Abstract
Background/Methods
The purpose of this review was to assess the current evidence supporting operative fixation versus casting for acute scaphoid fractures through a systematic review and meta-analysis of the literature.
Results
Our search yielded 59 articles that met our inclusion criteria with five studies achieving high, 22 moderate, and 32 low Structured Effectiveness Quality Evaluation Scale scores. Pooled results of the four Sackett level 1 evidence studies showed no significant difference between the operative (114/115, 99%) versus non-operative group (106/112, 95%) (p = 0.07) when the definition of nonunion was based on more definitive criterion versus plain radiographs that may be insufficient to assess bony union. Similar results were found for the Sackett level 2 and 4 articles.
Conclusions
This systematic review reveals that significant weaknesses exist in the literature with respect to the level of evidence and quality of published studies on this topic. Currently, there is insufficient evidence to support the most effective treatment for acute scaphoid fractures.
Keywords: Acute scaphoid fractures, Systematic review, Treatment scaphoid fractures
Introduction
Fractures of the scaphoid account for over 60% of carpal bone fractures and 11% of all hand fractures [27]. Casting with thumb immobilization has historically been the primary method of treatment. In recent years, there has been a movement away from non-operative management for these fractures. For example, Bond et al. (2006) highlight that joint stiffness may arise due to prolonged casting that may be avoidable with surgical intervention [4]. In particular, refinement of percutaneous fixation methods has increased the enthusiasm for operative intervention.
The evidence favoring early operative management of acute scaphoid fractures resides in a number of small studies of variable quality. Since nonunion rates are low, such underpowered studies do not provide conclusive evidence. The purpose of this paper was to further summarize the evidence supporting the management of acute scaphoid fractures by conducting a systematic review and meta-analysis of published literature.
Materials and Methods
Given the expectation of an insufficient number of studies, we adopted a broad search strategy using the keyword scaphoid and the databases PubMed and OVID Embase. Two independent evaluators reviewed all English language articles published between January 1988 and December 2008.
Studies were selected for data extraction and critical appraisal if they reported on acute isolated fractures, if they contained observations on healing, and if they were Sackett level of evidence 1 to 4. Specific exclusion criteria were as follows: Sackett level 5 evidence studies, including expert opinion, cadaveric, biomechanical, individual case studies, review, technical, and epidemiology papers; clinical scaphoid fractures; stress fractures; acute scaphoid fractures with concurrent wrist or hand fractures affecting management of the scaphoid fracture; secondary treatments including revision cases for acute scaphoid fractures; and skeletally immature subjects (Table 1).
Table 1.
Inclusion and exclusion criteria for article selection.
| Papers were selected for our final review if they met the following criteria: |
| 1. Type of study: Sackett levels 1–4; |
| — randomized control trials, prospective trials, retrospective trials, and case series |
| 2. Type of fracture: isolated acute scaphoid fractures; |
| 3. Type of treatment: primary treatment; |
| 4. Date of articles: articles published between 1988 and 2008; |
| 5. Type of patient: skeletally mature. |
| Papers were excluded for our final review if they met any of the following criteria: |
| 1. Type of study: Sackett level 5 (expert opinion, biomechanical, and individual case studies) and review, technical, and epidemiology papers; |
| 2. Type of fracture: clinical scaphoid fractures, nonunions, malunions, stress fractures, acute scaphoid fractures with concurrent wrist or hand fractures affecting management of the scaphoid fracture; |
| 3. Type of treatment: secondary treatment including revision cases for acute scaphoid fractures; |
| 4. Type of article: non-English articles; |
| 5. Type of patient: skeletally immature. |
In total, 1,566 English language articles were identified through the bibliographic literature search. Two raters independently reviewed the titles and abstracts to identify studies meeting the inclusion/exclusion criteria. Based on the title and abstract, 1,416 were excluded. The full text of the remaining 150 was subsequently reviewed. Based on the inclusion and exclusion criteria above, an additional 91 were excluded. This left 59 articles remaining for evaluation and inclusion into our systematic review. Articles with combined data for the treatment of nonunions and acute scaphoid fractures were only used if the data for acute fractures could be delineated and examined separately from the data for nonunions.
Two independent evaluators then assessed the selected papers using a standardized critical appraisal form and process previously described [26, 37]. The level of evidence of each study was also graded (1 to 4) based on the Sackett level of evidence scale [37]. The structured appraisal was performed using the Structured Effectiveness Quality Evaluation Scale (SEQES) validated in previous work, as seen in Table 2 [26, 37]. The SEQES score rates the quality of the article methodology through examination of seven general categories: study question, study design, subjects, intervention, outcomes, analysis, and recommendations. Each category has several criteria and each criterion was scored 0, 1, or 2. A score of 0 meant the criterion was not met at all, 1 meant the criterion was partially met, and 2 meant the criterion was fully met according to the published SEQES guidelines. Using the SEQES scores, high-, moderate-, and low-quality levels were assigned. High-quality studies had SEQES scores between 33 to 48. Moderate-quality studies had SEQES scores between 17 to 32, and low-quality studies had scores ≤16. Each article was independently scored using the SEQES checklist. The results were then compared, any discrepancies were discussed, and the scores were re-evaluated assigning a final consensus score for each paper. The consensus scores were used for the final evaluation.
Table 2.
