Abstract
Objective
To enhance student learning of a complex therapeutic concept through the incorporation of 2 case-based, active-learning strategies with lecture in a required advanced therapeutics course.
Design
A virtual patient session using a branched-outcome decision-making model and a problem-based learning (PBL) practica were developed from the course learning objectives for severe sepsis and septic shock. Following lecture of this material, students were required to complete the simulation session and attend the PBL.
Assessment
Student learning was assessed through review of examination scores, as well as quality and accuracy of the pharmaceutical care plan developed as part of the PBL. Satisfaction of the teaching format was assessed through a course evaluation survey. For questions pertaining to sepsis or septic shock on the final examination, the class average was 90%, despite an average of 76% on the examination as a whole. Class average for the pharmacuetical care plan was 90%. Sixty-three percent of students stated the simulation contributed to their learning, and 93% stated the PBL contributed to their learning.
Conclusion
Using a multifaceted teaching approach, combining active- and passive-learning strategies, was well received by students and fostered an effective learning environment.
Keywords: active learning, virtual patient, simulation, problem-based learning, clinical decision making
INTRODUCTION
The teaching of complex therapeutic concepts can be challenging in pharmacy education. With a majority of pharmacists practicing in community pharmacy settings,1 class time devoted to advanced topics within a pharmacy curriculum is often nominal. In addition, students may view such concepts as inconsequential to their career objectives.
However, as is the case with severe sepsis and septic shock (estimated mortality of 30%, affecting millions worldwide each year2,3), pharmacists can and do play a pivotal role in direct patient care and medication therapy management. A study of critically ill patients with nosocomial infections, community-acquired infections, and sepsis found that the involvement of a clinical pharmacist in their care was associated with a highly significant reduction in patient mortality, length of stay, and costs of care.4
The Center for the Advancement of Pharmaceutical Education (CAPE) Outcomes5 and Accreditation Council for Pharmacy Education (ACPE) Accreditation Standards and Guidelines6 stress the importance of graduating pharmacy students with competence in providing independent, patient-centered, evidence-based pharmaceutical care. In order to accomplish this, pharmacy faculty are encouraged to develop innovative teaching methods through the application of computer and other instructional technologies, as well as by promoting active-learning strategies to develop critical-thinking and problem-solving skills.
This manuscript details the design and assessment of an innovative course delivery format, integrating 2 case-based, active-learning strategies with lecture in a required advanced therapeutics course. The goal of this multifaceted teaching approach was to improve student learning of complex therapeutic concepts. The course put great emphasis on computer-assisted learning (CAL), virtual patient technology, branched-outcome decision making, guided group discussion, and lecture to stimulate critical thinking, development of knowledge and skills, patient assessment, pharmaceutical care plan development, and life-long learning.
In this manuscript, severe sepsis and septic shock will represent “complex clinical concepts” in which course teaching methods were applied. However, any therapeutic topic could be applied to this model.
DESIGN
In 2009, a virtual patient simulation program, vpSim (Decision Simulation), and PBL practica involving severe sepsis and septic shock were incorporated into Advanced Pharmaceutical Care II, a 2-credit required course taken in the spring semester of the third year. The course provides students with an understanding and appreciation of the challenges in delivering pharmaceutical care to critically ill patients, as well as those with kidney disease. Didactic sessions were used to introduce concepts and principles, and then students were expected to apply their knowledge and skills through a variety of activities, including the PBL and virtual patient sessions, discussion boards, examinations, and a comprehensive capstone case.
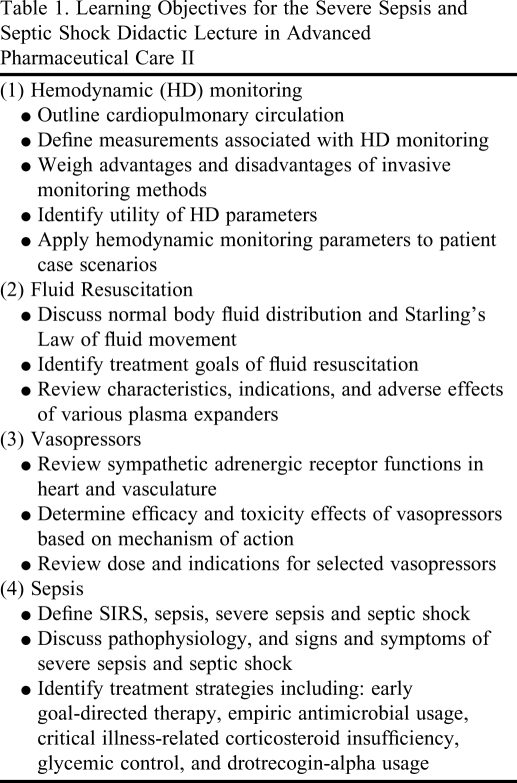
Embedded in this course was a 2-hour severe sepsis and septic shock lecture highlighting core concepts and principles needed to gain a fundamental understanding of the subject. Topics included in the lecture were cardiopulmonary hemodynamic monitoring, fluid resuscitation, use of vasopressors, early goal-directed therapy in sepsis, empiric antibiotic coverage, critical illness-related corticosteroid insufficiency, glycemic goals, and drotrecogin-alpha usage. Learning objectives for this lecture are presented in Table 1.
