Abstract
Signal transducer and activator of transcription 3 (STAT3) is an oncogenic transcription factor implicated in prostate carcinogenesis. The present study demonstrates that diallyl trisulfide (DATS), a promising cancer chemopreventive constituent of processed garlic, inhibits phosphorylation of STAT3 in prostate cancer cells in culture and in vivo. Exposure of DU145 and LNCaP human prostate cancer cells to growth suppressive and pharmacologically-relevant concentrations of DATS (20 and 40 µmol/L) resulted in suppression of constitutive (DU145) as well as interleukin-6 (IL-6)-induced (LNCaP) phosphorylation of STAT3 (Tyr705), which correlated with inhibition of Janus-activated kinase 2 phosphorylation. Constitutive and/or IL-6-induced nuclear translocation of pSTAT3 and STAT3 dimerization was also inhibited markedly on treatment with DATS in both cell lines. Inhibition of prostate cancer development in Transgenic Adenocarcinoma of Mouse Prostate (TRAMP) mice by gavage of DATS correlated with a visible decrease in the levels of pSTAT3. Interestingly, the IL-6-mediated activation of STAT3 largely failed to confer protection against proapoptotic response to DATS in both cells. Likewise, the DATS-mediated inhibition of cell migration was either not affected or minimally reversed by the IL-6 treatment or ectopic expression of constitutively active STAT3. In conclusion, the present study indicates that DATS treatment suppresses STAT3 phosphorylation in prostate cancer cells in culture and in vivo, but activation of this oncogenic transcription factor is largely dispensable for cellular responses to DATS. Ability of DATS to overcome STAT3 activation is a therapeutic advantage for this chemopreventive agent.
Keywords: STAT3, Prostate Cancer, Diallyl Trisulfide, Chemoprevention
Introduction
Signal transducer and activator of transcription 3 (STAT3) is an oncogenic transcription factor belonging to the seven member STAT gene family (1). The STAT3 is activated by phosphorylation of Tyr705 at the C-terminus (1,2). The STAT3 is constitutively active in a large fraction of human prostate cancer cells and clinical prostate cancers (4–7), and its hyperactivity is associated with advanced stage of the disease (3,7). Furthermore, STAT3 activation promotes survival and inhibits apoptosis in prostate cancer cells (8,9). The STAT3 regulates expression of genes common to wound healing and cancer (10). Agents that are safe but can either suppress activation of STAT3 or overcome STAT3 activation for their anticancer effects are attractive for prevention and treatment of prostate cancer. Natural products have attracted tremendous attention for the discovery of novel agents potentially useful for prevention and treatment of human cancers (11–13).
Epidemiologic studies continue to support the premise that dietary intake of Allium vegetables, such as garlic, may be protective against risk of various malignancies including cancer of the prostate (14–16), which is a leading cause of cancer related deaths among American men (17). In a population-based case-control study, the risk of prostate cancer was found to be significantly lower in men consuming >10 g/d of total Allium vegetables than in men with total Allium vegetable intake of <2.2 g/d (16). Anticancer effect of Allium vegetables, which have been used for medicinal purposes throughout the recorded history (18), is attributed to organosulfur compounds (OSC) that are generated on cutting or chewing of these vegetables (19). Garlic-derived OSCs, including diallyl trisulfide (DATS), have been shown to afford significant protection against cancer in animal models induced by a variety of chemical carcinogens (20–25). The OSC-mediated prevention of chemically-induced cancer in experimental rodents correlates with induction of phase 2 carcinogen-detoxifying enzymes as well as inhibition of phase 1 carcinogen-activating enzymes (26–28). Studies from our laboratory have demonstrated that gavage of DATS not only retards growth of PC-3 human prostate cancer cells subcutaneously implanted in male athymic mice but also affords significant protection against cancer development in Transgenic Adenocarcinoma of Mouse Prostate (TRAMP) mice without causing any toxicity (29,30).
In human prostate cancer cells, the DATS treatment has been shown to cause cell cycle arrest, apoptosis induction, and transcriptional repression of androgen receptor (31–37). The DATS treatment also inhibits angiogenic features in human umbilical vein endothelial cells (38). The mechanisms underlying growth arrest and apoptosis induction by DATS have been investigated thoroughly in human prostate cancer cells (31–37). We showed previously that the DATS-induced apoptosis in prostate cancer cells correlates with down-regulation and phosphorylation of Bcl-2 (31). Because Bcl-2 is one of the targets of STAT3 (39), it was of interest to determine the role of this transcription factor in DATS-induced apoptosis. The present study demonstrates that DATS inhibits activation of STAT3 in prostate cancer cell in culture as well as in vivo, but this transcription factor in largely dispensable for cellular anticancer responses to DATS.
Materials and Methods
Reagents
DATS (purity >98%) was purchased from LKT Laboratories. Cell culture reagents were purchased from Life Technologies, whereas interleukin-6 (IL-6), eosin, and anti-actin antibody were obtained from Sigma-Aldrich. Antibodies against phospho- STAT3 (pSTAT3; Tyr705), phospho-Janus-activated kinase 2 (pJAK2; Tyr1007/1008), total STAT3, and total JAK2 were obtained from Cell Signaling. The pSTAT3 (Tyr705) antibody used for immunofluorescence microscopy was procured from Santa Cruz Biotechnology. Cytoplasmic histone-associated apoptotic DNA fragmentation was measured using a kit from Roche (Mannheim, Germany).
Cell lines
Prostate cancer cell lines LNCaP and DU145 were purchased from the American Type Culture Collection (ATCC) in 2004–2005 and maintained as previously described (31,36). Cell line authentication was done to test for inter-species contamination and alleles for 9 different short tandem repeats (performed by RADIL, University of Missouri, Columbia, MO) identifiable in ATCC database. The cells were last tested in July, 2010. Each cell line was found to be of human origin and no mammalian inter-species contamination was detected. Moreover, the genetic profiles for the LNCaP and DU145 were found to be consistent with the genetic profiles in the ATCC database. Stock solution of DATS was prepared in dimethyl sulfoxide (DMSO) and an equal volume of DMSO (final concentration <0.2%) was added to the controls.
Immunoblotting
Cells were treated with DATS and/or IL-6 for specified time periods and lysed as described by us previously (40). Cell lysates were cleared by centrifugation at 14,000 rpm for 20 minutes. Lysate proteins were resolved by sodium-dodecyl sulfate-polyacrylamide gel electrophoresis and transferred onto polyvinylidene fluoride membrane. After blocking with 5% (w/v) non-fat dry milk solution in Tris-buffered saline containing 0.05% Tween- 20, the membrane was incubated with the desired primary antibody for 2 hours at room temperature or overnight at 4°C. The membrane was treated with an appropriate secondary antibody for 1 hour at room temperature. The immunoreactive bands were visualized by the enhanced chemiluminescence method. The blots were stripped and reprobed with anti-actin antibody to normalize for differences in protein loading. The intensity of the immunoreactive band was determined by densitometric scanning to quantify changes in protein levels. Quantitation of the immunoreactive bands was performed using Image-QuaNT (version 4.2a) software (Molecular Dynamics, Sunnyvale, CA).
