Abstract
Objective
To evaluate whether student participation in ambulatory clinics influenced the percentage of therapeutic international normalized ratio (INR) results among patients on chronic warfarin therapy.
Methods
Medical records in outpatient anticoagulation clinics managed by pharmacists under physician protocol were reviewed retrospectively in 2 university-affiliated clinics in Amarillo and Lubbock, TX. Pharmacy student activities included patient interviews, vital sign measurements, fingersticks, counseling, and documentation. Patient visits were conducted by a precepted pharmacy student or a pharmacist without a student, and the INR was measured at the subsequent patient visit.
Results
Records of 1,958 anticoagulation patient visits were reviewed; 865 patients were treated by pharmacists, and 1093 were treated by precepted students. The follow-up INR was therapeutic for 48.5% of third-year (P3) students' patients, 45.6% of fourth-year (P4) students' patients, 51.2% of residents' patients, and 44.7% of pharmacists's patients (p = 0.23). Eight variables were associated with the follow-up INR (baseline INR, warfarin noncompliance, held warfarin doses, a warfarin dosage adjustment, diet change, alcohol use, tobacco use, and any medication changes).
Conclusion
Student participation in the patient-care process did not compromise patient care and no significant difference in patient outcomes was found between patients in an anticoagulation clinic cared for by precepted students and those cared for by pharmacists.
Keywords: student, pharmacist, anticoagulation clinic, international normalized ratio, warfarin, practice experience
INTRODUCTION
Pharmacy education is structured to ensure that students are exposed to all aspects of patient care. At an early point in most programs, students are taught basic patient-care skills that are reinforced through classroom or laboratory activities. In the latter portion of all programs, students participate in experiential practice, which is designed to allow students to participate actively in providing patient care.1 Because pharmacists and pharmacy students participate in a variety of patient-care activities in various settings, they more readily become integral members of the healthcare team responsible for the provision of patient care services.
Colleges and schools of pharmacy and other health care institutions collaborate to provide quality educational experiences to students. Experiential practice should enable students to achieve professional competencies without compromising quality patient care, patient safety, or patient outcomes. Several papers have described the types of clinical services provided by pharmacy students during experiential courses.2-7 However, the impact of these student interventions is limited in terms of objectively measured patient outcomes. Therefore, members of the primary care faculty division from Texas Tech Health Sciences Center (TTUHSC) School of Pharmacy developed a project to evaluate the effect of precepted student participation in ambulatory care clinics on the percentage of therapeutic INR results among patients on chronic warfarin therapy.
Clerkship Program
At TTUHSC, doctor of pharmacy (PharmD) candidates are required to participate in 5 introductory practice experiences in the first through third years, and 8 six-week advanced practice experiences in the fourth year. Students complete the first 2 years of the program on either of the main campuses (Amarillo or Abilene, TX). The third and fourth years may be completed on either of the main campuses or at a satellite campus (Dallas/Fort Worth or Lubbock, TX).
The data was collected from pharmacist-run anticoagulation service patient visits in 2 university- affiliated internal medicine clinics. In both clinics the pharmacists managed anticoagulation therapy under a collaborative practice agreement with supervising physicians. The clinic in Amarillo, TX, had approximately 48 to 60 patient visits dispersed over 4 half-day clinics per week. The Lubbock, TX, clinic had approximately 40 to 50 patient visits spread over 3 half-day clinics per week. In both clinics, patients were referred initially to the clinic by physicians.
During the course of P3 and P4 students' clerkships, students were continually under the supervision of a licensed pharmacist. At the beginning of the practice experience the students were trained in patient interview techniques and the workflow of the clinic. At the beginning of the practice experience the students shadowed clinical pharmacists to become familiar with the patient interview and documentation process. Based on the syllabi of the TTUHSC practice experience courses, different expectations existed for student performance, depending on their location in the PharmD program.
The P3 practice experience focused primarily on the skills associated with clinical visits, including interview skills, visit documentation, limited physical assessment, and the ability to make clinical decisions pertaining to a straightforward clinic patient. The P4 advanced practice experience expectations included those of the P3 year experience in addition to the expectation that the P4 pharmacy students were able to make clinical decisions pertaining to the care of complex patients as well.
