Abstract
To examine the prevalence of criminal thinking in mentally disordered offenders, incarcerated male (n = 265) and female (n = 149) offenders completed measures of psychiatric functioning and criminal thinking. Results indicated 92% of the participants were diagnosed with a serious mental illness, and mentally disordered offenders produced criminal thinking scores on the Psychological Inventory of Criminal Thinking Styles (PICTS) and Criminal Sentiments Scale-Modified (CSS-M) similar to that of non-mentally ill offenders. Collectively, results indicated the clinical presentation of mentally disordered offenders is similar to that of psychiatric patients and criminals. Implications are discussed with specific focus on the need for mental health professionals to treat co-occurring issues of mental illness and criminality in correctional mental health treatment programs.
Keywords: Offender, Inmate, Mental illness, Mentally disordered offender, Criminal thinking
It was recently estimated that persons with serious mental illness are 1.5 times as likely to be incarcerated as to be hospitalized for treatment of their psychiatric disorders (Morrissey, Meyer, & Cuddeback, 2007). This observation is among the latest evidence fueling a longstanding concern that persons with serious mental illness are disproportionately represented in America’s jails and prisons (Lamb & Weinberger, 1998; Teplin, 1990; Teplin, Abram, & McClelland, 1996). In many jurisdictions, local jails have superseded mental health facilities as principal providers of mental health treatment; indeed, more than 15 years ago it was noted that the Los Angeles County Jail system had surpassed all state and private psychiatric specialty hospitals to become the nation’s largest provider of institutionally based mental health services (Torrey, 1995).
Officials from both the criminal justice and mental health communities view these observations with alarm, and there are numerous collaborative efforts underway in many jurisdictions aimed at developing interventions for reducing what is seen as the often unnecessary use of criminal justice interventions with mentally ill arrestees (Laberge & Morin, 1995). These interventions are designed to identify and divert justice-involved persons at various junctures or “intercept points” (Munetz & Griffin, 2006) in the criminal justice process. They include a growing number of jail diversion mechanisms (Steadman, Morris, & Dennis, 1995; Steadman et al., 1999) which attempt to shift offenders with mental illness from the criminal justice system to the mental health treatment system, as well as reentry programs which are designed to facilitate linkage of correctional inmates with mental illness to community-based services upon release from prisons and jails (Hartwell & Orr, 1999).
Underlying the development of services operating at the interface of the mental health and criminal justice systems is a belief that criminal behavior among many offenders with serious mental illness results primarily from the symptoms of their major Axis I psychiatric disorders, and that providing proper treatment and support services will reduce their likelihood of offending and re-offending (Fisher, Silver, & Wolff, 2006). Overlooked in this approach to the prevention of offending among persons with mental illness is the possibility that a subset of offenders who have major Axis I diagnoses, such as schizophrenia or major affective disorders, also have co-occurring antisocial tendencies (ASPD; Hiday, 1999). Although the “mad or bad?” debate dates back to asylums of the European Enlightenment era (Weiner, 2008), a number of recent clinical and epidemiological studies support the possibility of co-occurring criminal tendencies and mental illness (cf, Moran & Hodgins, 2004). Additionally, retrospective studies of adults diagnosed with schizophrenia have found that, as a group, these individuals had higher rates of childhood conduct disorder (a precursor to ASPD) than did persons in the general population (Mueser et al., 2006; Robins, 1993). Data on patterns of criminal involvement provide further support; in the ACCESS study of homeless adults with co-occurring serious mental illness and substance abuse disorders (Randolph et al., 2002), those with a history of juvenile offending were at elevated risk for arrest as adults (Desai, Lam, & Rosenheck, 2000). For these individuals, their offending behaviors and their major Axis I disorders may or may not be strongly linked; instead, some might best be characterized as persons with propensities to engage in criminal or antisocial behaviors who happen to also have major psychiatric disorders.
Together, these data suggest that simply treating offenders’ Axis I disorders, although essential, may be insufficient to prevent their involvement in criminal activities. These data further suggest that, if we are to understand fully and better address the problems of offending in this population, we need to look beyond the mental health services and treatment perspective and examine the extent to which these individuals share risk factors with offenders who do not have serious mental illness. It is commonly accepted that, to be effective, offender rehabilitation must target risk factors (termed criminogenic needs) associated with criminal behavior (Andrews & Bonta, 2006; Andrews et al., 1990; Gendreau, 1996). One critically important but largely overlooked risk factor, which is the focus of this investigation, is the extent to which criminal thinking, common among the general offender population (Andrews & Bonta, 2006; Walters, 1990, Yochelson & Samenow, 1976), is prevalent among offenders with major Axis I disorders. Offenders think differently than non-offenders (Yochelson & Samenow, 1976), and their attitudes, values, beliefs, and cognitions are predictive of criminal involvement (Simourd, 1997; Simourd & Olver, 2002; Simourd & Van de Ven, 1999; Walters, 1996, 2002; Yochelson & Samenow, 1976).
Identifying the prevalence of criminal thinking for offenders with mental illness is necessary for three reasons. First, data on this co-occurrence would help to explain why it is that providing comprehensive mental health services, even those that are deemed “evidence based practices,” fail to alter rearrest patterns among offenders with mental illness. Second, from a treatment design perspective, such data might stimulate the development of new approaches for managing the problem of the persistently arrested person with serious mental illness by incorporating treatment protocols for addressing criminal thinking patterns among offenders with mental illness. Finally, data such as these would expand the theoretical and policy discourse centering on offenders with mental illness from one focusing exclusively on their unique needs as persons with psychiatric disorders to one that also addresses their co-occurring—and possibly unrelated, criminal propensities. Although Bonta, Law, and Hanson (1998) noted that risk factors for mentally disordered offenders are similar to non-mentally disordered offenders, the prevalence of these factors has not been investigated with the subset of inmates who have serious psychiatric disorders. As a result, there currently are no data that allow determination of the prevalence of co-occurring criminogenic thought patterns among inmates with major mental illnesses.
Thus, the purpose of this study was to assess the prevalence of criminal thinking in a sample of offenders suffering mental illnesses. Given previous speculations that mentally disordered offenders present with similar criminogenic risk factors as non-mentally disordered offenders, we hypothesized that mentally ill inmates would evidence criminal thinking and antisocial attitudes comparable to their non-mentally ill counterparts.
METHOD
Participants
Participants consisted of 416 incarcerated male (n = 265, 64%) and female (n = 149, 36%) adults from the Texas Department of Criminal Justice (TDCJ). The inmates had a mean age of 36.23 years (SD = 10.59) and were predominantly Caucasian (n = 189, 45.7%) and African American (n = 139, 33.6%); however, other racial groups were represented in this sample including Hispanics (n = 56, 13.5%), American Indian/Native Americans (n = 4, 1.0%), and participants who defined themselves as “other” (n = 26; 6.3%). Approximately half of the participants were single or non-partnered (50.1%, n = 205), whereas 15% (n = 61) were married/partnered. The remainder were divorced (n = 86, 21.0%), separated (n = 53, 12.7%), or widowed (n = 5, 1.2%). The average years of education were 11.01 (SD = 2.63). Inmates were incarcerated for a variety of crimes including drug/alcohol-related crime(s) such as possession or distribution (n = 88, 16.7%); robbery/theft (n = 105, 19.2%); murder/manslaughter (n = 46, 8.3%); sex crime (n = 50, 9.3%); assault/battery (n = 22, 4.1%); aggravated assault/aggravated battery (n = 31, 5.7%); and other types of offenses (n = 65, 12.4%).
Participants were serving a median sentence of 120 months (10 years), with 5% serving a life sentence. At the time of this study, the inmate participants had served an average of 6 years (SD = 7 years) of their current prison sentence.