Immunocytochemical analysis for nuclear localization of pSTAT3
Nuclear translocation of pSTAT3 was determined by immunocytochemistry. Briefly, DU145 or LNCaP cells (104 cells/mL) were cultured on coverslips and allowed to attach by overnight incubation. The cells were treated with 20 or 40 µmol/L DATS in the absence or presence of 25 ng/mL IL-6 for 3 or 24 hours at 37°C. After washing with phosphate-buffered saline (PBS), the cells were fixed with 2% paraformaldehyde for 1 hour at room temperature and permeabilized using 0.05% Triton X-100 for 5 minutes. The cells were then incubated with PBS supplemented with 0.5% bovine serum albumin and 0.15% (w/v) glycine for 1 hour followed by overnight incubation with anti-pSTAT3 antibody (1:500 dilution) at 4°C. The cells were then treated with 2 µg/mL Alexa Fluor 568-conjugated secondary antibody (Molecular Probes) for 1 hour at room temperature. After washing with PBS, the cells were counterstained with 0.5 µmol/L SytoxGreen for 3 minutes at room temperature. The cells were washed with PBS, mounted and observed under a Leica DC300F microscope at ×100 objective magnification.
Analysis of STAT3 dimerization
Cells were treated for 24 hours with 20 or 40 µmol/L DATS in the absence (DU145) or presence of 10 ng/mL IL-6 (LNCaP). Subsequently, protein extracts were prepared as described by Shin et al. (41). Proteins were resolved by 6% non-denaturing gel electrophoresis and transferred onto polyvinylidene fluoride membrane. The membrane was probed with anti-STAT3 antibody as described above.
Immunohistochemical analysis of pSTST3 in TRAMP tissues
We used prostate tissues from control and DATS-treated TRAMP mice to determine the effect of DATS administration on pSTST3 expression in vivo (30). Prostate tissues were sectioned at 5 µm thickness, quenched with 3% hydrogen peroxide, and blocked with normal serum. The sections were then incubated with the pSTAT3 primary antibody and washed with Tris-buffered saline followed by incubation with appropriate secondary antibody. Characteristic brown color was developed by incubation with 3,3-diaminobenzidine. The sections were counterstained with Meyers Hematoxylin (Sigma) and examined under a Leica microscope.
Cell viability and apoptosis assays
Viability of DU145 and LNCaP cells following 24 hours of treatment with DATS (20 or 40 µmol/L) and/or IL-6 (25 ng/mL) was determined by trypan blue dye exclusion assay as described by us previously (31). Apoptosis in DATS and/or IL-6-treated cells (24 hour exposure) was assessed by analysis of histone-associated DNA fragment release into the cytosol (31).
Reverse transcription-PCR
Total RNA from DU145 or LNCaP cells treated for 24 hours with DATS (20 or 40 µmol/L) and/or IL-6 (25 ng/mL) was extracted using RNeasy kit (Invitrogen). Complementary DNA was synthesized from 2 µg of total RNA with reverse transcriptase and oligo(dT)20. Reverse transcription-PCR was carried out using High Fidelity Taq Polymerase (Invitrogen), 0067ene-specific primers, and cDNA. The primers were as follows; (a) Bcl-2 Forward- 5'-TGCACCTGACGCCCTTCAC-3' and Reverse-5'-TAGCTGATTCGACGTTTTGCCTGA-3' (product size 560 bp), and (b) Bcl-xL Forward-5'CCCAGAAAGGATACAGCTGG-3' and Reverse- 5'-GCGATCCGACTCACCAATAC-3' (product size 448bp). Amplification conditions were as follows: Bcl-2 94°C/2 minutes, 25 cycles 94°C/15 s, 69°C/1 minute, 72°C/2 minutes, and 72°C/8 minutes; Bcl-xL 94°C/2 minutes, 25 cycles 94°C/45 s, 56°C/30 s, 72°C/60 s, and 72°C/8 minutes. The house keeping gene β-actin was used as an internal control and amplified using the primers Forward- 5'-CAAAGACCTGTACGCCAACAC-3' and Reverse- 5'-CATACTCCTGCTTGCTGATCC-3' (product size 277 bp) and the amplification conditions of 95°C/3 minutes, 18 cycles 95°C/60 s, 56°C/60 s, 68°C/60 s, and 68°C/10 minutes. The PCR products were resolved by 2% agarose gel pre-stained with ethidium bromide.
Migration assay
Migration of DU145 or LNCaP cells was determined using Transwell Boyden chamber (Corning, Acton, MA) containing a polycarbonate filter with a pore size of 8 µm as previously described by us (38). Briefly, 0.2 mL cell suspension containing 4×104 cells was mixed with 40 µmol/L DATS or DMSO (control) and the suspension was added to the upper compartment of the chamber. The lower compartment of the chamber contained 0.6 mL of cell culture medium (chemoattractant) containing the same concentrations of DATS or DMSO. After 24 hours of incubation at 37°C, non-migrant cells from the upper surface of the membrane were removed using a cotton swab. The membrane was washed with PBS and the migrated cells on the bottom face of the membrane were fixed with 90% ethanol and stained with eosin for 3 minutes. Four randomly selected fields were examined under a microscope at 10× objective magnification.
Stable overexpression of constitutively active STAT3
LNCaP cells were stably transfected with pIRES empty vector or vector encoding for constitutively active STAT3 (S3c; kindly provided by Dr. Beverly E Barton, UMDNJ-New Jersey Medical school, NJ; Ref. 9) using Fugene6 (Roche Applied Science). Several clones were selected and screened for overexpression of STAT3.
Statistical analysis
Statistical significance of difference in measured variables between control and treated groups was determined by one-way ANOVA followed by Bonferroni's test. Difference was considered significant at P<0.05.
Results
DATS inhibited constitutive and IL-6-induced activation of STAT3 in human prostate cancer cells
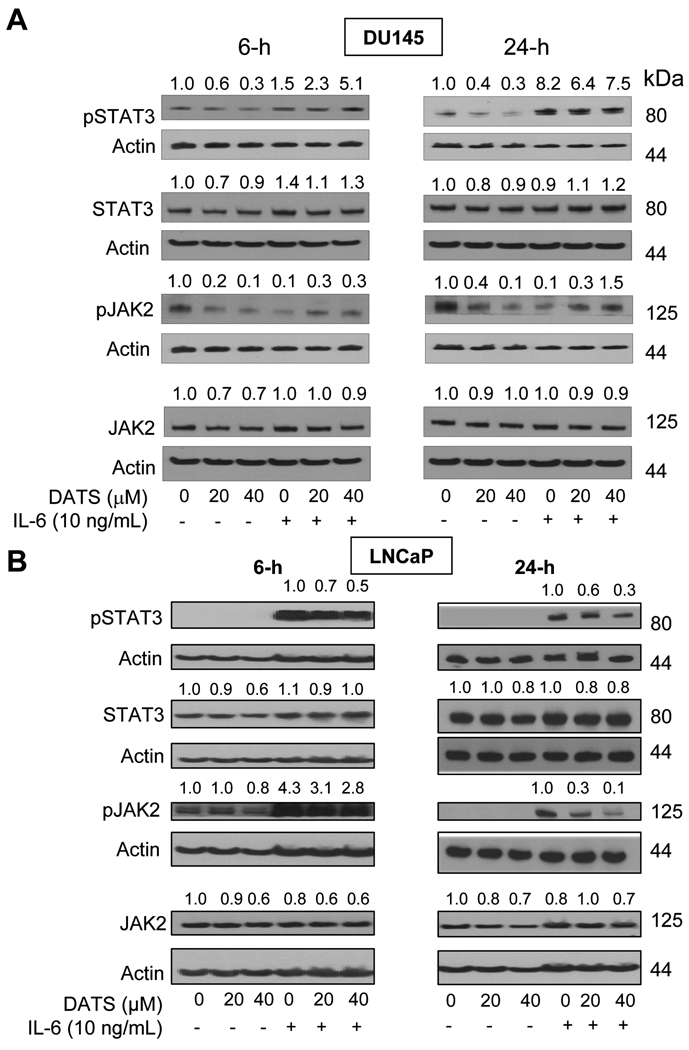
As shown in Fig. 1A, treatment of DU145 cells with DATS resulted in about 40–70% decrease in constitutive STAT3 phosphorylation at 6 and 24 hour time points. The pSTAT3 level was increased by 1.5- to 8.2-fold in the presence of 10 ng/mL IL-6 in DU145 cells. The IL-6-induced phosphorylation of STAT3 was decreased only slightly in the presence of DATS at the 24 hour time point (Fig. 1A). The DATS-mediated inhibition of constitutive STAT3 phosphorylation in DU145 cells did not correlate with decrease in level of total STAT3 protein. Constitutive phosphorylation of JAK2, an upstream kinase implicated in activation of STAT3 (42,43), was decreased by DATS treatment (Fig. 1A). Constitutive pSTAT3 was not detectable in the LNCaP cell line. Exposure of LNCaP cells to IL-6 for 6 or 24 hours resulted in a robust increase in phosphorylation of STAT3 at both time points. The IL-6-inducible activation of STAT3 was decreased in a concentration-dependent manner upon co-treatment with DATS (Fig. 1B), which was not due to down-regulation of total STAT3 protein (Fig. 1B). The DATS treatment inhibited IL-6-induced phosphorylation of JAK2 in the LNCaP cell line. The DATS-mediated inhibition of IL-6-inducible phosphorylation of JAK2 was comparatively more pronounced after 24 hours of treatment relative to the 6 hour time point (Fig. 1B). Nevertheless, these results showed that constitutive and/or IL-6-inducible activation of pSTAT3 in human prostate cancer cells was inhibited in the presence of DATS.