Structured effectiveness quality evaluation scale (SEQES) criteria.
| Study question: |
| 1. Was relevant background work cited to establish a foundation for the research questions? |
| Study design: |
| 2. Was a comparison group used? |
| 3. Was patient status at more than one time point considered? |
| 4. Was data collection performed prospectively? |
| 5. Were patients randomized to groups? |
| 6. Were patients blinded to the extent possible? |
| 7. Were treatment providers randomized to the extent possible? |
| 8. Was an independent evaluator used to administer the outcome measures? |
| Subjects: |
| 9. Did sampling procedures minimize sample/selection biases? |
| 10. Were inclusion/exclusion criteria defined? |
| 11. Was an appropriate enrollment obtained? |
| 12. Was appropriate retention/follow-up obtained? |
| Intervention: |
| 13. Was the intervention applied according to established principles? |
| 14. Were biases due to the treatment provider minimized? |
| 15. Was the intervention compared to the appropriate comparator? |
| Outcomes: |
| 16. Was an appropriate primary outcome defined? |
| 17. Was an appropriate secondary outcomes considered? |
| 18. Was an appropriate follow-up period incorporated? |
| Analysis: |
| 19. Was an appropriate statistical test(s) performed to indicate differences related to the intervention? |
| 20. Was it established that the study had significant power to identify treatment effects? |
| 21. Was the size and significance of the effects reported? |
| 22. Were missing data accounted for and considered in interpreting results? |
| 23. Were clinical and practical significance considered in interpreting results? |
| Recommendations: |
| 24. Were the conclusions/clinical recommendations supported by the study objectives, analysis, and results? |
| Scoring methodology: |
| 0—criterion was not met |
| 1—criterion was partially met |
| 2—criterion was fully met |
| Total quality score: |
| Low (0 to 16) |
| Moderate (17 to 32) |
| High (33 to 48 points) |
The Sackett level of evidence score was used to categorize the papers [37]. The data within each level of evidence was pooled for analysis to examine the effect of study quality. Due to the wide variation of treatment methods used, patients were classified into two broad treatment categories, operative versus non-operative treatment. This pooled data then provided a sufficient sample size to allow a meta-analysis to be performed. A meta-analysis was performed by deconstructing union rates reported in individual studies and pooling the cases for analysis. This approach was not possible for other measures as the outcome measurements were inconsistently reported among the various papers, patient populations differed and confounding factors prohibited comparison.
Data extraction was performed by two raters using a standardized form. The following data were extracted from each article: sample size, type of intervention used, complications, percentage union, percentage nonunion, and number of weeks to union. These variables were chosen because they were the most consistently reported variables in the majority of the articles chosen for our review. Unfortunately, data such as patient reported disability measures, pain scales such as the visual analogue scale, grip strength, range of motion, time to return to work, and indirect or direct economic loss secondary to scaphoid fractures were not collected as they were inconsistently reported by the various articles.
Statistical Methods
A Chi square and Fisher's exact test were used to compare the proportion of unions and nonunions in each group.
Results
Fifty-nine publications met the inclusion and exclusion criteria of this systematic review. Only six articles were considered level 1 evidence [1, 4, 13, 14, 58, 59], four were level 2 evidence [20, 25, 34, 46], and the remainder were level 4 evidence articles [2, 3, 5–12, 15–19, 21–24, 28–33, 35, 36, 38–45, 47–53, 54–57, 60, 61, 63].
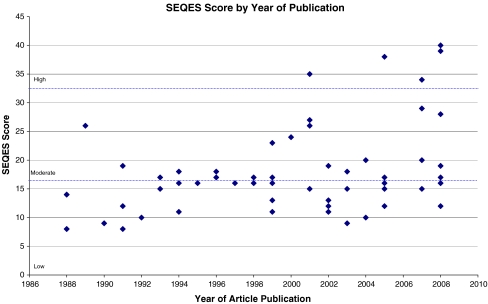
Overall, the majority of studies in the literature were of poor quality. Using the SEQES scores, high-, moderate-, and low-quality levels were assigned. Only five articles (9% of all articles) [4, 13, 14, 58, 59] achieved high-quality scores, 22 (37% of all articles) [1–3, 7, 8, 11, 15, 18–20, 24, 25, 34, 35, 39, 41–43, 46, 51, 56, 63] were ranked moderate, and 32 (54% of all articles) were low-quality articles [5, 6, 9, 10, 12, 16, 17, 21–23, 28–33, 36, 38, 40, 44, 45, 47–50, 52, 53, 54, 55, 57, 60, 61] according to their SEQES score. The mean SEQES score was 18 (7.0) (37% of the maximum score). Scores ranged from 8 (17% of the maximum) [36] to 40 (83% of the maximum) [59], with none reaching the maximal score of 48 (Fig. 1).
Figure 1.
Progression of SEQES scores 1988–2008.
Inconsistencies in the reporting of patients' age, hand dominance, occupation, medical comorbidities, smoking habits, and specific fracture patterns limited the collection of patient demographics. When the mechanism of injury was reported, a fall on the outstretched hand was the most frequently cited reason for the patients' fracture. As expected, the patient population for scaphoid fractures was predominantly male (80%, n = 1782). There were 244 (56%) women treated nonsurgically and 190 (44%) operatively while 945 (53%) men were treated nonsurgically and 837 (47%) operatively.
Summary of Level 1 Evidence
The literature search yielded only six randomized control trials [1, 4, 13, 14, 58, 59], two of which reported on the same subset of patients [13, 14, 58, 59], essentially yielding four studies. These four studies were deemed by both scorers to be Sackett level of evidence 1b. Bond et al., Dias et al., and Vinnars et al. were found to have high SEQES scores while Adolfsson et al. was ranked as moderate quality.
All patients undergoing non-operative treatment [short-arm thumb-spica casting (n = 52) [1, 58, 59], long-arm thumb-spica casting (n = 14) [4], and short-arm Colles casting (n = 42) [13, 14] were combined into a single group to allow meta-analysis. Of the 128 individuals in the non-operative group, 20 were excluded from final analyses by their respective authors generally secondary to loss to follow-up. Patients (115) treated with surgical fixation [percutaneous insertion of Acutrak screw (n = 36) [1, 4] or open reduction with a Herbert screw (n = 79) [13, 14, 58, 59] were also combined into a single group to allow meta-analysis.
