important to note that the differences observed in the phagocytic index were due to differences in the mean fluorescent intensity, not the percent of cells phagocytosing bacteria. Alveolar macrophages isolated from either saline- or ethanol-treated mice had a phagocytosis rate of about 60% of the total population of the macrophages isolated. The variance was observed in the mean fluorescent intensity, which was calculated by using AxioVision Rel. 4.5 program.
Discussion
Many risk factors are involved after acute and chronic alcohol consumption, affecting numerous host systems, including the nervous, cardiovascular, and immune systems (Ponnappa and Rubin 2000; Haddad 2004). Typically, acute ethanol exposure is associated with attenuation or dampening of the inflammatory response. Studies have shown decreases in the production of TNF-α, IL-1β, and IL-6 by cells, including, but not limited to, neutrophils and macrophages, after in vivo or in vitro ethanol exposure (Nelson and others 1989b; Verma and others 1993; Szabo and others 1996; Szabo 1998; Boe and others 2001; Goral and others 2004; Goral and Kovacs 2005). Some attribute these effects to alterations in the integrity of cellular membranes, specifically due to increased fluidity (Peters and Preedy 1998). Membrane alteration can influence lipid raft stability, which are known to be involved in cell signaling (Simons and Toomre 2000; Pike 2003). In response to alterations in membrane and lipid raft fluidity, the downstream pathways associated with receptors on the plasma membrane may be compromised. Examples are the TLRs and their downstream signaling molecules such as the MAP kinases (Boe and others 2001). Acute ethanol exposure has been associated with decreased activation of both p38 and ERK1/2 after TLR activation (Goral and others 2004; Goral and Kovacs 2005). The authors of those studies suggested that the reduced activation of MAP kinases may result from ethanol-mediated effects on phosphatase regulation. Other studies examining the effect of chronic alcohol exposure, including the work of Guidot and co-workers, suggest that interactions between ethanol and PU.1, the master regulator for Granulocyte-macrophage colony-stimulating factor (GM-CSF), can have widespread effects on macrophage maturation and function (Joshi and others 2005). It is important to note that using an acute ethanol model, such as ours, only models a single episode of binge drinking in humans, and may not always mirror the immune deficiencies seen in chronic exposure models. In the lungs, however, TNF-α is suppressed in both the acute and chronic models of ethanol exposure, and data from the studies by Guidot and co-workers do parallel our observations.
These studies confirm the previous work of others as well as our previous observations demonstrating an ethanol-mediated attenuation of the production of proinflammatory cytokines (Szabo 1999; Nelson and Kolls 2002; Goral and others 2004; Goral and Kovacs 2005). This observation is consistent between species (human and rodent), the differentiation status of the cells (splenic or alveolar macrophages, dendritic cells, and blood monocytes), and whether ethanol was administered in vivo or in vitro. It is also important to note that both the moderate and high dose of ethanol showed lasting effects on macrophages after ethanol returned to baseline levels. The lasting inhibition was observed with all the cytokines measured, and has implications that there may be some intrinsic modifications that ethanol is having with the cell, as opposed to direct effects via interactions from circulating ethanol. Ethanol has been shown to alter genomic regulation and processing such as modifying histone acetylation and DNA methylation (Aroor and Shukla 2004; Seitz and Stickel 2007), and may be reasons of prolonged dampening of macrophage function seen after ethanol exposure.
Production of IL-12 in response to LPS, on the other hand, was not altered by the lower dose of ethanol at any time point examined, but was decreased at 6 h after animals were given the higher dose. This is consistent with Pruett et al. (2005) who showed that 24-h in vitro ethanol decreases IL-12 in peritoneal macrophages. These data may suggest that exposure to different levels of ethanol may have variable effects on how the cell is able to respond to a PAMP. As IL-12 is not as early released as TNF-α and IL-6, one could hypothesize that the molecular defects observed after a lower dose exposure have returned to normal before IL-12 pathway activation is initiated, and that higher doses of ethanol may prolong these molecular alterations. Additionally, both TNF-α and IL-6 can upregulate IL-12 production. A reduced production of both TNF-α and IL-6 by LPS-treated macrophages, obtained from ethanol-exposed mice observed after 3 h, may insufficiently induce IL-12 production at the 6-h time point.