Fig. 1.
Immunoblotting for pSTAT3, total STAT3, pJAK2, and total JAK2 using lysates from (A) DU145 cells and (B) LNCaP cells treated for 6 or 24 hours with 20 or 40 µmol/L DATS in the absence or presence of 10 ng/mL IL-6. The blots were stripped and reprobed with anti-actin antibody to normalize for differences in protein level. Numbers on top of the immunoreactive bands represent change in protein level relative to corresponding DMSO-treated control. Immunoblotting for each protein was performed at least twice using independently prepared lysates, and representative data from one such experiment are shown.
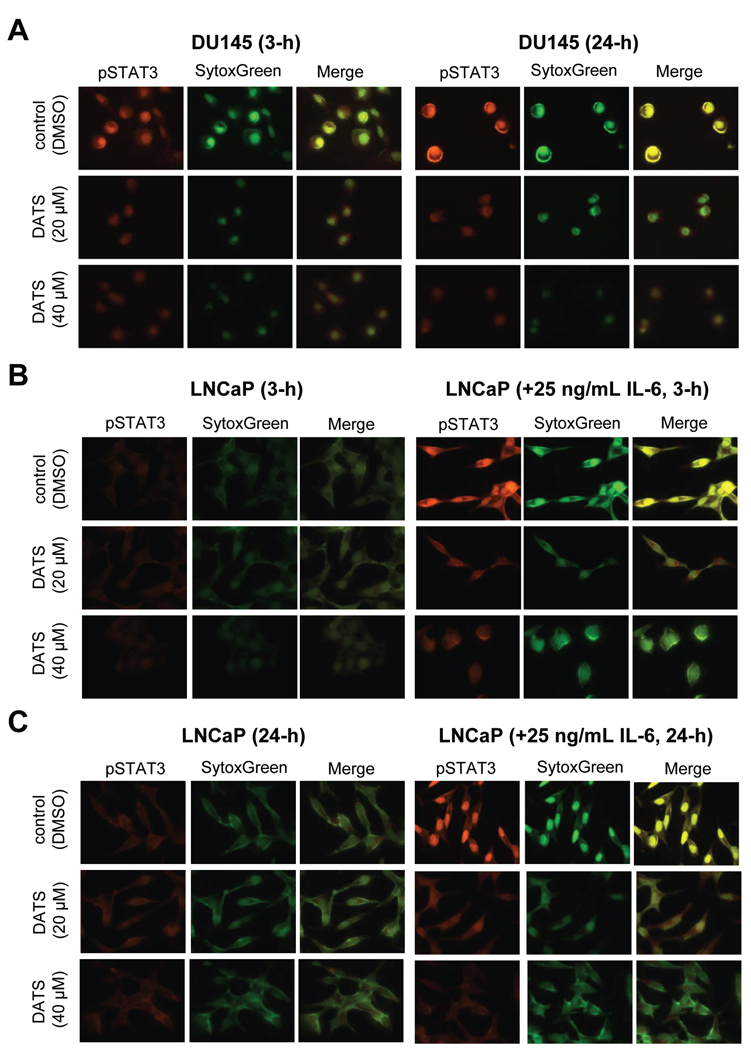
DATS treatment inhibited nuclear translocation of pSTAT3
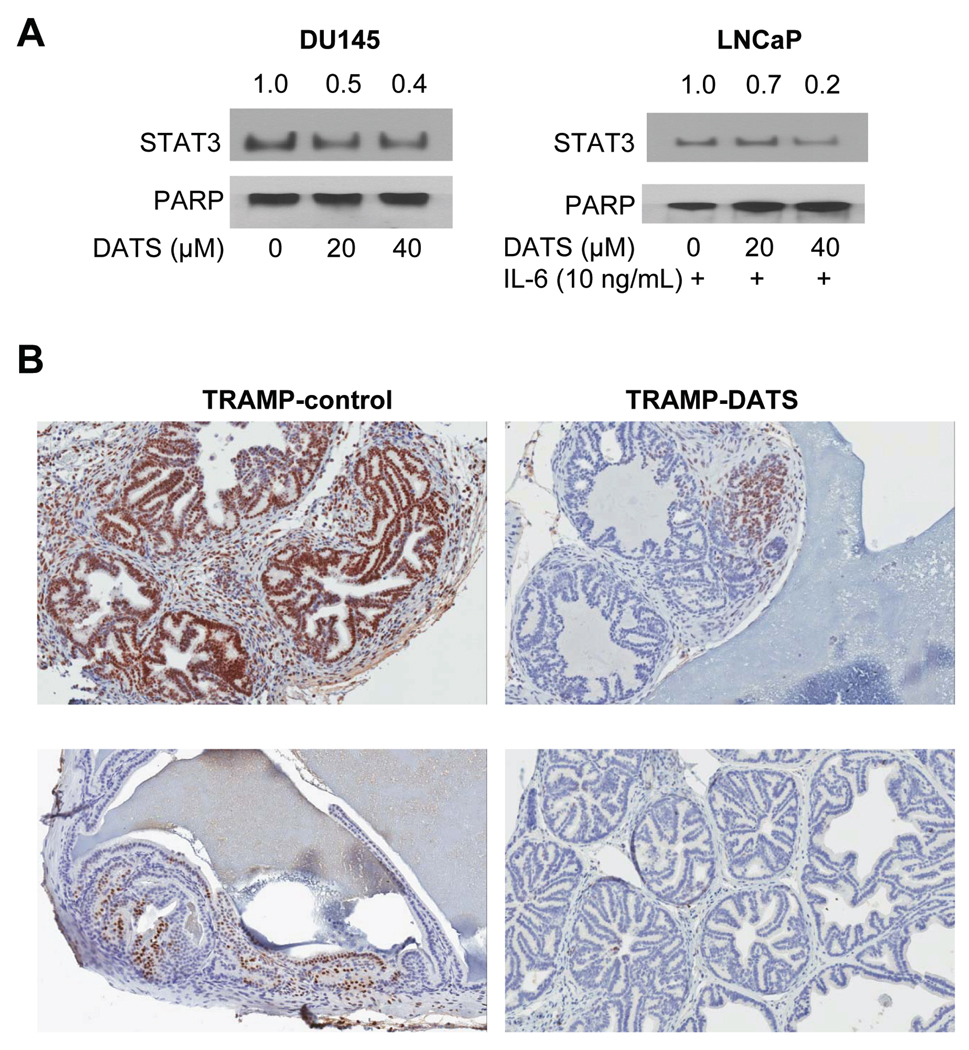
The Tyr705 phosphorylation of STAT3 results in its homodimerization or heterodimerization with other STATs enabling nuclear translocation of STAT3 for binding to specific sequences of target genes (1,2,43). Because DATS treatment decreased level of pSTAT3 in both cells, we designed experiments to determine the effect of DATS on nuclear translocation of pSTAT3. Immunostaining for pSTAT3 (red fluorescence) and SytoxGreen-associated nuclear staining (green fluorescence) in DU145 cells following 3 or 24 hour treatment with DMSO (control) or the indicated concentrations of DATS are shown in Fig. 2A. In DMSO-treated control DU145 cells, the pSTAT3 was detectable in both cytoplasm and nucleus at the 3 hour time point but its enrichment in the nucleus was clearly evident after 24 hours. Nuclear level of constitutively active pSTAT3 in DU145 cells was visibly reduced in the presence of DATS at both 20 and 40 µmol/L concentrations (Fig. 2A). Consistent with the immunoblotting results shown in Fig. 1B, immunostaining for pSTAT3 was very weak in DMSO-treated LNCaP cells at both 3 (Fig. 2B) and 24 hour time points (Fig. 2C). Nuclear level of pSTAT3 was increased on stimulation with IL-6 as evidenced by appearance of yellow color due to the merging of pSTAT3-associated red fluorescence and SytoxGreen-associated green fluorescence. The IL-6 stimulated nuclear translocation of pSTAT3 in LNCaP cells was inhibited in a concentration-dependent manner in the presence of DATS at both 3 (Fig. 2B) and 24 hour time points (Fig. 2C). In addition, DATS treatment (24-hour) resulted in suppression of constitutive (DU145) as well as IL-6-stimulated (LNCaP) dimerization of STAT3 (Fig. 3A). Collectively, these results demonstrated DATS-mediated inhibition of constitutive and IL-6-induced nuclear translocation of pSTAT3 as well as suppression of STAT3 dimer formation.