Table 1.
Learning Objectives for the Severe Sepsis and Septic Shock Didactic Lecture in Advanced Pharmaceutical Care II
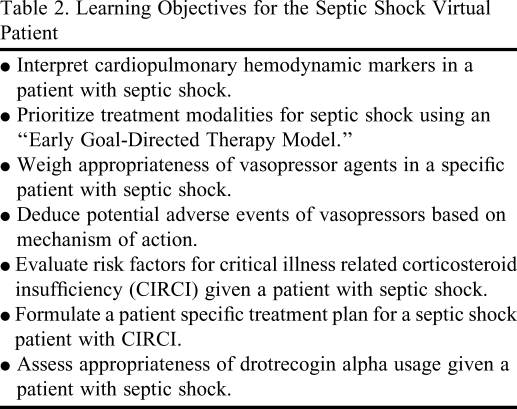
The sepsis vpSim was created to provide students practice at applying the learning objectives encountered in the lecture. Learning objectives for this simulation reflected this goal and can be found in Table 2.
Table 2.
Learning Objectives for the Septic Shock Virtual Patient
Virtual patients have been defined as computer programs that simulate lifelike clinical scenarios in which the learner becomes the health care professional making therapeutic decisions.7 This technology was first published in the medical literature,8 but has been described in the training of medical, nursing, dental, and other health professionals.9 Advantages to virtual patient technology include allowing educators to assess application of course content in a “safe” environment, while allowing students to both learn and err in private.10
vpSim is distinct from most other virtual simulations because of its branched-outcome decision-making model from which sessions are built. In this model, learners are presented with a challenge, given choices, and then provided with a consequence specific to their choice. Application of this “branching” model allowed students to encounter a patient problem, choose a recommendation that they believed to be the most correct, and then receive an outcome directly related to their choice. Success through the simulation, therefore, was defined by the student's own recommendations in that every possible recommendation in vpSim was linked with a distinct “branch” or path in the session.
Branching within the simulation eventually terminates at a session endpoint. Endpoints can reflect positive or negative patient outcomes that likely would have resulted from the collective decisions made by the student. These collective decisions form the student's learning path, a term that represents the route a student has taken to complete the simulation. The learning path, therefore, is the culmination of recommendations a student has made in reaching the endpoint.
In the sepsis vpSim, all patient problems or challenges originated from a faculty-designed patient case, which was viewed online by students prior to simulation commencement. Individually, students encountered clinical questions or scenarios based on this case and were asked to choose appropriate recommendations. The students' decisions led to specific consequences (positive and negative) to their virtual patient. At the conclusion of the session, patient endpoints were provided to the students reflecting the culmination of their decisions throughout the session.
Students were given 1 week to complete the sepsis vpSim, which was activated immediately after completion of the severe sepsis and septic shock lecture. Students were required to complete the simulation, but were not given a specific “grade” on their success. However, formative feedback was provided throughout the session involving the appropriateness of each decision made along an individual student's learning path. Feedback reinforced good recommendations and corrected bad ones. This combination of application and feedback gave students the opportunity to practice clinical decision making in a realistic but protected environment.
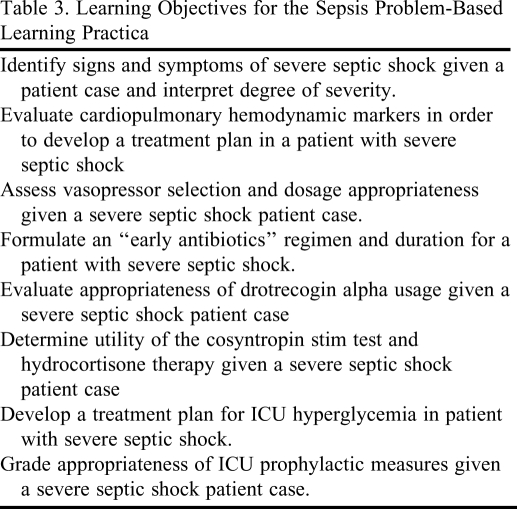
The second case-based, active-learning strategy used in the Advanced Pharmaceutical Care II course was the sepsis PBL practica. The practica followed both the lecture and simulation session. Learning objectives from the severe sepsis and septic shock lecture (Table 1) were again used to develop the PBL's learning objectives (Table 3). The goal of this PBL was to allow further application of the didactic course content.