Acute in vivo ethanol exposure lowered ex vivo alveolar macrophage production of TNF-α and IL-6 after LPS stimulation. These data parallel the diminished cytokine release that we observed with the splenic macrophages exposed to ethanol in vivo for 3 h. Others have shown that intratracheal LPS treatment resulted in a decrease in TNF-α levels in BAL fluid after an acute exposure to ethanol (Nelson and others 1989a, 1989b; Kolls and others 1995). These studies consisted of a single 5.5 g/kg ethanol administration for 30 min followed by intratracheal LPS administration for 1 to 4 h. The ethanol dose administered was higher in those studies, but our observations parallel their results. Another study showed that ex vivo stimulation of alveolar macrophages decreased TNF-α production after ethanol exposure (D'Souza and others 1996). Ethanol administration consisted of a priming dose 175 mg/100 g of body weight, followed by a 7-h continuous intravenous infusion of 30 mg/100 g of body weight/h. Similar to the aforementioned reports, this study consisted of a higher dose of ethanol for a longer exposure but showed a similar pattern of TNF-α production by the macrophages.
Macrophage activation by bacteria can occur through multiple PRRs (Linehan and others 2000; Taylor and others 2005). Examples of PRRs that recognize bacteria include TLRs, complement receptors, and scavenger receptors. Though there are no studies linking ethanol and its potential interaction between a PRR and a PAMP, TLRs may be inhibited in their ability to colocalize with CD14, as mentioned above. In the present study, we chose to model the interaction between a pathogen and macrophages, instead of focusing on only one pathway. This interaction is a more physiologically accurate representation of infection, compared to stimulating the macrophages only with LPS. When compared with LPS treatment, ethanol suppressed E. coli stimulation of TNF-α and IL-6 production by macrophages. Though we do not have extensive evidence about the mechanism by which ethanol impairs the E. coli activation pathway, our data suggest that changes in the levels of expression of TLR or scavenger receptors can be excluded. Moreover, we cannot attribute the effects of ethanol on the induction of TNF-α production with respect to changes in the TNF-α converting enzyme (TACE). TACE normally cleaves membrane-bound TNF-α as a second mechanism of releasing TNF-α (Peschon and others 1998). Studies by Zhang et al. (2000) have shown that an increase in cell-associated TNF-α is accompanied by a decrease in secreted TNF-α after ethanol exposure, consistent with the decreased TACE activity. Though we do not have the evidence that TACE is being affected by ethanol, we observed a decrease in IL-6 production, and since alterations in TACE would not have an effect on IL-6 release, we cannot attribute the decrease in cytokine production to alterations in TACE alone. Finally, though we cannot comment on whether the mechanism of ethanol's suppression of cytokine production differs between LPS or E. coli stimulation of macrophages, we can say that at early time points, activation of other PRRs (through intact E. coli stimulation) is unable to compensate for the suppressed cytokine production seen in LPS-stimulated macrophages.
Our data noted a difference in IL-6 production in the alveolar macrophages stimulated with LPS compared to alveolar macrophages stimulated with E. coli, but not in TNF-α levels. There were higher levels of IL-6 production in LPS-stimulated macrophages compared to E. coli–stimulated macrophages, which may be explained by a couple of reasons. First, the time of exposure to bacteria is only 3 h, whereas the LPS was present in cultures for 16 h. Second, TLR4 stimulation of macrophages would result in an early TNF-α expression followed by IL-6 production (Garcia-Lazaro and others 2005; Plackett and others 2007). Therefore, measuring IL-6 after an extended stimulation by E. coli may have returned levels of this cytokine to the magnitude measured in the supernatants from LPS-stimulated macrophages.
