Abstract
OBJECTIVES
Evidence suggests an association between maternal vitamin C levels and preterm premature rupture of membranes (PROM) or preterm labor. The objective of this study was to estimate whether maternally administered vitamins C and E lowers the risk of spontaneous preterm birth (SPB).
METHIODS
This is a secondary analysis of a randomized, double-masked, placebo-controlled trial in low-risk nulliparous women administered 1000 mg vitamin C and 400 IU vitamin E or placebo daily from 9-16 weeks’ gestation until delivery. Outcomes include preterm birth due to PROM and total spontaneous preterm births (SPB due to PROM or spontaneous labor).
RESULTS
Of the 10,154 women randomized, outcome data were available on 9,968 (4,992 vitamin group and 4,976 placebo group). 1,038 women (10.4%) delivered preterm of whom 698 (7.0%) had a SPB. A SPB occurred in 356 women (7.1%) assigned to daily vitamin C/E suplementation and in 342 (6.9%) assigned to placebo. There were 253 women (2.5%) delivered after preterm PROM and 445 (4.5%) after a spontaneous preterm labor. In women supplemented with vitamins C and E, births attributed to preterm PROM were similar at less than 37 and 35 weeks gestation but were less frequent before 32 weeks gestation (0.3% vs. 0.6% adjusted OR 0.3-0.9). However, total spontaneous preterm births across gestation in women supplemented with vitamins C and E or a placebo were similar.
CONCLUSION
Maternal supplementation with vitamins C/E beginning at 9 to 16 weeks gestation in low risk nulliparous women did not reduce spontaneous preterm births. (Clinical Trials.gov number NCT00135707)
Birth prior to 37 weeks gestation (preterm) has increased since 1990 and was 12.7% of all births in the U.S. in 2007.(1) There has been consistency among reports that about one-fourth of preterm births are indicated due to various factors, primarily maternal hypertensive conditions, and three-fourths occur spontaneously with or without preterm premature ruptured membranes (PROM).(2-3) In all women with a spontaneous preterm birth, the contribution of premature membrane rupture has been estimated to be up to one-third with two-thirds due to spontaneous labor.(4) Preterm premature membrane rupture has been associated with many factors, including ascorbic acid deficiency (vitamin C).(4-7) These observations are of great importance because if vitamin C supplementation reduces the occurrence of preterm PROM a deficiency of vitamin C is a modifiable risk factor and supplementation would be a corrective interventional behavior.
Our intent was to further assess the hypothesis that daily maternal antioxidant supplementation with vitamins C and E from early pregnancy would reduce the incidence of spontaneous preterm birth due to either spontaneous labor or preterm PROM. To test this hypothesis we accomplished a secondary analysis of the NICHD Maternal-Fetal Medicine Units Network multicenter randomized, double-masked trial of low risk nulliparas assigned to daily vitamin C and E supplementation or matching placebo to reduce adverse outcomes due to pregnancy associated hypertension.(8)
MATERIALS AND METHODS
The trial was conducted at the sixteen clinical centers that were members of the Eunice Kennedy Shriver National Institutes of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network between 2003 and 2008. Full details of the study design and technique of data collection have been previously described.(8) Women with a singleton pregnancy between 9 weeks 0 days and 16 weeks 6 days of gestation were eligible if they had not experienced a prior pregnancy lasting beyond 19 weeks 6 days. Gestational age was determined before randomization by a previously described algorithm(9) using the date of the last menstrual period (if reliable) and results of the earliest ultrasound examination. Women were not eligible if they had elevated systolic (135 mm Hg or higher) or diastolic (85 mm Hg or higher) blood pressure or proteinuria (at least 300 mg by 24-hour urine collection or 1+ protein by dipstick), were prescribed antihypertensive medication, or were taking more than 150 mg vitamin C or more than 75 IU vitamin E daily. Other exclusion criteria were pregestational diabetes, treatment with antiplatelet drugs or nonsteroidal anti-inflammatory agents, uterine bleeding within the week prior to recruitment, uterine malformation, serious medical complication, known fetal anomaly or aneuploidy, in vitro fertilization resulting in the current pregnancy, or illicit drug or alcohol abuse. Eligible and consenting women were randomly assigned to capsules containing a combination of 1000 mg vitamin C (ascorbic acid) and 400 IU of vitamin E (RRR alpha tocopherol acetate) or matching placebo (mineral oil). Both the vitamin and placebo capsules were manufactured by Strides, which had no role in the design of the study, the analysis or interpretation of the data, the preparation of the manuscript, or the decision to submit the manuscript for publication. The simple urn method, with stratification according to clinical center, was used by the data coordinating center to create a randomization sequence.(10)
The study was double-masked. Certified research staff collected information on the women's demographic features, medical history, social history at enrollment, and neonatal and maternal outcomes at delivery. The study was approved by the institutional review boards of each clinical site and the data coordinating center. All participants provided written informed consent before enrollment.