Several of the above demographics and status variables of the participants in this study were highly consistent with that of all offenders incarcerated in TDCJ prison facilities in 2005 (Texas Department of Criminal Justice, 2006), including mean age, ethnic/racial identity (with the exception of over representation of White/Caucasian inmates and under-representation of Hispanic/Latino inmates), and years of completed education (see Table 1). Participants in this sample were sentenced, on average, to five fewer years of incarceration than the average TDCJ inmate. The categorization options for housing security level and index offense as presented on the demographic form prohibited comparison of these variables to the population of offenders in TDCJ prisons. Information about current relationship status, amount of time served, and reception of mental health services was not available for the general TDCJ prisoner population and therefore could not be compared to our sample.
Table 1.
Race, age, years of education, and length of sentence in the current sample and population of TDCJ prisoners
| Current sample | TDCJ prisoner population | |
|---|---|---|
| Race (%) | ||
| Black/African American | 33.6 | 38.3 |
| Hispanic/Latino | 13.5 | 31.2 |
| White/Caucasian | 45.7 | 30.0 |
| Other | 6.3 | 0.5 |
| Age (years) | 36.23 | 37 |
| Years education completed | 11.01 | 9.7 |
| Sentence length (months) | 177.89 | 235.2 |
Materials
A written informed consent form and federal certificate of confidentiality informed inmates of the nature and purpose of the study, procedures to protect confidentiality, perceived risks, and their rights as human subjects. A demographic form requested the following information: age, race/ethnicity, relationship status, years of formal education, legal status (including the index offense, current sentence length, time served toward current sentence, and security level), prevalence and specificity of a mental disorder, and whether they were or were not receiving mental health services at the time of their participation.
The Psychological Inventory of Criminal Thinking Styles (PICTS) is an 80-item self-report measure designed to measure how criminals think (Walters, 2006). The PICTS utilizes a 4-point Likert-type scale (1 = disagree, 4 = strongly agree; Walters, 2006), and was developed to assess the cognitive thinking patterns associated with serious criminal behavior regardless of criminal type. Scores are calculated for two content scales (Current Criminal Thinking, Historical Criminal Thinking), the eight scales representing the thinking patterns (i.e., Mollification, Cutoff, Entitlement, Power Orientation, Sentimentality, Superoptimism, Cognitive Indolence, and Discontinuity), and five Factor and Special Scales (i.e., Problem Avoidance, Interpersonal Hostility, Self-Assertion, Denial of Harm, and the Fear of Change) with higher scores being indicative of a higher degree of criminal thinking (Walters, 2006). Internal consistency reliability coefficients for the PICTS scales ranged from moderate to high: 0.55 to 0.88 for male offenders (Walters, 1995), and 0.54 to 0.88 for female offenders (Walters, Elliott, & Miscoll, 1998). Scale test–retest reliability coefficients were also found to be adequate for male and female offenders, ranging from 0.68 to 0.85 after 2 weeks, and 0.57 to 0.72 after 12 weeks (Walters, 1995; Walters et al., 1998). In terms of validity, the PICTS scales were found to correlate modestly to moderately with other measures of criminality, such as the number of prior arrests, the number of prior commitments, the age at first arrest, the age at first commitment, disciplinary infractions, psychopathy, and the Lifestyle Criminality Screening Form (for a complete review, see Walters, 2006; Walters & Mandell, 2007; Walters & Schlauch, 2008).
The Criminal Sentiments Scale-Modified (CSS-M; Simourd, 1997) is a 41-item self-report instrument designed to measure “attitudes, values, and beliefs related to criminal behavior” (Wormith & Andrews, 1984). Whereas the PICTS measures the process of criminal thinking (i.e., how a criminal thinks), the CSS-M measures the content of criminal thinking (i.e., what a criminal thinks; Simourd & Olver, 2002). The CSS-M utilizes a 3-point Likert-type scale with subscales and the total score being sums of the item scores. Items are scored 2 points if the criminal endorsed an antisocial statement (or rejected of a prosocial statement), 0 points if the criminal rejected an antisocial statement (or accepted of a prosocial statement), and 1 point for undecided responses (Simourd, 1997; Simourd & Olver, 2002). Scoring the CSS-M results in a total score and five subscales: attitude toward the law (Law); attitude toward the Court (Court); attitude toward the police (Police); tolerance for law violations (TLV); and identification with criminal others (ICO; Simourd, 1997; Simourd & Olver, 2002; Simourd & van de Ven, 1999). The first three sub-scales (i.e., Law, Court, Police) are combined to form the Law-Court-Police (LCP) subscale. The LCP subscale assesses the criminals respect for the law and criminal justice system (Simourd & Olver, 2002). The TLV subscale assesses the criminals’ justification for criminal behavior (Simourd & Olver, 2002). The ICO assesses personal evaluative judgments about other criminals (Simourd & Olver, 2002). Higher scores reflect the presence of greater criminal attitudes (Simourd, 1997, Simourd & Olver, 2002). Several studies established the CSS as a reliable and valid instrument for use with adult offenders (Andrews, Wormith, & Kiessling, 1985; Roy & Wormith, 1985; Wormith & Andrews, 1984). The CSS-M has demonstrated equally reliable and valid results. The CSS-M total score has demonstrated adequate to good internal consistency (alpha = .73 and .91, respectively) and the subscales evidenced moderate to high internal consistency, with the following respective alpha levels: Law = .71 and .72, Courts = .74 and .76, Police = .76 and .72, LCP = .73 and .87, TLV = .70 and .76, and ICO = .73 and .51 (Simourd, 1997; Simourd & Olver, 2002). The CSS-M also evidenced good convergent validity with moderate correlations with established measures of criminal risk (e.g., Level of Service Inventory-Revised, General Statistical Information on Recidivism Scale, Hare Psychopathy Checklist-Revised), with correlations ranging between .25 and .37 for the total score (Simourd, 1997). Although correlations for the subscales were lower on some of the measures (i.e., .08), all subscales were significantly correlated to a moderate degree (e.g., .26 to .41) with at least two of the criminal risk measures (Simourd, 1997).
The Millon Clinical Multiaxial Inventory-III (MCMI-III) (Millon, 1994) is a 175-item true-false inventory that measures 14 personality patterns and 10 clinical syndromes, and is consonant with the nosology of the DSM-IV (American Psychiatric Association, 1994). Five clusters of indices comprise the MCMI-III: (1) Modifying Indices assess profile validity (i.e., response style); (2) Clinical Personality Patterns scales measure personality styles; (3) Severe Personality scales evaluate severe forms of the basic personality patterns (i.e., dysfunctional personality patterns); (4) Clinical Syndromes scales assess distortions in the basic personality patterns; and (5) Severe Syndromes scales measure severe symptomatic psychopathology (Van Denburg & Choca, 1997). The MCMI-III has a high concordance with the MCMI-II with correlations among scales ranging from .59 to .88, but with most scales correlating on average between .60 and .80 (Millon, 1994). The MCMI-III is a reliable scale as indicated by test–retest reliability coefficients ranging from .82 to .96 for each scale with a retesting interval ranging between 5 and 14 days (Millon, 1994). Internal consistency estimates are also indicative of good reliability with alpha coefficients ranging from .66 to .90 on the MCMI-III scales (Millon, 1994). Validity of the MCMI-III was established by assessing correlations between MCMI-III scale scores and clinician ratings and collateral test scores. Correlations with clinician ratings were moderate for some scales (e.g., Alcohol Dependence scale [.37], Major Depression scale [.32], Histrionic scale [.31], and Compulsive scale [.30]); however, other scales were less correlated with clinician ratings (e.g., Dependent scale [.07], and Dysthymia and Post-Traumatic Stress Disorder scales [−.07]; Millon, 1994). Furthermore, as discussed in the MCMI-III manual, the MCMI-III scales generally evidenced moderate to strong correlations with other relevant test scores (Millon, 1994) such that the MCMI-III is generally considered a valid clinical instrument. In fact, the MCMI-III ranks as one of the most frequently utilized psychological tests in clinical practice (Piotrowski, 1997).
