Abstract
Objective
To implement and evaluate a simulation activity and related assignments within a geriatric elective to teach pharmacy students about the medication management difficulties experienced by low-vision patients.
Design
Students wore low-vision simulation goggles while engaging in medication management tasks. Students also reflected on their experiences in journals and developed modalities to improve low-vision patients' access to prescription information.
Assessment
Results of a perception survey indicated that students were able to identify and differentiate among various low-vision medication management difficulties. Students' reflections suggested that they recognized the challenges encountered by low-vision patients. All patient assistance project submissions were suitable for the targeted populations and medication management difficulties. Peer review and student feedback of the activities were favorable.
Conclusion
Through this low-vision goggle simulation exercise and other activities, students were able to identify the medication management difficulties encountered by low-vision patients and propose solutions to their drug information access problems.
Keywords: simulation, medication management, adherence, geriatrics
INTRODUCTION
“Low vision” is visual impairment that cannot be corrected by standard glasses, contact lenses, medicine, or surgery, and interferes with a person's performance of daily activities. Low vision is usually a consequence of age-related eye diseases such as cataracts, glaucoma, diabetic retinopathy, or macular degeneration, but may also be a result of genetic diseases such as retinitis pigmentosa. The condition affects up to 14 million Americans and as many as 135 million people worldwide, most of whom are over 65 years of age.1-4 Older adults with vision impairment are 3.1 times more likely to have difficulty managing medications compared to people with no vision loss.5 They have difficulty reading prescription and nonprescription medication information and may take the wrong medication or incorrect doses of medication, resulting in serious negative consequences, including overdoses or inadequate treatment of health problems, which may lead to emergency room visits or hospitalization.6,7 The majority of individuals with vision loss also report increased anxiety related to medication management and having to rely on companions, or in some cases complete strangers, to obtain necessary drug information. Furthermore, 65% of Americans indicate that if they were to have severe vision loss, they would be most concerned about not being able to properly identify their medications.8
To address these medication safety issues, in 2008 the American Society of Consultant Pharmacists (ASCP) Foundation and the American Foundation for the Blind (AFB) jointly published the Guidelines for Prescription Labeling and Consumer Medication Information for People with Vision Loss to “provide pharmacists and pharmacies with specific recommendations for making important medication information accessible for patients with vision loss.”9(p1) The magnitude of this problem will increase dramatically in the next 20 years, as the number of visually impaired Americans is expected to double. Also, with many older adults living independently at home without the support of a caregiver to read prescription labels for them, future pharmacists must be aware of the difficulties experienced by individuals in this population and be prepared to accommodate them.2,4
The American Association of Colleges of Pharmacy's (AACP) Center for the Advancement of Pharmaceutical Education (CAPE) Educational Outcomes state that doctor of pharmacy (PharmD) programs should prepare students to carry out duties in accordance with professional guidelines,10 such as those published by ASCP and AFB.9 Furthermore, AACP and the Accreditation Council for Pharmaceutical Education (ACPE) both recommend that PharmD programs employ strategies by which students are active in and take responsibility for their learning and through which they think critically and learn to solve problems related to drug therapy. Among the methods recommended for accomplishing these tasks are active-learning strategies, including simulations.11-13
Simulation activities may be the most effective method to achieve some educational objectives and can be specifically structured to meet learning objectives and tailored to fit individual needs. Simulations allow the instructor to move away from teacher-centered direction and present more student-centered learning opportunities that improve student interest in material, increase learning, and contribute to students' affective growth.14,15 Although studies in healthcare education, including pharmacy, have described classroom simulations of a variety of age-related impairments including vision loss, none have specifically focused on visual impairments.16-26 Some of these multi-factorial activities have included awareness of the medication management difficulties of older adults, but the activities did not target identification of students' ability to identify particular medication-related problems of the visually impaired.17-20 The AACP suggests that professional pharmacy programs should not only prepare students to provide population-based care by identifying patients who require special attention, but should also teach students to provide patient-specific care, as therapeutic management is most effective on an individual level.10,13 Since not all patients with low vision are impaired as a result of the same disease, it is important to provide students with simulation experiences that include a variety of low-vision diseases. Although 1 article described an activity in which pharmacy students were exposed to a series of visual impairment simulations as part of a comprehensive geriatric experience, the article did not spotlight the impairment differences among the diseases nor address the medication management difficulties associated with each impairment.19 In order to prepare students to provide assistance to this underserved population, learning situations must include first-hand exposure to a variety of visual impairments as well as a detailed investigation of the difficulties related to medications.