The occurrence of spontaneous preterm births (due to preterm PROM or to spontaneous preterm labor) in women randomized to vitamin or placebo supplementation was a planned secondary outcome of the original trial. Preterm birth was defined as prior to 37 weeks’ gestation and as an indicated or a spontaneous preterm birth. Spontaneous preterm birth included spontaneous labor with or without subsequent intrapartum oxytocin augmentation. Similar to some prior MFMU Network trials, preterm premature rupture of membranes was defined as spontaneous rupture of membranes and one of the following criteria: membrane rupture 60 minutes or more before onset of labor, labor induced for pre-labor ruptured membranes, or no labor and onset of rupture 60 minutes or more before delivery.
Data from all women were analyzed according to the group to which they were randomized, regardless of whether they took the study capsules. Continuous variables were compared using the Wilcoxon rank-sum test, and categorical variables with the chi-square test. Logistic regression was used to calculate odds ratios and the multivariable analysis included race or ethnic group, smoking, body mass index at baseline (9-16 weeks gestational age) and clinical center. Survival analysis, using the Kaplan-Meier method, was performed to estimate whether treatment with vitamins was associated with a longer time to rupture (censoring at term). For each of the outcomes, the Breslow-Day test for homogeneity was used to estimate if there was a difference in the effect among women who started treatment prior to 13 weeks’ gestation compared with those that started on or after 13 weeks’ gestation. For all statistical tests, a nominal p value less than 0.05 was considered to indicate statistical significance; no adjustments were made for multiple comparisons. Analyses were performed using SAS software (Cary, NC).
RESULTS
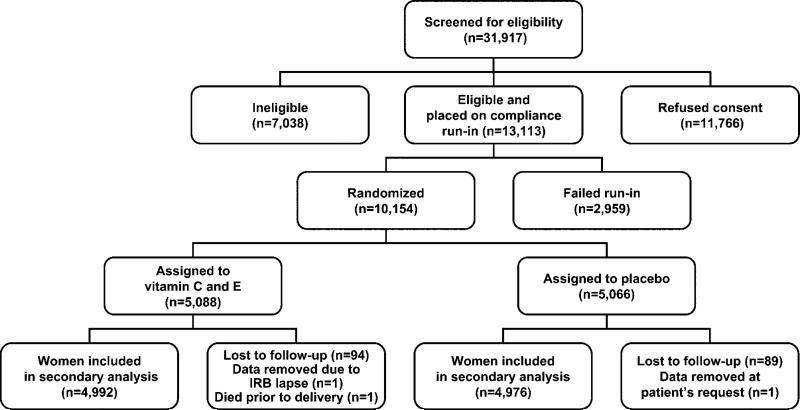
Figure 1 details the enrollment, randomization and follow-up of the participants in this trial. A total of 10,154 women were randomized and outcome data was available on 9,969 women. One woman who died and never delivered her baby was excluded, leaving 9,968 women for this analysis (4,992 vitamins and 4,976 placebo). Baseline characteristics were similar between the two groups (Table 1). Seventy-seven percent of enrolled subjects were taking a prenatal or multivitamin when they were randomized. The median ratio of the number of study capsules taken to the number that should have been taken between randomization and delivery was 88% in both treatment arms.