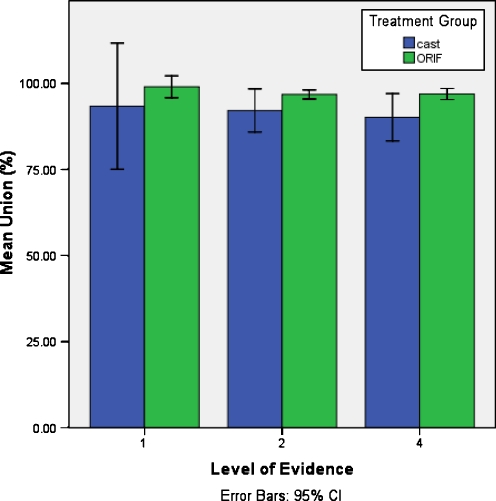
An analysis of the pooled data demonstrated that the percent of patients achieving union was significantly higher in the operative group [114/115, 99% (0.02%)] than the non-operative group [106/117, 91% (0.12%)], (p = 0.005) (Fig. 2). However, closer analysis of the data reported by Dias et al. revealed that five of the nonunions in the non-operative group did not represent true nonunions. One of the cases classified as a nonunion was reported to have healed without further intervention, and four were not found to have any evidence of mobility intra-operatively and “the fracture could not be easily identified” [13]. Since it was not clear whether these cases represented “true nonunions”, a second analysis was performed excluding these five cases. Interestingly, exclusion of these five cases eliminated any significant difference previously seen between the two groups (union rates, 99% operative group versus 95% non-operative group, p = 0.07).
Figure 2.
Percent of patients achieving union with operative versus non-operative management (based on weighted means).
A meta-analysis for time to union could not be performed as this was only reported in two articles. Bond et al. was the only study to report significance with respect to average time to union. In their non-operative group, average time to union was 12 (0.7) weeks and 7 (0.5) weeks in the operative group (p = 0.0003, n = 25). Conversely, Adolfsson et al. found no significance in healing time or rate between the two treatment arms. Vinnars et al. failed to report time to union while Dias et al. stated that union had occurred by 12 weeks for both arms of their study, making statistical analyses for this endpoint difficult.
There were no reported complications with casting. However, one case of reflex sympathetic dystrophy [1], seven implant-related issues [4], and ten problematic scars [13] were reported for the operative group. Long-term follow-up on a subset of these patients [14] revealed radiographic evidence of osteoarthritis in the scaphotrapezial (8/59) and radioscaphoid (6/59) joints, with no significant difference between those treated operatively and non-operatively.
The recommendations for the initial management of acute scaphoid fractures made by the four studies were variable. Two studies advocated percutaneous screw fixation, one study recommended conservative management, and one study did not identify any substantial differences between treatment modalities. Our pooled results indicate that a higher percentage of patients achieved union with surgery; however, this was dependant on the author's definition of union. Unfortunately, fracture union was not rigorously defined, and in many studies, plain radiographs were used for determining union rather than more sensitive modalities such as computed tomography which may have influenced results. Our pooled results are based on a small number of articles, variable interventions within each intervention type, plain radiography to determine union, and no consideration of the impact of complications on the determination of the “best” initial management for scaphoid fractures.
Summary of Level 2 Evidence
Four low quality, randomized control trials met the requirements for Sackett level of evidence 2b [20, 25, 34, 46]. None achieved 2a status as none of the authors conducted a systematic review of homogenous cohort studies. McQueen et al. and Saeden et al. compared operative and non-operative management while Gellman et al. and Hambidge et al. compared various casting methods. All four articles had moderate SEQES scores.
Patient data were pooled to identify 302 patients (of whom 70 were eventually excluded from final statistical analyses) who were treated in short arm Colles (n = 151) [25, 34], short-arm thumb-spica or long-arm thumb-spica casting (n = 81) [20]. Meanwhile, the operative group of McQueen et al. and Saeden et al. enrolled and retained 62 patients. Saeden et al. reported on 32 fractures which underwent open reduction and internal fixation using the volar approach and Herbert screw while McQueen et al. performed percutaneous screw fixation with the Acutrak screw in the remaining 30 fractures. No statistical difference was observed between the two management arms for percent of patients achieving union [ORIF [60/62, 97% (0.001%)] versus casting [211/232, 91% (0.05%), p = 0.13]] (Fig. 2).
Again, we could not perform a meta-analysis for time to union due to the limitations of data reporting. Saeden et al. and Hambidge et al. did not report time to union while Gellman et al. reported only the average time to union for long- or short-arm thumb-spica casting. They concluded that fractures of the proximal and middle thirds had a significantly shorter time to union when treated with long-arm thumb-spica casting (p < 0.05), but no significance was found for distal third fractures. McQueen et al. did find improved time to union for percutaneous screw fixation over short-arm casting (9 weeks versus 14 weeks, p < 0.001), but their numbers were based on a small patient population (n = 60) treated at two trauma centers by various surgeons.
For the casted group, complications included persistent pain of various intensities [21, 25], avascular necrosis (9) [20, 34], radiocarpal and scaphotrapezial osteoarthritis (5) [34, 46], and complex regional pain syndrome (1) [34]. In the operative treatment group, intraoperative screw breakage (2) [34], a proud screw requiring removal after the index procedure (1) [34], and radiocarpal and scaphotrapezial osteoarthritis (5) [46] were reported. Saeden et al. noted that radiographic signs of arthritis were more common in patients treated surgically compared to casting (p = 0.049); however, all patients were asymptomatic at the time of assessment [46].