This paper describes a low-vision simulation activity in which students experience the medication management difficulties of patients with various low-vision conditions and use their new-found knowledge to devise methods for improving access to prescription information for these patients. Students first participated in this simulation at the University of Louisiana at Monroe (ULM) College of Pharmacy in 2005 in the geriatric elective course Aging and Drug Use in the Elderly. The major objective of this course is to define medication-related problems that affect medication use and therapeutic outcomes in older adults, including age-related eye diseases and low vision. Subjects that cannot be addressed in great detail in the geriatric components of the required curriculum due to course time constraints are covered in this elective course. This experience was designed to provide students with a better understanding of the various medication-related difficulties faced by visually impaired patients and to expand students' opportunities to develop patient- and population-specific services related to low vision.
DESIGN
In this simulation activity, students wore welder's goggles with lenses that had been altered to simulate low-vision conditions of glaucoma, cataracts, macular degeneration, diabetic retinopathy, and retinitis pigmentosa, while manipulating pills, prescription vials, and other medication-related materials. The low-vision goggles used in the activity have been previously described.27 The objectives for the learning series were for students to: (1) recognize challenges encountered by older adults with low-vision conditions; (2) compare and contrast medication management difficulties among low-vision conditions; (3) differentiate medication management difficulties of individual low-vision conditions; and (4) propose solutions to prescription drug information access problems for patients with low vision.
Description of Low-Vision Learning Module
Learning activities throughout this series transitioned from a teacher-directed format to student-centered activities and critical-thinking exercises. The concept of low vision was introduced via a traditional lecture that covered age-related changes in the eye and the disease processes of the selected low-vision conditions. Some online pictorial simulations of disease characteristics and progression also were provided. Prior to the start of the next class meeting, 5 simulation activity stations were set up at separate tables in the classroom, 1 for each low-vision disease covered. All materials for each station were organized and placed in a zippered bag prior to the simulations. Approximately 30 minutes were required to assemble the stations. At the beginning of the class period, the background disease information was reviewed in an informal quiz format using animated PowerPoint slides. Students were then divided into groups and rotated among the stations, engaging in 9 medication-related tasks at each station while wearing the given pair of low-vision simulator goggles. The list of tasks included many of the most common ways in which patients interact with medications on a regular basis. Students read prescription labels, auxiliary labels, and patient information leaflets; distinguished the color, shape, and size of, and fine markings on tablets and capsules; poured doses of liquid medications (colored simple syrup) into spoons; and measured doses of medications in syringes (without needles). Students only manipulated medications; no medications were ingested. Students were instructed to look at all parts of the prescription label, including the number of refills and expiration date, and to approach reading the label as a patient would, word-for-word, without relying on pharmacy knowledge that might allow them to infer the directions for a particular drug. In addition to the course coordinator and other instructors, students previously enrolled in the course also served as facilitators. Facilitators trained in the simulation procedures by the course coordinator to ensure consistency in manipulation of all components of the learning activities were available at each station. Prior to leaving each station, students completed a worksheet on which they listed visual characteristics of each disease, daily activities that may be affected by each condition, and medication-related issues that may be affected by each disease. These worksheets were intended to serve as notes for students' next assignment related to the simulation. In addition, students completed a survey evaluating their perceptions of the level of difficulty associated with each task completed for each low-vision condition. They were also asked to submit honest, anonymous comments on the simulation prior to leaving the classroom.