The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I; First, Spitzer, Gibbon, & Williams, 1997) is a semi-structured interview used for making DSM-IV Axis I Disorders (First et al., 1997). The SCID-I consists of six modules: Module A (Mood Episodes), Module B (Psychotic Symptoms), Module C (Psychotic Disorders), Module D (Mood Disorder), Module E (Substance Use Disorders) and Module F (Anxiety and Other Disorders; First et al., 1997). Questions from the SCID-I are presented to the patient and clinician’s rate (judge) the symptom as positive (+) if the symptom is present, or negative (−) if the symptom is absent (First et al., 1997). The clinician then tabulates the ratings for each diagnosis (within the modules) and indicates whether the diagnosis is present (all diagnostic criteria for the disorder have been met) or absent (all diagnostic criteria for the disorder have not been met; First et al., 1997). According to the User’s Guide (First et al., 1997), the SCID-I is acceptably reliable with test–retest kappa coefficients ranging from .70 to 1.00 for various diagnostic groups. Furthermore, it has been concluded that the SCID-I yields highly reliable diagnoses for most Axis I disorders (Segal, Hersen, & Van Hasselt, 1994). Although validity estimates are difficult to obtain with a semi-structured interview, due to the absence of a valid comparison, Kranzler et al. (1996) were able to demonstrate adequate concurrent and discriminant validity for many Axis I disorders, and moderate predictive validity for substance abuse disorders. Lastly, although the psychometric properties of the SCID-I need to be continually evaluated, it is nevertheless a frequently used diagnostic instrument (Malgady, Rogler, & Tryon, 1992). It should be noted that due to costs and time constraints, the SCID-I was limited to a subsample of randomly selected offenders with mental illness (approximately 20% of the overall sample).
Procedure
Recruitment procedures differed for male and female participants, due to institutional logistical issues and warden preferences. Male participants were housed in a specialized psychiatric/medical unit. Although the male inmate’s diagnosis was not known a priori, the majority of the inmates were placed in this facility due to severe and persistent mental illnesses, with a small percentage of inmates housed for medical reasons. Specific diagnoses were identified during the research process. Research assistants identified potential research participants using “bed-locator sheets” (i.e., daily updated record with information about the inmate(s) assigned to each cell). All inmates listed on the bed-locator sheets were considered for participation with the exception of those placed in seclusion or on Assault Precaution status (i.e., short-term high-risk level). Inmates were selected for recruitment from the bed-locator sheet in successive order, such that the first available inmate (i.e., inmates not already recruited, inmates not on restriction) on the list was recruited for participation. Inmates were retrieved from their cell by an officer and met with a research assistant in a consultation room or day-room. All sessions were conducted individually.
Female participants were recruited from a general population female unit. Prior to data collection, a flyer was posted throughout the unit to elicit research volunteers. This flyer provided information regarding the nature and purpose of the study, including the focus on offenders suffering severe mental illnesses, and instructed potential participants how to submit their request for participation. Additionally, treatment staff (e.g., psychologists, social workers) enlisted inmate volunteers from treatment programs. Research assistants then met individually with each potential participant to secure voluntary consent.
Upon meeting with research participants, each potential participant was provided a verbal overview of the nature and purpose of the current study, informed of their rights as a research participant (e.g., right to withdraw without penalty, rights and procedures to protect confidentiality), and informed of risks and benefits for participating in the study. Inmates that volunteered to participate were provided a written informed consent form and a Federal Certificate of Confidentiality. Inmates were asked to read each document, provided an opportunity to ask questions, and asked to sign the written informed consent document indicating their voluntary consent to participate. Inmates who indicated reading difficulties (e.g., poor reading abilities without access to reading glasses) were read the documents by research assistants.
Inmates who consented to participation were instructed to return the signed written informed consent form and instructed to retain the Federal Certificate of Confidentiality for their records. Participants were then verbally asked, via a structured interview, basic demographic (i.e., age, race, education, relationship status), incarceration (i.e., index offense, sentence length, time served), and mental health information (i.e., current diagnoses, reception of psychological services, current psychotropic medications). Participants were then instructed to complete the research materials (i.e., CSS-M, PICTS, MCMI-III). Research assistants remained with participants during data collection to respond to questions or logistical issues that arose (e.g., participant became emotionally distressed, to ensure confidentiality of responses if participant was approached by prison staff). The CSS-M and PICTS were counterbalanced to control for order effects; however, due to length and concerns regarding attrition, the MCMI-III was always administered after the participant completed both the CSS-M and PICTS. Consistent with the informed consent procedure, participants with reading difficulties were read the items aloud and their responses recorded on the measures by the research assistant.
Research assistants attempted to complete data collection in one uninterrupted data collection session of approximately 2 hours; however, data collection sessions were often interrupted by staff members for medication distribution (i.e., approximately 5 to 10 min interruption) or meals (i.e., approximately 20 to 25 min interruption). In certain instances, inmates who became severely agitated or needed substantially more time to complete the measures (e.g., several inmates required eight or more hours to complete the research materials) were temporarily dismissed and asked to continue at a later time (i.e., typically no longer than a 1-week delay). At the conclusion of each data collection session research assistants rated the participant’s level of cooperation throughout their participation with a 7-point Likert-type scale (1 = argumentative or paranoid to the extent that it inhibited effective completion of materials or responding to items randomly or not completing the majority of items, 7 = motivated to contribute to research efforts and actively engaged in responding to all items), the time the data collection session ended, and other relevant information as warranted (e.g., remarkable/problematic behavior exhibited by the participant, the participant’s questions about the measures or specific items, interruptions during the session).
Participating male inmates’ institutional records were reviewed for supplemental information and to investigate accuracy of self-report data. Following the conclusion of a male participant’s data-collection session, the researcher accessed the participants’ medical chart and recorded the most recent mental health diagnoses in accordance with the DSM-IV (i.e., Axis I through IV, diagnostic labels, diagnostic codes). Initially, medical records at the psychiatric facility were filed as paper charts in a binder which were kept in the nurses’ station in the pod in which the participant was housed. Approximately 1 year into data collection, however, all medical records at the psychiatric facility were scanned and transferred to an electronic database. After this transition, the researchers accessed the participants’ medical records via the facility’s in-house records system. After obtaining the participants’ mental health diagnoses, the researchers accessed TDCJ institutional records (i.e., via a system-wide electronic database) to obtain the participants’ index offense, sentence length, time served, and disciplinary record for their current incarceration. It should be noted that institutional records for female participants were not available for review by researchers.
Inmates who refused to participate in the study were asked to review and sign an alternate consent form indicating their willingness to provide basic demographic, criminal history, and mental health information, as well as an explanation for their refusal to participate in the study. Inmates who consented to provide this information did so verbally, via a brief structured interview, prior to returning to their regularly scheduled activities/location. Inmates who refused to provide this information were immediately dismissed without further prompting for information, and returned to their regularly scheduled activities/location. A research log was maintained to track participants (to avoid duplicating participation requests). For each inmate identified as a potential participant, research assistant transcribed information from the bed-locator sheet including the inmate’s name, TDCJ number, security classification, and the time and date of the recruiting session.
