Abstract
Despite its recognition as a key dimension of health care quality, it is often unclear what exactly patient-centeredness means to providers and patients: a generally accepted measurement model of patient-centeredness is still non-existent, current operational definitions lack sufficient specificity to inform providers how it relates to outcomes, and the influence of patient-centeredness on pediatric patients and families has not been quantified. This study demonstrates that patient-centeredness is a measurable ability of pediatricians that increases family trust. As an ability, it is teachable. We offer an evidence-based model for future research with specific implications for quality measurement and improvement in the outpatient pediatrician’s office.
Keywords: patient-centeredness, provider-patient relationship, quality
Background
As a result of extraordinary advances in science and technology and abundant capital, the producers of healthcare in the United States enjoy thousands of multimillion dollar hospitals, purportedly the best medical schools and clinically competent physicians, extraordinary diagnostic tools, new and potentially more effective drugs, the latest surgical procedures, supporting nursing, allied health, and ancillary personnel, and more. Yet despite these amazing resources, we are consistently confronted with reports of questionable quality, safety, patient-centeredness, service, equity, and now more than ever, out of control costs that challenge the very economic well-being of the nation. There is so much bad news any thoughtful consumer or producer must question the progress. All the vaunted science and technology, splendid hospitals, prestigious medical schools and clinically competent physicians have not been enough. Something is missing.
Always a trait of the best physicians and hospitals, patient-centered care received national attention in 2001 with the Institute of Medicine’s (IOM) release of Crossing the Quality Chasm: A New Health System for the 21st Century (Institute of Medicine. Committee on Health Care in America, 2001). The IOM correctly confirmed the importance of patient-centeredness and recommended that the producers of healthcare focus more on the preferences, needs, and values of patients rather than their own (Institute of Medicine. Committee on Health Care in America, 2001).
In agreement, the Department of Health and Human Services (DHHS) and the Agency for Healthcare Research and Quality (AHRQ) included patient-centeredness, as an important component of healthcare quality, in their National Healthcare Quality and Disparities Reports to Congress. (Agency for Healthcare Research and Quality, 2005 (December)-a, 2005 (December)-b) In the same vein, The American Academy of Pediatrics (AAP) advanced the Medical Home, recommending that pediatric care be “accessible, continuous, comprehensive, family-centered, coordinated, compassionate, and culturally effective.”(American Academy of Pediatrics. Medical Home Initiatives for Children With Special Needs Project Advisory Committee, 2002).
Despite these calls for more patient-centered care, a generally accepted measurement model of patient-centeredness is non-existent, current operational definitions lack sufficient specificity (Taylor, 2008), and its influence on pediatric patients and families has not been quantified and is still unknown. In this paper we attempt to describe patient-centeredness with sufficient specificity to guide the implementation of quality improvement efforts in the outpatient pediatrician’s office. Specifically, we examine whether patient-centeredness is a measurable ability of pediatricians, and whether increases in the patient-centeredness of a pediatrician lead to increased family trust.