Fig. 2.
A, immunocytochemical analysis for pSTAT3 in DU145 cells following 3 or 24 hour treatment with DMSO (control) or DATS (20 or 40 µmol/L). B, immunocytochemical analysis for pSTAT3 in LNCaP cells following 3 hour treatment with DMSO (control) or DATS (20 or 40 µmol/L) in the absence or presence of 25 ng/mL IL-6. C, immunocytochemical analysis for pSTAT3 in LNCaP cells following 24 hour treatment with DMSO (control) or DATS (20 or 40 µmol/L) in the absence or presence of 25 ng/mL IL-6. Staining for pSTAT3 and nuclear DNA are indicated by red and green fluorescence, respectively (×100 objective magnification). Each experiment was repeated twice, and representative data from one such experiment are shown.
Fig. 3.
A, analysis for STAT3 dimerization in DU145 and LNCaP cells treated for 24 hours with 20 and 40 µmol/L DATS in the absence (DU145) or presence of 10 ng/mL IL-6 (LNCaP). Numbers on top of the immunoreactive bands represent change in STAT3 dimer level relative to DMSO-treated control. B, immunohistochemical detection of pSTAT3 in dorsolateral prostate of control and DATS-treated male TRAMP mice. Representative images from two different mice of each group are shown (×20 objective magnification). Mice of control group were gavaged with 0.1 mL PBS, whereas the experimental group of mice received 2 mg DATS/d in 0.1 mL PBS. Mice were gavage three times per wk for 13 wk (30).
DATS administration decreased level of pSTAT3 in the prostate of TRAMP mice
We have shown previously that gavage of 1 and 2 mg DATS/d (three times per wk for 13 wk) significantly inhibits incidence as well as burden (affected area) of poorly-differentiated cancer in male TRAMP mice without causing weight loss or any other side effects (30). Specifically, the incidence of poorly-differentiated cancer was decreased by about 34–41% in DATS-treated TRAMP mice compared with vehicle-treated controls (30). In the present study, we used the prostate tissues from the mice of control and 2 mg DATS groups of the same experiment to determine in vivo relevance of the cellular results showing DATS-mediated inhibition of pSTAT3 (Fig. 1). Representative images for pSTAT3 expression in the dorsolateral prostate of 2 individual mice of both groups are shown in Fig. 3B. Immunostaining for pSTAT3 was not uniform but detectable in the epithelial cells as well as in the stroma of dorsolateral prostate from control mice. The level of pSTAT3 was markedly lower in the prostate of DATS-treated mice compared with control (Fig. 3B). These results provided evidence for DATS-mediated suppression of STAT3 phosphorylation in vivo.
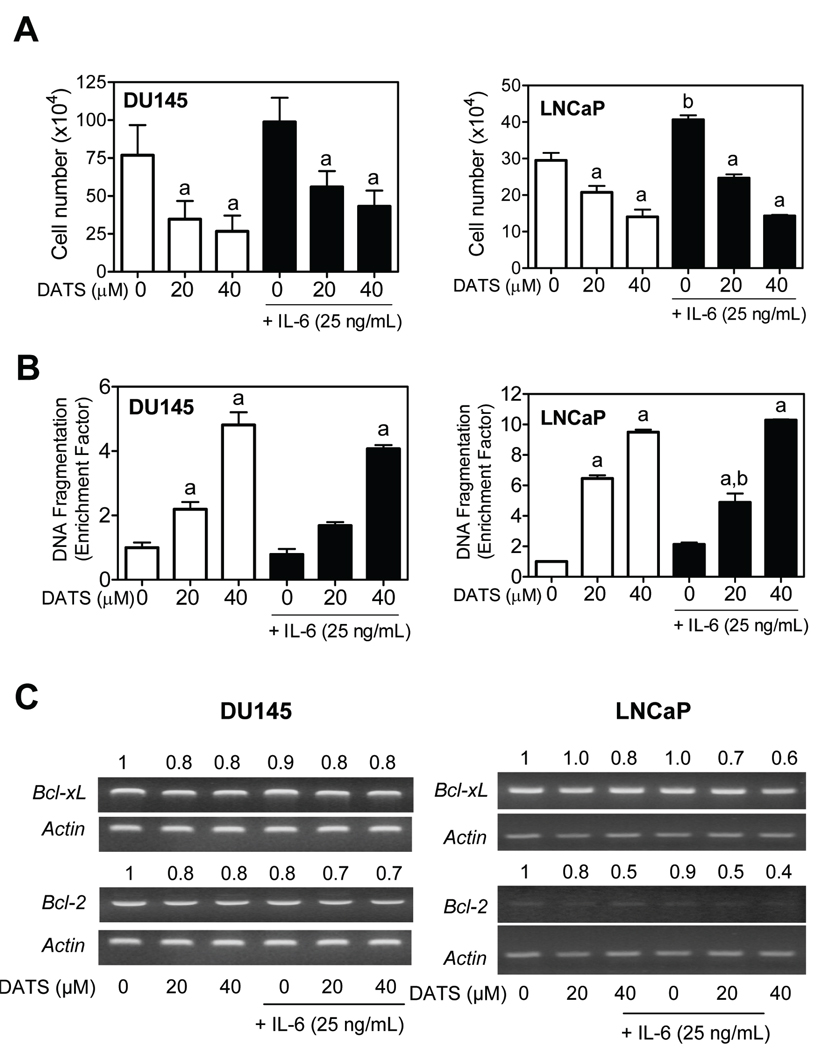
IL-6-stimulated STAT3 activation failed to confer resistance against DATS-induced apoptosis
Expression of many anti-apoptotic genes, including Bcl-2, Bcl-xL, and survivin, is transcriptionally regulated by STAT3 (39,43). Consistent with anti-apoptotic role for STAT3, its direct inhibition has been shown to induce apoptosis in prostate cancer cell lines (9). We have also shown previously that DATS treatment decreases protein level of Bcl-2 in PC-3 human prostate cancer cell line and ectopic expression of Bcl-2 confers partial but statistically significant protection against DATS-induced apoptosis in PC-3 cells (31). We therefore questioned if DATS-induced apoptosis was blunted by STAT3 activation. We tested this possibility by determining growth suppressive and pro-apoptotic effects of DATS in the absence or presence of IL-6 (25 ng/mL). As shown in Fig. 4A, 24 hour treatment with DATS inhibited viability of both DU145 and LNCaP cells. Inhibition of cell viability resulting from DATS exposure was not reversed in the presence of IL-6 in either cell line (Fig. 4A). Consistent with these results, IL-6 failed to confer resistance against DATS-induced cytoplasmic histone-associated DNA fragmentation enrichment over DMSO-treated control in both cell lines, except for a marginal protection observed in the LNCaP cells at 20 µmol/L DATS concentration (Fig. 4B). To our surprise, the IL-6 did not increase expression of either Bcl-2 or Bcl-xL mRNA in either cell line (Fig. 4C). We conclude that STAT3 activation resulting from co-treatment with IL-6 is largely dispensable for pro-apoptotic response to DATS in DU145 and LNCaP cells.