Finally, our data show that alveolar macrophage phagocytosis is decreased after acute ethanol exposure. These data are consistent with reports showing that ethanol treatment of monocyte-derived dendritic cells results in a decrease in phagocytosis along with antigen presentation (Szabo and others 1993). Additionally, studies of rabbit alveolar macrophages cultured with high levels of ethanol (400 mg/dL) in vitro have decreased phagocytosis of latex beads by 49%, compared to control cells (Rimland and Hand 1980). The authors incubated the cells with ethanol for 3 h, and allowed phagocytosis of the beads for 30 min. Our studies complement these observations, and are the first to show that acute in vivo ethanol exposure inhibits alveolar macrophage bacterial phagocytosis. We next plan to elucidate the mechanism by which phagocytosis is decreased. One method by which ethanol exhibits its effects, and may have a role on attenuating phagocytosis, is through modification in actin organization (Sordella and Van Aelst 2006; Szabo and others 2007). Preliminary data reveal that in vivo exposure to 2.9 g/kg ethanol for 3 h yields actin reorganization to the periphery of the macrophage as well as microspike formation (J. Karavitis and E.J. Kovacs, Loyola University Medical Center, unpublished observation). Other molecules involved in actin regulation are small GTPases, such as Rho and Rac, and such molecules downstream as myosin and myosin light chain kinase (Ma and others 1999; Schaffert and others 2006; Guasch and others 2007). Decreases in small GTPases in response to ethanol exposure have been observed in other cell types such as astrocytes and hepatocytes (Schaffert and others 2006; Martinez and others 2007). The impact of altered downstream regulators of actin after ethanol exposure may explain how macrophage phagocytosis and migration is decreased. Small GTPases have also been implicated in MAP kinase activation and, therefore, can be linked to the decrease in cytokine production in macrophages after acute ethanol exposure, as observed in our study.
Taken together, these studies demonstrate that acute ethanol exposure impairs PAMP-stimulated cytokine release and phagocytosis of bacteria by macrophages. Both splenic and alveolar macrophages are inhibited, and the attenuated functions observed after ethanol treatment last after the ethanol is cleared from the circulation. This suggests multiple molecular modifications. Ultimately, the reduction in macrophage functions after ethanol exposure may result in an insufficient initial response and robust reaction of the innate immune system to pathogens after acute ethanol exposure.
Acknowledgments
We would like to thank Michelle O. Morgan for technical assistance. Thanks to Dr. Joanna Goral (Midwestern University) and the members of Loyola University Alcohol Research Program for thoughtful discussions. We are appreciative of the critical review of the manuscript by Dr. Melanie Bird. This work was supported by the National Institutes of Health R01 AA12034 (EJK), Institutional Training Grant T32 AA13527 (EJK), Illinois Excellence in Academic Medicine Grant, and Ralph and Marian C. Falk Research Trust.
References
- Aroor AR. Shukla SD. MAP kinase signaling in diverse effects of ethanol. Life Sci. 2004;74(19):2339–2364. doi: 10.1016/j.lfs.2003.11.001. [DOI] [PubMed] [Google Scholar]