Data Preparation
Prior to conducting data analyses, all participants’ MCMI-III profiles were examined for incomplete profiles and validity issues. The MCMI-III is considered invalid when (1) two or more items from the Validity Index (Scale V) are endorsed (marked true); (2) the Disclosure Index (Scale X) raw score is below 34 or above 178; (3) the Desirability Index (Scale Y) exceeds 75; or (4) the Debasement Index (Scale Z) exceeds 75 (Millon, Davis, & Millon, 1997). If the MCMI-III profile indicated an invalid profile based on review of Scale V, X, Y, or Z, then the participant responses to all instruments were determined to be invalid and the participant was deleted from further data analyses. If results of the MCMI-III validity scales indicated no validity concerns, the participant was determined to have provided valid responses to instruments and remained in the sample. Review of validity indicators, as described above, indicated 91 participants with elevated V scales, 85 with elevated X scales, 6 participants with elevated Y scales and 86 participants with elevated Z scales (note 85 participants produced elevations on multiple validity scales). Thus, 131 participants were removed from further data analyses due to invalidated MCMI-III scale scores. Therefore, the final sample for data analyses included 283 offenders suffering from a mental illness (178 male inmates, 105 female inmates).
To identify systematic differences between participants producing valid and invalid MCMI-III profiles, those producing invalid profiles were compared to participants that producing valid profiles on demographic variables (i.e., age, educational history, race/ethnicity, relationship status, index offense, length of prison sentence, and time served on current sentence). For purposes of this comparison, analysis of variance (ANOVA) procedures for continuous demographic variables, and chi-square procedures, for categorical demographic variables, were utilized to assess for differences between participants that produced valid and invalid MCMI-III profiles. Results indicated that participants providing valid MCMI-III profiles had completed approximately one more year of education (M = 11.4 years) than those producing invalid profiles (M = 10.2 years), F(1, 413) = 16.684, p ≤ .001. Participants providing valid and invalid MCMI-III profiles did not differ (p > .05) with regard to age, race/ethnicity, relationship status, index offense, length of prison sentence, or time served on current prison sentence.
RESULTS
Prevalence of Mental Illness
To confirm that the sample utilized in this study accurately represented a sample of mentally disordered offenders, three sources of data measuring mental illness were obtained. Psychiatric diagnosis was retrieved from inmate mental health files for 178 of the male inmates (as previously noted, medical/mental health files for female inmates were not available). Male inmates participating in this study were diagnosed with a variety of disorders including schizophrenia (22.2%), schizoaffective disorder (12.7%), other psychotic disorders (8.7%), bipolar disorder (17%), major depressive disorder (21.6%), other mood disorders (15.2%), anxiety disorders (i.e., panic disorder, obsessive-compulsive disorder, posttraumatic stress disorder, generalized anxiety disorder; 4.7%), adjustment disorders (10%), impulse control disorders (9.4%), and attention deficit/hyperactivity disorder (3.5%).
The SCID-I was administered to approximately 20% of the sample (n = 61), including 43 males and 18 females. The following psychiatric diagnoses were obtained: schizophrenia (26.2%, n = 16), schizoaffective disorder (4.9%, n = 3), other psychotic disorders (34.4%, n = 21), bipolar disorder (14.8%, n = 9), major depressive disorder (47.5%, n = 29), other mood disorder (4.9%, n = 3), anxiety disorders (75.4%, n = 46), adjustment disorder (1.6%, n = 1), attention deficit/hyperactivity disorder (1.6%, n = 1), and other diagnoses (26.2%, n = 16).
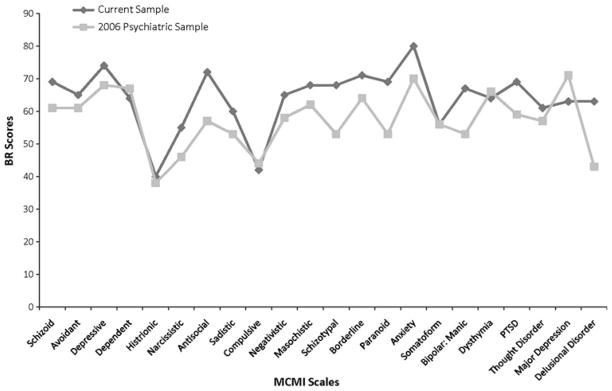
MCMI-III profiles were examined for psychiatric symptomatology (note 20 participants did not produce complete profiles and, thus, were not included in these analyses). The MCMI-III Clinical Personality Pattern scales measure stable and pervasive personality patterns (Millon et al., 1997) and, not surprisingly, 96.1% (n = 250; 91.8% [n = 146] male and 100% [n = 104] female, respectively) offenders elevated at least one Clinical Personality Pattern scale. The Severe Personality Pathology scales measure more maladaptive levels of personality functioning (Millon et al., 1997), and 66% (n = 104) of male offenders and 73.1% (n = 76) of female offenders elevated at least one of the three Severe Personality Pathology scales. Five of the Clinical Syndrome Scales were of interest in the study (alcohol and drug dependence scales were dropped from consideration) and 91.8% (n = 146) male offenders and 80.8% (n = 84) of female offenders elevated at least one scale indicating transient symptoms indicative of DSM-IV Axis I disorders (McCann & Dyer, 1996). Finally, 50% (n = 78) of male offenders and 55.8% (n = 58) of female offenders elevated one of the three Severe Clinical Syndrome Scales indicating the presence of severe psychopathology with debilitating symptomatology (McCann & Dyer, 1996). Figure 1 presents a comparison of inmate participants in this study with a comparison group of psychiatric inpatients (Schoenberg, Dorr, & Morgan, 2006). It should be noted that the comparison group of psychiatric inpatients consisted of male and female patients; therefore, male and female offenders in this study are presented together as well. As evidenced in Fig. 1, mentally disordered inmates in this study presented symptomatology similar to psychiatric inpatients, with noticeable exceptions of increased antisocial, schizotypal and paranoid personality patterns, bipolar (manic), post-traumatic stress, and delusional disorder symptomatology.
Fig. 1.
Comparison of mentally ill inmate’s MCMI-III scores with a psychiatric inpatient sample from Schoenberg et al. (2006)
Prevalence of Criminal Thinking
The PICTS Composite Scales measure the presence of “overt criminal thinking” (Walters, 2006, p. 42; T-scores ≥ 55 are clinically significant). Sixty-six percent (n = 186) of offenders with mental illness endorsed a belief system that is supportive of a criminal lifestyle. Specifically, 48% of male participants endorsed a proactive criminal thought process characterized by goal-directed criminal activity with the expectation of positive (gained) outcomes (M Proactive Scale Score = 55.6, SD = 11.1), whereas 66% endorsed a reactive cognitive process characterized by impulsivity, hostility, and emotionality (M Reactive Scale Score = 60.4, SD = 11). Female participants produced slightly lower percentages of criminal belief system as 39% and 49%, respectively, endorsed proactive and reactive criminal thought processes (M Pro-active Scale Score = 51.6, SD = 11.3; M Reactive Scale Score = 53.8, SD = 9.2).
