Summary
Background
Evidence suggests that dispatcher-assisted chest compression-only bystander CPR may be superior to standard CPR (chest compressions and rescue ventilation) in out-of-hospital cardiac arrest, yet recent clinical trials did not observe improved outcomes. The goal of the study was to determine the association between chest compression-only CPR and survival after out-of-hospital cardiac arrest.
Methods
Studies published until August 2010 were systematically searched and identified in MEDLINE and EMBASE databases. For the primary meta-analysis only clinical trials were included that prospectively randomized dispatcher instructions to chest compression-only versus standard bystander CPR in out-of-hospital adult cardiac arrest patients; for the secondary meta-analysis observational cohort studies were included that distinguished between standard CPR and chest compression-only CPR. All studies were required to contain survival data. Data on study characteristics, methods and outcomes (return of spontaneous circulation, survival to discharge, 30-day survival, and favourable neurologic outcome) were extracted. A fixed-effects model was used for both meta-analyses for lack of heterogeneity among the studies (I2 0%).
Findings
All three published randomized clinical trials were included in the meta-analysis. The pooled analyses shows that dispatcher-assisted chest compression-only bystander CPR for adult out-of-hospital cardiac arrest was associated with a 22% improved chance of survival (risk ratio [RR] 1.22 [95% confidence interval {CI}, 1.01 – 1.47]; I2, 0%) compared to standard CPR. The absolute increase in survival was 2.4%; the number needed to treat was 41. The secondary meta-analysis included seven observational studies of bystander-CPR (not dispatcher-assisted) and showed no difference between the two CPR techniques (RR, 0.96 [95% CI, 0.83 – 1.11]; I2, 0%).
Interpretation
Dispatcher-assisted chest compression-only bystander CPR is associated with improved survival in adult patients after out-of-hospital cardiac arrest compared to standard CPR.
Introduction
The optimal method for bystander out-of-hospital cardiopulmonary resuscitation (CPR) is controversial.1, 2 Recommended standard basic life support combines chest compressions and rescue ventilation.3, 4 Over the course of the last decade, evidence from animal experiments5, 6 and observational human studies7–13 questioned the usefulness of rescue ventilation during adult CPR. These studies found chest compression-only CPR either equivalent to standard CPR with rescue ventilation or suggested even a benefit. However, the evidence was largely inconclusive mostly due to the observational study design or small sample size.
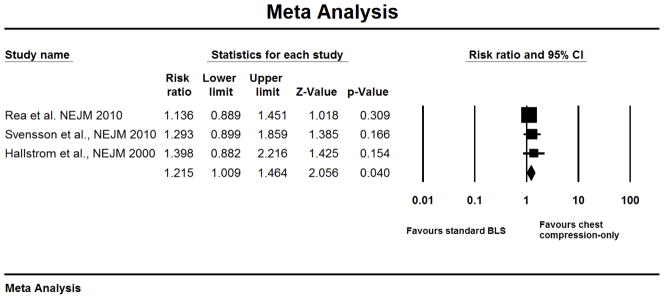
A single clinical trial published in 2000 randomized 520 patients with out-of-hospital cardiac arrest to either dispatcher-assisted chest compression-only or standard CPR and found a statistically non-significant survival benefit for chest compression-only CPR (relative difference: 40%, absolute difference: 4.2%, p=0.18).14 Very recently, two additional randomized clinical trials reported a similar, albeit statistically non-significant, positive trend for dispatcher-assisted chest compression-only CPR. Rea et al.15 found a 14% increased survival to hospital discharge (1.5% absolute increased survival, p= 0.31) among 1941 patients and Svensson et al.16 report a 24% improved 30-day survival (1.7% absolute increased survival, p= 0.29) among 1276 patients with cardiac arrest. Despite a uniform trend favouring chest compression-only CPR in all three trials, the results were inconclusive as of which dispatcher-assisted bystander-CPR method is superior.
Therefore, the goal of this study was to summarize the existing evidence regarding chest compression-only CPR in a systematic review and to compare it to standard CPR in a meta-analysis.
Methods
We followed the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) guideline17 for randomized clinical trials and the MOOSE (Meta-analysis Of Observational Studies in Epidemiology) guideline18 for observational cohort studies in this meta-analysis.