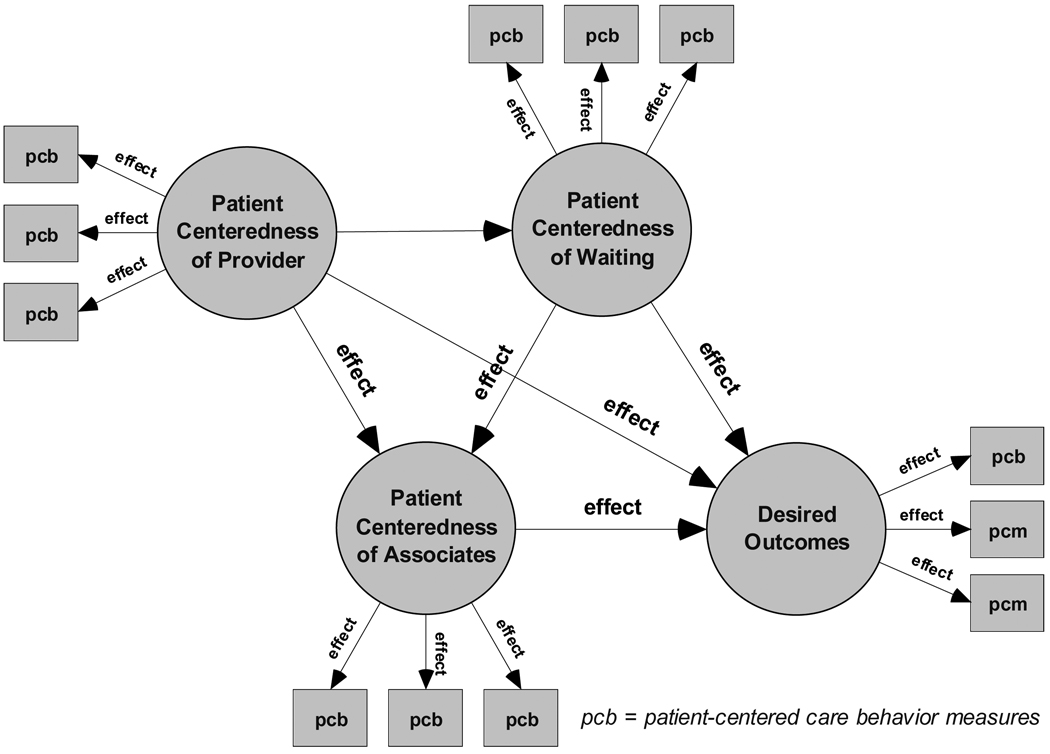
The theoretical foundation for this investigation, The Primary Provider Theory (Figure 1) (SJ Aragon, 2009; SJ. Aragon, 2009), is a generalizable theory of how the patient-centeredness of health providers affects their care behaviors in patient encounters and related outcomes. The theory is patient-centered because it is driven by principles that favor patients in healthcare encounters (see below). The Primary Provider Theory maintains that physicians with higher magnitudes of patient-centeredness are, for example, concerned first and foremost with their patients’ best interests; careful to understand their patients’ feelings, perspectives, and needs; approachable, tactful and skilled in relationships; communicative and informative; encourage rapport, and patient participation in decision-making. The theory can be applied to a full range of healthcare providers, including physicians, allied health practitioners, nurses, nurse practitioners, dentists, physician assistants and others, across multiple settings and patient groups.
Figure 1.
The Primary Provider Theory
The Primary Provider Theory Principles
Clinical competency is a necessary but insufficient condition of desired outcomes.
Desired outcomes require more than clinical competency alone, because the transmission of clinical knowledge and care requires effective communication and social interaction with patients.
Patient-centeredness is the underlying ability of providers that affects the quality of their transmission of clinical knowledge and care to patients.
Providers are uniquely responsible for the quality of the transmission of their clinical knowledge and care to patients.
Providers who are both clinically competent and patient-centered are more likely to achieve desired outcomes.
Patients and families value the patient-centeredness of their health providers.
The patient-centeredness of the provider is more important than the financial profit of a patient encounter.
Patients are the best judges of the patient-centeredness of their health providers. (Note: These principles are consistent with the scientific method and the Hippocratic Oath.)
To understand the measurement of patient-centeredness itself, as opposed to patient-centered care (behaviors, processes and their related outcomes, such as patient satisfaction with care), one must first appreciate the concept of an underlying ability or latent trait. Latent trait theory holds that an individual’s response to a challenge or performance on a test, for example, can be explained by their underlying ability in the domain of interest. Latent trait models have long been used by psychometricians for studying variables and relationships that must be measured indirectly, like verbal and math ability, knowledge of history, interpersonal skill, humility, or hubris for example. Likewise, the Primary Provider Theory holds that patient-centeredness is an underlying ability of healthcare providers that is measured indirectly. It further holds that individual healthcare providers possess differing magnitudes of patient-centeredness, and that as an ability, it is teachable.