Final conclusions from these authors were disparate. Saeden et al. and McQueen et al. concluded that operative management was superior to non-operative management with regard to return to activity and found a relatively low complication rate. Conversely, Gellman et al. and Hambidge et al. advocated casting as appropriate initial management for acute scaphoid fractures. However, the basis of the authors' recommendations is limited as the study designs were flawed with small patient populations and inadequate use of control groups.
Summary of Level 4 Evidence
Forty-nine papers met the criteria for level 4 evidence [2, 3, 5–12, 15–19, 21–23, 28–33, 35–45, 47–53, 54–57, 60, 61, 63]. In total, 1,416 patients, of which 278 were excluded, were treated with casting [2, 11, 16, 17, 19, 28, 30, 33, 39–41, 45, 48, 53, 54, 60], and 1,247 patients, of which 124 were excluded, were treated with surgery [2, 3, 5–10, 12, 15, 16, 18, 21, 23, 24, 28, 29, 31, 32, 35, 38, 39, 41–44, 47, 49–51, 55–57, 61, 63]. In these groups, all methods of non-operative and operative management previously mentioned were used. Nineteen had moderate SEQES scores while the remainder had low scores [5, 6, 9, 10, 12, 16, 17, 21–23, 28–33, 36, 38, 40, 44, 45, 47–49, 51–53, 54, 55, 57, 60, 61].
The percent of patients achieving union in the case series reporting on operatively treated scaphoid fractures [1,074/1,122, 96% (0.14%)] was significantly higher than for those treated with casting [1,025/1,138, 90% (0.05%), (p < 0.001)] (Fig. 2). The difference in time to union for cast treatment and operative management did not demonstrate statistical significance [12 (1.9) weeks and 10 (3.2) weeks (p = 0.4)]. Further analyses did not reveal any significance within different casting or surgical subtypes.
The most common complications for the casted individuals were carpal osteoarthritis [40, 17, 33, 40] and pain [27, 19, 28, 45]. Only one malunion was reported for this group of articles [53]. Five articles (33% of the total) did not document adverse treatment outcomes, or they could not be extracted from the paper [11, 16, 30, 39, 48].
Intra-operative and post-operative hardware issues [20, 5, 6, 21, 55, 56, 61, 63] as well as pain [17, 5, 28, 56] were the most frequently cited complications in the surgical group. Wound infections (eight) [2, 8, 12, 21, 61], radial nerve dysesthesia (five) [23, 24, 61], Sudeck's atrophy (two) [61], carpal osteoarthritis (two) [56], reflex sympathetic dystrophy (two) [2], distal radial ulnar joint instability (one) [10], avascular necrosis (one) [56], recurrent carpal tunnel syndrome (one) [10], and post-operative proximal scaphoid pole fracture (one) [6] were other much less frequently cited complications. For surgically treated patients, six articles (27% of the total) either did not document adverse treatment outcomes, or this data could not be delineated from the paper [15, 16, 18, 39, 42, 52].
Due to the large number of papers, the casting protocols, surgical approaches, fixation devices, and post-operative care were highly variable. Recommendations garnered from the studies were also variable. Most reports concluded that operative management allowed an earlier return to activity with less cost to society and minimal complications but did not provide conclusive data to support this. Care should be exercised when drawing conclusions from case series and low-quality cohort studies.
Discussion
Acute scaphoid fractures remain a challenging area of hand surgery. While one of the more common hand fractures, the overall incidence, and in particular, nonunion incidence, is insufficient for most single centers to produce fully powered trials. Thus, the most appropriate treatment modality remains poorly supported by the current clinical research. Our systematic review used a simplistic meta-analysis by which to improve the stability in estimates of union rates by pooling data regarding acute scaphoid fractures treated over the past 20 years.
Our systematic review uncovered many concerns with respect to the current literature regarding acute scaphoid fractures. Therefore, it is difficult to report treatment recommendations with adequate evidence-based support. Although our search criteria included all English language reports published in the past 20 years, only 59 articles met our inclusion and exclusion criteria for examination of acute scaphoid fracture management. Of these articles, only six qualified as level 1 evidence [1, 4, 13, 14, 58, 59], and the vast majority were case series and level 4 evidence articles. Consequently, there is little high-quality literature upon which clinical recommendations can be based. In addition, the quality of these papers was found to be poor based on the SEQES scores. Only 5 of 59 articles achieved high-quality scores (6–8) [4, 13, 14, 58, 59] and the majority of all reviewed articles were of low quality (32/59, 54%) [5, 6, 9, 10, 12, 16, 17, 21, 22, 24, 28–33, 36, 38, 40, 44, 45, 47–50, 52, 53, 54, 55, 57, 60, 61].
A key flaw in the current studies is the lack of a clear or consistent definition of union. Consequently, the comparability of union rates across studies is questionable. Dias et al. used plain radiographs as the primary modality to determine union and only if a gap was seen at 16 weeks would computed tomography be used. The lack of serial computed tomography to follow union may account for the fact that five cases classified as “nonunions” went on to demonstrate signs of healing. Serial CT scans may have classified these cases as delayed unions and not as failures of cast treatment. The importance of computed tomography for baseline fracture classification is also imperative as displaced fractures have a higher nonunion rate. In papers such as McQueen et al. and Dias et al., both displaced and undisplaced fractures were combined together, possibly confounding the final results.
The most clinically relevant method for examining the literature would be to base discussions of appropriate interventions on the fracture pattern. However, attempts to do so were unsuccessful since some articles failed to report the fracture pattern. Consequently, the level of evidence was used to separate papers for the formulation of conclusions.
