ABSTRACT
BACKGROUND
Patients must be informed about risks before any treatment can be implemented. Yet serious problems in communicating these risks occur because of framing effects.
OBJECTIVE
To investigate the effects of different information frames when communicating health risks to people with high and low numeracy and determine whether these effects can be countered or eliminated by using different types of visual displays (i.e., icon arrays, horizontal bars, vertical bars, or pies).
DESIGN
Experiment on probabilistic, nationally representative US (n = 492) and German (n = 495) samples, conducted in summer 2008.
OUTCOME MEASURES
Participants’ risk perceptions of the medical risk expressed in positive (i.e., chances of surviving after surgery) and negative (i.e., chances of dying after surgery) terms.
KEY RESULTS
Although low‐numeracy people are more susceptible to framing than those with high numeracy, use of visual aids is an effective method to eliminate its effects. However, not all visual aids were equally effective: pie charts and vertical and horizontal bars almost completely removed the effect of framing. Icon arrays, however, led to a smaller decrease in the framing effect.
CONCLUSIONS
Difficulties with understanding numerical information often do not reside in the mind, but in the representation of the problem.
KEY WORDS: risk communication, risk perception, numeracy, framing, visual aids, medical decision making
INTRODUCTION
Many professionals in health care provide information about risks to enhance patients’ informed choices. Recently, the structure and content of these health messages have received substantial attention in the literature in judgment and decision making.1 A prominent example is the impact of how the messages are framed on people’s attitudes and behaviors.2–6 Following the work of Kahneman and Tversky in the 1970s and early 1980s,7–10 framing is defined as the presentation of two logically equivalent situations, where one is presented in positive or gain terms and the other in negative or loss terms.5,11 Examples of framing are chances of mortality versus survival from surgery and a focus on the risks or disadvantages of not agreeing to a medical screening versus emphasis on the benefits or advantages of doing so.2,12
Framing studies dealing with health messages have shown mixed results. In line with Kahneman and Tversky’s7,8 conclusion that people show risk aversion under gain framings and risk-seeking behaviors under loss framings, several authors2,4,6,11,13–15 suggested that gain frames might be more effective in promoting disease prevention behaviors, whereas loss frames might be more effective for disease detection behaviors. In line with this hypothesis, gain frames have been more effective when promoting exercise,16 reduced alcohol use,17 parental use of children’s car seat restraints,18,19 skin cancer prevention behaviors,20,21 and use of condoms to prevent HIV22; loss frames have been more effective at encouraging individuals to engage in breast self-examination,23,24 mammography screenings,25–30 blood-cholesterol screenings,31 HIV screenings,32,33 and skin cancer detection.20,34 Finally, for decisions about surgical procedures and treatments, gain frames (probability of success or survival) induce greater compliance than loss frames (probability of failure or death10,35–38).
Previous research has also shown important individual differences in susceptibility to framing.39–41 Individuals who have low educational attainment demonstrated a stronger framing effect than did highly educated individuals.42 Similarly, people with low numeracy—who have difficulties grasping numerical concepts necessary for understanding risk communications43–45—are more susceptible to framing than those with high numeracy.46,47 Other studies, however, reported no differences between framing conditions or even found framing effects in the opposite direction to that hypothesized (48–54; see55,56 for reviews), leaving open a number of important questions related to the effects of different health message frames.
First, to the best of our knowledge all the studies about framing were conducted on convenience samples of specific groups of participants (e.g., patients with particular diseases or students2–6). These studies provide valuable information about the influence of framing in these participants. Framing variations, however, have different effects depending on factors such as participants’ demographic characteristics and previous experiences.2,6,32,57 Differences between studies in these factors might explain the contradictory results in the literature. Moreover, due to nonprobabilistic sampling methods, results in the published literature cannot be generalized to a wider population. In this study, we examine the effect of different information frames using probabilistic, nationally representative samples. To test the generalizability of our findings, we conducted a study in two countries—the United States and Germany.
Second, several authors have suggested that using framing to enhance the effects of health messages is not consistent with truly informed decision making and, consequently, should be avoided.2,11 Others have suggested that encouraging people to become aware of framing effects, rather than trying to eliminate them, might lead to sustained improvements in patient care.58 To our knowledge, however, few empirical studies have evaluated methods for avoiding or making salient the effects of framing.59 Visual aids have been proposed as a potentially promising method for communicating risks. They can improve understanding of risks associated with different treatments, screenings, and lifestyles (60–66; but see67) and promote consideration of beneficial treatments that have side effects.68 Visual aids are also effective in eliminating errors induced by anecdotal narratives69 and biases.70,71 In addition, risk information presented via visual aids is perceived as easier to understand72,73 and has been shown to substantially increase risk avoidance.74 What is still an open question is whether visual aids can reduce framing effects. Which visual aids, if any, are particularly effective has also not been investigated.