Table 3.
Learning Objectives for the Sepsis Problem-Based Learning Practica
Problem-based learning practica employ small interactive student groups (6-8 students) and a faculty facilitator. The goal of a PBL session is not to identify a single solution to a case-based scenario, but to identify several potential solutions and to understand how the solutions were generated. Key characteristics of PBL sessions have been published.11
In PBL sessions, students are active participants as they recognize learning deficits, seek new knowledge, apply new knowledge across varying landscapes, formulate plans, and determine the plan's parameters of success or failure. This teaching method allows students to actively learn from each other and independent study.
In contrast, a PBL facilitator has a passive role. Facilitators act as guides to encourage participation and discussion, promote positive dialogue, raise questions that lead students to make “connections,” maintain the PBL format, reduce “side-tracking,” and manage time. Facilitator roles are quite opposite to traditional instructor roles; content “expertise” is not a requirement.
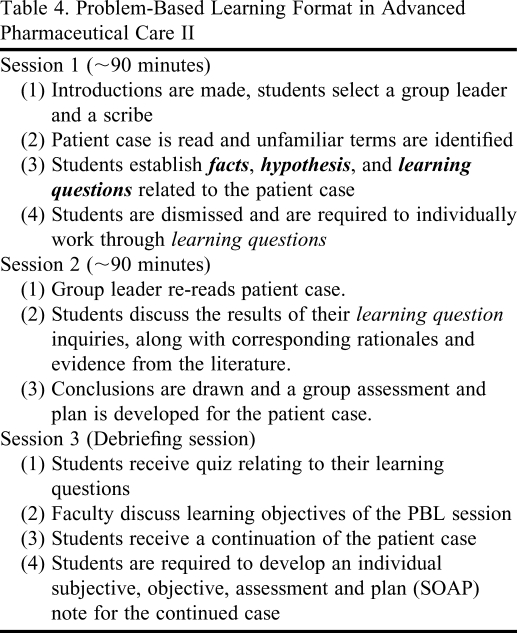
With regards to the sepsis PBL, 3 interactive practica sessions were held (Table 4). In these sessions, students worked collaboratively with each other and faculty members to develop facts, hypothesis, and learning questions for a patient case. Following each session, students were required to independently answer the “learning questions” prior to the next session. Following the final PBL practica, students were required to write an individual clinical note that incorporated subjective and objective patient data, an assessment, and a plan (SOAP note). Both formative and summative feedback on their SOAP note was provided to the students.
Table 4.
Problem-Based Learning Format in Advanced Pharmaceutical Care II
EVALUATION AND ASSESSMENT
For the 107 students enrolled in Advanced Pharmaceutical Care II course, learning assessments for material taught in the severe sepsis and septic shock lecture were made through review of PBL SOAP note and examination scores. Using a grading rubric, individual SOAP notes were evaluated on the following criteria: subjective and objective information; problem list completeness; problem ranking; plan development for each problem including drug, dose, route, frequency, duration, monitoring and goals; and note clarity, legibility, and conciseness. Scores ranged from 78% to 99%, with an average of 90%. Fifty-eight percent of the class scored 90% or greater on their SOAP notes.
The cumulative examination for the critical care component of the course consisted of 50 multiple-choice and case-based questions. Topics included intensive care unit (ICU) prophylaxis, analgesia, sedation, delirium, alcohol withdrawal, ICU hyperglycemia, pulmonary arterial hypertension, postoperative nausea and vomiting, anesthetics, and neuromuscular blockade, as well as sepsis. Of the 50 examination questions, 12 were dedicated to the material taught during the severe sepsis and septic shock lecture. The average class score on the entire examination was 76%. Scores on the 12 questions involving sepsis ranged from 53%-97% with a class average of 87%.
In the scheduled, end of course evaluation survey, 98% of students felt they were intellectually challenged in this course. Seventy-one percent and 81% of students believed that learning objectives were covered in the simulation and PBL practica, respectively. Sixty-three percent of students stated that the simulation session contributed to their learning, while 93% stated this for the PBL. Nearly all students enjoyed the simulation (85%) and PBL sessions (95%).