- Boe DM. Nelson S. Zhang P. Bagby GJ. Acute ethanol intoxication suppresses lung chemokine production following infection with Streptococcus pneumoniae. J Infect Dis. 2001;184(9):1134–1142. doi: 10.1086/323661. [DOI] [PubMed] [Google Scholar]
- Cook RT. Alcohol abuse, alcoholism, and damage to the immune system—a review. Alcohol Clin Exp Res. 1998;22(9):1927–1942. [PubMed] [Google Scholar]
- Cook RT. Ballas ZK. Waldschmidt TJ. Vandersteen D. LaBrecque DR. Cook BL. Modulation of T-cell adhesion markers, and the CD45R and CD57 antigens in human alcoholics. Alcohol Clin Exp Res. 1995;19(3):555–563. doi: 10.1111/j.1530-0277.1995.tb01548.x. [DOI] [PubMed] [Google Scholar]
- Corinti S. Pastore S. Mascia F. Girolomoni G. Regulatory role of nitric oxide on monocyte-derived dendritic cell functions. J Interferon Cytokine Res. 2003;23(8):423–431. doi: 10.1089/107999003322277838. [DOI] [PubMed] [Google Scholar]
- D'Souza NB. Nelson S. Summer WR. Deaciuc IV. Alcohol modulates alveolar macrophage tumor necrosis factor-alpha, superoxide anion, and nitric oxide secretion in the rat. Alcohol Clin Exp Res. 1996;20(1):156–163. doi: 10.1111/j.1530-0277.1996.tb01059.x. [DOI] [PubMed] [Google Scholar]
- Deviere J. Content J. Denys C. Vandenbussche P. Schandene L. Wybran J. Dupont E. High interleukin-6 serum levels and increased production by leucocytes in alcoholic liver cirrhosis. Correlation with IgA serum levels and lymphokines production. Clin Exp Immunol. 1989;77(2):221–225. [PMC free article] [PubMed] [Google Scholar]
- Drechsler Y. Dolganiuc A. Norkina O. Romics L. Li W. Kodys K. Bach FH. Mandrekar P. Szabo G. Heme oxygenase-1 mediates the anti-inflammatory effects of acute alcohol on IL-10 induction involving p38 MAPK activation in monocytes. J Immunol. 2006;177(4):2592–2600. doi: 10.4049/jimmunol.177.4.2592. [DOI] [PubMed] [Google Scholar]
- Fagon JY. Chastre J. Domart Y. Trouillet JL. Gibert C. Mortality due to ventilator-associated pneumonia or colonization with Pseudomonas or Acinetobacter species: assessment by quantitative culture of samples obtained by a protected specimen brush. Clin Infect Dis. 1996;23(3):538–542. doi: 10.1093/clinids/23.3.538. [DOI] [PubMed] [Google Scholar]
- Faunce DE. Gregory MS. Kovacs EJ. Effects of acute ethanol exposure on cellular immune responses in a murine model of thermal injury. J Leukoc Biol. 1997;62(6):733–740. doi: 10.1002/jlb.62.6.733. [DOI] [PubMed] [Google Scholar]
- Garcia-Lazaro JF. Thieringer F. Luth S. Czochra P. Meyer E. Renteria IB. Galle PR. Lohse AW. Herkel J. Kanzler S. Hepatic over-expression of TGF-beta1 promotes LPS-induced inflammatory cytokine secretion by liver cells and endotoxemic shock. Immunol Lett. 2005;101(2):217–222. doi: 10.1016/j.imlet.2005.06.003. [DOI] [PubMed] [Google Scholar]
- Gaynes RP. Edwards JR. Jarvis WR. Culver DH. Tolson JS. Martone WJ. Nosocomial infections among neonates in high-risk nurseries in the United States. National Nosocomial Infections Surveillance System. Pediatrics. 1996;98(3 Pt 1):357–361. [PubMed] [Google Scholar]
- Germann G. Barthold U. Lefering R. Raff T. Hartmann B. The impact of risk factors and pre-existing conditions on the mortality of burn patients and the precision of predictive admission-scoring systems. Burns. 1997;23(3):195–203. doi: 10.1016/s0305-4179(96)00112-x. [DOI] [PubMed] [Google Scholar]