Fig. 4.
A, viability of DU145 and LNCaP cells after 24 hour treatment with DMSO (control) or the indicated concentrations of DATS in the absence or presence of 25 ng/mL IL-6. B, cytoplasmic histone-associated DNA fragmentation in DU145 and LNCaP cells after 24 hour treatment with DMSO (control) or the indicated concentrations of DATS in the absence or presence of 25 ng/mL IL-6. In panels A and B, columns, mean (n=3–4); bars, SD. Significantly different (P<0.05) compared with acorresponding DMSO-treated control, and bwithout IL-6 at respective DATS dose (0, 20, and 40 µmol/L) by one-way ANOVA followed by Bonferroni's multiple comparison test. C, expression of Bcl-2 and Bcl-xL mRNA in DU145 and LNCaP cells after 24 hour treatment with DMSO (control) or the indicated concentrations of DATS in the absence or presence of 25 ng/mL IL-6. Numbers on top of the bands represent change in expression relative to corresponding DMSO-treated control.
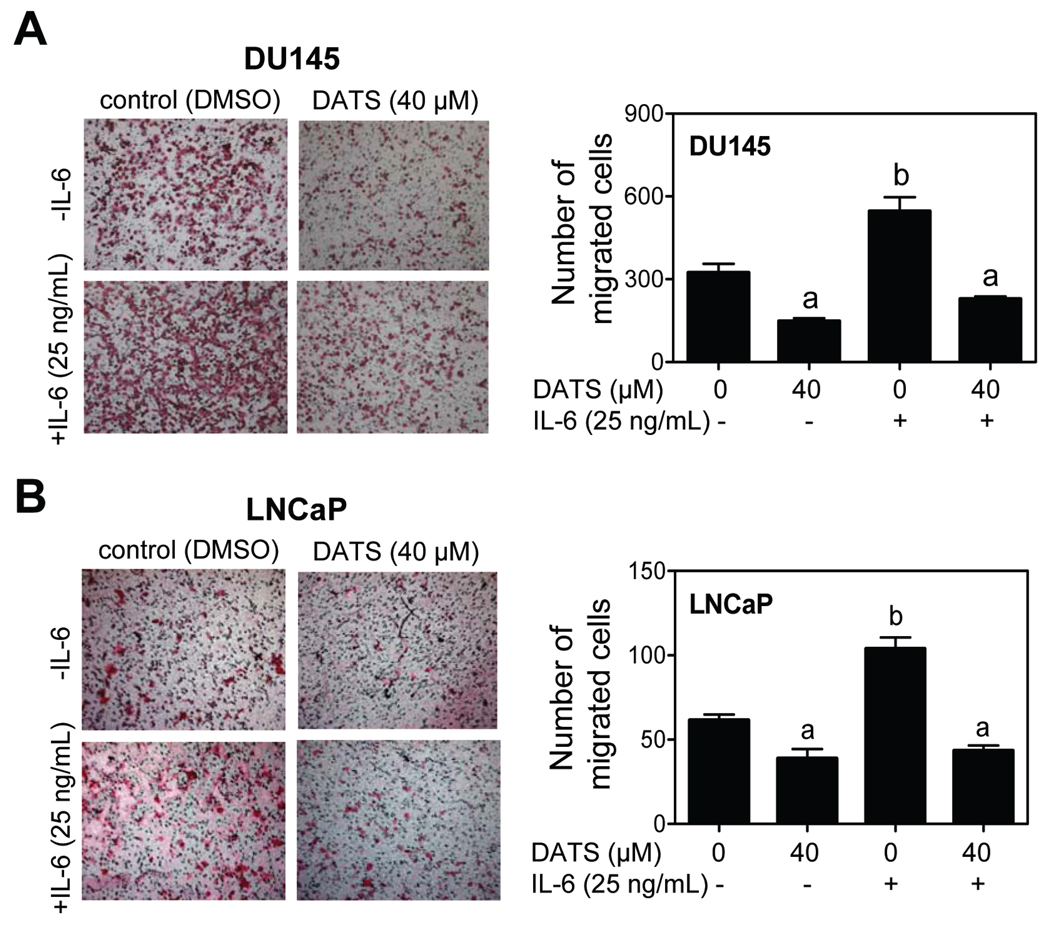
DATS treatment inhibited migration of DU145 and LNCaP cells
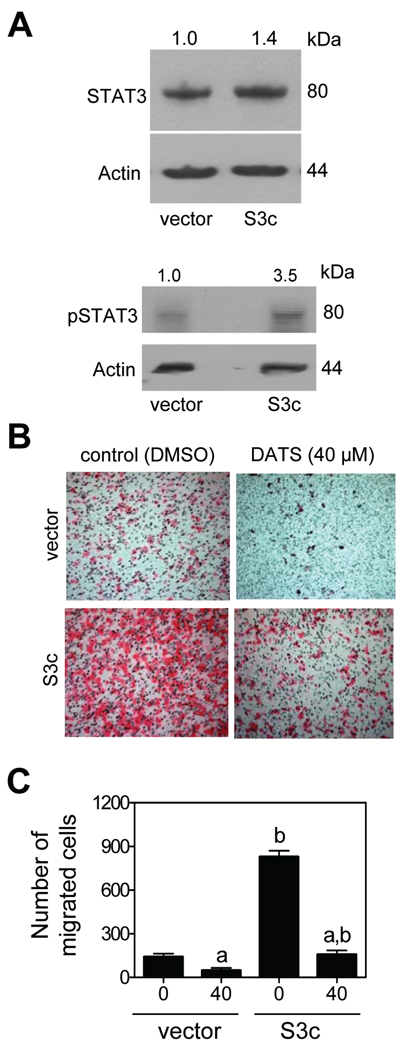
Cell migration and invasion are characteristics of metastatic disease. The STAT3 signaling has been linked to cancer cell invasion and migration (39,43). We therefore determined the effect of DATS treatment on migration of DU145 and LNCaP cells with or without IL-6. Migration by DU145 cells was inhibited significantly in the presence of 40 µmol/L DATS (Fig. 5A). The IL-6 increased migration of DU145 cells by about 1.7-fold compared with DMSO-treated control. The DATS-mediated inhibition of DU145 cell migration was maintained in the presence of IL-6 (Fig. 5A). The DU145 cell line was relatively more migratory compared with LNCaP cells, which may, at least in part, be attributed to status of constitutively active STAT3. The LNCaP cells were also sensitive to IL-6-induced migration similar to the DU145 cell line. Similar to DU145 cells (Fig. 5A), DATS was able to inhibit migration of LNCaP cells regardless of IL-6 treatment (Fig. 5B). These results indicated that ability of DATS to inhibit cell migration was not affected by IL-6-mediated activation of STAT3. We confirmed these results using LNCaP cells stably transfected with constitutively active STAT3 (S3c). As can be seen in Fig. 6A, the level of total STAT3 and pSTAT3 was higher by about 1.4- and 3.5-fold, respectively, in S3c cells compared with empty vector transfected control LNCaP cells. Ectopic expression of pSTAT3 in S3c cells resulted in potentiation of cell migration as expected (Fig. 6B). However, the S3c cell line exhibited only marginal resistance towards DATS-mediated inhibition of cell migration compared with empty vector transfected cells (Fig. 6C).