Search Strategy
Accessing MEDLINE and EMBASE databases, we performed a literature search for studies published between 1985 and August 2010 using the following search terms and key words: chest compression-only, compression alone, hands-only, bystander CPR. In addition, we manually checked the reference list of each article. The main focus of this study was on randomized clinical trials, but we also performed a secondary analysis of observational cohort studies.
Study Selection
We separated the systematic review and meta-analysis into two parts: in the primary analysis, randomized clinical trials were included and in the secondary, observational cohort studies. Only three randomized clinical trials have been conducted where adult patients suffering from out-of-hospital cardiac arrest received randomized instructions by a dispatcher for either chest compression-only CPR or standard CPR, and all three trials were included in the systematic review and meta-analysis. For observational studies, the following eligibility criteria were required for inclusion: (1) observational cohort studies (no case series); (2) comparison between chest-compression-only CPR and standard CPR; (3) survival data available; (3) adult population; (4) unstratified cohort (e.g., arrests of non-cardiac origin only); (5) bystander CPR; (6) out-of-hospital arrest. Articles were considered if published in English and German; this notwithstanding, no other foreign language study was found.
Data Extraction
Besides information about study design, characteristics, and sample size, we extracted the following data from the articles: actual numbers of survivors and non-survivors and corresponding cohort sizes and event rates. Survival to discharge was the primary outcome variable, but we also obtained outcome data on: return of spontaneous circulation (ROSC); 30-day survival; favourable neurologic outcome. If survival to discharge data were not available, we used 30-day survival as the primary outcome.
Statistical Analysis
We performed the analysis with the Comprehensive Meta Analysis software, version 2.2.050 (Biostat, Englewood, NJ). Risk ratios (RR) and 95% confidence intervals were (re-)calculated for each study and pooled in both a fixed-effects and random effects model. However, since the heterogeneity of within all meta-analyses was negligible, as indicated by an I2 statistics of 0%, we report only the results of the fixed-effects model. The Comprehensive Meta Analysis software uses the inverse variance method for weighing studies; however other methods can be selected, such as Mantel-Haenszel. The results in our meta-analyses did not differ between each method. The primary analysis included only randomized controlled trials, and the secondary analysis observational cohort studies.
Heterogeneity among studies was formally assessed by the Q and I2 statistics. Publication bias was tested with the Egger’s regression test.
Results
The systematic review identified three randomized clinical trials where adult patients suffering from out-of-hospital cardiac arrest received dispatcher-assisted bystander CPR that was randomized to either chest compression-only CPR or standard CPR including rescue ventilation.14–16 The quality of these trials was high; all reported their outcomes on an intention-to-treat analysis, had scarce missing data and had a low rate of intervention cross-overs. All three trials were included in the meta-analysis and we used survival to discharge as primary outcome in our analysis (Figure 1). Uniformly, each of the three clinical trials showed individually a small, but statistically non-significant, survival benefit for patients who received chest compression-only CPR. After pooling the studies in a meta-analysis, chest compression-only bystander CPR was associated with a statistically significant 22% improved chance of survival (risk ratio [RR] 1.22 [95% confidence interval {CI}, 1.01 – 1.47]) compared to standard CPR (Figure 2). The meta-analysis had no heterogeneity as indicated by an I2 of 0. The absolute increase in survival was 2.4% and the number needed to treat was 41.
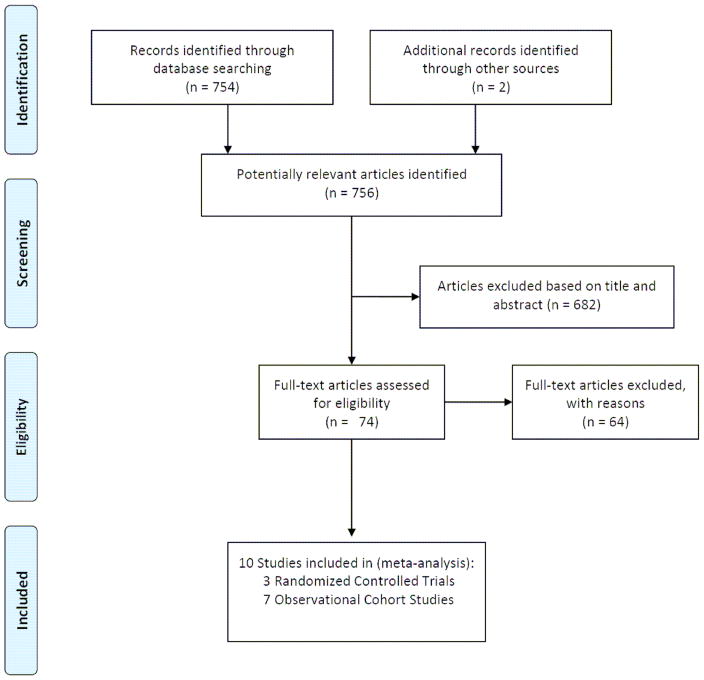
Figure 1.