Consistent with this theory, we hypothesized that patient-centeredness would have a significant and positive effect on pediatric patient families’ trust in their provider. Correspondingly, physician attitudes and care behaviors, including interpersonal skills and communication style, have all been found to be the strongest predictors of patient trust (Hall, Dugan, Zheng, & Mishra, 2001; Murphy, Chang, Montgomery, Rogers, & Safran, 2001; Street, O’Malley, & Cooper, 2008; Thom, 2001). Further, patient trust has also been positively associated with fewer disputes, complaints and lawsuits, higher satisfaction and effectiveness of care, higher self-reported health, and the patient’s willingness to recommend the physician. Conversely, patient characteristics and personality, as well as physician demographics and professional attributes, have been found to be weak covariates of patient trust.(Hall et al., 2001)
Purpose
The purpose of this investigation was four-fold: (a) To describe and measure the patient-centeredness of pediatricians as a precursor of their care behavior performance; (b) to determine how pediatric patient-centeredness influences family trust, confidence, and the likelihood to recommend; (c) to assess the stability of pediatricians’ patient-centeredness on family trust across national random samples; and (d) to test the hypothesized pediatric patient-centeredness model’s strength against a competing model.
STUDY DESIGN AND METHOD
Sample
This study used data collected from January through December 2004 and maintained in the Press Ganey National Medical Practice Database, which contained 1,202,193 patients from 542 pediatric practices, throughout the United States and all American Hospital Association regions. The locations of these practices were distributed across large cities (26%), rural areas (19%), small cities (25%) and city suburbs (20%). Annual visits in these practices ranged from 260 to 129,142, and they identify themselves as free standing clinics (33%), medical school based clinics (5%), hospital clinics (25%), private physician practices (12%); teaching hospital residency (14%), university–based residency (4%). Ownership was distributed across hospital-owned (33%), integrated health system-owned (49%), university medical school-owned (11%), physician-owned (3%), and other (2%).
All parent contacts of pediatric patients seen at participating outpatient practices were eligible to receive surveys. The database captures the views of those parents who randomly received and returned a survey. Randomly selected patient-level test (N=294) and cross-validation (N=311) samples from this database were used. At each outpatient clinic, data were collected as part of ongoing quality improvement initiatives. All data were de-identified by the vendor prior to release to the authors.
Institutional Review Board (IRB) Approval
IRB approval was obtained from Vanderbilt University (IRB Number 090127).
Inclusion Criteria
The selection of cases was based on the following: (1) inclusion in the Press Ganey National Medical Practice Database; (2) the primary clinician was a pediatrician, and (3) SPSS randomselection of full-information cases on the variables of interest.
Instrument
All data used in this study were collected with the Press Ganey Medical Practice Survey, a widely-used self-administered standardized instrument, which captures patients’ ratings of their healthcare visit, including scores on physician care behavior performance. Evidence of the instrument’s internal consistency (α = .97) and construct validity has been documented in previous research (Drain, 2001). The instrument is used nationally, has significant end-user acceptance, and is listed by the National Quality Measures Clearinghouse (NQCM). Responses are scored on a balanced 5-point scale ranging from very poor (1) to very good (5).
Data Collection
Surveys were mailed throughout the year to random samples of patients in each pediatric practice, with a post-paid return envelope and a cover letter assuring confidentiality. Continuous sampling was employed to reduce seasonal variation. Typically received within five days of the visit by patient families, surveys were distributed within the six weeks recommended by current research on reliability of patient responses (Bredart et al., 2002). Automated mailing reduced the possibility of selection bias by ensuring that all patients chosen by a practice’s sampling logic received a survey. Completed surveys were returned to the research firm for coding and processing.