The pooled results of the level 1 articles showed a significantly higher percentage of patients achieving union with operative management versus non-operative management [1, 4, 13, 14, 58, 59]. However, this was based on only six articles (n = 232) with variable interventions within each treatment group. When the definition of union was closely scrutinized, five questionable cases of nonunion were excluded from the analysis [13]. The exclusion of only five cases eliminated any significant difference between the two groups (union rates, 99% operative group versus 94% non-operative group, p = 0.07). With as little as five cases having a significant effect on the final results, we can conclude that the current literature is underpowered and cannot be used to provide any definitive conclusions.
The results for time to union could not be pooled as insufficient reporting hampered data analysis. Consensus was not reached among the four studies, and final conclusions for time to union of the level 1 articles should be interpreted cautiously when making evidence-based treatment decisions.
The pooled results of the four level 2 articles showed no statistical significance between operative and non-operative management arms with respect to percent of patients achieving union [20, 25, 34, 46]. Of the four articles, McQueen et al. were the only authors to find statistical significance for time to union in favor of operative management, but their results were based on small patient numbers with various surgeons performing the operative intervention [34]. In addition, union was determined without the use of computed tomography and the authors' pooled undisplaced and displaced fractures, which may have influenced their results. Another concern was that their article only scored a moderate level of quality according to their SEQES score.
The meta-analysis of the 49 level 4 articles [2, 3, 5–12, 15–19, 21–23, 28–33, 35–45, 47–53, 54–57, 60, 61, 63] provides weak evidence as it is based on case series with moderate to low SEQES scores. In addition, pooling the data were extremely difficult as the data reporting of data among these papers was very poor. Recommendations from these papers cannot be established since comparison or control groups were not used.
Consensus regarding the optimal treatment modality for an acute scaphoid fracture could not be reached based on our review of the literature. The recent trend suggesting that operative management is preferable is not adequately supported by literature. In fact, operative management can be associated with post-operative complications making it less desirable than casting with certain patient populations.
Our findings are consistent with another recently published systematic review and meta-analysis [62]. The authors utilized stricter inclusion criteria to examine only randomized and quasi-randomized trials. In total, they examined seven articles that were also included in our study. Their final conclusions echo our own conclusions that operative management of acute nondisplaced or minimally displaced fractures has not yet been proven to be superior to cast management. Furthermore, they highlighted that operative intervention was associated with complications such as scaphotrapezial osteoarthritis making surgical intervention less appealing.
The conclusions of our study are limited by the fact that a complete meta-analysis was not possible. Although we performed a meta-analysis on some variables, the inconsistency of reported data made pooling of our data impossible at times. Moreover, the lack of patient homogeneity and the presence of confounding factors limited our ability to perform meta-analyses on the entire group. The inability to differentiate treatment options based on the fracture pattern also limited our study.
Bias in the assignment of quality scores is another possible limitation of this study. We attempted to minimize potential bias with the use of pre-determined inclusion and exclusion criteria, standard evaluation forms, two reviewers, and a blinded statistician.
The applicability of our conclusions is also limited by the fact that the only outcome measures used were the percent of patients achieving union and time to union. Other clinically relevant outcomes such as grip strength, range of motion, pain, return to work, and patient satisfaction were not examined as they were inconsistently reported.
This systematic review indicates that there is currently insufficient evidence to make definitive conclusions on the indications for, or effectiveness of operative versus non-operative management of acute scaphoid fractures. Future studies should include the use of a large multi-center randomized trial to overcome the limitations of small patient populations currently present in the literature. As well, computed tomography should be used in replacement of plain radiographs to more reliably define fracture patterns and union progression. The general paucity of literature on this important topic should be further clarified through these studies so that the most appropriate treatment for acute scaphoid fractures can be delineated.
Conflict of Interest
The authors declare that they have no conflict of interest.
Contributor Information
Nina Suh, Email: nsuh@uwo.ca.
Eric C. Benson, Phone: +1-505-2724107, FAX: +1-505-2728098, Email: ebenson@salud.unm.edu
Kenneth J. Faber, Phone: +44-519-6466312, FAX: +44-519-6466049, Email: kjfaber@uwo.ca
Joy MacDermid, Phone: +44-519-6466100, FAX: +44-519-6466049, Email: joy.macdermid@sjhc.london.on.ca.
Ruby Grewal, Phone: +44-519-6466286, FAX: +44-519-6466049, Email: rgrewa@uwo.ca.