Initially, students observed a pharmacist-managed patient visit, then the students were observed performing the visit, and eventually the students conducted patient visits and developed drug therapy management plans with the supervision and collaboration of a licensed pharmacist. All students presented their interview findings and initial plan to the preceptor, then together the final decision about patient care was made, and the students implemented the plan with the patient.
As with any clerkship experience, students progressed at their own pace and required differing levels of intervention and prompting from their preceptor. During this study all clinical pharmacists precepted their students in a similar manner.
METHODS
This study was reviewed and approved by the TTUHSC Institutional Review Board. A retrospective, cohort design was used to examine medical records in outpatient anticoagulation clinics managed by pharmacists under physician protocol. All data was deidentified and collected using a standardized data collection sheet.
The study sites included 2 university-affiliated clinics in Amarillo and Lubbock, TX. Medical records were identified through a list of patients followed by a pharmacist anticoagulation service. Patient inclusion criteria included age greater than 18 years and longitudinal follow-up for anticoagulation therapy of more than 3 months. P3 and P4 students in the PharmD program were precepted frequently at both sites. The roles of precepted students in these clinics included interviewing the patient, measuring vital signs, performing a fingerstick coagulation test, communicating the results and instructions to the patient, and documenting the visit in the medical record.
The primary independent variable was whether the patient visit was conducted by a precepted student or a pharmacist. All pharmacists also served as preceptors for the precepted pharmacy students. The primary dependent variable was the INR result at the subsequent patient visit. Other study variables included patient age, sex, indication for warfarin, goal INR, medication noncompliance, new prescription or nonprescription medications, dietary vitamin K intake, alcohol and tobacco use, and hemorrhagic or thromboembolic events. The primary outcome compared the percentage of INR results that were within the target range after a visit was conducted by a precepted student and after a visit was conducted by a pharmacist. The target sample size was determined to be 1,550 patient visits in each group, based on a 5% change in the rate of therapeutic INR values, a 2-tailed hypothesis test, alpha less than 0.05, and a desired power ≥ 80%.
RESULTS
On each follow-up visit to the anticoagulation clinic, the patient's INR was measured and compared to the goal INR for the visit. INR outcomes were defined as therapeutic if the follow-up INR fell within ± 0.5 of the goal INR. Thus, for each patient visit, the patient was assessed as having achieved or not achieved a therapeutic INR.
To compare the performance of precepted students versus pharmacists relative to patient outcomes, the percentage of patients achieving therapeutic INR were compared. Of the 1958 patient visits, 865 were treated by pharmacists only and 1093 were treated by precepted students. Four hundred (46.2%) cases managed by pharmacists only had therapeutic INRs, while 507 (46.4%) cases managed by precepted students had therapeutic INRs. The percentage of patients with therapeutic INRs did not differ significantly between pharmacists and precepted students (chi-square = 0.004, p = 0.950), suggesting that the pharmacists' performance and precepted students' performance were roughly equivalent.
To further assess the impact of type of provider (precepted student vs. pharmacist), provider type was stratified into multiple categories (P3 student, P4 student, resident, and pharmacist). Therapeutic INR outcomes by provider type were 48.5% for P3 students, 45.6% for P4 students, 51.2% for residents, and 44.7% for pharmacists. These percentages did not differ significantly (p = 0.23), confirming that pharmacists' and precepted students' performances were roughly equivalent, even across education categories.
For each patient visit, the difference between goal INR and observed INR was calculated. The absolute value of this difference was then calculated to characterize how far the observed INR was from the goal (as measured in INR units). For the 865 pharmacist-managed visits, the difference in achieved and goal INR was 0.760 ± 0.765 (mean ± SD). For the 1093 precepted student-managed visits, the difference in achieved and goal INR was 0.722 ± 0.704. The mean difference in achieved and goal INR was not significant between precepted student-managed and pharmacist-managed cases (p = 0.256), providing further confirmation that pharmacists' and precepted students' performance was equivalent. Performing a similar analysis with provider type stratified into multiple categories (P3 student, P4 student, resident, pharmacist), a 1-way analysis of variance confirmed that performance among the 4 provider groups did not differ significantly (p = 0.087).