Analysis
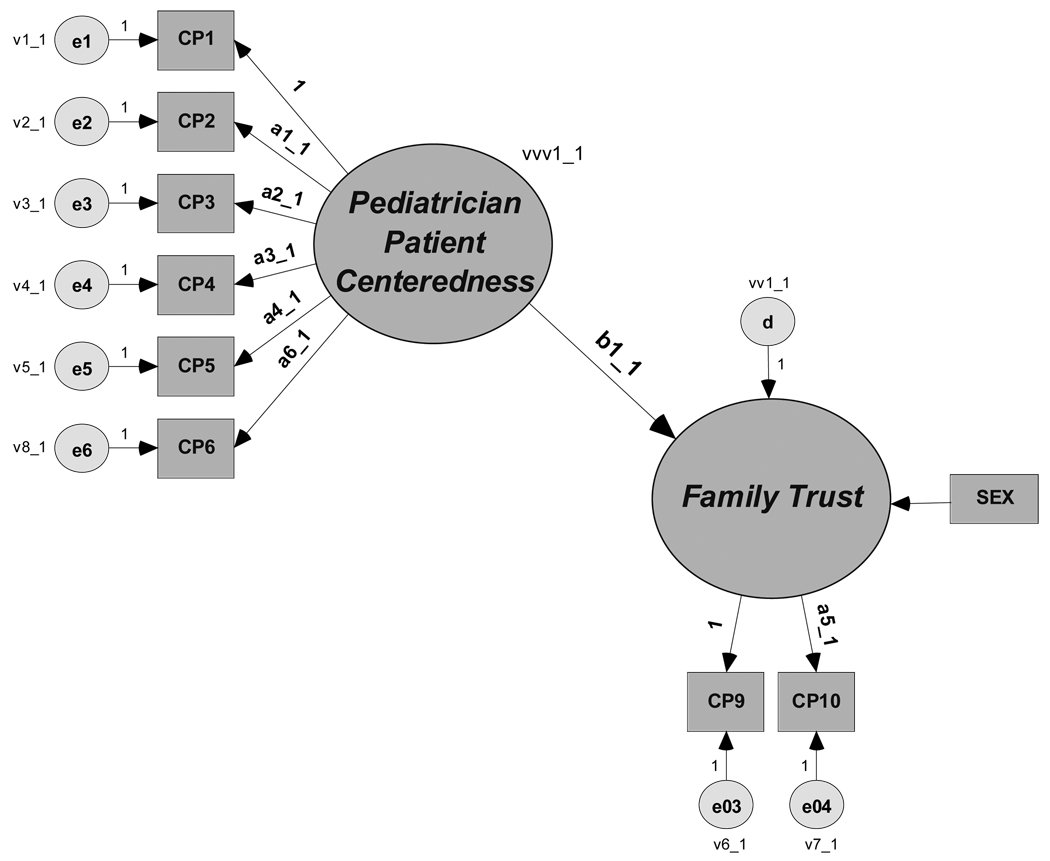
Structural equation modeling was used to test the Primary Provider Theory’s sub-proposition that the pediatrician’s patient-centeredness has a direct effect on the desired outcome of patient trust (Figure 2). This analytical approach involves a 2-step process. In the first step, the hypothesized constructs (patient-centeredness and family trust) and their observed-variable linkages are tested using confirmatory factor analysis; this step leads to what is known as the measurement model. In the second step, the structural relationships between constructs (patient-centeredness and family trust) are specified and tested; this step leads to what is known as the structural model. Results from the second step reveal whether latent variables relate to each other as hypothesized (up stream vs. down stream) and the strength of the relationships. It also provides model fit, validity, and reliability evidence. To further challenge the validity of our results we first tested the hypothesized model with effect sizes not equal in both samples, and then repeated the analyses with effect sizes equal in both samples. At each of these steps, the hypothesized pediatric patient-centeredness model (Figure 2) could be disconfirmed by the resulting empirical evidence.
Figure 2.
Hypothesized Pediatric Patient-Centeredness Model
RESULTS
Measurement Models
Patient-Centeredness
Consistent with the Primary Provider Theory, patient-centeredness was specified to have a causal effect on family trust (Figure 2); that is, when patient-centeredness increased, family trust was expected to increase, and conversely, when patient-centeredness decreased family trust was expected to decrease.