Fig. 5.
Representative images depicting in vitro migration by (A) DU145 cells and (B) LNCaP cells after 24 hour treatment with DMSO (control) or the indicated concentrations of DATS in the absence or presence of 25 ng/mL IL-6 (×10 objective magnification). Quantitative results are shown in right panels for each cell line. Columns, mean (n=8–10); bars, SD. Significantly different (P<0.05) compared with acorresponding DMSO-treated control, and bwithout IL-6 by one-way ANOVA followed by Bonferroni's multiple comparison test. Experiments were performed twice, and representative data from a single experiment are shown.
Fig. 6.
A, immunoblotting for total STAT3 and pSTAT3 using lysates from LNCaP cells stably transfected with pIRES empty vector (abbreviated as vector) or vector encoding for constitutively active STAT3 (abbreviated as S3c). The blots were stripped and reprobed with anti-actin antibody to normalize for differences in protein level. Numbers on top of the immunoreactive bands represent change in protein levels relative to empty vector transfected cells. B, representative images depicting in vitro migration by vector and S3c LNCaP cells after 24 hour treatment with DMSO (control) or 40 µmol/L DATS. C, quantitation of in vitro migration by vector and S3c LNCaP cells after 24 hour treatment with DMSO (control) or 40 µmol/L DATS. Columns, mean (n=8); bars, SD. Significantly different (P<0.05) compared with acorresponding DMSO-treated control, and bcorresponding empty vector transfected cells (DMSO or DATS) by one-way ANOVA followed by Bonferroni's multiple comparison test. Experiments were done twice, and representative data from a single experiment are shown.
Discussion
The primary objective of the present study was to test whether anticancer responses to DATS, which is a highly promising cancer chemopreventive constituent of processed garlic, are related to inhibition of STAT3. The STAT3 is a valid chemopreventive/therapeutic target for prostate cancer because: (a) elevated STAT3 activation has been observed in a large fraction of human prostate tumors compared with matched adjacent normal prostate tissues (3,6); (b) the STAT3 regulates gene expression of many pro-survival molecules (39,43); (c) inhibition of STAT3 activation triggers apoptotic cell death in human prostate cancer cells (3); and (d) stable expression of constitutively active STAT3 alone has been shown to alter phenotype of benign prostate epithelial cells to resemble malignant cells (5). Moreover, STAT3 is implicated in transition of hormone-sensitive prostate cancer to androgen-independent state (also referred to as “castration-resistant” or “hormone-refractory”) (8,44). The present study reveals that DATS treatment inhibits constitutive as well as IL-6-inducible activation of STAT3, which is not a cell line-specific effect. However, the underlying mechanism for IL-6-induced STAT3 phosphorylation is likely different between DU145 and LNCaP cells. The IL-6 treatment clearly increases phosphorylation of JAK2 in LNCaP cells but not in the DU145 cell line. Activation of STAT3 can also be mediated by other kinases (e.g., Src and Rac1; Ref. 1,2,42,45) and the possibility that such kinases are involved in the activation of STAT3 in DU145 cells can’t be excluded. Noticeably, the DATS-mediated inhibition of STAT3 activation is evident at pharmacologically relevant concentrations based on a rat pharmacokinetic study (46). We also show that the DATS-mediated decrease in STAT3 phosphorylation is not restricted to cultured cells because dorsolateral prostate from DATS-treated mice exhibits reduced Tyr705 phosphorylation of STAT3 (Fig. 3B).
The Tyr705 phosphorylation of STAT3 causes its dimerization (43). The STAT3 dimer translocates to the nucleus for binding to specific DNA sequences in the promoter of target genes (43). We found that DATS-mediated inhibition of STAT3 phosphorylation is accompanied by not only suppression of nuclear translocation of pSTAT3 but also its dimerization. Inhibition of nuclear level of pSTAT3 by DATS treatment is evident at 3 hours and occurs even in IL-6-stimulated cells. Likewise, the DATS-mediated suppression of STAT3 dimerization is observed in cells without (DU145) or with IL-6 treatment (LNCaP) (Fig. 3A).
Another critical goal of the present study was to determine whether activation of STAT3 confers protection against cellular responses to DATS. This was a strong possibility considering expression of many anti-apoptotic genes (e.g., Bcl-2, Bcl-xL, and survivin) and those involved in angiogenesis and metastasis (e.g., MMP2, MMP9, and VEGF) are regulated by STAT3 (39,43). Consistent with anti-apoptotic role of STAT3 activation, antisense inhibition of STAT3 triggers apoptosis in human prostate cancer cells (3). Peptide-mediated inhibition of STAT3 has been shown to sensitize ErbB2-overexpressing breast cancer cells to growth inhibition by Taxol (47). Likewise, blockade of STAT3 activation by treatment with inhibitors of epidermal growth factor receptor and JAK2 or by transfection with a dominant negative STAT3 renders 435B cells more sensitive to chemotherapy-induced apoptosis (48). To our surprise, growth inhibitory or proapoptotic effect of DATS is not significantly impaired by IL-6-mediated activation of STAT3 (present study). The anti-migratory effect of DATS is also either not altered or only modestly blunted by IL-6 stimulation or by forced expression of constitutively active STAT3. These effects are not cell line-specific because similar responses are evident in both DU145 and LNCaP cells. It is interesting to note that STAT5 has been shown to modify effects of STAT3 from the level of gene expression to cellular phenotype (49). Co-activation of STAT5 and STAT3 in breast cancer cells results in decreased cellular proliferation and increased sensitivity to paclitaxel and vinorelbine (49). It is plausible that DATS treatment causes activation of STAT5 to counteract the anti-apoptotic effect of STAT3 activation resulting from the IL-6. Further studies are needed to systematically explore this possibility.
Mechanism for growth suppressive effect of DATS has been studied extensively in prostate cancer cells (31–37). For example, we have shown previously that DATS treatment causes activation of checkpoint kinase 1 (Chk1) in human prostate cancer cells regardless of the androgen responsiveness or the p53 status, and activation of Chk1 is critical for both mitotic arrest and apoptotic cell death (32, 35, 50). Moreover, the Chk1 dependence for DATS-induced cell cycle arrest and apoptosis induction is not unique to the prostate cancer cells because similar effects are seen in a human colon cancer cells line (50). Previous studies have also established that the initial signal for cellular effects of DATS (apoptosis and cell cycle arrest) is derived from generation of reactive oxygen species (31,33), which causes activation of c-Jun N-terminal kinase and extracellular signal-regulated kinase leading to phosphorylation, and hence inactivation of Bcl-2 (31). Suppression of Akt leading to mitochondrial translocation of proapoptotic protein BAD and activation of caspases have also been documented in DATS-treated prostate cancer cells (34). Thus, it is safe to conclude that DATS is capable of targeting multiple signaling pathways to execute cell death.