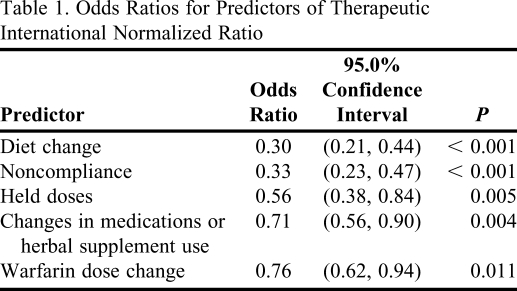
Logistic regression was used to predict the dichotomous outcome (success versus failure) of patients achieving therapeutic INR at follow-up visits. Independent variables (predictors) included provider type (student versus pharmacist) and 8 potential risk factors. The risk factors were baseline INR, warfarin dose change from initial visit, noncompliance, held doses, diet change from initial visit, change in medications or herbal supplements from initial visit, alcohol use, and tobacco use. A principal finding from the initial multivariate model with the 9 predictor variables was that provider type (precepted student versus pharmacist) was not significant after controlling for the effects of covariates. After excluding nonsignificant predictors from the multivariate model, a refined logistic regression model with the 5 significant risk factors was developed. Odds ratios, 95% confidence intervals, and significance are depicted in Table 1. All of the odds ratios for the 5 predictors were < 1, indicating that the odds of a patient achieving therapeutic INR at follow-up was reduced for each of the 5 risk factors. The predictor variables with the smallest odds ratios had the greatest potential to reduce the odds of achieving therapeutic INR at follow-up. Thus, diet change and noncompliance were the 2 predictors that most lowered the odds of achieving therapeutic INR outcomes.
Table 1.
Odds Ratios for Predictors of Therapeutic International Normalized Ratio
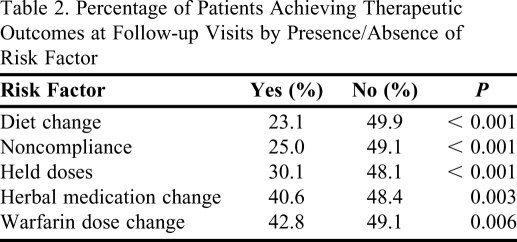
The percentage of patients who achieved therapeutic INR outcomes at follow-up visits based upon the presence/absence of 5 risk factors are identified in Table 2. Only 25% of noncompliant patients achieved therapeutic INR outcomes at follow-up visits, while 49% of compliant patients achieved therapeutic outcomes. Similarly, only 23% of the patients who had a diet change achieved a therapeutic INR outcome, while 50% of those without the risk factor achieved a therapeutic INR outcome. For each of the 5 risk factors, patients with the risk factor were less likely to achieve therapeutic INR than those without the risk factors.
Table 2.
Percentage of Patients Achieving Therapeutic Outcomes at Follow-up Visits by Presence/Absence of Risk Factor
DISCUSSION
To our knowledge, this was the first study to evaluate the impact of precepted pharmacy students on patient care compared with pharmacists in an outpatient anticoagulation setting. All PharmD programs around the nation include an experiential learning component. This learning provided at experiential practice sites allows improved clinical skills for pharmacy students. Furthermore, this effectively prepares students to practice pharmacy independently. While pharmacy students may benefit from experiential learning, it is imperative that patient care is not compromised during the learning experience. Therefore, the purpose of this study was to assess the performance of precepted P3 and P4 students versus that of pharmacists relative to patient outcomes specifically in the anticoagulation clinic setting.
Precepted pharmacy students in this study performed all clinical actions similar to a pharmacist participating in an anticoagulation clinic. They initially interviewed the patient to gather subjective information. Next, they checked Prothrombin time and INR laboratory tests using a point-of-care device. Subsequently, they made appropriate drug-related assessments and treatment plans which were communicated to the patient. Last they documented all of the findings and provided applicable counseling as needed.