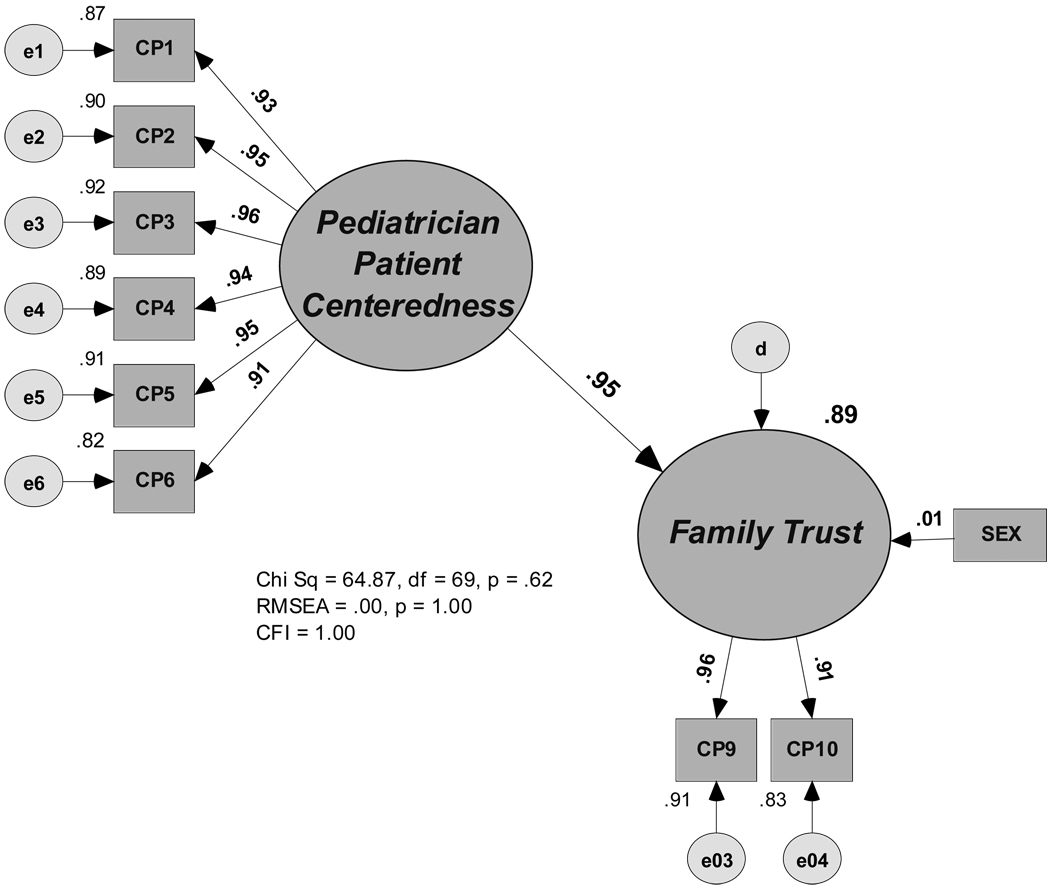
Patient-centeredness was measured and tested as an ability of pediatricians using patient family ratings of their physician’s performance on six care behaviors, including: their friendliness and courtesy, explanation of the patient’s problem to the family, concern for the family’s questions, efforts to share decision-making with the family, efforts to provide medication information and follow-up instructions (Table 1). This measurement structure was judged appropriate on the basis of validity and reliability evidence, including the size, significance, and stability of the care behavior’s structural relationships with the construct patient-centeredness in both the national random test and cross-validation samples (Figure 3). Random measurement error associated with each care behavior was minimal and the variance explained was high (Figure 3). Also, both coefficients alpha and H (Hancock & Mueller, 2001) (α = .96, H = .98) converged in providing further evidence of the construct reliability of pediatricians’ patient-centeredness ability.
Table 1.