Figure 1.
Enrollment, randomization, and follow-up of participants
Table 1.
Baseline Maternal Characteristics*
| Vitamins N=4,992 | Placebo N=4,976 | |
|---|---|---|
| Maternal age (years) | 23.5 ± 5.2 | 23.5 ± 5.3 |
| Weeks of gestation at randomization | 13.4 ± 2.1 | 13.4 ± 2.1 |
| Randomization ≤ 12 weeks | 2,181 (43.7) | 2,162 (43.4) |
| Race or ethnic group+ | ||
| African American | 1,245 (24.9) | 1,273 (25.6) |
| Hispanic | 1,559 (31.2) | 1,524 (30.6) |
| Other | 2,188 (43.8) | 2,179 (43.8) |
| Body-mass index at randomization (kg/m2) | 26.3 ± 6.1 | 26.3 ± 6.1 |
| Smoker | 788 (15.8) | 763 (15.3) |
| Educational level (years) | 12.8 ± 2.7 | 12.8 ± 2.7 |
| Prenatal or multivitamin usage | 3,852 (77.2) | 3,838 (77.1) |
| Daily dose of vitamin C (mg) | ||
| Median | 120 | 100 |
| Range | 0-150 | 0-300 |
| Daily dose of vitamin E (IU) | ||
| Median | 22 | 22 |
| Range | 0-100 | 0-100 |
| Previous pregnancy | 1,138 (22.8) | 1,149 (23.1) |
Plus-minus values are means ± standard deviation
P ≥ 0.05 for all between-group comparisons.
Race or ethnic group was self-reported.
One thousand thirty-eight women delivered preterm of which 698 (7.0%) had a spontaneous preterm birth (SPB). There were 253 women (2.5%) delivered after preterm PROM and 445 (4.5%) after a spontaneous preterm labor. A SPB less than 37 weeks’ gestation occurred in 356 women (7.1%) assigned to daily vitamin C/E supplementation and in 342 (6.9%) assigned a placebo (p=0.61). These results were similar regarding SPB before 35 or 32 weeks gestation (Table 2). Additionally, the survival analysis showed there was no difference in gestational age at membrane rupture (censoring at term) between the two treatment groups (p=0.62, log rank test). The frequency of SPB attributable to preterm PROM before 37 and before 35 weeks’ gestation in the vitamin supplemented and placebo groups were similar (Table 2.) However, SPB before 32 weeks’ gestation and attributable to preterm PROM was less frequent in the vitamin supplemented group (0.3% vs. 0.6%, adjusted OR 0.3-0.9). Because PROM remote from term is often treated conservatively to prolong pregnancy, we also evaluated the impact of vitamin supplementation based on the gestational age at the time of membrane rupture. Preterm PROM occurring before 32 weeks 0 days gestation was also less frequent in the women supplemented with vitamins (0.36% vs. 0.64%, p=0.046). For each of the outcomes, the test for homogeneity was not significant indicating there was no difference in the effect among women who started treatment prior to 13 weeks’ gestation compared with women who started at or after 13 weeks’ gestation.
Table 2.