At the next class meeting, students were challenged to use their experience with the low-vision simulator goggles and their creativity and critical-thinking skills to complete a patient assistance project. The period began with a brief review and discussion of students' simulation experiences, then perception survey results were shared with the students. After the discussion, students were divided into groups and tasked with designing a device, technique, or routine to improve access to prescription drug information for older adults with 1 of the 5 low-vision diseases. Students were given the remainder of the 50-minute class period to work on the project; however, an additional 2 to 3 hours of students' time were required to complete the assignment depending on the complexity of the project design. Groups presented prototypes of their projects to the class a week later. In addition, students also were required to submit justification for their design, including the characteristics of the chosen disease, the group's reason for choosing that condition, their perceived medication management difficulties in the population, a description of the assistive method, and the rationale for how the method would help individuals in that population. The assignment was graded on 4 areas: (1) suitability for the chosen condition and population; (2) ease of use; (3) reproducibility, including cost; (4) creativity and effort. Scores were assigned using a rubric developed based on the critical features recommended by the AFB for effective assistance modalities for visually impaired individuals.28
As part of the regular weekly requirements of the course, students also completed a reflective journal exercise on their experience with the medication management difficulties of low-vision patients. All journal entries for the course were graded subjectively using a rubric to score content, thought, effort, mechanics, and professionalism. (The rubrics are available from the author upon request.)
EVALUATION AND ASSESSMENT
Approximately 1½ to 2 hours of class time were required to complete all 5 low-vision simulation stations and the worksheet exercises, based on a class size of about 20 second-year (P2) and third-year (P3) students, with time required dependent upon the availability of at least 2 pairs of simulation goggles at each station.
Because there was no documentation in the literature of the medication management difficulties associated with different low-vision conditions with which students' experiences could be compared, a survey was conducted to evaluate students' perceptions of task difficulty for each condition. Prior to administration, the questionnaire was evaluated for face and content validity with a focus group of faculty members and students. Minor changes in language and formatting were made to the final instrument based on feedback from the focus group. The ULM Institutional Review Board granted expedited approval for this survey and written informed consent was obtained from all participants. After each simulation, students (n=18) independently responded to 9 Likert-type survey items evaluating task difficulty on a scale of 0 to 4 for each disease (0 = no difficulty and 4 = great difficulty). Students were instructed to respond to each item by evaluating their experiences with each simulated disease compared to their experience performing the same tasks with normal vision, including accommodations made because of having low vision and time involved in completing each task.
The task difficulty ratings within each low-vision condition were compared with Kruskal-Wallis tests due to the ordinal nature of the rating scale. Differences in task-difficulty ratings for students in different professional years of the PharmD program were evaluated with the Wilcoxon rank sum test. In addition, a difficulty index score was calculated for each condition in order to compare the overall level of medication management difficulty among the 5 diseases. Each difficulty index score was calculated as the total of the 9 task difficulty ratings for the given low-vision condition and could range from 0 to 36. Difficulty index scores among the low-vision conditions and for each professional year were evaluated for differences using ANOVA, with post-hoc analysis using Tukey's Honestly Significance Difference test. Data were analyzed with SAS, version 9.1 (SAS, Chicago, IL) using an alpha level of 0.05.
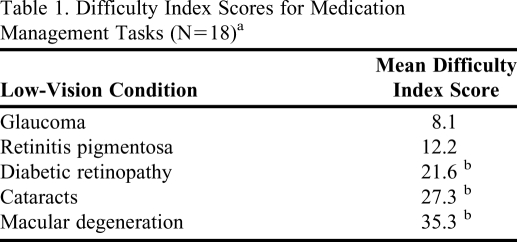
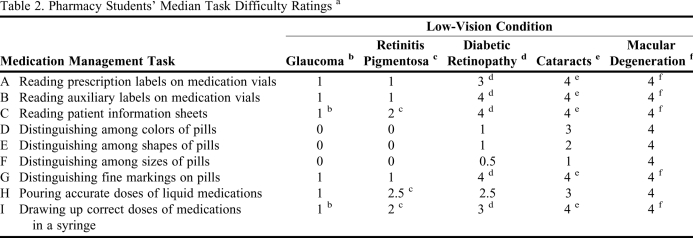
Eighteen students (100% of the class) completed the perception survey. When comparing and contrasting medication management difficulties among low-vision conditions, medication management difficulty index scores (Table 1) indicated that students perceived the greatest medication management difficulty with macular degeneration and the least with glaucoma. The difficulty index scores were significantly higher for macular degeneration, cataracts, and diabetic retinopathy than with glaucoma and retinitis pigmentosa. There were significant differences in the degree of difficulty reported for performing various medication-related tasks with each simulated disease (p<0.001). The most difficult tasks for all diseases were reading patient information leaflets and drawing correct doses of medications in a syringe (Table 2). When comparing differences in task difficulty ratings by professional year, P2 students found reading tablet markings during the glaucoma simulation significantly more difficult than did P3 students (P2 median = 2; P3 median = 0; p = 0.023). No other significant differences in ratings occurred between P2 and P3 students. There also was no significant difference in overall index scores for each condition by professional year (p > 0.32).