Measures
| Measure | Description |
|---|---|
| No PC | PATIENT-CENTEREDNESS |
| CP1 | Friendliness and courtesy of the pediatrician |
| CP2 | Explanations the pediatrician gave about the problem or condition |
| CP3 | Concern the pediatrician showed for questions or worries |
| CP4 | Pediatrician’s efforts to include you in treatment decisions |
| CP5 | Information the pediatrician provided the about medications |
| CP6 | Information the pediatrician provided the about follow-up care |
| FT | FAMILY TRUST |
| CP9 | Confidence in the pediatrician |
| CP10 | Likelihood of recommending the pediatrician to others |
Figure 3.
Standardized Results
Family Trust
Consistent with the structure of the Primary Provider Theory, family trust was specified in this study as a causal outcome of pediatric patient-centeredness (Figure 2). Families with high trust were expected to have more confidence and be more likely to recommend their pediatricians. Families with lower trust were expected to have less confidence and be less inclined to recommend their pediatricians to others (Table 1).
As with patient-centeredness, this measurement configuration was deemed appropriate on the basis of validity and reliability evidence, including the size, significance, and stability of the family trust’s structural relationships with its associated care behaviors across national random test and cross-validation samples (Figure 3). The random measurement error associated with family trust’s measures was minimal and the variation explained was high (Figure 3). Also, both coefficients alpha and H (Hancock & Mueller, 2001) (α = .95, H = .97) converged in providing further evidence of family trust’s construct reliability.
Structural Model
The structural model fit the data well, providing evidence supporting the hypothesis that patient-centeredness was an underlying ability of pediatricians that influenced family trust, χ2 = 64.87, df = 69, p = .619; RMSEA = .000, p = 1.00; CFI = 1.00. Pediatric patient-centeredness significantly influenced family trust and explained 89 percent of its variability, p < .001; R2 = .89. Indirectly, through family trust, pediatrician patient-centeredness significantly influenced family’s confidence and likelihood to recommend, p < .001. As reflected in Table 2, one standard deviation increase in patient-centeredness increased family trust, confidence, and the likelihood to recommend by .946, .904, and .863 standard units respectively.
Table 2.
Total Effects of Pediatrician Patient-Centeredness on Family Trust
| DEPENDENT VARIABLES | EFFECTS (Standardized) | EFFECTS (Unstandardized) |
|---|---|---|
| FAMILY TRUST | .946 | 1.049 |
| Confidence in pediatrician (CP9) | .904 | 1.049 |
| Likelihood of recommending pediatrician (CP10) | .863 | 1.077 |
Note: Above effects are significant at the 0.001 level (two-tailed).
Pediatrician’s patient-centeredness also significantly affected family’s ratings of their care behavior performance. When pediatrician’s patient-centeredness increased by one standardized unit, there was a corresponding increase in family ratings of their pediatrician’s friendliness and courtesy, explanations of the patient’s condition, concern for the family’s questions and worries, efforts to include the family in decision-making, efforts to provide medication information and follow-up instructions by .933, .948, .957, .942, .951, respectively (Figure 3).
The effect of pediatrician’s patient-centeredness on family trust, confidence, and the likelihood to recommend the practitioner was stable across both the test and cross-validation samples. Further, the hypothesized model was sustained when compared to the competing independence model (χ2 = 143.92, df = 72, p = .000 versus χ2 = 64.87, df = 69, p = .619) and the unconstrained model, (χ2Δ = 13.94, df = 17, p = .671). The influence of gender on family trust was insignificant in both the test group and in the cross-validation group (p = .623, p = .711).
DISCUSSION
The value or usefulness of models first depends on the evidence supporting the validity and reliability of their inferences, and secondly, the extent to which they offer added-value in the field. Using these criteria, evidence converged in support of the model’s inference that patient-centeredness was an underlying ability of pediatricians that influences patient family trust, confidence, and the likelihood to recommend. For example, evidence of a strong “stimulus-response effect” between patient-centeredness and family trust was apparent; when patient-centeredness increased or decreased, family trust changed almost on a 1:1 basis. As such, the model can serve the interests of pediatricians, their patients and families by illuminating examples of care behaviors that influence the quality of the transmission of care. In this study, these care behaviors included the pediatrician’s friendliness and courtesy, explanations of the patient’s condition, concern for the family’s questions and worries, efforts to include the family in decision-making, and efforts to provide medication information and follow-up instructions. The model offers a template for testing many others, of which the number and quality of patient-centered care behaviors is only limited by the imagination and creativity of the provider. Pediatricians can improve their patient-centeredness scores by increasing and improving their care behaviors that serve the interests of patients and families.