As noted above, the PICTS includes eight Thinking Style Scales; Walters developed his conception of criminal thinking by delineating eight related yet distinct criminal thinking styles which encapsulate the self-serving, impulsive, antisocial, and interpersonally intrusive nature of criminals’ cognitive patterns (Walters, 1990). T-scores of 60 or higher are considered clinically significant. Mentally ill male and female inmates in this study, on average, did not elevate any of the eight Thinking Style Scales (mean range of T-scores = 49.2–58.3) with the exceptions that male participants elevated, on average, the Cutoff (M = 60.9, SD = 11.3) and Discontinuity (M = 60, SD = 10.8). Although only two scales were elevated by male offenders suffering mental illness and none by female offenders, 71% of participants elevated at least one of the eight Thinking Style Scales. Regarding the individual thinking style scales, 37% of male and 22% of female participants elevated the Mollification scale, a measure of an offender’s tendency to blame external factors (e.g., family, social economic status, government) for one’s criminal behavior. Fifty-two percent of male offenders and 31% of female offenders elevated a scale measuring emotional control (e.g., “hot temper”) with a propensity to maintain a “screw it” approach to dealing with problems (Cutoff scale). The Entitlement scale is a measure of “ownership, privilege, and uniqueness” (Walters, 2006, p. 44), and 26% and 17% of male and female offenders with mental illness, respectively, endorsed this scale, suggesting the belief that others (e.g., society) “owe them,” and that their uniqueness affords them the right to take what they want. Forty-eight percent of male participants and 23% of female participants endorsed items suggesting the need for power and control (Power Orientation). Sentimentality is characterized by superficial concern with lack of insight regarding harm they might cause, such that one’s criminal behaviors are believed to be in the best interest of others; 30% and 19% of male and female participants, respectively, elevated this scale. Thirty percent of male and 19% of female offenders with mental illness believe they can engage in criminal acts and avoid negative consequences for their actions (Superoptimism scale). Cognitive Indolence refers to the lack of reasoning skills resulting in offenders taking “short-cuts” around problems and 48% and 31% of male and female participants, respectively, elevated this scale. Finally, Discontinuity is characterized by lack of direction such that offenders are easily distracted and subsequently lose sight of goals; 51% of male participants and 31% of female participants elevated the Discontinuity scale.
Two Content Scales are also relevant for purposes of this study. The Current Criminal Thinking scale identifies current identification with a criminal belief system; the Historical Criminal Thinking scale, on the other hand, captures individuals’ identification with a criminal belief system in the past. With a T-score cutoff of ≥60, male offenders with mental illness elevated the Current Criminal Thinking Scale (M = 60.3, SD = 10.9), but not the Historical Criminal Thinking Scale (M = 56, SD = 10.9); however, 50% of male participants currently identified with a criminal belief system and 37% of male participants endorsed a historical identification with a criminal belief system. Female offenders with mental illness did not elevate either the Current or Historical Criminal Thinking Scales (M = 54.1, SD = 9.2, M = 51.7, SD = 10.6, respectively), but 35% elevated the Current- and 28% elevated the Historical Criminal Thinking Scale.
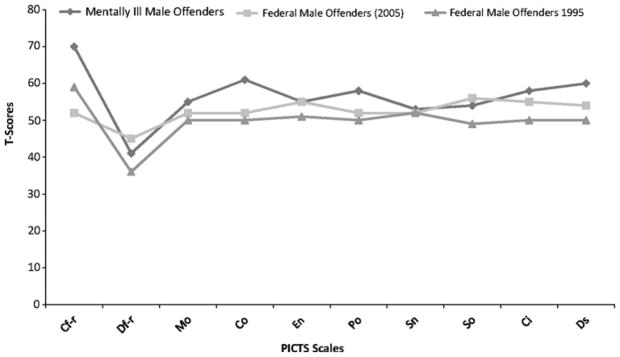
When compared to other offender samples (Walters, 1995; Walters & Geyer, 2005), mentally disordered male offenders in this study scored similarly or higher on each of the PICTS scales than non-mentally disordered offenders in two separate correctional samples (see Fig. 2).
Fig. 2.
Comparison of mentally ill male inmate’s PICTS scales with two samples of non-mentally ill male prison samples from Walters (1995) and Walters and Geyer (2005), respectively
The CSS-M Total raw score, an overall measure of criminal attitudes and behavior, includes a clinical cut off of 19, with an average of 34 and 26 for male and female offenders with mental illness, respectively, participating in this study (scores ≥ 30 are considered “high;” Commonwealth of Pennsylvania Department of Corrections, 2006). Not surprising, given the mean total score, 85% of male participants and 72.4% of female participants produced an elevated total score indicating antisocial attitudes, values, and beliefs related to criminal activity. Figure 3 presents CSS-M scale scores for male and female offenders with mental illness from the current sample and a non-mentally ill offender samples (Simourd & Olver, 2002), and offenders with mental illness in this study produced higher scores on all but one scale (Identification with Criminal Others) of the CSS-M compared to offenders not suffering from mental illnesses.
Fig. 3.
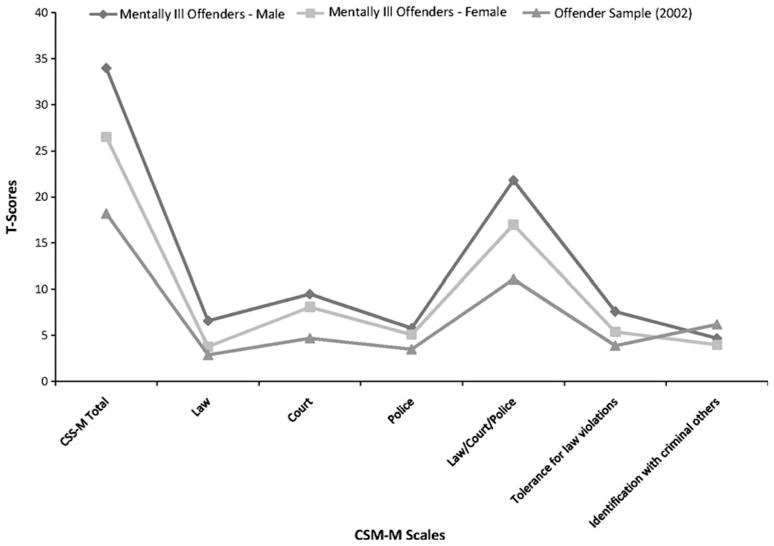
Comparison of CSS-M scale scores for male and female offenders with mental illness with a non-mentally ill offender sample (Simourd & Olver, 2002)
DISCUSSION
The purpose of this study was to examine the prevalence of mental illness and criminal thinking and attitudes in a population of offenders suffering from mental illness. Similar to the “chicken or the egg” debate, this study sought to clarify whether mentally ill inmates are psychiatric patients that end up in the criminal justice system, or whether they are criminals that happen to be mentally ill. Consistent with Hiday (1999) and Morgan, Kroner, and Mills (2008) hypotheses, the results of this study indicated that mentally ill inmates presented with severe mental illness and psychiatric symptomatology comparable to that of non-inmate psychiatric populations as well as criminal thinking comparable to non-mentally ill inmates (with the exception that contrary to results of Walters et al., 1998, female offenders in this study did not produce higher scores on scales of criminal thinking when compared to their male counterparts). In other words, contrary to previous speculations (e.g., Fisher et al., 2006), mentally ill inmates present similarly to psychiatric patients and criminals with co-occurring issues of mental illness and “criminalness” (behavior that violates the rights and wellbeing of others and may or may not lead to arrestable offenses; Morgan et al., 2008).
With respect to psychiatric illness, it has been speculated that there is minimal discrepancy between psychiatric symptomatology presented by mentally ill offenders in the criminal justice system and mentally ill offenders in mental health settings such as psychiatric hospitals (Quinsey, Harris, Rice, & Cormier, 1998). The results of this study support Quinsey et al.’s hypothesis. As expected, the majority (i.e., 92%) of inmate participants in this study were diagnosed with a severe mental illness (i.e., Schizophrenia, Schizoaffective Disorder, Delusional Disorder, Other Psychotic Disorder, Bipolar Disorder, Major Depressive Disorder, or other Mood Disorder; 92%). It was also of no surprise that almost all of the participants in this study endorsed clinically significant symptoms of mental illness, with MCMI-III clinical profiles similar to that of psychiatric patients; however, it was not expected that 80% of inmates would endorse clinically significant anxiety. Although it is commonly accepted that stress is a byproduct of imprisonment (e.g., Hassine, 1996; Toch, 1992), the fact that 80% of inmates endorsed clinically significant levels of anxiety presents concerns regarding issues of co-morbidity. Anxiety exacerbates other mental illnesses such as thought disorders and severe mood disorders (see Lysaker & Salyers, 2007); thus, correctional mental health professionals treating mentally disordered offenders must be cognizant of heightened anxiety as a co-morbidity issue. Future research should examine the effects of imprisonment as a precursor to anxiety and subsequently a risk factor for mental health functioning of incarcerated mentally ill offenders.