Table 1.
Difficulty Index Scores for Medication Management Tasks (N=18)a
Difficulty index score range = 0 - 36.
b Scores on these items were significantly higher than those for glaucoma or retinitis pigmentosa (p < 0.001).
Table 2.
Pharmacy Students' Median Task Difficulty Ratings a
Based on a scale of 0 – 4 on which 0 = no difficulty and 4 = great difficulty. Indicated differences are based on Kruskal-Wallis post hoc analysis.
b Glaucoma: tasks C and I were more difficult than D, E, and F (p < 0.001).
c Retinitis pigmentosa: tasks C, H, and I were more difficult than D, E, and F (p < 0.001).
d Diabetic retinopathy: tasks A, B, C, G, and I were more difficult than D, E, and F (p < 0.001).
e Cataracts: tasks A, B, C, G, and I were more difficult than E or F (p < 0.001).
f Macular degeneration: tasks A, B, C, G, and I were more difficult than D (p < 0.015).
Student group submissions for the patient assistance project included a variety of assistance modalities. Two groups submitted different talking prescription vials, created by attaching inexpensive audio recording devices to prescription vial caps. The pharmacist would be able to record information on the device prior to dispensing and the patient could simply press a button to hear the name and strength of the medication, dosing and frequency instructions, indication, and other important information. Two other groups labeled vials with tactile indicators, including 3-dimensional paint or stickers in the form of letters, numbers, and shapes, to identify drug indications and dosing instructions, frequency, and timing. These groups also provided a variety of large, high-contrast reference sheets or charts to link the prescription vials to the indicators and to serve as patient reminders of what the symbols represent. While students were instructed only to focus on an individual low-vision condition, some groups stated that their designs might be applicable to multiple impairments, which was in keeping with the AFB's recommendations.28 The average project score was 96%. All submissions were suitable for the targeted populations and addressed the medication management difficulty associated with the disease chosen. The assistance modalities were determined to be at least relatively easy for the intended audience to use and could be reproduced inexpensively by a community pharmacist, requiring little to no cost to be passed on to the patient.
Based on the rubric used for all journal entries in the course, reflection scores on students' reflective journal entries indicated that they were able to provide real-life examples of the medication management issues addressed in the simulation, convey evidence of a personal response to the issues raised in class, and demonstrate personal growth and societal awareness. The average score on this entry assignment was 98.8%, the highest average score for all journal topics during the semester (range 87.6% - 98.8%). All students reported that the simulation experience was valuable to them in understanding the struggles faced by this patient population.
There were several common themes in students' reflections on the low-vision simulations; one was an appreciation of the level of generalized impairment associated with low vision. One student noted: “When I would put the goggles on and perform the tasks, I would just be thinking the whole time about how glad I was that I would be able to take the goggles off. These patients can't just take the goggles off, though. They are stuck with this disability, and we can play a significant role in easing the difficulties of daily medication use.”
Another recurring theme related to the difficulty visual impairment created with medication management. A student commented: “Overall, I now see that although there are many different types of disorders, that every disorder will cause problems with medication compliance. In almost every disorder, you had trouble reading. That's the initial step in taking the medication--read how to take it.”
Most importantly, however, students recognized the inherent responsibility to apply lessons learned from the experience to patient care. As expressed by 1 student, “When completing the goggle exercises, I was thinking that all of these people just need a family member to give them their medicines every day. That would make them lose a sense of independence though…so I felt a sense of responsibility to find a way to at least give these patients the independence of taking their own medicine!”
Anonymous feedback submitted by students was also uniformly positive. In general, students supported simulation as a learning method, expressed appreciation for the knowledge and experience they gained through the simulation, and endorsed continuation of this activity. One student noted, “If I would have just listened to a lecture on the information, I don't think I would have realized the extent of these problems and how truly life-changing these eye conditions are to those affected.” Several students also suggested that all pharmacy students should participate in the activity prior to graduation.