In summary, the present study demonstrates inhibition of STAT3 activation by DATS in human prostate cancer cells in culture and mouse prostate tumors in vivo. Equally exciting is our finding that DATS can overcome survival advantage imparted by STAT3 activation.
Acknowledgments
We thank Abhai Kumar for technical assistance.
Grant Support: This study was supported by the USPHS grant 2 RO1 CA113363-06 awarded by the National Cancer Institute.
References
- 1.Ihle JN. The Stat family in cytokine signaling. Curr Opin Cell Biol. 2001;13:211–217. doi: 10.1016/s0955-0674(00)00199-x. [DOI] [PubMed] [Google Scholar]
- 2.Levy DE, Darnell JE., Jr Stats: transcriptional control and biological impact. Nat Rev Mol Cell Biol. 2002;3:651–662. doi: 10.1038/nrm909. [DOI] [PubMed] [Google Scholar]
- 3.Mora LB, Buettner R, Seigne J, et al. Constitutive activation of Stat3 in human prostate tumors and cell lines: direct inhibition of Stat3 signaling induces apoptosis of prostate cancer cells. Cancer Res. 2002;62:6659–6666. [PubMed] [Google Scholar]
- 4.Campbell CL, Jiang Z, Savarese DM, Savarese TM. Increased expression of the interleukin-11 receptor and evidence of STAT3 activation in prostate carcinoma. Am J Pathol. 2001;158:25–32. doi: 10.1016/S0002-9440(10)63940-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang HF, Murphy TF, Shu P, Barton AB, Barton BE. Stable expression of constitutively-activated STAT3 in benign prostatic epithelial cells changes their phenotype to that resembling malignant cells. Mol Cancer. 2005;4:2. doi: 10.1186/1476-4598-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhir R, Ni Z, Lou W, DeMiguel F, Grandis JR, Gao AC. Stat3 activation in prostatic carcinomas. Prostate. 2002;51:241–246. doi: 10.1002/pros.10079. [DOI] [PubMed] [Google Scholar]
- 7.Horinaga M, Okita H, Nakashima J, Kanao K, Sakamoto M, Murai M. Clinical and pathologic significance of activation of signal transducer and activator of transcription 3 in prostate cancer. Urology. 2005;66:671–675. doi: 10.1016/j.urology.2005.03.066. [DOI] [PubMed] [Google Scholar]
- 8.Lee SO, Lou W, Hou M, de Miguel F, Gerber L, Gao AC. Interleukin-6 promotes androgen-independent growth in LNCaP human prostate cancer cells. Clin Cancer Res. 2003;9:370–376. [PubMed] [Google Scholar]
- 9.Barton BE, Karras JG, Murphy TF, Barton A, Huang H. Signal transducer and activator of transcription 3 (STAT3) activation in prostate cancer: direct STAT3 inhibition induces apoptosis in prostate cancer lines. Mol Cancer Ther. 2004;3:11–20. [PubMed] [Google Scholar]
- 10.Dauer DJ, Ferraro B, Song L, et al. Stat3 regulates genes common to both wound healing and cancer. Oncogene. 2005;24:3397–3408. doi: 10.1038/sj.onc.1208469. [DOI] [PubMed] [Google Scholar]
- 11.Surh YJ. Cancer chemoprevention with dietary phytochemicals. Nature Rev Cancer. 2003;3:768–780. doi: 10.1038/nrc1189. [DOI] [PubMed] [Google Scholar]
- 12.Newman DJ, Cragg GM, Snader KM. Natural products as sources of new drugs over the period 1981–2002. J Nat Prod. 2003;66:1022–1037. doi: 10.1021/np030096l. [DOI] [PubMed] [Google Scholar]
- 13.Stan SD, Kar S, Stoner GD, Singh SV. Bioactive food components and cancer risk reduction. J Cell Biochem. 2008;104:339–356. doi: 10.1002/jcb.21623. [DOI] [PubMed] [Google Scholar]
- 14.You WC, Blot WJ, Chang YS, et al. Allium vegetables and reduced risk of stomach cancer. J Natl Cancer Inst. 1989;81:162–164. doi: 10.1093/jnci/81.2.162. [DOI] [PubMed] [Google Scholar]
- 15.Fleischauer AT, Poole C, Arab L. Garlic consumption and cancer prevention: meta-analyses of colorectal and stomach cancers. Am J Clin Nutr. 2000;72:1047–1052. doi: 10.1093/ajcn/72.4.1047. [DOI] [PubMed] [Google Scholar]
- 16.Hsing AW, Chokkalingam AP, Gao YT, et al. Allium vegetables and risk of prostate cancer: a population-based study. J Natl Cancer Inst. 2002;94:1648–1651. doi: 10.1093/jnci/94.21.1648. [DOI] [PubMed] [Google Scholar]
- 17.Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer Statistics, 2007. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 18.Rivlin RS. Historical perspective on the use of garlic. J Nutr. 2001;131:951S–954S. doi: 10.1093/jn/131.3.951S. [DOI] [PubMed] [Google Scholar]
- 19.Block E. The organosulfur chemistry of the genus Allium- implications for the organic chemistry of sulfur. Angew Chem Int Ed Engl. 1992;31:1135–1178. [Google Scholar]
- 20.Herman-Antosiewicz A, Powolny AA, Singh SV. Molecular targets of cancer chemoprevention by garlic-derived organosulfides. Acta Pharmacol Sin. 2007;28:1355–1364. doi: 10.1111/j.1745-7254.2007.00682.x. [DOI] [PubMed] [Google Scholar]
- 21.Powolny AA, Singh SV. Multitargeted prevention and therapy of cancer by diallyl trisulfide and related Allium vegetable-derived organosulfur compounds. Cancer Lett. 2008;269:305–314. doi: 10.1016/j.canlet.2008.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sparnins VL, Barany G, Wattenberg LW. Effects of organosulfur compounds from garlic and onions on benzo[a]pyrene-induced neoplasia and glutathione S-transferase activity in the mouse. Carcinogenesis. 1988;9:131–134. doi: 10.1093/carcin/9.1.131. [DOI] [PubMed] [Google Scholar]
- 23.Wargovich MJ, Woods C, Eng VWS, Stephens LC, Gray K. Chemoprevention of N-nitrosomethylbenzylamine-induced esophageal cancer in rats by the naturally occurring thioether, diallyl sulfide. Cancer Res. 1988;48:6872–6875. [PubMed] [Google Scholar]
- 24.Dwivedi C, Rohlfs S, Jarvis D, Engineer FN. Chemoprevention of chemically induced skin tumor development by diallyl sulfide and diallyl disulfide. Pharm Res. 1992;9:1668–1670. doi: 10.1023/a:1015845315500. [DOI] [PubMed] [Google Scholar]
- 25.Reddy BS, Rao CV, Rivenson A, Kelloff G. Chemoprevention of colon carcinogenesis by organosulfur compounds. Cancer Res. 1993;53:3493–3498. [PubMed] [Google Scholar]
- 26.Brady JF, Ishizaki H, Fukuto JM, et al. Inhibition of cytochrome P-450 2E1 by diallyl sulfide and its metabolites. Chem Res Toxicol. 1991;4:642–647. doi: 10.1021/tx00024a008. [DOI] [PubMed] [Google Scholar]
- 27.Hu X, Benson PJ, Srivastava SK, et al. Glutathione S-transferases of female A/J mouse liver and forestomach and their differential induction by anti-carcinogenic organosulfides from garlic. Arch Biochem Biophys. 1996;336:199–214. doi: 10.1006/abbi.1996.0550. [DOI] [PubMed] [Google Scholar]