- Girouard L. Mandrekar P. Catalano D. Szabo G. Regulation of monocyte interleukin-12 production by acute alcohol: a role for inhibition by interleukin-10. Alcohol Clin Exp Res. 1998;22(1):211–216. [PubMed] [Google Scholar]
- Goral J. Kovacs EJ. In vivo ethanol exposure down-regulates TLR2-, TLR4-, and TLR9-mediated macrophage inflammatory response by limiting p38 and ERK1/2 activation. J Immunol. 2005;174(1):456–463. doi: 10.4049/jimmunol.174.1.456. [DOI] [PubMed] [Google Scholar]
- Goral J. Choudhry MA. Kovacs EJ. Acute ethanol exposure inhibits macrophage IL-6 production: role of p38 and ERK1/2 MAPK. J Leukoc Biol. 2004;75(3):553–559. doi: 10.1189/jlb.0703350. [DOI] [PubMed] [Google Scholar]
- Guasch RM. Blanco AM. Perez-Arago A. Minambres R. Talens-Visconti R. Peris B. Guerri C. RhoE participates in the stimulation of the inflammatory response induced by ethanol in astrocytes. Exp Cell Res. 2007;313(17):3779–3788. doi: 10.1016/j.yexcr.2007.07.018. [DOI] [PubMed] [Google Scholar]
- Haddad JJ. Alcoholism and neuro-immune-endocrine interactions: physiochemical aspects. Biochem Biophys Res Commun. 2004;323(2):361–371. doi: 10.1016/j.bbrc.2004.08.119. [DOI] [PubMed] [Google Scholar]
- Joshi PC. Applewhite L. Ritzenthaler JD. Roman J. Fernandez AL. Eaton DC. Brown LA. Guidot DM. Chronic ethanol ingestion in rats decreases granulocyte-macrophage colony-stimulating factor receptor expression and downstream signaling in the alveolar macrophage. J Immunol. 2005;175(10):6837–6845. doi: 10.4049/jimmunol.175.10.6837. [DOI] [PubMed] [Google Scholar]
- Khan KN. Yatsuhashi H. Effect of alcohol consumption on the progression of hepatitis C virus infection and risk of hepatocellular carcinoma in Japanese patients. Alcohol Alcohol. 2000;35(3):286–295. doi: 10.1093/alcalc/35.3.286. [DOI] [PubMed] [Google Scholar]
- Khoruts A. Stahnke L. McClain CJ. Logan G. Allen JI. Circulating tumor necrosis factor, interleukin-1 and interleukin-6 concentrations in chronic alcoholic patients. Hepatology. 1991;13(2):267–276. [PubMed] [Google Scholar]
- Kishore R. Hill JR. McMullen MR. Frenkel J. Nagy LE. ERK1/2 and Egr-1 contribute to increased TNF-alpha production in rat Kupffer cells after chronic ethanol feeding. Am J Physiol Gastrointest Liver Physiol. 2002;282(1):G6–G15. doi: 10.1152/ajpgi.00328.2001. [DOI] [PubMed] [Google Scholar]
- Kolls JK. Xie J. Lei D. Greenberg S. Summer WR. Nelson S. Differential effects of in vivo ethanol on LPS-induced TNF and nitric oxide production in the lung. Am J Physiol. 1995;268(6 Pt 1):L991–L998. doi: 10.1152/ajplung.1995.268.6.L991. [DOI] [PubMed] [Google Scholar]
- Linehan SA. Martinez-Pomares L. Gordon S. Macrophage lectins in host defence. Microbes Infect. 2000;2(3):279–288. doi: 10.1016/s1286-4579(00)00300-2. [DOI] [PubMed] [Google Scholar]
- Ma TY. Nguyen D. Bui V. Nguyen H. Hoa N. Ethanol modulation of intestinal epithelial tight junction barrier. Am J Physiol. 1999;276(4 Pt 1):G965–G974. doi: 10.1152/ajpgi.1999.276.4.G965. [DOI] [PubMed] [Google Scholar]
- Martinez SE. Lazaro-Dieguez F. Selva J. Calvo F. Piqueras JR. Crespo P. Claro E. Egea G. Lysophosphatidic acid rescues RhoA activation and phosphoinositides levels in astrocytes exposed to ethanol. J Neurochem. 2007;102(4):1044–1052. doi: 10.1111/j.1471-4159.2007.04581.x. [DOI] [PubMed] [Google Scholar]