Furthermore, according to a peer reviewer, the lesson design, learning methods, organization, materials, and student participation were rated as excellent. The peer reviewer recommended 2 improvements for future simulations— providing worksheets for students in class rather than requiring them to print their own copies of the document previously provided electronically and including a materials checklist in each simulation kit. (The checklist is available from the author upon request.)
DISCUSSION
The goal of this simulation activity was to provide students with first-hand knowledge of vision-related medication management difficulties needed to devise methods for improving access to prescription information for these patients. The lack of assistance available to this underserved population may have potentially fatal consequences; therefore, it is important for future pharmacists to be prepared to address this health system deficit. Since not all visually impaired individuals experience the same problems in management of their medications, students must be given the opportunity to consider the differences in older adults with low vision and how to tailor methods of assistance to individual patients. Patients with macular degeneration, ie, loss of central vision, do not have the same needs as patients with glaucoma, ie, loss of peripheral vision. According to the AFB, there is no single assistance modality that meets the needs of most individuals with visual impairment.28
Through this simulation activity, students “became the patient” and gained a personal understanding of the medication management difficulties of patients with a variety of low-vision conditions. Students will not understand fully the medication-related problems of someone with low vision unless they “see through their eyes” and are challenged to deal with seemingly simple tasks. Only then will they be better prepared to meet the patient's needs because they will have personally experienced those needs.
Also, when students were not wearing simulation goggles, they were able to observe their peers as they struggled with the medication management tasks; thus, all students were able to experience the challenges of low-vision medication management difficulties from the viewpoints of both the “patient” and an observer. Student feedback from the activity suggests an improved understanding of problems experienced by patients with these conditions that would not have been afforded by teacher-directed activities. Students' reflective journal entries also indicated that students were able to recognize the challenges of low-vision patients and the need for pharmacists to intervene on their behalf.
In addition to providing valuable information about the needs of patients, the results of the perception survey also indicated students recognized that “low vision” was not the same for all individuals and that some medication-related tasks were more difficult for some low-vision patients than others. The significant differences in difficulty index scores for low-vision diseases suggest that students were able to compare and contrast medication management difficulties among low-vision conditions. The significant differences in difficulty levels for medication-related tasks suggest that students also were able to differentiate medication management difficulties of individual low-vision conditions. Students' perceptions that macular degeneration (the leading cause of vision loss over age 65 years) and cataracts (the leading cause of blindness worldwide) are among the most difficult diseases with which to live are notable. In addition, students' perceptions that patients with macular degeneration, cataracts, and diabetic retinopathy will have the greatest medication management difficulties are in line with the fact that these diseases primarily impair the central visual field, while glaucoma and retinitis pigmentosa are impairments of peripheral vision. Completion of medication management tasks present greater difficulty for those with impaired central vision and therefore these patients require more assistance from the pharmacist.
In the patient assistance project, students were challenged to think critically and develop creative solutions to patient problems, consistent with recommendations of the AACP and ACPE.11-13 The characteristics of the projects submitted signified that students “learned”' on a variety of levels. First, they were able to apply knowledge attained from the simulation to a patient situation. Students also analyzed the unique qualities of the specific low-vision patient population, including other age-related impairments such as arthritis, cost concerns, and limited access to resources. Then they synthesized the information and evaluated the specific situation to select an effective assistance modality that pharmacists may provide at the community pharmacy level. Although some projects were judged by the course coordinator to have some suspected flaws related to ease of use by the intended audience, all were minor problems that could easily be remedied with some refinement by the students.
Prior to the first offering of this activity, several hours of time are required to create the simulator goggles and assemble all supplementary materials required for the simulation tasks. However, once materials are created and kits are assembled, subsequent offerings only require that liquids be replenished in bottles and missing or broken supplies be replaced. While the schedule of this geriatric elective allows for all simulation stations to be completed in one 100-minute class period, courses without the benefit of an extended class time would require the stations to be set up on multiple days if the classroom space is shared by other classes. Estimated costs for this activity are about $80 to $90 per single complete set of simulation materials ($130 to $150 with 2 sets of goggles per kit as recommended in the checklist). In addition, many of the materials can be prepared in a pharmacy school dispensing laboratory.