Student participation in the patient care process in the anticoagulation setting was not associated with a difference in patient outcomes. Students independently performed tasks such as subjective interviews, and obtained objective information through performance of a fingerstick coagulation test. Although the process of care was different among precepted student-led visits and pharmacist-led visits, as students had a certain degree of autonomy in clinic, the percentage of patients achieving therapeutic INR and differences between goal INR and observed INR for patients were similar for patients seen by a precepted student or pharmacist. This lack of difference in patient outcomes may be due to timely identification and correction by the pharmacist of any precepted student deficits in communication, objective testing, assessment, clinical decision-making, and counseling skills. Therefore, P3 and P4 student performance in experiential learning sessions allowed student learning without compromising patient care. The results of this study help ensure the value of including experiential learning at different stages in the PharmD program. Experiential learning gives students an opportunity to learn and refine pharmacy practice skills in a variety of settings. In an ambulatory care setting, students learn communication, physical assessment, clinical decision-making, and counseling skills. Development of these skills contributes to optimal drug therapy management and patient interactions.
Several risk factors may increase the likelihood of a patient's INR outcomes being non-therapeutic. Of all the risk factors we identified to affect INR outcomes, the 2 risk factors with the most pronounced effect on INR outcomes were medication noncompliance and diet changes. Improving patient compliance with warfarin doses and a steady vitamin K diet may improve the quality of anticoagulation care significantly. This study was conducted at 2 sites within the TTUHSC system. As additional anticoagulation clinics are developed for Texas Tech School of Pharmacy students during their experiential learning experience, future plans include the addition of data from more sites.
A limitation of this study was the retrospective, chart-review design. As this is not a causal design, the study is limited to the available data, and charts may be incomplete or have errors. Another limitation of this study is the limited sample size of patients. Due to the restricted availability of data at our clinic sites, the study did not achieve the desired power. However, the sample size of 1,958 patients was relatively large. Further studies should be conducted to validate our findings.
CONCLUSIONS
Anticoagulation control among patients who received care from precepted pharmacy students was not significantly different than that among patients seen by a pharmacist. Involvement of pharmacy students in an ambulatory care experiential course did not compromise the quality of patient care in this study.
REFERENCES
- 1.Handbook on Outcomes Assessment. Alexandria, VA: American Association of Colleges of Pharmacy; 1995. AACP Resource Notebook for Implementing Curricular Change. [Google Scholar]
- 2.Taylor CT, Church CO, Byrd DC. Documentation of clinical interventions by pharmacy faculty, residents, and students. Ann Pharmacother. 2000;34(7):843–847. doi: 10.1345/aph.19310. [DOI] [PubMed] [Google Scholar]
- 3.Slaughter RL, Erickson SR, Thomson PA. Clinical interventions provided by doctor of pharmacy students. Ann Pharmacother. 1994;28(5):665–670. doi: 10.1177/106002809402800519. [DOI] [PubMed] [Google Scholar]
- 4.Briceland LL, Kane MP, Hamilton RA. Evaluation of patient-care interventions by PharmD clerkship students. Am J Hosp Pharm. 1992;49(5):1130–1132. [PubMed] [Google Scholar]
- 5.Brockmiller H, Abel SR, Koh-Knox CP, Birk CW. Cost impact of PharmD candidates' drug therapy recommendations. Am J Health-Syst Pharm. 1999;56(9):882–884. doi: 10.1093/ajhp/56.9.882. [DOI] [PubMed] [Google Scholar]
- 6.Condren ME, Haase MR, Luedtke SA, Gaylor AS. Clinical activities of an academic pediatric pharmacy team. Ann Pharmacother. 2004;38(4):574–578. doi: 10.1345/aph.1D384. [DOI] [PubMed] [Google Scholar]
- 7.Mueller BA, Abel SR. Impact of college of pharmacy-based educational services within the hospital. DICP. 1990;24(4):422–425. doi: 10.1177/106002809002400416. [DOI] [PubMed] [Google Scholar]