Criminal thinking and attitudes have long been recognized as risk factors for recidivism. In fact, criminal thinking and attitudes is one of the “Central Eight” risk factors for future criminal behavior (Andrews & Bonta, 2006). Thus, finding that mentally disordered offenders scored as high as or higher than non-mentally disordered offenders on measures of criminal thinking (PICTS) and criminal attitudes (CSS-M) suggest that these individuals are, in fact, criminals warranting placement in the criminal justice system. In other words, mentally disordered offenders are not merely mentally ill individuals unable to survive without breaking the law, rather, these mentally ill individuals appear to think and process information as criminals. Although the criminal justice system has become the “defacto mental health system” (e.g., Holton, 2003; Wilson & Draine, 2006), a notion that offending among persons with serious mental illness is principally a function of their psychiatric symptomatology would be inaccurate. In fact, mentally disordered offenders in this study endorsed criminal thinking at a rate consistent with incarcerated offenders who are not mentally ill (see Walters, 1995; Walters & Geyer, 2005). Thus, correctional mental health professionals providing rehabilitation services (i.e., services designed to reduce criminal recidivism; e.g., Morgan, Winterowd, & Ferrell, 1999) must target criminogenic risk factors (dynamic attributes of offenders that are predictive of future criminal conduct; Andrews & Bonta, 2003).
The results of this study demonstrated that mentally disordered offenders in state correctional facilities are both mentally ill psychiatric patients and criminals. Thus, treatment providers must consider co-occurring issues of mental illness and criminalness. Not surprisingly, the co-occurring problems of mental illness and criminalness and their respective treatment needs present a unique challenge to mental health professionals. Morgan et al. (2008) recommend practitioners conceptualize mental illness and criminalness as co-occurring therapeutic issues, similar to practitioners treating co-occurring mental illness and substance abuse. Steadman (1992) noted the necessity of spanning boundaries of mental health services that work within the criminal justice system. Thus, consistent with treating co-occurring mental illness and substance use disorders, the findings of this study emphasize the importance of treating both mental illness and criminalness simultaneously and in a seamless manner (see Essock et al., 2006).
Correctional policy makers and administrators must also recognize the co-occurring issues of mental illness and criminalness. That is, while developing special housing (e.g., the psychiatric inpatient correctional facility sampled in this study) or treatment programming to meet the special needs of the mentally disordered population, policy makers and administrators must remain cognizant of the criminal rehabilitation needs of this population. That is, in addition to psychiatric and mental health staffing needs, consideration must also be given to correctional mental health professionals trained to provide correctional rehabilitation aimed at reducing criminal recidivism.
Although we believe that the results of this study are informative, specifically for highlighting the mental health and correctional rehabilitation needs of mentally disordered offenders, this study is not without limitations. Of primary concern is the absence of control groups consisting of mentally ill psychiatric patients or non-mentally disordered offenders to allow for direct comparisons. In particular, the absence of a control group does not allow for the investigation of alternative hypothesis, such as the possibility that mentally ill individuals present thinking patterns that are similar to criminals. Although it is also possible that prisonization contributed to increased criminal thinking as indicated by Walters (2003), this is not likely as participants in this study were not naïve inmates as were those experiencing a prisonization effect in Walters study; nevertheless, future studies with control procedures need to clarify this and other alternative hypotheses. Additionally, this study was limited to adults incarcerated in one state’s correctional system. Thus, generalizability to other incarcerated offenders (e.g., federal inmates, juveniles, offenders in jail facilities) is unknown. Future studies should address these limitations by examining issues of mental illness and criminal thinking in comparison samples and with other samples of offenders (e.g., federal inmates). Future research should also examine interactions between mental illness and levels or subtypes of criminal thinking (e.g., do subtypes of criminal thinking differ with severity or type of mental illness?). Additionally, future research should examine if criminal thinking can differentiate between criminal thinking this is inherently criminal versus criminal thinking that is secondary to other etiological factors (e.g., psychopathology, socioeconomic status). Finally, future studies should examine other criminal risk factors (e.g., criminal associates) and risk factors that are likely co-morbid for both mental illness and criminalness (e.g., substance abuse, family and/or marital relations, school/work functioning, socioenvironmental factors) to further identify specific treatment needs of this particular inmate population.
In spite of these limitations, the results provide important information for practitioners and administrators working with mentally disordered offenders. Specifically, the results of this study contribute to the debate regarding whether mentally disordered offenders are psychiatric patients who ended up in the criminal justice system as either a direct or indirect result of their psychiatric symptomatology, or whether at least some have characteristics which predispose them to criminal behaviors co-occurring with, but largely independent of, their psychiatric illnesses. These data suggest that the latter group may be larger than is generally assumed by those designing current interventions for this population, which mainly stress the provision of mental health services and generally overlook non-psychiatrically related risk factors for offending. This group poses a challenge. They present with a myriad of symptoms and diagnoses similar to psychiatric patients, as well as criminal thinking and attitudes consistent with offenders that endorse the criminal lifestyle, factors which are targets for intervention in the general offending population.
The data presented here suggest a new approach to addressing the problem of offending among persons with serious mental illness. Developing such an approach requires that we learn to do two things. First, it is important to implement protocols for identifying those arrestees and correctional inmates with psychiatric disorders who have co-occurring criminal thinking patterns. This could be done using the instruments (i.e., PICTS, CSS-M) used in this prevalence study, and could be accomplished at any of the various intercept points in the criminal justice process described by Munetz and Griffin (2006). Screenings, as recommended by Munetz and Griffen, might be introduced as part of the routine mental health service assessments provided individuals who are diverted from the criminal justice to the mental health system.
The second step is to determine if and to what extent treatment approaches for criminal thinking provided to persons in the general offender population are effective for persons who have serious psychiatric disorders. If they are determined to be effective or effective for a subset of the population, efforts should be made to integrate this treatment with existing psychiatric treatment protocols, in much the same way as treatments for co-occurring behavioral disorders have been blended. Thus, analogous to Drake and colleagues’ conclusions regarding the treatment of co-occurring substance abuse and mental illness (Drake, Yovetich, Bebout, Harris, & Mchugo, 1997; Drake & Mueser, 2000; Drake, Becker, Bond, & Mueser, 2003), systems must consider a comprehensive and integrated intervention rather than parallel or sequential intervention models.
The studies cited in the introduction to this paper suggest that we need to develop new ways of approaching the justice system’s involvement among persons with mental illness. Intensive, targeted treatment and service delivery approaches have not proven to be sufficiently preventive, nor has psychiatric treatment by itself. The data presented here indicate that we need to focus more on individuals’ criminal and antisocial propensities independently of their psychiatric illnesses. That said, however, the monumental efforts undertaken by mental health service and correctional agencies to address offending among persons with mental illness have established service system interventions which may prove to be the ideal platforms for addressing this critical problem.
Acknowledgments
This study was funded by the National Institute of Mental Health (R34 MH070401-01A1). The research contained in this document was coordinated in part by the Texas Department of Criminal Justice (Project Number 475-R05). The contents of this manuscript reflect the views of the authors and do not necessarily reflect the views or policies of the Texas Department of Criminal Justice.
Contributor Information
Robert D. Morgan, Email: robert.morgan@ttu.edu, Texas Tech University, Lubbock, USA
William H. Fisher, University of Massachusetts Medical School, Worcester, USA
Naihua Duan, Columbia University, New York, USA.