Spontaneous preterm birth and preterm PROM prior to 37, 35 and 32 weeks’ gestation.*
| Outcome | Vitamins N=4,992 | Placebo N=4,976 | OR [95% CI] | Adjusted OR# [95% CI] |
|---|---|---|---|---|
| SPB < 37 weeks | 356 (7.1) | 342 (6.9) | 1.04 [0.89, 1.21] | 1.05 [0.90, 1.22] |
| SPB < 35 weeks | 177 (3.6) | 185 (3.7) | 0.95 [0.77, 1.17] | 0.96 [0.77, 1.18] |
| SPB < 32 weeks | 109 (2.2) | 124 (2.5) | 0.87 [0.67, 1.13] | 0.88 [0.67, 1.14] |
| SPB due to preterm PROM <37 weeks | 124 (2.5) | 129 (2.6) | 0.96 [0.75, 1.23] | 0.96 [0.75, 1.23] |
| SPB due to preterm PROM <35 weeks | 56 (1.1) | 58 (1.2) | 0.96 [0.66, 1.39] | 0.97 [0.67, 1.40] |
| SPB due to preterm PROM <32 weeks | 15 (0.3) | 30 (0.6) | 0.50 [0.27, 0.92] | 0.50 [0.27, 0.93] |
| Preterm PROM <37 weeks | 130 (2.6) | 132 (2.7) | 0.98 [0.77, 1.25] | 0.98 [0.77, 1.26] |
| Preterm PROM <35 weeks | 58 (1.2) | 61 (1.2) | 0.95 [0.66, 1.36] | 0.95 [0.66, 1.37] |
| Preterm PROM <32 weeks | 18 (0.4) | 32 (0.6) | 0.56 [0.31, 1.00] | 0.56 [0.32, 1.00] |
Presented as number (%). SPB total spontaneous preterm births (preterm PROM or preterm labor), preterm PROM preterm premature rupture of membranes.
Adjusted for race, smoking, baseline body mass index and center.
Neonatal outcomes according to treatment group for the entire cohort have previously been published.(8) Selected neonatal outcomes in the 698 women who had a spontaneous preterm birth prior to 37 weeks gestation were similar between those assigned to daily vitamin and placebo supplementation (Table 3).
Table 3.
Neonatal outcomes for spontaneous preterm births occurring before 37 weeks.*
| Vitamins N=356 | Placebo N=342 | p-value | |
|---|---|---|---|
| Fetal/neonatal death | 72 (20.5) | 80 (23.5) | 0.33 |
| Fetal loss < 20 weeks | 45 (12.6) | 47 (13.7) | 0.67 |
| Fetal death ≥ 20 weeks | 8 (2.2) | 10 (2.9) | 0.57 |
| Neonatal death | 19 (5.4) | 23 (6.8) | 0.45 |
| SGA < 3rd centile† | 3 (1.0) | 8 (2.8) | 0.10 |
| LBW < 2500 (grams)† | 157 (52.0) | 160 (56.5) | 0.27 |
| Apgar score ≤ 3 at 5 minutes† | 14 (4.7) | 17 (6.0) | 0.48 |
| RDS† | 56 (18.6) | 49 (17.3) | 0.67 |
| Sepsis† | 20 (6.6) | 11 (3.9) | 0.13 |
| Necrotizing enterocolitis† | 8 (2.7) | 8 (2.8) | 0.91 |
| IVH (grade III and IV)† | 5 (1.7) | 7 (2.5) | 0.49 |
| Retinopathy of prematurity† | 16 (5.3) | 13 (4.6) | 0.68 |
| NICU admission† | 149 (49.2) | 142 (50.0) | 0.84 |
Presented as number (%). SGA small for gestational age, LBW low birth weight, NICU neonatal intensive care unit, RDS respiratory distress syndrome, IVH intraventricular hemorrhage.
Live births only (303 in the Vitamins group and 285 in the Placebo group).
DISCUSSION
We found a similar occurrence of spontaneous births prior to 37, 35, and 32 weeks’ gestation in women assigned to daily vitamin C/E or to placebo treatment in a planned secondary analysis of an NICHD Maternal-Fetal Medicine Units Network trial. The frequencies of preterm birth before 37 and 35 weeks due to either preterm PROM or preterm labor were also similar between groups. Our analysis does demonstrate less frequent preterm births before 32 weeks’ gestation due to preterm PROM in women assigned to daily vitamin supplementation (0.30 % vs. 0.60 %], adjusted OR [95% CI] 0.50 [0.27, 0.93]), and also less frequent preterm PROM occurring before 32 weeks gestation (0.36% vs. 0.64%, adjusted OR 0.56 [0.32, 1.00]). It is possible that this single significant occurrence is due to the clinical imprecision of determining the SPB subcategories of preterm PROM or spontaneous preterm labor. Spontaneous preterm labor and or preterm PROM are precisely defined but are less precisely determined due to the difficulties inherent in the “best estimate” of the onset of labor and or the timing of membrane rupture in relation to the onset of contractions. Though we limited the diagnosis of PROM to those women with onset of membrane rupture at least one hour before the onset of symptomatic contractions, the possibility of incorrect categorization remains and should be considered. Further, the presence of this statistically significant finding for a relatively uncommon finding and in the absence of similar trend or pattern for other similar outcomes raises the possibility that the result occurred because of a Type I (alpha) error. Most precisely, SPB includes all of the women who had a preterm birth that was not indicated. We found no difference in SPBs across gestation whether the women were assigned to daily vitamin supplementation or to a placebo. We also found no benefit of daily maternal vitamin C/E supplementation for any of the pre-specified outcomes of the neonates delivered preterm due to spontaneous birth.