- Messingham KA. Faunce DE. Kovacs EJ. Alcohol, injury, and cellular immunity. Alcohol. 2002;28(3):137–149. doi: 10.1016/s0741-8329(02)00278-1. [DOI] [PubMed] [Google Scholar]
- Messingham KA. Fontanilla CV. Colantoni A. Duffner LA. Kovacs EJ. Cellular immunity after ethanol exposure and burn injury: dose and time dependence. Alcohol. 2000;22(1):35–44. doi: 10.1016/s0741-8329(00)00100-2. [DOI] [PubMed] [Google Scholar]
- Nelson S. Kolls JK. Alcohol, host defence and society. Nat Rev Immunol. 2002;2(3):205–209. doi: 10.1038/nri744. [DOI] [PubMed] [Google Scholar]
- Nelson S. Bagby G. Summer WR. Alcohol suppresses lipopolysaccharide-induced tumor necrosis factor activity in serum and lung. Life Sci. 1989a;44(10):673–676. doi: 10.1016/0024-3205(89)90472-4. [DOI] [PubMed] [Google Scholar]
- Nelson S. Bagby GJ. Bainton BG. Summer WR. The effects of acute and chronic alcoholism on tumor necrosis factor and the inflammatory response. J Infect Dis. 1989b;160(3):422–429. doi: 10.1093/infdis/160.3.422. [DOI] [PubMed] [Google Scholar]
- Nolan JP. Alcohol as a factor in the illness of university service patients. Am J Med Sci. 1965;249:135–142. [PubMed] [Google Scholar]
- Peschon JJ. Slack JL. Reddy P. Stocking KL. Sunnarborg SW. Lee DC. Russell WE. Castner BJ. Johnson RS. Fitzner JN. Boyce RW. Nelson N. Kozlosky CJ. Wolfson MF. Rauch CT. Cerretti DP. Paxton RJ. March CJ. Black RA. An essential role for ectodomain shedding in mammalian development. Science. 1998;282(5392):1281–1284. doi: 10.1126/science.282.5392.1281. [DOI] [PubMed] [Google Scholar]
- Peters TJ. Preedy VR. Metabolic consequences of alcohol ingestion. Novartis Found Symp. 1998;216:19–24. doi: 10.1002/9780470515549.ch3. discussion 24–34. [DOI] [PubMed] [Google Scholar]
- Peterson JD. Herzenberg LA. Vasquez K. Waltenbaugh C. Glutathione levels in antigen-presenting cells modulate Th1 versus Th2 response patterns. Proc Natl Acad Sci U S A. 1998;95(6):3071–3076. doi: 10.1073/pnas.95.6.3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pike LJ. Lipid rafts: bringing order to chaos. J Lipid Res. 2003;44(4):655–667. doi: 10.1194/jlr.R200021-JLR200. [DOI] [PubMed] [Google Scholar]
- Plackett TP. Colantoni A. Heinrich SA. Messingham KA. Gamelli RL. Kovacs EJ. The early acute phase response after burn injury in mice. J Burn Care Res. 2007;28(1):167–172. doi: 10.1097/BCR.0b013E31802CB84F. [DOI] [PubMed] [Google Scholar]
- Ponnappa BC. Rubin E. Modeling alcohol's effects on organs in animal models. Alcohol Res Health. 2000;24(2):93–104. [PMC free article] [PubMed] [Google Scholar]
- Pruett SB. Fan R. Zheng Q. Schwab C. Differences in IL-10 and IL-12 production patterns and differences in the effects of acute ethanol treatment on macrophages in vivo and in vitro. Alcohol. 2005;37(1):1–8. doi: 10.1016/j.alcohol.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Rimland D. Hand WL. The effect of ethanol on adherence and phagocytosis by rabbit alveolar macrophages. J Lab Clin Med. 1980;95(6):918–926. [PubMed] [Google Scholar]
- Ruiz M. Ewig S. Torres A. Arancibia F. Marco F. Mensa J. Sanchez M. Martinez JA. Severe community-acquired pneumonia. Risk factors and follow-up epidemiology. Am J Respir Crit Care Med. 1999;160(3):923–929. doi: 10.1164/ajrccm.160.3.9901107. [DOI] [PubMed] [Google Scholar]