Some limitations to the simulation activity and methods of assessment were identified. A convenience sample was used rather than a random sample and the survey sample size was small. The difference in difficulty index scores between P2 and P3 students for glaucoma is likely attributable to the small sample size rather than reliance of the P3 students on prior knowledge of the disease state from previous courses to complete the simulation activities. Also, the results represent students who voluntarily enrolled in this geriatric elective course and may not be representative of all student pharmacists.
Although all station facilitators were trained prior to the activity, facilitation of some stations by course instructors rather than other students may have led to bias in student responses on the perception questionnaire. Also, the rubrics used to grade the student assignments had not been validated and the scores for the rubric dimensions were subjectively assigned by the course coordinator.
For the most recent offering of this simulation activity, worksheets were provided to students and a material checklist was prepared as recommended by the peer reviewer. The checklist was extremely helpful in preparing for the simulation. Furthermore, the list of tasks in which students engage while wearing the goggles will be expanded to include manipulation of pill splitters, blood glucose monitors, and automatic home blood pressure machines for future simulations. Also, based on student feedback suggesting that this activity would be beneficial to all student pharmacists, plans have been made to move the simulation from the geriatric elective course into the required curriculum. At the time this activity was developed, the curriculum at the University of Louisiana at Monroe College of Pharmacy was being redesigned into a modular, integrated curriculum with incorporation of an integrated laboratory sequence to provide for more active learning. This low-vision simulation will be part of the required laboratory course so that all students may gain the knowledge, skills, and attitudes afforded by this unique learning experience.
SUMMARY
A patient-centered, student-directed learning activity involving simulation of low vision using goggles with altered lenses provided students with hands-on opportunities to experience the medication management difficulties faced by patients with a variety of low-vision conditions. Following the simulation exercise, students were well-prepared to devise ways to improve vital access to prescription information and hopefully help to minimize the risk of medication errors in this population.
ACKNOWLEDGMENTS
The authors express special thanks to Dr. Lamar Pritchard, Dean, ULM College of Pharmacy, 2004-2009, for administrative and financial support, and to Dr. Lesa Lawrence for helpful peer review of this classroom activity. The authors also wish to posthumously acknowledge Dr. Greg Leader, Dean, ULM College of Pharmacy, 2010, for mentorship and encouragement to submit this manuscript for publication.
REFERENCES
- 1. Information for Healthy Vision, Low Vision FAQs, National Eye Institute, National Institutes of Health. Available at: http://www.nei.nih.gov/lowvision/content/faq.asp. Accessed July 21, 2010.
- 2.Janiszewski R, Heath-Watson SL, Semidey AY, Rosenthal AM, Do Q. The low visibility of low vision: increasing awareness through public health education. J Vis Impair Blind. 2006;100:849–861. [Google Scholar]
- 3. Facts and Figures on Americans with Vision Loss. American Foundation for the Blind. Available at: http://www.afb.org/Section.asp?SectionID=15&TopicID=413&DocumentID=4900. Accessed July 21, 2010.
- 4. National Plan for Eye and Vision Research, National Eye Institute, National Institutes of Health. Available at: http://www.nei.nih.gov/strategicplanning/np_low.asp. Accessed September 29, 2009.
- 5. US Department of Health and Human Services, National Center for Health Statistics. National Health Interview Survey, 1994: Second Supplement On Aging. ICPSR02563-v3. Hyattsville, MD: U.S. Dept. of Health and Human Services, National Center for Health Statistics, 1998. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2007-02-12. doi:10.3886/ICPSR02563.
- 6. Access to Drug Labels Survey Report. American Foundation for the Blind. http://www.afb.org/Section.asp?SectionID=3&TopicID=135&DocumentID=4520. Accessed July 21, 2010.
- 7. Comments on Prescription Drug Information Accessibility. American Foundation for the Blind. http://www.afb.org/Section.asp?SectionID=3&TopicID=329&DocumentID=2454. Accessed July 21, 2010.
- 8. Key Findings: National Poll on Severe Vision Loss/Blindness, 2007. American Foundation for the Blind. http://www.afb.org/seniorsite.asp?SectionID=68&TopicID=320&DocumentID=3376. Accessed July 21, 2010.