In addition to providing evidence that patient-centeredness increases pediatric family trust, the model establishes that families value the patient-centeredness of their practitioner. For providers and patients/families, the model offers the potential for improved relationships, communication, care, and outcomes. Increased patient-centeredness can lead to greater patient satisfaction - more pleasant, more comforting, more compassionate, less frightening, and less humiliating care.
Lastly, the model provides an evidence-based framework for designing future research on patient-centeredness and desired outcomes, physician-patient-family relations and communication, and quality measurement and improvement.
What are potential consequences of adhering to the model if it is wrong? For some practitioners, being more patient-centered may require change. Change can be difficult. Being more friendly and courteous and showing more concern for the family’s questions and worries may reduce the formal distance between a practitioner and the family, and require vulnerability and risk. Increased efforts to include families in the decision-making process may require giving up some hard earned control and power. Being more patient-centered may require changes in practice patterns and the amount of time providers spend with their patients and patients’ families. This could result less patient through-put and revenue. Practitioners will have to individually weigh the benefits against the potential consequences of increased patient-centeredness and family trust.
Based on the above results and supporting evidence, we conclude that patient-centeredness is a variable, measurable, and teachable latent ability of pediatricians. Moreover, increases in a pediatrician’s patient-centeredness enhance family trust, confidence, recommendations, and ratings of care behaviors. On the other hand, decreases in a pediatrician’s patient-centeredness drive these outcomes down.
Lastly, and in general, we hold that clinical competency is a necessary but insufficient condition of provider quality. The very best pediatricians will be both clinically competent and patient-centered.
Limitations
All data for this investigation were accumulated with one instrument. While there is no generally accepted response rate in survey research, (Babbie, 1990) patients who respond to surveys could be different from those who do not. A study of non-response bias concluded that minority patients could be under-represented by not being as likely to return a completed patient survey (Kaldenberg, 1998a, 1998b).
Directions for Future Research
Within the context of the Primary Provider Theory, the results of this study offer an evidence-based model for future research with specific implications for the measurement and improvement of pediatric patient-centeredness, family trust, confidence, the likelihood to recommend, physician-patient-family relations and communication, and quality measurement and improvement. The model should be validated in other healthcare settings (e.g., inpatient, NICU, OB/GYN) and with non-physician primary providers.
The American Academy of Pediatrics’s conceptualization of the Medical Home requires that care be “accessible, continuous, comprehensive, family-centered, coordinated, compassionate, and culturally effective.” (American Academy of Pediatrics. Medical Home Initiatives for Children With Special Needs Project Advisory Committee, 2002) In this light, research measuring the influence of pediatricians’ patient-centeredness on these outcomes could contribute value to those currently struggling with implementation of the Medical Home.
Acknowledgments
This research was substantially supported by NIH/NCMHD Grant #P20MD002303 and partially supported by AHRQ/NRSA Grant #T32HS00032, The Center of Excellence for the Elimination of Health Disparities, Winston-Salem State University, The Cecil G. Sheps Center for Health Services Research, The University of North Carolina, and The Child Study Center, University of Oklahoma Health Sciences.
Contributor Information
Stephen J. Aragon, Associate Professor of Health Services Measurement, Winston-Salem State University, School of Health Sciences, 436 F.L. Atkins Building, Winston-Salem, NC 27110, Tel: (336) 750-3086, Fax: (336) 750-3173, aragons@wssu.edu.
Laura McGuinn, University of Oklahoma, Child Study Center, 1100 NE 13th Street, Oklahoma City, OK 73117, Tel: (405) 271-6824 ext 45175, Fax: (405) 271-8835, laura-mcguinn@ouhsc.edu.