- Schaffert CS. Todero SL. Casey CA. Thiele GM. Sorrell MF. Tuma DJ. Chronic ethanol treatment impairs Rac and Cdc42 activation in rat hepatocytes. Alcohol Clin Exp Res. 2006;30(7):1208–1213. doi: 10.1111/j.1530-0277.2006.00135.x. [DOI] [PubMed] [Google Scholar]
- Seitz HK. Stickel F. Molecular mechanisms of alcohol-mediated carcinogenesis. Nat Rev Cancer. 2007;7(8):599–612. doi: 10.1038/nrc2191. [DOI] [PubMed] [Google Scholar]
- Simons K. Toomre D. Lipid rafts and signal transduction. Nat Rev Mol Cell Biol. 2000;1(1):31–39. doi: 10.1038/35036052. [DOI] [PubMed] [Google Scholar]
- Song K. Coleman RA. Alber C. Ballas ZK. Waldschmidt TJ. Mortari F. LaBrecque DR. Cook RT. TH1 cytokine response of CD57+ T-cell subsets in healthy controls and patients with alcoholic liver disease. Alcohol. 2001;24(3):155–167. doi: 10.1016/s0741-8329(01)00146-x. [DOI] [PubMed] [Google Scholar]
- Sordella R. Van Aelst L. Driving actin dynamics under the influence of alcohol. Cell. 2006;127(1):37–39. doi: 10.1016/j.cell.2006.09.017. [DOI] [PubMed] [Google Scholar]
- Szabo G. Monocytes, alcohol use, and altered immunity. Alcohol Clin Exp Res. 1998;22(Suppl 5):216S–219S. doi: 10.1097/00000374-199805001-00002. [DOI] [PubMed] [Google Scholar]
- Szabo G. Consequences of alcohol consumption on host defence. Alcohol Alcohol. 1999;34(6):830–841. doi: 10.1093/alcalc/34.6.830. [DOI] [PubMed] [Google Scholar]
- Szabo G. Dolganiuc A. Dai Q. Pruett SB. TLR4, ethanol, and lipid rafts: a new mechanism of ethanol action with implications for other receptor-mediated effects. J Immunol. 2007;178(3):1243–1249. doi: 10.4049/jimmunol.178.3.1243. [DOI] [PubMed] [Google Scholar]
- Szabo G. Mandrekar P. Girouard L. Catalano D. Regulation of human monocyte functions by acute ethanol treatment: decreased tumor necrosis factor-alpha, interleukin-1 beta and elevated interleukin-10, and transforming growth factor-beta production. Alcohol Clin Exp Res. 1996;20(5):900–907. doi: 10.1111/j.1530-0277.1996.tb05269.x. [DOI] [PubMed] [Google Scholar]
- Szabo G. Verma B. Catalano D. Selective inhibition of antigen-specific T lymphocyte proliferation by acute ethanol exposure: the role of impaired monocyte antigen presentation capacity and mediator production. J Leukoc Biol. 1993;54(6):534–544. doi: 10.1002/jlb.54.6.534. [DOI] [PubMed] [Google Scholar]
- Taylor PR. Martinez-Pomares L. Stacey M. Lin HH. Brown GD. Gordon S. Macrophage receptors and immune recognition. Annu Rev Immunol. 2005;23:901–944. doi: 10.1146/annurev.immunol.23.021704.115816. [DOI] [PubMed] [Google Scholar]
- Verma BK. Fogarasi M. Szabo G. Down-regulation of tumor necrosis factor alpha activity by acute ethanol treatment in human peripheral blood monocytes. J Clin Immunol. 1993;13(1):8–22. doi: 10.1007/BF00920631. [DOI] [PubMed] [Google Scholar]
- Waltenbaugh C. Peterson JD. Ethanol impairs the induction of delayed hypersensitivity in C57BL/6 mice. Alcohol. 1997;14(2):149–153. doi: 10.1016/s0741-8329(97)83137-0. [DOI] [PubMed] [Google Scholar]
- Wiese JG. Shlipak MG. Browner WS. The alcohol hangover. Ann Intern Med. 2000;132(11):897–902. doi: 10.7326/0003-4819-132-11-200006060-00008. [DOI] [PubMed] [Google Scholar]
- Zhang Z. Cork J. Ye P. Lei D. Schwarzenberger PO. Summer WR. Shellito JE. Nelson S. Kolls JK. Inhibition of TNF-alpha processing and TACE-mediated ectodomain shedding by ethanol. J Leukoc Biol. 2000;67(6):856–862. doi: 10.1002/jlb.67.6.856. [DOI] [PubMed] [Google Scholar]