References
- 1.Adolfsson L, Lindau T, Arner M. Acutrak screw fixation versus cast immobilization for undisplaced scaphoid waist fractures. J Hand Surg [Br] 2001;26B(3):192–195. doi: 10.1054/jhsb.2001.0558. [DOI] [PubMed] [Google Scholar]
- 2.Arora R, Gschwentner M, Krappinger D, Lutz M, Blauth M, Gabl M. Fixation of nondisplaced scaphoid fractures: making treatment cost effective: prospective controlled trial. Arch Orthop Trauma Surg. 2007;127:39–46. doi: 10.1007/s00402-006-0229-z. [DOI] [PubMed] [Google Scholar]
- 3.Bedi A, Jebson PJL, Hayden RJ, Jacobson JA, Martus JE. Internal fixation of acute, non-displaced scaphoid waist fracture via a limited dorsal approach: an assessment of radiographic and functional outcomes. J Hand Surg. 2007;32A:326–33. doi: 10.1016/j.jhsa.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 4.Bond CD, Shin AY, McBride MT, Dao KD. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. J Bone Joint Surg Am. 2001;83A(4):483–8. doi: 10.2106/00004623-200104000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Brutus JP, Baeten Y, Chahidi N, Kinnen L, Moermans JP, Ledoux P. Percutaneous Herbert screw fixation for fractures of the scaphoid: review of 30 cases. Chir Main. 2002;21:350–4. doi: 10.1016/S1297-3203(02)00138-5. [DOI] [PubMed] [Google Scholar]
- 6.Bushnell BD, McWilliams AD, Messer TM. Complications in dorsal percutaneous cannulated screw fixaton of nondisplaced scaphoid waist fractures. J Hand Surg. 2007;32A(6):827–33. doi: 10.1016/j.jhsa.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Caloia MF, Gallino RN, Caloia H, Rivarola H. Incidence of ligamentous and other injuries associated with scaphoid fractures during arthroscopically assisted reduction and percutaneous fixation. Arthroscopy. 2008;24(7):754–9. doi: 10.1016/j.arthro.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Chen ACY, Chao EK, Hung SS, Lee MSS, Ueng SWN. Percutaneous screw fixation for unstable scaphoid fractures. J Trauma. 2005;59(1):184–7. doi: 10.1097/01.TA.0000171525.62755.33. [DOI] [PubMed] [Google Scholar]
- 9.Christodoulou L, Chamberlain ST. Internal fixation of scaphoid fractures with an AO mini-fragment lag screw, using temporary interoperative AO mini external fixation. J Hand Surg Br. 1999;24B(6):676–8. doi: 10.1054/jhsb.1999.0262. [DOI] [PubMed] [Google Scholar]
- 10.Chung KC. A simplified approach for unstable scaphoid fracture fixation using the Acutrak screw. Plast Reconstr Surg. 2002;110(7):1697–703. doi: 10.1097/00006534-200212000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Clay NR, Dias JJ, Costigan PS, Gregg PJ, Barton NJ. Need the thumb be immobilized in scaphoid fractures? J Bone Joint Surg Br. 1991;73B:828–32. doi: 10.1302/0301-620X.73B5.1894676. [DOI] [PubMed] [Google Scholar]
- 12.Vos J, Vandenberghe D. Acute percutaneous scaphoid fixation using a non-cannulated Herbert screw. Chir Main. 2003;22:78–83. doi: 10.1016/S1297-3203(03)00026-X. [DOI] [PubMed] [Google Scholar]
- 13.Dias JJ, Wildin CJ, Bhowal B, Thompson JR. Should acute scaphoid fractures be fixed? J Bone Joint Surg Am. 2005;87A(10):2160–8. doi: 10.2106/JBJS.D.02305. [DOI] [PubMed] [Google Scholar]
- 14.Dias JJ, Dhukaram V, Abhinav A, Bhowal B, Wildin CJ. Clinical and radiological outcome of cast immobilisation versus surgical treatment of acute scaphoid fractures at a mean follow-up of 93 months. J Bone Joint Surg Br. 2008;90(7):899–905. doi: 10.1302/0301-620X.90B7.20371. [DOI] [PubMed] [Google Scholar]
- 15.Reis FB, Koeberle G, Leite NM, Katchburian MV. Internal fixation of scaphoid injuries using the Herbert screw through a dorsal approach. J Hand Surg. 1993;18A:792–7. doi: 10.1016/0363-5023(93)90044-4. [DOI] [PubMed] [Google Scholar]
- 16.Drac P, Manak P, Labonek I. Percutaneous osteosynthesis versus cast immobilization for the treatment of minimally and non-displaced scaphoid fractures: functional outcomes after a follow-up of at least 12 month. Biomed Papers. 2005;149(1):149–51. doi: 10.5507/bp.2005.018. [DOI] [PubMed] [Google Scholar]
- 17.Duppe H, Johnell O, Ludborg G, Karlsson M, Redlund-Johnell I. Long-term results of fracture of the scaphoid. J Bone Joint Surg Am. 1994;76A(2):249–52. doi: 10.2106/00004623-199402000-00012. [DOI] [PubMed] [Google Scholar]
- 18.Filan SL, Herbert TJ. Herbert screw fixation of scaphoid fractures. J Bone Joint Surg. 1996;78B(4):519–29. [PubMed] [Google Scholar]
- 19.Fusetti C, Garavaglia G, Papaloizos MY, Wasserfallen JB, Buchler U, Nagy L. Direct and indirect costs in the conservative management of undisplaced scaphoid fractures. Eur J Orthop Surg Traumatol. 2003;13:241–4. doi: 10.1007/s00590-003-0101-6. [DOI] [Google Scholar]
- 20.Gellman H, Caputo RJ, Carter V, Aboulafia A, McKay M. Comparison of short arm and long thumb-spica casts for non-displaced fractures of the carpal scaphoid. J Bone Joint Surg Am. 1989;71A(3):354–7. [PubMed] [Google Scholar]