Stefoni A. Bavin, Press Ganey Associates, Inc., 404 Columbia Place, South Bend, IN 46601, Tel: (574) 232-3387 Ext. 574, (800) 232-8032 Ext. 574, Fax: (574) 232-3485, sbavin@pressganey.com.
Sabina Gesell, Associate Professor of Pediatrics, Vanderbilt University School of Medicine, AA-0216 Medical Center North, Nashville, TN 37232-2504, Tel: (615) 343-6283, Fax: (615) 343-6249, sabina.gesell@vanderbilt.edu.
REFERENCES
- Agency for Healthcare Research and Quality. The National Healthcare Disparities Report. AHRQ Publication No.06-0017. Washington, DC: Department of Health and Human Services; 2005 (December)-a;
- Agency for Healthcare Research and Quality. The National Healthcare Quality Report. AHRQ Publication No.06-0018. Washington, DC: Department of Health and Human Services; 2005 (December)-b;
- American Academy of Pediatrics. Medical Home Initiatives for Children With Special Needs Project Advisory Committee. The medical home. Pediatrics. 2002;110(1 Pt 1):184–186. [Google Scholar]
- Aragon S. [Retrieved Retrieved February 28, 2009];The Primary Provider Theory©. 2009 from. http://www.ceehd.com/index.php?option=com_content&task=view&id=10Itemid=16.
- Aragon S. The Provider Patient-Centeredness and Disparities Outcome Measurement Initiative." Practice What You Preach: Examining the Role of Medical Providers in Eliminating Health Disparities. MD: National Harbor; The Third National Leadership Summit on Eliminating Racial and Ethnic Disparities in Health. 2009
- Babbie E. Survey Research Methods. Belmont, California: Wadsworth Publishing Company; 1990. [Google Scholar]
- Bredart A, Razavi D, Robertson C, Brignone S, Fonzo D, Petit JY, et al. Timing of patient satisfaction assessment: effect on questionnaire acceptability, completeness of data, reliability and variability of scores. Patient Educ Couns. 2002;46(2):131–136. doi: 10.1016/s0738-3991(01)00152-5. [DOI] [PubMed] [Google Scholar]
- Drain M. Quality improvement in primary care and the importance of patient perceptions. J Ambul Care Manage. 2001;24(2):30–46. doi: 10.1097/00004479-200104000-00005. [DOI] [PubMed] [Google Scholar]
- Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79(4):613–639. doi: 10.1111/1468-0009.00223. v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancock GR, Mueller RO. In: Rethinking construct reliability within latent variable systems. In Structural equation modeling: Present and future—A Festschrift in honor of Karl Jöreskog. Cudeck SdTR, Sörbom D., editors. Lincolnwood, IL: Scientific Sofware International; 2001. pp. 195–216. [Google Scholar]
- Institute of Medicine. Committee on Health Care in America. Washington, DC: National Academy Press; Crossing the Quality Chasm: A New Health System for the 21st Century. 2001
- Kaldenberg D. Results from the Press, Ganey response study (Part 1) The Satisfaction Monitor. 1998a March–April 4–5;12 [Google Scholar]
- Kaldenberg D. Results from the Press, Ganey response study (Part 2) The Satisfaction Monitor. 1998b May–June 5–7;10 [Google Scholar]
- Murphy J, Chang H, Montgomery J, Rogers W, Safran D. The Quality of Physician-Patient Relationships. J Fam Pract. 2001;50(2):123–129. [PubMed] [Google Scholar]
- Street RL, O’Malley KJ, Cooper LA. Understanding Concordance in Patient-Physician Relationships: Personal and Ethnic Dimensions of Shared Identity. Ann Fam Med. 2008;6(3):198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor K. Paternalism, participation and partnership-The evolution of patient centeredness in the consultation. Patient Educ Couns. 2008 doi: 10.1016/j.pec.2008.08.017. [DOI] [PubMed] [Google Scholar]
- Thom D. Physician Behaviors that Predict Patient Trust. J Fam Practice. 2001;50(4):323–328. [PubMed] [Google Scholar]