Study Selection Process for Studies Included in Meta-Analysis (based on PRISMA guidelines).17
Figure 2.
Primary Analysis of Randomized Controlled Trials in Chest Compression-Only CPR
In a secondary systematic review, all observational cohort studies were identified that investigated chest compression-only bystander-CPR versus standard CPR (not dispatcher-assisted). After a comprehensive search, seven articles were identified that met the search criteria (Figure 1). Out of 74 articles with suggestive titles and abstract, 64 had to be excluded because they did not report any chest compression-only CPR data. It must be pointed out that none of these non-randomized studies investigated dispatcher-assisted CPR. All seven studies investigated prospectively or retrospectively the association between the CPR method lay bystander performed (chest compression-only or standard CPR) and survival.
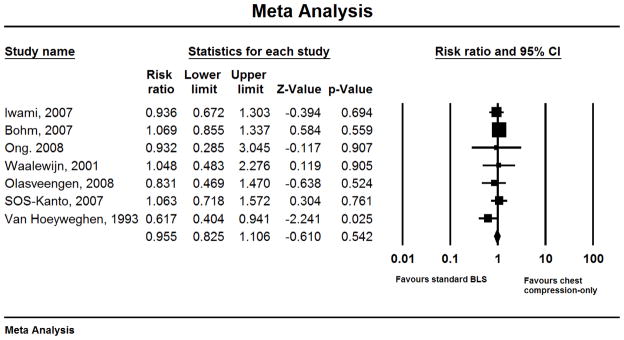
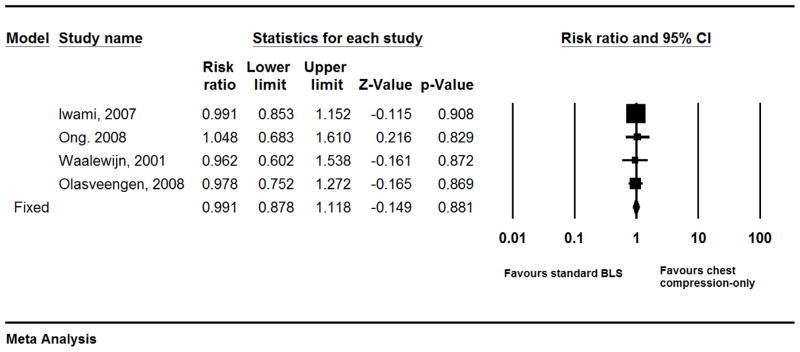
Except for one study,12 all observational studies showed no statistically significant survival difference between the two CPR methods. It is of note that despite our intention to use survival to discharge as the primary outcome in the meta-analysis, we had to use 30-day survival for lack of reporting survival to discharge data in 2 studies.7, 8 In the pooled meta-analysis of all observational cohort studies (Figure 3), chest compression-only CPR was not associated with a difference in survival compared to standard CPR (RR, 0.96 [95% CI, 0.83 – 1.11]; I2, 0%). Furthermore, chest compression-only CPR did not improve the rate of return of spontaneous circulation (RR, 0.99 [95% CI, 0.88 – 1.12]; I2, 0%; Figure 4).
Figure 3.
Secondary Analysis of Observational Cohort Studies in Chest Compression-Only CPR
Figure 4.
Return of Spontaneous Circulation in Chest Compression-Only CPR
Discussion
The results of this meta-analysis show that dispatcher-assisted chest compression-only bystander CPR is associated with improved survival after out-of-hospital cardiac arrest in adults patients compared to standard CPR (chest compression plus rescue ventilation).