Jon T. Mandracchia, Texas Tech University, Lubbock, USA
Danielle Murray, Texas Tech University, Lubbock, USA.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Andrews DA, Bonta J. The psychology of criminal conduct. 3. Cincinnati, OH: Anderson Publishing Company; 2003. [Google Scholar]
- Andrews DA, Bonta J. Psychology of criminal conduct. 4. Cincinnati, OH: Anderson Publishing; 2006. [Google Scholar]
- Andrews DA, Wormith JS, Kiessling JJ. Solicitor General Canada. 1985. Self-reported criminal propensity and criminal behavior: Threats to the validity of assessments of attitudes and personality. [Google Scholar]
- Andrews DA, Zinger I, Hodge RD, Bonta J, Gendreau P, Cullen FT. Does correctional treatment work? A clinically relevant and psychologically informed meta-analysis. Criminology. 1990;28:369–404. doi: 10.1111/j.1745-9125.1990.tb01 330.x. [DOI] [Google Scholar]
- Bonta J, Law M, Hanson K. The prediction of criminal and violent recidivism among mentally disordered offenders: A meta-analysis. Psychological Bulletin. 1998;123:123–142. doi: 10.1037/0033-2909.123.2.123. [DOI] [PubMed] [Google Scholar]
- Commonwealth of Pennsylvania Department of Corrections. Risk and needs assessment guidelines. 2006 http://www.cor.state.pa.us/bis/lib/bis/Risk_and_Needs_Assessment_Guidelines.pdf. Retrieved 13 March 2008.
- Desai RA, Lam J, Rosenheck RA. Childhood risk factors for criminal justice involvement in a sample of homless people with serious mental illness. The Journal of Nervous and Mental Disease. 2000;188:324–332. doi: 10.1097/00005053-20000 6000-00002. [DOI] [PubMed] [Google Scholar]
- Drake RE, Becker DR, Bond GR, Mueser KT. A process analysis of integrated and non-integrated approaches to supported employment. Journal of Vocational Rehabilitation. 2003;18:51–58. [Google Scholar]
- Drake RE, Mueser KT. Psychosocial approaches to dual diagnosis. Schizophrenia Bulletin. 2000;26:105–118. doi: 10.1093/oxfordjournals.schbul.a033429. [DOI] [PubMed] [Google Scholar]
- Drake RE, Yovetich NA, Bebout RR, Harris M, Mchugo G. Integrated treatment for dually diagnosed homeless adults. The Journal of Nervous and Mental Disease. 1997;185:298–305. doi: 10.1097/00005053-199705000-00003. [DOI] [PubMed] [Google Scholar]
- Essock SM, Mueser KT, Drake RE, Covell NH, McHugo GJ, Frisman LK, et al. Comparison of ACT and standard case management for delivering integrated treatment for co-occurring disorders. Psychiatric Services (Washington, DC) 2006;57:185–196. doi: 10.1176/appi.ps.57.2.185. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I Disorders (SCID-I): Clinical version. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Fisher WH, Silver E, Wolff N. Beyond criminalization: Toward a criminologically-informed mental health policy and services research. Administration & Policy in Mental/Health & Mental Health Services Research. 2006;33:544–557. doi: 10.1007/s10488-006-0072-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gendreau P. Offender rehabilitation: What we know and what needs to be done. Criminal Justice and Behavior. 1996;23:144–161. doi: 10.1177/0093854896023001010. [DOI] [Google Scholar]
- Hartwell SW, Orr K. The Massachusetts forensic transition program for mentally ill offenders re-entering the community. Psychiatric Services (Washington, DC) 1999;50:1220–1222. doi: 10.1176/ps.50.9.1220. [DOI] [PubMed] [Google Scholar]
- Hassine V. Life without parole. Los Angeles: Roxbury Publishing; 1996. [Google Scholar]
- Hiday VA. Mental illness and the criminal justice system. In: Horwitz AV, Scheid TL, editors. A handbook for the study of mental health: Social context, theories, and systems. New York: Cambridge University Press; 1999. pp. 508–525. [Google Scholar]
- Holton SMB. Managing and treating mentally disordered offenders in jails and prisons. In: Fagan T, Ax RK, editors. Correctional mental health handbook. Thousand Oaks, CA: Sage Publications; 2003. pp. 101–122. [Google Scholar]
- Kranzler HR, Kadden RM, Babor TF, Tennen H. Validity of the SCID in substance abuse patients. Addiction (Abingdon, England) 1996;91:859–868. doi: 10.1111/j.1360-0443.1996.tb03580.x. [DOI] [PubMed] [Google Scholar]
- Laberge D, Morin D. The overuse of criminal justice dispositions: Failure of diversionary policies in the management of mental health problems. International Journal of Law and Psychiatry. 1995;18:389–414. doi: 10.1016/0160-2527(95)00019-E. [DOI] [PubMed] [Google Scholar]
- Lamb HR, Weinberger LE. Persons with severe mental illness in jails and prisons: A review. Psychiatric Services (Washington, DC) 1998;49:483–492. doi: 10.1176/ps.49.4.483. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Salyers MP. Anxiety symptoms in schizophrenia spectrum disorders: Associations with social function, positive and negative symptoms, hope and trauma history. Acta Psychiatrica Scandinavica. 2007;116:290–298. doi: 10.1111/j.1600-0447.2007.01067.x. [DOI] [PubMed] [Google Scholar]
- Malgady RG, Rogler LH, Tryon WW. Issues of validity in the diagnostic interview schedule. Journal of Psychiatric Research. 1992;26:59–67. doi: 10.1016/0022-3956(92)90 016-H. [DOI] [PubMed] [Google Scholar]
- McCann JT, Dyer FJ. Forensic assessment with the Millon inventories. New York: Guilford Press; 1996. [Google Scholar]
- Millon T. Millon clinical multiaxial inventory-III manual. Minneapolis, MN: National Computer Services; 1994. [Google Scholar]
- Millon T, Davis R, Millon C. Millon clinical multiaxial inventory-III manual. 2. Minneapolis, MN: National Computer Services; 1997. [Google Scholar]
- Moran P, Hodgins S. The correlates of antisocial personality disorder in schizophrenia. Schizophrenia Bulletin. 2004;30:791–802. doi: 10.1093/oxfordjournals.schbul.a007132. [DOI] [PubMed] [Google Scholar]
- Morgan RD, Kroner DG, Mills JF. Treating the mentally disordered offender: A model and guide for empirically supported practice. New York: Oxford University Press; 2008. Manuscript under contract. [Google Scholar]
- Morgan RD, Winterowd CL, Ferrell SW. A national survey of group psychotherapy services in correctional facilities. Professional Psychology, Research and Practice. 1999;30:600–606. doi: 10.1037/0735-7028.30.6.600. [DOI] [Google Scholar]
- Morrissey JP, Meyer P, Cuddeback G. Extending ACT to criminal justice settings: Origins, current evidence and future directions. Community Mental Health Journal. 2007;43:527–544. doi: 10.1007/s10597-007-9092-9. [DOI] [PubMed] [Google Scholar]
- Mueser KT, Cricker AG, Frisman LB, Drake RE, Covell NH, Essock SM. Conduct disorder and Antisocial Personality Disorder in persons with severe psychiatric and substance abuse disorders. Schizophrenia Bulletin. 2006;32:626–636. doi: 10.1093/schbul/sbj068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munetz MR, Griffin PA. Use of the sequential intercept model as an approach to decriminalization of people with serious mental illness. Psychiatric Services. 2006;57:544–549. doi: 10.1176/ps.2006.57.4.544. [DOI] [PubMed] [Google Scholar]
- Piotrowski C. The use of the Millon Clinical Multiaxial Inventory in clinical practice. Perceptual and Motor Skills. 1997;84:1185–1186. doi: 10.2466/pms.1997.84.3c.1185. [DOI] [PubMed] [Google Scholar]