- 21.Gunal I, Oztuna V, Seber S. Trapezio-lunate external fixation for scaphoid fractures: an experimental and clinical study. J Hand Surg Br. 1994;19B:759–62. doi: 10.1016/0266-7681(94)90254-2. [DOI] [PubMed] [Google Scholar]
- 22.Gunal Y, Oztuna V, Ozcelik A, Kose N, Turgut A, Gokturk E, Seber S. Medium-term results of trapezio-lunate external fixation for scaphoid fractures. J Hand Surg Br. 2002;27B(5):410–2. doi: 10.1054/jhsb.2002.0786. [DOI] [PubMed] [Google Scholar]
- 23.Haddad FS, Goddard NJ. Acute percutaneous scaphoid fixation using a cannulated screw. Ann Chir Main. 1998;17(2):119–26. doi: 10.1016/s0753-9053(98)80005-7. [DOI] [PubMed] [Google Scholar]
- 24.Haddad FS, Goddard NJ. Acute percutaneous scaphoid fixation. J Bone Joint Surg Br. 1998;80B(1):95–9. doi: 10.1302/0301-620X.80B1.8076. [DOI] [PubMed] [Google Scholar]
- 25.Hambidge JE, Desai VV, Schranz PJ, Compson JP, Davis TRC, Barton NJ. Acute fractures of the scaphoid: treatment by cast immobilization with the wrist in flexion or extension. J Bone Joint Surg Br. 1999;81B(1):91–2. doi: 10.1302/0301-620X.81B1.9367. [DOI] [PubMed] [Google Scholar]
- 26.Harniman E, Carette S, Kennedy C, Beaton D. Extracorporeal shock wave therapy for calcific and noncalcific tendonitis of the rotator cuff: a systematic review. J Hand Ther. 2004;17:132–51. doi: 10.1197/j.jht.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Hove LM. Epidemiology of scaphoid fractures in Bergen, Norway. Scand J Plast Reconstr Surg Hand Surg. 1999;33:423–6. doi: 10.1080/02844319950159145. [DOI] [PubMed] [Google Scholar]
- 28.Inoue G, Shionoya K. Herbert screw fixation by limited access for acute factures of the scaphoid. J Bone Joint Surg Br. 1997;79B:418–21. doi: 10.1302/0301-620X.79B3.7254. [DOI] [PubMed] [Google Scholar]
- 29.Jeon IH, Oh CW, Park BC, Ihn JC, Kim PT. Minimal invasive percutaneous Herbert screw fixation in acute unstable scaphoid fracture. Hand Surg. 2003;8(2):213–8. doi: 10.1142/S0218810403001807. [DOI] [PubMed] [Google Scholar]
- 30.Khan FA, Harby S. Fresh scaphoid fractures (analysis of 45 cases) Afr J Med Med Sci. 1995;24:201–6. [PubMed] [Google Scholar]
- 31.Korkala OL, Kuokkanen HO, Eerola MS. Compression-staple fixation for fractures, nonunions, and delayed unions of the carpal scaphoid. J Bone Joint Surg Am. 1992;74:423–6. [PubMed] [Google Scholar]
- 32.Kujala S, Raatikainen T, Kaarela O, Ashammakhi N, Ryhanen J. Successful treatment of scaphoid fractures and nonunions using bioabsorbable screws: report of six cases. J Hand Surg. 2004;29A:68–73. doi: 10.1016/j.jhsa.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 33.Lindstrom G, Nystrom A. Incidence of post-traumatic arthrosis after primary healing of scaphoid fractures: a clinical and radiological study. J Hand Surg Br. 1990;15B:11–3. doi: 10.1016/0266-7681_90_90041-2. [DOI] [PubMed] [Google Scholar]
- 34.McQueen MM, Gelbke MK, Wakefield A, Will EM, Gaebler C. Percutaneous screw fixation versus conservative treatment for fractures of the waist of the scaphoid. J Bone Joint Surg Br. 2008;90B(1):66–71. doi: 10.1302/0301-620X.90B1.19767. [DOI] [PubMed] [Google Scholar]
- 35.Meermans G, Verstreken F. Percutaneous transtrapezial fixation of acute scaphoid fractures. J Hand Surg Eur. 2008;33(6):791–6. doi: 10.1177/1753193408092785. [DOI] [PubMed] [Google Scholar]
- 36.Moran R, Curtin J. Scaphoid fractures treated by Herbert screw fixation. J Hand Surg. 1988;13B(4):453–5. doi: 10.1016/0266-7681_88_90178-7. [DOI] [PubMed] [Google Scholar]
- 37.Muller M, Tsui D, Schnurr R, Biddulph-Deisroth L, Hard J, MacDermid JC. Effectiveness of hand therapy interventions in primary management of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004;17:210–28. doi: 10.1197/j.jht.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 38.Müller M, Germann G, Sauerbier M. Minimal invasive screw fixation and early mobilization of acute scaphoid fractures in the middle third: operative technique and early functional outcome. Tech Hand Up Extrem Surg. 2008;12(2):107–13. doi: 10.1097/BTH.0b013e3181629401. [DOI] [PubMed] [Google Scholar]
- 39.Papaloizos MY, Fusetti C, Christen T, Nagy L, Waserfallen JB. Minimally invasive fixation versus conservative treatment of undisplaced scaphoid fractures: a cost-effectiveness study. J Hand Surg Br. 2004;29B(2):116–9. doi: 10.1016/j.jhsb.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 40.Raudasoja L, Rawlins M, Kallio P, Vasenius J. Conservative treatment of scaphoid fractures: a follow-up study. Ann Chir Gynaecol. 1999;88:289–93. [PubMed] [Google Scholar]
- 41.Rettig AC, Weidenbener EJ, Gloyeske R. Alternative management of midthird scaphoid fractures in the athlete. Am J Sports Med. 1994;22(5):711–4. doi: 10.1177/036354659402200522. [DOI] [PubMed] [Google Scholar]
- 42.Rettig AC, Kollias SC. Internal fixation of acute stable scaphoid fractures in the athlete. Am J Sports Med. 1996;24(2):182–6. doi: 10.1177/036354659602400211. [DOI] [PubMed] [Google Scholar]