Since meta-analyses are statistical tools for pooling existing evidence, we should consider the strength of the evidence favouring chest compression-only CPR. Despite the small number of trials included in this meta-analysis,14–16 the evidence favouring dispatcher-assisted chest compression-only CPR appears to be robust since all randomized clinical trials found a similar, albeit statistically non-significant, positive effect of chest compression-only CPR on survival. The effect size may appear small (~22%), but rates of survival after out-of-hospital cardiac arrest have been stagnating around 4–8 % for the last decades and thus a 22% increase in survival may actually represent an important progress. The incidence of cardiac arrest is about 0.5/1000 in North America.19 Extrapolating this number to include North America and the European Union (population: ~850 mio.), an absolute 2% increase of survival (as found in our meta-analysis), e.g. from 10% to 12% (20% relative increase), would mean an additional 8,000 lives saved per year.
The main reason why neither clinical trial showed a benefit of dispatcher-assisted chest compression-only CPR over standard CPR was probably because of lack of adequate power. The fact that only three clinical trials investigating dispatcher-assisted chest compression-only CPR have ever been conducted in out-of-hospital cardiac arrest, speaks for the difficulty of conducting well-designed prospective studies in this setting. Well identified challenges involve obtaining informed consent, the limited time to randomize patients, the fidelity of following the study protocol, the tracking of patients and outcomes and the difficulties in blinding the interventions. Because survival rates after out-of-hospital cardiac arrest are low and large treatment effects unlikely, very large sample sizes are required to show a statistically significant survival benefit. No chest compression-only clinical trial had more than 125 “events” (survivors) in a study arm, a number that may be considered fairly small for statistical analyses.
A second question that needs to be addressed is the plausibility of our findings. While being considered a controversial topic,20, 21 several independent lines of evidence suggest that chest compression-only CPR, assisted by dispatchers but perhaps also for non-assisted bystander CPR, may indeed be superior to standard bystander CPR in out-of-hospital cardiac arrest. Because this topic has been intensively discussed over the last few years, only the most pertinent explanations will be mentioned. The importance of uninterrupted, high-quality chest compressions for CPR success has been repeatedly documented.22–24 Limiting hands-off time, both for lay people and healthcare professionals, is an important predictor for survival after cardiac arrest. By avoiding rescue ventilations during CPR, which are commonly fairly time-consuming for lay bystanders,25 a continuous uninterrupted coronary perfusion pressure is maintained which increases the probability of a successful outcome.6 It should be noted that these considerations were the main reason to increase the compression:ventilation ratio for standard BLS from 15:2 to 30:2 in the 2005 resuscitation guidelines. All three dispatcher-assisted CPR trials used the old 15:2 ratio. It is unclear if using the current 30:2 ratio would have changed the results. Secondly, particularly for witnessed cardiac arrest it may be of less importance to provide oxygenation and ventilation during the first minutes than to provide high-quality chest compressions. Thirdly, chest compression-only CPR is easier to teach, to learn and to perform compared to the fairly complex standard CPR algorithm, thus increasing the chances of bystander to intervene and provide any CPR.
It is an interesting observation that our secondary meta-analysis that included only observational cohort studies and not randomized controlled trials, did not show any benefit of chest compression-only CPR compared to standard CPR. It needs, again, be pointed out that these observational studies did not investigate dispatcher-assisted bystander CPR, but aimed to investigate the chances of survival after out-of-hospital cardiac arrest between chest compression-only and standard CPR. In none of these studies, chest compression-only CPR had been taught to bystanders; rather, it was a deliberate decision of the lay bystander to avoid mouth-to-mouth rescue ventilation. While evidence suggests now that dispatcher-assisted chest compression-only CPR may be superior to standard CPR in adult out-of-hospital cardiac arrest, several special circumstances exist where chest compression-only CPR may not be beneficial. Recent evidence from a large-scale prospective cohort study indicates that in cardiac arrest from non-cardiac causes, e.g., drowning, trauma, asphyxia, standard CPR may actually improve survival.26 Moreover, in paediatric out-of-hospital cardiac arrest which is also commonly of non-cardiac origin, a similar benefit may be conferred by standard CPR as well.27 Therefore, it appears that the benefits of chest compression-only bystander CPR are largest in adult patients suffering from “cardiac” arrest.