- 28.Chen C, Pung D, Leong V, et al. Induction of detoxifying enzymes by garlic organosulfur compounds through transcription factor NRF2: effect of chemical structure and stress signals. Free Radical Biol Med. 2004;37:1578–1590. doi: 10.1016/j.freeradbiomed.2004.07.021. [DOI] [PubMed] [Google Scholar]
- 29.Xiao D, Lew KL, Kim YA, et al. Diallyl trisulfide suppresses growth of PC-3 human prostate cancer xenograft in vivo in association with Bax and Bak induction. Clin Cancer Res. 2006;12:6836–6843. doi: 10.1158/1078-0432.CCR-06-1273. [DOI] [PubMed] [Google Scholar]
- 30.Singh SV, Powolny AA, Stan SD, et al. Garlic constituent diallyl trisulfide prevents development of poorly differentiated prostate cancer and pulmonary metastasis multiplicity in TRAMP mice. Cancer Res. 2008;68:9503–9511. doi: 10.1158/0008-5472.CAN-08-1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xiao D, Choi S, Johnson DE, et al. Diallyl trisulfide-induced apoptosis in human prostate cancer cells involves c-Jun N-terminal kinase and extracellular-signal regulated kinase-mediated phosphorylation of Bcl-2. Oncogene. 2004;23:5594–5606. doi: 10.1038/sj.onc.1207747. [DOI] [PubMed] [Google Scholar]
- 32.Herman-Antosiewicz A, Singh SV. Checkpoint kinase 1 regulates diallyl trisulfide-induced mitotic arrest in human prostate cancer cells. J Biol Chem. 2005;280:28519–28528. doi: 10.1074/jbc.M501443200. [DOI] [PubMed] [Google Scholar]
- 33.Xiao D, Herman-Antosiewicz A, Antosiewicz J, et al. Diallyl trisulfide-induced G2-M phase cell cycle arrest in human prostate cancer cells is caused by reactive oxygen species-dependent destruction and hyperphosphorylation of Cdc25C. Oncogene. 2005;24:6256–6268. doi: 10.1038/sj.onc.1208759. [DOI] [PubMed] [Google Scholar]
- 34.Xiao D, Singh SV. Diallyl trisulfide, a constituent of processed garlic, inactivates Akt to trigger mitochondrial translocation of BAD and caspase-mediated apoptosis in human prostate cancer cells. Carcinogenesis. 2006;27:533–540. doi: 10.1093/carcin/bgi228. [DOI] [PubMed] [Google Scholar]
- 35.Herman-Antosiewicz A, Stan SD, Hahm E-R, Xiao D, Singh SV. Activation of a novel ataxia-telangiectasia mutated and Rad3 related/checkpoint kinase 1-dependent prometaphase checkpoint in cancer cells by diallyl trisulfide, a promising cancer chemopreventive constituent of processed garlic. Mol Cancer Ther. 2007;6:1249–1261. doi: 10.1158/1535-7163.MCT-06-0477. [DOI] [PubMed] [Google Scholar]
- 36.Kim YA, Xiao D, Xiao H, et al. Mitochondria-mediated apoptosis by diallyl trisulfide in human prostate cancer cells is associated with generation of reactive oxygen species and regulated by Bax/Bak. Mol Cancer Ther. 2007;6:1599–1609. doi: 10.1158/1535-7163.MCT-06-0754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stan SD, Singh SV. Transcriptional repression and inhibition of nuclear translocation of androgen receptor by diallyl trisulfide in human prostate cancer cells. Clin Cancer Res. 2009;15:4895–4903. doi: 10.1158/1078-0432.CCR-09-0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Xiao D, Li M, Herman-Antosiewicz A, et al. Diallyl trisulfide inhibits angiogenic features of human umbilical vein endothelial cells by causing Akt inactivation and down-regulation of VEGF and VEGF-R2. Nutr Cancer. 2006;55:94–107. doi: 10.1207/s15327914nc5501_12. [DOI] [PubMed] [Google Scholar]
- 39.Yu H, Kortylewski M, Pardoll D. Crosstalk between cancer and immune cells: role of STAT3 in the tumor microenvironment. Nat Rev Immunol. 2007;7:41–51. doi: 10.1038/nri1995. [DOI] [PubMed] [Google Scholar]
- 40.Xiao D, Srivastava SK, Lew KL, et al. Allyl isothiocyanate, a constituent of cruciferous vegetables, inhibits proliferation of human prostate cancer cells by causing G2/M arrest and inducing apoptosis. Carcinogenesis. 2003;24:891–897. doi: 10.1093/carcin/bgg023. [DOI] [PubMed] [Google Scholar]
- 41.Shin DS, Kim HN, Shin KD, et al. Cryptotanshinone inhibits constitutive signal transducer and activator of transcription 3 function through blocking the dimerization in DU145 prostate cancer cells. Cancer Res. 2009;69:193–202. doi: 10.1158/0008-5472.CAN-08-2575. [DOI] [PubMed] [Google Scholar]
- 42.Heinrich PC, Behrmann I, Müller-Newen G, Schaper F, Graeve L. Interleukin-6-type cytokine signalling through the gp130/Jak/STAT pathway. Biochem J. 1998;334:297–314. doi: 10.1042/bj3340297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Darnell JE., Jr STATs and gene regulation. Science. 1997;277:1630–1635. doi: 10.1126/science.277.5332.1630. [DOI] [PubMed] [Google Scholar]
- 44.Tam L, McGlynn LM, Traynor P, Mukherjee R, Bartlett JM, Edwards J. Expression levels of the JAK/STAT pathway in the transition from hormone-sensitive to hormone-refractory prostate cancer. Br J Cancer. 2007;97:378–383. doi: 10.1038/sj.bjc.6603871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yu CI, Meyer DJ, Campbell GS, et al. Enhanced DNA binding activity of a Stat3-related protein in cells transformed by the Src oncoprotein. Science. 1995;269:81–83. doi: 10.1126/science.7541555. [DOI] [PubMed] [Google Scholar]
- 46.Sun X, Guo T, He J, et al. Simultaneous determination of diallyl trisulfide and diallyl disulfide in rat blood by gas chromatography with electron-capture detection. Pharmazie. 2006;61:985–988. [PubMed] [Google Scholar]
- 47.Hawthorne VS, Huang WC, Neal CL, Tseng LM, Hung MC, Yu D. ErbB2-mediated Src and signal transducer and activator of transcription 3 activation leads to transcriptional up-regulation of p21Cip1 and chemoresistance in breast cancer cells. Mol Cancer Res. 2009;7:592–600. doi: 10.1158/1541-7786.MCR-08-0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lou W, Ni Z, Dyer K, Tweardy DJ, Gao AC. Interleukin-6 induces prostate cancer cell growth accompanied by activation of STAT3 signaling pathway. Prostate. 2000;42:239–242. doi: 10.1002/(sici)1097-0045(20000215)42:3<239::aid-pros10>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 49.Walker SR, Nelson EA, Zou L, et al. Reciprocal effects of STAT5 and STAT3 in breast cancer. Mol Cancer Res. 2009;7:966–976. doi: 10.1158/1541-7786.MCR-08-0238. [DOI] [PubMed] [Google Scholar]
- 50.Xiao D, Zeng Y, Singh SV. Diallyl trisulfide-induced apoptosis in human cancer cells is linked to checkpoint kinase 1-mediated mitotic arrest. Mol Carcin. 2009;48:1018–1029. doi: 10.1002/mc.20553. [DOI] [PMC free article] [PubMed] [Google Scholar]