DISCUSSION
Active-learning theory is an essential ingredient of all pharmacy curricula. Students often underestimate the need to go beyond superficial recall and strategic learning of core fundamentals with passive learning (ie, lecture) alone. Hands-on training experiences are necessary to move students into deeper levels of learning (ie, learning to understand) by affording them practice at the application of the basic skills and knowledge necessary for provision of independent patient care as it relates to curricular material.
The goal of this course design was to improve student learning of complex concepts such as sepsis and septic shock through a multifaceted teaching approach that integrated active and passive learning. The course allowed students to learn basic knowledge and skills in a familiar format, namely through lectures. Students could then practice using their skills and knowledge in realistic but controlled environments with the virtual patients and PBL practica. Simulation and PBL sessions granted students independent, repetitive training in the design, implementation, monitoring, and evaluation of clinical recommendations specific for the septic patient. In turn, faculty members were granted the opportunity to standardize learning and assess comprehension of course content in legitimate settings, without risk of harm to patients or students.
Student scores on PBL SOAP notes were remarkably high, indicating comprehension of core material and an understanding of sepsis fundamentals. In addition, students scored well on the cumulative final examination for those questions involving sepsis, despite overall scores being average at best. This can most likely be attributed to the “hands on” application of this material in the simulation and PBL sessions.
Based on students' overwhelmingly positive responses on course evaluation surveys, they not only enjoyed but also appreciated the active-learning strategies used in this course. Numerous obstacles were encountered in implementing the PBL practica, including considerable faculty time commitments for facilitation, case development, and grading. Obstacles also were encountered with implementation of the patient simulation using vpSim, including extensive case and simulation development time (3-4 weeks per simulation). Despite these obstacles, course faculty members considered the course teaching design a success. As a result, the Advanced Pharmaceutical Care II course was expanded and additional complex topics (ie, sedation, analgesia, ICU prophylaxis, etc) have been incorporated into the PBL and virtual patient sessions. Our course now supports 8 virtual patient tutorials and 2 PBL workshops consisting of 3 practica sessions each.
SUMMARY
A multifaceted teaching approach was implemented in an advanced therapeutics course to improve student learning of complex therapeutic concepts such as severe sepsis and septic shock. Active-learning strategies using virtual patient technology with branched-outcome decision making capabilities and PBL practica were integrated to augment lectures. Based on student learning assessments and course survey evaluations, the course was not only well received by students, but also fostered an effective learning environment.
REFERENCES
- 1. 2009 National Pharmacist Workforce Survey – 2009, accessible at: http://www.aacp.org/resources/research/pharmacymanpower/Documents/2009%20National%20Pharmacist%20Workforce%20Survey%20-%20FINAL%20REPORT.pdf Accessed July 21, 2010.
- 2.Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. Crit Care Med. 2008;36(1):296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 3.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 4.MacLaren R, Bond CA, Martin S, Fike D. Clinical and economic outcomes of involving pharmacists in the direct care of critically ill patients with infection. Crit Care Med. 2008;36(12):3184–3189. doi: 10.1097/CCM.0b013e31818f2269. [DOI] [PubMed] [Google Scholar]
- 5. Center for the Advancement of Pharmaceutical Education (CAPE) Educational Outcomes 2004. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf Accessed July 21, 2010.
- 6. Accreditation Council for Pharmacy Education. Accreditation Standards. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed July 21, 2010.
- 7.Huang G, Reynolds R, Candler C. Virtual patient simulation at US and Canadian medical schools. Acad Med. 2007;82(5):446–451. doi: 10.1097/ACM.0b013e31803e8a0a. [DOI] [PubMed] [Google Scholar]
- 8.Harless W, Drennon G, Marxer J, Root J, Miller G. CASE: a computer-aided simulation of the clinical encounter. J Med Educ. 1971;46(5):443–8. [PubMed] [Google Scholar]
- 9.Cook D, Triola M. Virtual patients: a critical literature review and proposed next steps. Med Educ. 2009;43:303–311. doi: 10.1111/j.1365-2923.2008.03286.x. [DOI] [PubMed] [Google Scholar]
- 10.Tworek J, Coderre S, Wright B, McLaughlin K. Virtual patients: ED-2 Band-Aid or valuable asset in the learning portfolio? Acad Med. 2010;85(1):155–158. doi: 10.1097/ACM.0b013e3181c4f8bf. [DOI] [PubMed] [Google Scholar]
- 11.Kanter SL. Fundamental concepts of problem-based learning for the new facilitator. Bull Med Libr Assoc. 1998;86(3):391–395. [PMC free article] [PubMed] [Google Scholar]