In summary, findings from this meta-analysis provide evidence that in adult out-of-hospital cardiac arrest dispatcher-assisted chest compression-only bystander CPR is associated with improved survival compared to standard CPR (chest compressions plus rescue ventilations). It is, however, unclear if unassisted chest compression-only bystander CPR provides similar survival benefits.
Table 1.
Characteristics of Included Studies on Chest Compression-Only CPR
| Source | Study Design | Number of Survivors/Patients Chest Compression Only | Number of Survivors/Patients Standard CPR | Missing Outcome data | Primary Outcome | Secondary Endpoints |
|---|---|---|---|---|---|---|
| Randomized Controlled Trials | ||||||
| Hallstrom et al.,14 2000 | RCT | 35/240 (14.6%) | 29/278 (10.4%) | 2/520 (0.4%) | Survival to hospital discharge | Admission to hospital; neurologic status of survivors |
| Rea et al.,15 2010 | RCT | 122/978 (12.5%) | 105/958 (11.0%) | 7/1941 (0.4%) | Survival to hospital discharge | Favorable neurologic outcome at discharge |
| Svensson et al.,162010 | RCT | 54/282 (19.1%)* | 44/297 (14.8%)* | 0/1276 (0%) [30-day] 697/1276 (54.6%) [survival to discharge] | 30-day survival | 1-day survival; Survival to hospital discharge |
| Observational Cohort Studies** | ||||||
| Van Hoeyweghen et al.,12 1993 | retrospective | 26/263 (9.9%) | 71/443 (16.0%) | Not reported | Awake 14 days after CPR | |
| Waalewijn et al.,13 2001 | prospective | 6/41 (14.6%) | 61/437 (14.0%) | Not reported | Admission to hospital; Survival to hospital discharge | |
| SOS-Kanto study-group;11 2007 | prospective | 38/439 (8.7%) | 58/712 (8.1%) | 0/4068 (0%) | Favorable neurologic outcome 30 days after cardiac arrest | 30-day survival |
| Bohm et al.,7 2007 | retrospective | 82/1145 (7.2%) | 550/8209 (6.7%) | 0/11275 (0%) | Admission to hospital; 30-day survival | |
| Iwami et al.,8 2007 | prospective | 52/544 (9.6%) | 80/783 (10.2%) | 25/23438 (0.1%) | Favorable neurologic outcome 1 year after cardiac arrest | ROSC; admission to hospital; 1-week, 30-day, 1-year survival |
| Olasveengen et al.,9 2008 | retrospective | 15/145 (10.3%) | 35/281 (12.5%) | Not reported | Survival to hospital discharge | ROSC; admission to hospital |
| Ong et al.,10 2008 | Prospective | 4/154 (2.6%) | 8/287 (2.8%) | Not reported | Survival to hospital discharge | 30-day survival |
To ensure consistence between the three randomized clinical trials, we list survival to discharge in the study by Svensson et al. Their primary outcome (30-day survival) has 54/620 (8.7%) survivors in the chest compression-only CPR group and 46/656 (7.0%) in the standard CPR group.
In the observational cohort studies, data used for the meta-analysis were survival to discharge, except when this information was unavailable (Van Hoeyweghen et al.: awake after 14 days; Bohm et al. and SOS-Kanto: 30-day survival; Iwami et al: 1 week survival).
Acknowledgments
Funding: National Institutes of Health and American Heart Association
The authors would like to thank Professor J. Philipp Miller, director division of Biostatistics, Washington University School of Medicine, St. Louis, MO for his statistical contributions during manuscript preparation and revision.
PN is being supported by grants from the National Institute of General Medical Sciences, National Institutes of Health (NIH) and from the American Heart Association.
Footnotes
Contributors
PN was responsible for study design, acquisition of data, statistical analysis and drafting of the manuscript. All authors contributed to the study concept, critical data interpretation and the preparation and revision of the manuscript.
Conflicts of Interest
PN is receiving research support from Roche Diagnostics, unrelated to this study. MH is receiving salary from St. John’s Ambulance Service, Vienna, Austria and received research support, lecture fees and travel support from Novo Nordisk. HFS does not report a conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Michael Hüpfl, Email: michael.huepfl@meduniwien.ac.at, Dept of Anesthesiology, Critical Care and Pain Therapy, Medical University of Vienna, Austria.