- 43.Rettig ME, Raskin KB. Retrograde compression screw fixation of acute proximal pole scaphoid fractures. J Hand Surg. 1999;24A:1206–10. doi: 10.1053/jhsu.1999.1206. [DOI] [PubMed] [Google Scholar]
- 44.Rettig ME, Kozin SH, Cooney WP. Open reduction and internal fixation of acute displaced scaphoid waist fractures. J Hand Surg. 2001;26A:271–6. doi: 10.1053/jhsu.2001.21524. [DOI] [PubMed] [Google Scholar]
- 45.Roolker W, Maas M, Broekhuizen AH. Diagnosis and treatment of scaphoid fractures, can nonunion be prevented? Arch Orthop Trauma Surg. 1999;119:428–31. doi: 10.1007/s004020050014. [DOI] [PubMed] [Google Scholar]
- 46.Saeden B, Tornkvist H, Ponzer S, Hoglund M. Fracture of the carpal scaphoid: a prospective, randomized 12-year follow-up comparing operative and conservative treatment. J Bone Joint Surg Br. 2001;83B(2):230–4. doi: 10.1302/0301-620X.83B2.11197. [DOI] [PubMed] [Google Scholar]
- 47.Shih JT, Lee HM, Hou YT, Tan CM. Results of arthroscopic reduction and percutaneous fixation for acute displaced scaphoid fractures. Arthroscopy. 2005;21(5):620–6. doi: 10.1016/j.arthro.2005.02.020. [DOI] [PubMed] [Google Scholar]
- 48.Singh HP, Forward D, Davis TRC, Dawson JS, Oni JA, Downing ND. Partial union of acute scaphoid fractures. J Hand Surg Br. 2005;30B(5):440–5. doi: 10.1016/j.jhsb.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 49.Slade JF, III, Gutow AP, Geissler WB. Percutaneous internal fixation of scaphoid fractures via an arthroscopically assisted dorsal approach. J Bone Joint Surg. 2002;84:21–36. doi: 10.2106/00004623-200200002-00003. [DOI] [PubMed] [Google Scholar]
- 50.Slade JF, III, Gillon T. Retrospective review of 234 scaphoid fractures and nonunions treated with arthroscopy for union and complications. Scand J Surg. 2008;97(4):280–9. doi: 10.1177/145749690809700402. [DOI] [PubMed] [Google Scholar]
- 51.Slade JF, Lozano-Calderón S, Merrell G, Ring D. Arthroscopic-assisted percutaneous reduction and screw fixation of displaced scaphoid fractures. J Hand Surg Eur. 2008;33(3):350–4. doi: 10.1177/1753193408090121. [DOI] [PubMed] [Google Scholar]
- 52.Smith JT, Keeve JP, Bertin KC, Mann RJ. Simultaneous fractures of the distal radius and scaphoid. J Trauma. 1988;28(5):676–9. doi: 10.1097/00005373-198805000-00021. [DOI] [PubMed] [Google Scholar]
- 53.Smith K, Helm R, Tonkin MA. The Herbert screw for the treatment of scaphoid fractures. Ann Chir Main Memb Supér. 1991;10(6):556–63. doi: 10.1016/S0753-9053(05)80327-8. [DOI] [PubMed] [Google Scholar]
- 54.Terkelsen CJ, Jepsen JM. Treatment of scaphoid fractures with a removable cast. Acta Ortho Scand. 1988;59(4):452–3. doi: 10.3109/17453678809149402. [DOI] [PubMed] [Google Scholar]
- 55.Trumble TE, Benirschke SK, Vedder NB. Ipsilateral fractures of the scaphoid and radius. J Hand Surg. 1993;18A:8–14. doi: 10.1016/0363-5023(93)90237-W. [DOI] [PubMed] [Google Scholar]
- 56.Trumble TE, Gilbert M, Murray LW, Smith J, McCallister WV. Displaced scaphoid fractures treated with open reduction and internal fixation with a cannulated screw. J Bone Joint Surg. 2000;82:633–41. doi: 10.2106/00004623-200005000-00004. [DOI] [PubMed] [Google Scholar]
- 57.Tu YK, Chen AC, Chou YC, Ueng SW, Ma CH, Yen CY. Treatment for scaphoid fracture and nonunion—the application of 3.0 mm cannulated screws and pedicle vascularised bone grafts. Injury. 2008;39(Suppl 4):96–106. doi: 10.1016/j.injury.2008.08.035. [DOI] [PubMed] [Google Scholar]
- 58.Vinnars B, Af Ekenstam F, Gerdin B. Comparison of direct and indirect costs of internal fixation and cast treatment in acute scaphoid fractures: a randomized trial involving 52 patients. Acta Orthop. 2007;78(5):672–9. doi: 10.1080/17453670710014383. [DOI] [PubMed] [Google Scholar]
- 59.Vinnars B, Pietreanu M, Bodestedt A, Ekenstam F, Gerdin B. Nonoperative compared with operative treatment of acute scaphoid fractures. A randomized clinical trial. J Bone Joint Surg Am. 2008;90(6):1176–85. doi: 10.2106/JBJS.G.00673. [DOI] [PubMed] [Google Scholar]
- 60.Vukov V, Ristic K, Stevanovic M, Bumbasirevic M. Simultaneous fractures of the distal end of the radius and the scaphoid bone. J Orthop Trauma. 1988;2(2):120–3. doi: 10.1097/00005131-198802010-00006. [DOI] [PubMed] [Google Scholar]
- 61.Wozasek GE, Moser KD. Percutaneous screw fixation for fractures of the scaphoid. J Bone Joint Surg. 1991;73B(1):138–42. doi: 10.1302/0301-620X.73B1.1670499. [DOI] [PubMed] [Google Scholar]
- 62.Yin ZG, Zhang JB, Kan SL, Wang P. Treatment of scaphoid fractures: systematic review and meta-analysis. Clin Orthop Relat Res. 2007;460:142–51. doi: 10.1097/BLO.0b013e31803d359a. [DOI] [PubMed] [Google Scholar]
- 63.Yip HSF, Wu WC, Chang RYP, So TYC. Percutaneous cannulated screw fixation of acute scaphoid waist fracture. J Hand Surg Br. 2002;27B(1):42–6. doi: 10.1054/jhsb.2001.0690. [DOI] [PubMed] [Google Scholar]