Vitamin C deficiency has been associated with the occurrence of spontaneous preterm birth.(4,5,6,10) Vitamin C is involved in collagen synthesis and may be important to maintain the integrity of the chorioamnion membranes. Woods and colleagues(5) reported that reduced midgestational levels of vitamin C are associated with preterm premature rupture of membranes. They noted that reactive oxygen species generated in response to insults such as infection, cigarette smoking, bleeding, or cocaine use can activate collagenolytic enzymes and impair fetal membrane integrity. They hypothesized that an increase in dietary consumption or supplementation of vitamin C and E during pregnancy might reduce the risk of that portion of preterm premature rupture of membranes that may be mediated by oxidative injury to fetal membranes. Plessinger and colleagues(11) reported that pre-treatment of human amnion-chorion with vitamins C and E prevents hypochlorous acid-induced membrane damage. Casanueva and colleagues(7) tested the hypothesis that maternal supplementation with a relatively low dose of vitamin C (100 mg daily) would prevent SPB due to preterm PROM. In their trial, mean leukocyte vitamin C concentrations decreased in the placebo group and increased in the vitamin C group (p=0.001) and preterm PROM occurred in 14 of 57 (24.6%) women assigned to placebo treatment and in 4 of 52 (7.6%) assigned to vitamin C (RR 0.26; 95% CI [0.08, 0.83]). In a planned secondary analysis of a larger population, Spinnato and associates (12) reported that women assigned to 1000 mg of daily maternal vitamin C and 400 IU of vitamin E or to a placebo had a similar occurrence of spontaneous preterm births. These authors did report an increased frequency of preterm PROM among women randomized to vitamin supplementation (16/349 [4.6%] vs. 6/348 [1.7%], p=0.025). In both of these reports, and our analysis, the frequencies of total spontaneous births were not different between groups. The conflicting findings regarding preterm PROM in the Casanueva trial, the Spinnato analysis, and our analysis, further raise question regarding the veracity of our finding that vitamin C and E supplementation reduces the frequency of preterm PROM before 32 weeks’ gestation. This is particularly the case for combined vitamin C and E supplementation, as our analysis and the Spinnato analysis had opposite results.
In summary, maternal supplementation with vitamin C and E did not reduce the occurrence of spontaneous preterm birth. Neonatal outcomes of infants delivering preterm were similar in preterm newborns whose mothers were randomized to treatment with vitamin C or E or a placebo. Our results, taken in context with similar trials regarding vitamin C and E supplementation, do not support either the clinical use for prevention of spontaneous preterm birth or its neonatal sequelae or further trials of this treatment in similar low-risk populations.
Supplementary Material
Acknowledgments
The project described was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (HD34208, HD27869, HD40485, HD40560, HD40544, HD34116, HD40512, HD21410, HD40545, HD40500, HD27915, HD34136, HD27860, HD53118, HD53097, HD27917, and HD36801); the National Heart, Lung, and Blood Institute; and the National Center for Research Resources (M01 RR00080, UL1 RR024153, UL1 RR024989) and its contents do not necessarily represent the official view of NICHD, NHLBI, NCRR or NIH.
Footnotes
This paper was presented as a poster presentation at the Society for Maternal-Fetal Medicine 2010 Annual Meeting in Chicago, IL, February 4, 2010.