Harald F Selig, Email: harald.se@gmx.at, Dept of Anesthesiology, Critical Care and Pain Therapy, Medical University of Vienna, Austria.
Peter Nagele, Email: nagelep@wustl.edu, peter.nagele@meduniwien.ac.at, Dept of Anesthesiology, Washington University School of Medicine, St. Louis, MO; Dept of Anesthesiology, Critical Care and Pain Therapy, Medical University of Vienna, Austria.
References
- 1.Koster RW. Mouth-to-mouth ventilation and/or chest compression in basic life support: The debate continues. Resuscitation. 2008;77(3):283–5. doi: 10.1016/j.resuscitation.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 2.Nolan J. Push, blow or both: Is there a role for compression-only CPR? Anaesthesia. 2010;65(8):771–4. doi: 10.1111/j.1365-2044.2010.06448.x. [DOI] [PubMed] [Google Scholar]
- 3.2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005 Dec 13;112(24 Suppl):IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 4.Handley AJ, Koster R, Monsieurs K, Perkins GD, Davies S, Bossaert L. European Resuscitation Council Guidelines for Resuscitation 2005: Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation. 2005 Dec;67(Supplement 1):S7–S23. doi: 10.1016/j.resuscitation.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 5.Ewy GA, Zuercher M, Hilwig RW, Sanders AB, Berg RA, Otto CW, et al. Improved neurological outcome with continuous chest compressions compared with 30:2 compressions-to-ventilations cardiopulmonary resuscitation in a realistic swine model of out-of-hospital cardiac arrest. Circulation. 2007;116(22):2525–30. doi: 10.1161/CIRCULATIONAHA.107.711820. [DOI] [PubMed] [Google Scholar]
- 6.Sanders AB, Kern KB, Berg RA, Hilwig RW, Heidenrich J, Ewy GA. Survival and neurologic outcome after cardiopulmonary resuscitation with four different chest compression-ventilation ratios. Annals of Emergency Medicine. 2002;40(6):553–62. doi: 10.1067/mem.2002.129507. [DOI] [PubMed] [Google Scholar]
- 7.Bohm K, Rosenqvist M, Herlitz J, Hollenberg J, Svensson L. Survival Is Similar After Standard Treatment and Chest Compression Only in Out-of-Hospital Bystander Cardiopulmonary Resuscitation. Circulation. 2007 December 18;116(25):2908–12. doi: 10.1161/CIRCULATIONAHA.107.710194. [DOI] [PubMed] [Google Scholar]
- 8.Iwami T, Kawamura T, Hiraide A, Berg RA, Hayashi Y, Nishiuchi T, et al. Effectiveness of Bystander-Initiated Cardiac-Only Resuscitation for Patients With Out-of-Hospital Cardiac Arrest. Circulation. 2007 December 18;116(25):2900–7. doi: 10.1161/CIRCULATIONAHA.107.723411. [DOI] [PubMed] [Google Scholar]
- 9.Olasveengen TM, Wik L, Steen PA. Standard basic life support vs. continuous chest compressions only in out-of-hospital cardiac arrest. Acta Anaesthesiologica Scandinavica. 2008;52(7):914–9. doi: 10.1111/j.1399-6576.2008.01723.x. [DOI] [PubMed] [Google Scholar]
- 10.Ong MEH, Ng FSP, Anushia P, Tham LP, Leong BSH, Ong VYK, et al. Comparison of chest compression only and standard cardiopulmonary resuscitation for out-of-hospital cardiac arrest in Singapore. Resuscitation. 2008;78(2):119–26. doi: 10.1016/j.resuscitation.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 11.SOS-KANTO Study Group. Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. The Lancet. 2007;369(9565):920–6. doi: 10.1016/S0140-6736(07)60451-6. [DOI] [PubMed] [Google Scholar]
- 12.Van Hoeyweghen RJ, Bossaert LL, Mullie A, Calle P, Martens P, Buylaert WA, et al. Quality and efficiency of bystander CPR. Resuscitation. 1993 Aug;26(1):47–52. doi: 10.1016/0300-9572(93)90162-j. [DOI] [PubMed] [Google Scholar]