- Quinsey VL, Harris GT, Rice ME, Cormier CA. Mentally disordered offenders. In: Quincy VL, Harris GT, Rice ME, Cormier CA, editors. Violent offenders: Appraising and managing risk. Washington, DC: American Psychological Association; 1998. pp. 75–101. [Google Scholar]
- Randolph F, Blasinsky M, Morrissey JP, Rosenheck RA, Cocozza J, Goldman HH, et al. Overview of the ACCESS program. Psychiatric Services (Washington, DC) 2002;53:945–948. doi: 10.1176/appi.ps.53.8.945. [DOI] [PubMed] [Google Scholar]
- Robins LN. Childhood conduct problems, adult psychopathology and crime. In: Hodgins S, editor. Mental disorder and crime. London: Sage Publications; 1993. pp. 173–193. [Google Scholar]
- Roy RE, Wormith JS. The effects of incarceration: Measuring criminal sentiments. Ottawa: Ministry of the Solicitor General of Canada; 1985. [Google Scholar]
- Schoenberg MR, Dorr D, Morgan CD. Development of discriminant functions to detect dissimulation for the Millon Clinical Multiaxial Inventory (3rd ed.) Journal of Forensic Psychiatry & Psychology. 2006;17:405–417. doi: 10.1080/147899406 00761394. [DOI] [Google Scholar]
- Segal DL, Hersen M, Van Hasselt VB. Reliability of the structured clinical interview for DMS-III-R: An evaluative review. Comprehensive Psychiatry. 1994;35:316–327. doi: 10.1016/0010-440X(94)90025-6. [DOI] [PubMed] [Google Scholar]
- Simourd DJ. The Criminal Sentiments Scale-Modified and Pride in Delinquency Scale: Psychometric properties and construct validity of two measures of criminal attitudes. Criminal Justice and Behavior. 1997;24:52–70. doi: 10.1177/00938 54897024001004. [DOI] [Google Scholar]
- Simourd DJ, Olver ME. The future of criminal attitudes research and practice. Criminal Justice and Behavior. 2002;29:427–446. doi: 10.1177/0093854802029004005. [DOI] [Google Scholar]
- Simourd DJ, Van De Ven J. Assessment of criminal attitudes: Criterion-related validity of the Criminal Sentiments Scale-Modified and Pride in Delinquency Scale. Criminal Justice and Behavior. 1999;26:90–106. doi: 10.1177/0093854899 026001005. [DOI] [Google Scholar]
- Steadman HJ. Boundary spanners: A key component for the effective interaction of the justice and mental health systems. Law and Human Behavior. 1992;16:75–87. doi: 10.1007/BF02351050. [DOI] [Google Scholar]
- Steadman HJ, Deane MW, Morrissey JP, Westcott ML, Salasin S, Shapiro S. A SAMHSA research initiative assessing the effectiveness of jail diversion programs for mentally ill persons. Psychiatric Services (Washington, DC) 1999;50:1620–1623. doi: 10.1176/ps.50.12.1620. [DOI] [PubMed] [Google Scholar]
- Steadman HJ, Morris SM, Dennis DL. The diversion of mentally ill persons from jails to community-based services: A profile of programs. American Journal of Public Health. 1995;85:1630–1635. doi: 10.2105/AJPH.85.12.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA. The prevalence of severe mental disorders among male urban jail detainees. American Journal of Public Health. 1990;80:663–669. doi: 10.2105/AJPH.80.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM. Prevalence of psychiatric disorders among incarcerated women jail detainees. Archives of General Psychiatry. 1996;53:505–512. doi: 10.1001/archpsyc.1996.01830060047007. [DOI] [PubMed] [Google Scholar]
- Texas Department of Criminal Justice. Fiscal year 2005: Executive summary. 2006 Retrieved March 15, 2006 from http://www.tdcj.state.tx.us/publications/executive/FY2005_Statistical_Report.pdf.
- Toch H. Mosaic of despair: Human breakdowns in prison. Washington, DC: American Psychological Association; 1992. Rev. [Google Scholar]
- Torrey EF. Editorial: Jails and prisons—America’s new mental hospitals. American Journal of Public Health. 1995;85:1611–1613. doi: 10.2105/AJPH.85.12.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Denburg EJ, Choca JP. Interpretation of the MCMI-III. In: Millon T, editor. The Millon inventories: Clinical and personality assessment. New York: Guilford Press; 1997. pp. 41–58. [Google Scholar]
- Walters GD. The criminal lifestyle: Patterns of serious criminal conduct. Newbury Park: Sage Publications; 1990. [Google Scholar]
- Walters GD. The Psychological Inventory of Criminal Thinking Styles. Part I. Reliability and preliminary validity. Criminal Justice and Behavior. 1995;22:307–325. doi: 10.1177/0093854895022003008. [DOI] [Google Scholar]
- Walters GD. The Psychological Inventory of Criminal Thinking Styles: Part III. Predictive validity. International Journal of Offender Therapy and Comparative Criminology. 1996;40:105–112. doi: 10.1177/0306624X96402003. [DOI] [PubMed] [Google Scholar]
- Walters GD. The Psychological Inventory of Criminal Thinking Styles (PICTS): A review and meta-analysis. Assessment. 2002;9:278–291. doi: 10.1177/1073191102009003007. [DOI] [PubMed] [Google Scholar]
- Walters GD. Changes in criminal thinking and identity in novice and experienced inmates. Criminal Justice and Behavior. 2003;30:399–421. doi: 10.1177/0093854803253137. [DOI] [Google Scholar]
- Walters GD. The Psychological Inventory of Criminal Thinking Styles (PICTS) professional manual. Allentown, PA: Center for Lifestyle Studies; 2006. [Google Scholar]
- Walters GD, Elliott WN, Miscoll D. Use of the Psychological Inventory of Criminal Thinking Styles in a group of female offenders. Criminal Justice and Behavior. 1998;25:125–134. doi: 10.1177/0093854898025001008. [DOI] [Google Scholar]
- Walters GD, Geyer MD. Construct validity of the Psychological Inventory of Criminal Thinking Styles in relationship to the PAI, disciplinary adjustment, and program completion. Journal of Personality Assessment. 2005;84:252–260. doi: 10.1207/s15327752jpa8403_04. [DOI] [PubMed] [Google Scholar]
- Walters GD, Mandell W. Incremental validity of the Psychological Inventory of Criminal Thinking Styles and Psychopathy Checklist: Screening version in predicting disciplinary outcome. Law and Human Behavior. 2007;31:141–157. doi: 10.1007/s10979-006-9051-y. [DOI] [PubMed] [Google Scholar]
- Walters GD, Schlauch C. The Psychological Inventory of Criminal Thinking Styles and Level of Service Inventory-Revised: Screening version as predictors of official and self-reported disciplinary infractions. Law and Human Behavior. 2008;32:454–462. doi: 10.1007/s10979-007-9117-5. [DOI] [PubMed] [Google Scholar]
- Weiner DB. The madman in the light of reason: Enlightenment psychiatry. In: Wallace ER, Gach J, editors. History of psychiatry and medical psychology: With an epilogue on psychiatry and the mind-body relation. New York: Springer; 2008. pp. 255–277. [Google Scholar]
- Wilson AB, Draine J. Collaborations between criminal justice and mental health systems for prisoner reentry. Psychiatric Services (Washington, DC) 2006;57:875–878. doi: 10.1176/appi.ps.57.6.875. [DOI] [PubMed] [Google Scholar]
- Wormith JS, Andrews DA. Criminal sentiments and criminal behavior: A construct validation. Ottawa: Solicitor General Canada; 1984. [Google Scholar]
- Yochelson S, Samenow SE. The criminal personality volume I: A profile for change. New York: Jason Aronson; 1976. [Google Scholar]