PRÉCIS
Maternal supplementation with vitamins C/E beginning at 9 to 16 weeks gestation in low risk nulliparous women did not reduce total spontaneous preterm births.
REFERENCES
- 1.Hamilton BE, Martin JA, Ventura SJ. National vital statistics reports, web release. 12. Vol. 57. National Center for Health Statistics; Hyattsville, MD: [March 18, 2009]. Preliminary data for 2007. [Google Scholar]
- 2.Meis PJ, Michielutte R, Peter TJ, et al. Factors associated with preterm birth in Cardiff, Wales, I. Univariable and multivariable analysis. Am J Obstet Gynecol. 1995;173:590–6. doi: 10.1016/0002-9378(95)90287-2. [DOI] [PubMed] [Google Scholar]
- 3.Meis PJ, Goldenberg RL, Mercenter BM, et al. The preterm prediction study: risk factors for indicated preterm births. Am J Obstet Gynecol. 1998;178:562–7. doi: 10.1016/s0002-9378(98)70439-9. [DOI] [PubMed] [Google Scholar]
- 4.American College of Obstetricians and Gynecologists Premature rupture of membranes. ACOG practice bulletin no. 80. Obstet Gynecol. 2007;109:1007–19. doi: 10.1097/01.AOG.0000263888.69178.1f. [DOI] [PubMed] [Google Scholar]
- 5.Woods JR, Plessinger MA, Miller RK. Vitamins C and E: Missing links in preventing preterm premature rupture of membranes? Am J Obstet Gynecol. 2001;185:5–10. doi: 10.1067/mob.2001.115868. [DOI] [PubMed] [Google Scholar]
- 6.Siega-Riz AM, Promislow JHE, Savitz DA, Thorp JM, McDonald T. Vitamin C intake and the risk of preterm delivery. Am J Obstet Gynecol. 2003;189:519–25. doi: 10.1067/s0002-9378(03)00363-6. [DOI] [PubMed] [Google Scholar]
- 7.Casanueva E, Ripoll C, Tolentino M, et al. Vitamin C supplementation to prevent premature rupture of the chorioamniotic membranes : a randomized trial. Am J Clin Nutr. 2005;81:859–63. doi: 10.1093/ajcn/81.4.859. [DOI] [PubMed] [Google Scholar]
- 8.Roberts JM, Myatt L, Spong CY, et al. Vitamin C and E to prevent adverse outcomes with pregnancy associated hypertension. N Engl J Med. 2010;362:1282–91. doi: 10.1056/NEJMoa0908056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carey JC, Klebanoff MA, Hauth JC, et al. Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vaginosis. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 2000;342:534–40. doi: 10.1056/NEJM200002243420802. [DOI] [PubMed] [Google Scholar]
- 10.Lachin JM, Matts JP, Wei LJ. Randomization in clinical trials: conclusions and recommendations. Control Clin Trials. 1988;9:365–74. doi: 10.1016/0197-2456(88)90049-9. [DOI] [PubMed] [Google Scholar]
- 11.Stuart EL, Evans GS, Lin YS, Powers HJ. Reduced collagen and ascorbic acid concentrations and increased proteolytic susceptibility with prelabor fetal membrane rupture in women. Biol Reprod. 2005;72:230–5. doi: 10.1095/biolreprod.104.033381. [DOI] [PubMed] [Google Scholar]
- 12.Plessinger MA, Woods JR, Jr, Miller RK. Pre-treatment of human amnion-chorion with vitamins C and E prevents hypochlorous acid-induced damage. Am J Obstet Gynecol. 2000;183:979–85. doi: 10.1067/mob.2000.106676. [DOI] [PubMed] [Google Scholar]
- 13.Spinnato JA, II, Freire S, Pinto e Silva JL, et al. Antioxidant supplementation and premature rupture of the membranes: a planned secondary analysis. Am J Obstet Gynecol. 2008;199:433.e1–433.e8. doi: 10.1016/j.ajog.2008.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.