- 13.Waalewijn RA, Tijssen JG, Koster RW. Bystander initiated actions in out-of-hospital cardiopulmonary resuscitation: results from the Amsterdam Resuscitation Study (ARRESUST) Resuscitation. 2001 Sep;50(3):273–9. doi: 10.1016/s0300-9572(01)00354-9. [DOI] [PubMed] [Google Scholar]
- 14.Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary Resuscitation by Chest Compression Alone or with Mouth-to-Mouth Ventilation. New England Journal of Medicine. 2000;342(21):1546–53. doi: 10.1056/NEJM200005253422101. [DOI] [PubMed] [Google Scholar]
- 15.Rea TD, Fahrenbruch C, Culley L, Donohoe RT, Hambly C, Innes J, et al. CPR with Chest Compression Alone or with Rescue Breathing. New England Journal of Medicine. 2010;363(5):423–33. doi: 10.1056/NEJMoa0908993. [DOI] [PubMed] [Google Scholar]
- 16.Svensson L, Bohm K, Castrèn M, Pettersson H, Engerström L, Herlitz J, et al. Compression-Only CPR or Standard CPR in Out-of-Hospital Cardiac Arrest. New England Journal of Medicine. 2010;363(5):434–42. doi: 10.1056/NEJMoa0908991. [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG Group tP. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Annals of Internal Medicine. 2009 August 18;151(4):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 18.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of Observational Studies in Epidemiology: A Proposal for Reporting. JAMA. 2000 April 19;283(15):2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 19.Nichol G, Thomas E, Callaway CW, Hedges J, Powell JL, Aufderheide TP, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008 Sep 24;300(12):1423–31. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ewy GA. Continuous-chest-compression cardiopulmonary resuscitation for cardiac arrest. Circulation. 2007 Dec 18;116(25):2894–6. doi: 10.1161/CIRCULATIONAHA.107.751065. [DOI] [PubMed] [Google Scholar]
- 21.Gold LS, Eisenberg M. Chest-compression-only vs. standard cardiopulmonary resuscitation: Shouldn’t we wait for more evidence? Prehospital Emergency Care. 2008;12(3):406–9. doi: 10.1080/10903120802096696. [DOI] [PubMed] [Google Scholar]
- 22.Cardiopulmonary resuscitation by bystanders with chest compression only (SOS-KANTO): an observational study. Lancet. 2007 Mar 17;369(9565):920–6. doi: 10.1016/S0140-6736(07)60451-6. [DOI] [PubMed] [Google Scholar]
- 23.Berg RA, Kern KB, Sanders AB, Otto CW, Hilwig RW, Ewy GA. Bystander cardiopulmonary resuscitation. Is ventilation necessary? Circulation. 1993 Oct;88(4 Pt 1):1907–15. doi: 10.1161/01.cir.88.4.1907. [DOI] [PubMed] [Google Scholar]
- 24.Kern KB, Hilwig RW, Berg RA, Sanders AB, Ewy GA. Importance of continuous chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay-rescuer scenario. Circulation. 2002 Feb 5;105(5):645–9. doi: 10.1161/hc0502.102963. [DOI] [PubMed] [Google Scholar]
- 25.Heidenreich JW, Higdon TA, Kern KB, Sanders AB, Berg RA, Niebler R, et al. Single-rescuer cardiopulmonary resuscitation: ‘Two quick breaths’ - An oxymoron. Resuscitation. 2004;62(3):283–9. doi: 10.1016/j.resuscitation.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 26.Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Hiraide A. Bystander-initiated rescue breathing for out-of-hospital cardiac arrests of noncardiac origin. Circulation. 2010;122(3):293–9. doi: 10.1161/CIRCULATIONAHA.109.926816. [DOI] [PubMed] [Google Scholar]
- 27.Kitamura T, Iwami T, Kawamura T, Nagao K, Tanaka H, Nadkarni VM, et al. Conventional and chest-compression-only cardiopulmonary resuscitation by bystanders for children who have out-of-hospital cardiac arrests: a prospective, nationwide, population-based cohort study. The Lancet. 2010;375(9723):1347–54. doi: 10.1016/S0140-6736(10)60064-5. [DOI] [PubMed] [Google Scholar]