- 9. Guidelines for Prescription Labeling and Consumer Medication Information for People with Vision Loss. A Collaborative Project of American Society of Consultant Pharmacists Foundation and American Foundation for the Blind. American Society of Consultant Pharmacists Foundation. Available at: http://www.ascpfoundation.org/downloads/Rx-CMI%20Guidelines%20vision%20loss-FINAL2.pdf. Accessed July 21, 2010.
- 10. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education. Educational Outcomes 2004. http://aacp.org/resources/education/Pages/CAPEEducationalOutcomes.aspx. Accessed September 28, 2009.
- 11. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Adopted January 15, 2006. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed July 21, 2010.
- 12.AACP Commission to Implement Change in Pharmaceutical Education. Background paper II: entry-level, curricular outcomes, curricular content and educational process. Am J Pharm Educ. 1993;57(4):377–385. [Google Scholar]
- 13. AACP Commission to Implement Change in Pharmaceutical Education. Background Paper V: Maintaining our Commitment to Change. American Association of Colleges of Pharmacy; 1995. http://www.aacp.org/resources/historicaldocuments/Documents/BackgroundPaper5.pdf. Accessed July 21, 2010.
- 14.Heitzmann WM, editor. Educational Games and Simulations. Washington, DC: National Education Association; 1983. pp. 8–12. [Google Scholar]
- 15.Pate GS, Parker HA. Designing Classroom Simulations. Belmont, CA: Fearon Publishers; 1973. pp. 1–16. [Google Scholar]
- 16.Reichman SL, Weaver-Meyers P. Glaucoma and cataracts: a nurse-patient simulation for nursing students. J Nurs Educ. 1984;23(7):314–315. doi: 10.3928/0148-4834-19840901-13. [DOI] [PubMed] [Google Scholar]
- 17.Lorraine V, Allen S, Lockett A, Rutledge CM. Sensitizing students to functional limitations in the elderly: an aging simulation. Fam Med. 1998;30(1):15–18. [PubMed] [Google Scholar]
- 18.Varkey P, Chutka DS, Lesnick TG. The Aging Game: improving medical students' attitudes toward caring for the elderly. J Am Med Dir Assoc. 2006;7(4):224–229. doi: 10.1016/j.jamda.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 19.Plake KS. A course on chronic illness: learning the patient's perspective. Am J Pharm Educ. 2003;67(1):9. [Google Scholar]
- 20.Evans S, Lombardo M, Belgeri M, Fontane P. The Geriatric Medication Game in pharmacy education. Am J Pharm Educ. 2005;69(3):46. [Google Scholar]
- 21.Miller SW. Teaching geriatrics to Generation Y. Am J Pharm Educ. 2004;68(3):67. [Google Scholar]
- 22.Kennedy DH, Fanning KD, Thornton PL. The Age Game: an interactive tool to supplement course material in a geriatrics elective. Am J Pharm Educ. 2004;68(5):115. [Google Scholar]
- 23.Robinson SB, Rosher RB. Effect of the “Half-Full Aging Simulation Experience” on medical students' attitudes. Gerontol Geriatr Educ. 2001;21(3):3–12. [Google Scholar]
- 24.McVey LJ, Davis DE, Cohen JJ. The “Aging Game”: an approach to education in geriatrics. JAMA. 1989;262(11):1507–9. doi: 10.1001/jama.262.11.1507. [DOI] [PubMed] [Google Scholar]
- 25.Hoffman SB, Brand FR, Beatty PG, Hamill LA. Geriatrix: a role-playing game. Gerontologist. 1985;25(6):568–72. doi: 10.1093/geront/25.6.568. [DOI] [PubMed] [Google Scholar]
- 26.Chen JT, LaLopa J, Dang DK. Impact of patient empathy modeling on pharmacy students caring for the underserved. Am J Pharm Educ. 2008;72(2):40. doi: 10.5688/aj720240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zagar M, Baggarly S. Low vision simulator goggles in pharmacy education. Am J Pharm Educ. 2010;74(3) doi: 10.5688/aj740583. Article 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American Foundation for the Blind. Executive Summary of “A Study on How to Make Prescription Pharmaceutical Information, Including Drug Labels and Usage Instructions, Accessible for Blind and Visually Impaired Individuals.” www.afb.org/Section.asp?SectionID=3&;TopicID=329&DocumentID=3629 Accessed September 28, 2010.