Last but not least, people differ in the extent to which they benefit from visual aids. For instance, icon arrays—that is, visual representations symbolizing patients11,59,65—are useful for enhancing comprehension of risk reduction in people with low numeracy skills.61–65,68,69,75,76 Adding icon arrays to numerical information about risk reduction helps these people make more accurate assessments. Individuals with fewer difficulties with numerical concepts, by contrast, often make accurate estimates even if icon arrays are not provided. It is still an open question whether visual aids are more effective at eliminating framing effects in low-numeracy individuals—who are at the same time more susceptible to framing than those with high numeracy.46,47 In a similar vein, it is not known whether certain types of visual aids are more appropriate for low-numeracy individuals and other types for those with high numeracy.46 The present study sought to address these questions.
METHODS
Sample
The study was conducted with probabilistic, nationally representative samples in the US (n = 1,009) and Germany (n = 1,001), using panels of households selected through probabilistic random-digit-dial telephone surveys and supplied with equipment that enabled them to complete computerized questionnaires. These panels, maintained by the companies Forsa (Germany, 20,000 or 11% of initially contacted households) and Knowledge Networks (US, 43,000 or 16% of initially contacted households), allow for statistical inference to the general population. These panels were already used successfully in a number of studies in the areas of health and medicine, political and social sciences, and economics and public policy.77–81 Methodological studies have shown that data from such panels are comparable to the results obtained through traditional probabilistic surveys.82
A random half of the individuals in each country participated in this study, resulting in 495 participants in Germany and 492 participants in the US. The sample structure is shown in Table 1. According to official statistics, the percentage of less educated people is much higher in Germany than in the US. We then oversampled the less educated population in the US to ensure equivalent sample sizes of less educated participants in both countries. This was important because the study was conducted within a project that focused specifically on people with low educational attainment. To adjust for this, as well as for minor discrepancies due to nonresponse, post-stratification weights were used to bring the sample proportions in line with the population proportions. The Ethics Committee of the Max Planck Institute for Human Development approved the methodology, and all participants consented to participation through an online consent form at the beginning of the study.
Table 1.
Structure of the Sample in the Study by Gender, Age, and Education
| Germany | United States | |||||
|---|---|---|---|---|---|---|
| Sample size (unweighted) | Sample % (weighted) | Population %a | Sample size (unweighted) | Sample % (weighted) | Population %† | |
| Total | 495 | 492 | ||||
| Gender | ||||||
| Male | 254 | 50.3 | 49.9 | 236 | 48.4 | 49.2 |
| Female | 241 | 49.7 | 50.1 | 256 | 51.6 | 50.8 |
| Age | ||||||
| 25–39 | 125 | 31.4 | 32.5 | 120 | 31.2 | 35.7 |
| 40–54 | 210 | 39.0 | 39.9 | 194 | 40.6 | 38.3 |
| 55–69 | 160 | 29.6 | 27.7 | 178 | 28.2 | 26.1 |
| Education | ||||||
| High school or less | 393 | 74.1 | 72.3 | 356 | 44.5 | 44.6 |
| At least some college | 102 | 26.0 | 27.7 | 136 | 55.5 | 55.4 |
| Numeracy skills | 69% (SE = 1.1%)♣ | 65% (SE = 1.3%)♣ | ||||
aSource: Statistisches Bundesamt Deutschland, Microcensus, 2007 (https://www‐genesis.destatis.de/genesis/online; accessed September 15, 2008)
†Source: US Census Bureau, Current Population Survey, 2008 Annual Social and Economic Supplement (http://pubdb3.census.gov/macro/032008/perinc/toc.htm; accessed September 15, 2008
♣Percentage of items answered correctly
Response Rates
Of the panel members who were invited to the present study, 52% in Germany and 54% in the US completed the questionnaire. As shown in Table 1, the demographic structure of the sample corresponds to that of the general populations in both countries, and there were no obvious nonresponse biases.
Stimuli and Procedure
All participants completed a computerized questionnaire that was developed in English and translated into German. The materials in English and German were back-translated, and any inconsistencies were resolved by a bilingual speaker to ensure that the two versions were comparable. All translations were performed by skilled translators. When programming the questionnaire, special care was taken to ensure the interface looked the same in the German and American versions.
All of the participants in the study completed a numeracy scale consisting of nine items developed by Schwartz, Woloshin, Black, and Welch,83 and by Lipkus, Samsa, and Rimer.84 An example of an item is “Imagine that we flip a fair coin 1,000 times. What is your best guess about how many times the coin would come up heads in 1,000 flips?” In the analyses that follow, we split the participants into two groups according to their group’s median numeracy scores. The low-numeracy group includes participants with six or fewer correct answers, while the high-numeracy group includes those with seven or more correct answers (see Peters et al.47 for a similar procedure). US and German participants were evenly distributed in the high- and low-numeracy groups. The German participants had somewhat higher scores on this scale: They answered on average 69% of the items correctly, while Americans answered 65% of the items correctly.
Participants were presented with two medical scenarios expressing the risk associated with a surgical procedure in either negative (i.e., chances of dying) or positive (i.e., chances of surviving) terms. Following Schwartz, Woloshin, and Welch,85 participants received the following information when the risk was expressed in negative terms: “Mr. Roe needs surgery: 9 in 1,000 people die from this surgery.” When the risk was expressed in positive terms, participants were told: “Mr. Smythe needs surgery: 991 in 1,000 people survive this surgery.” The participants were then asked to evaluate the perceived risk of the surgical procedure on a 4-point scale, ranging from 1 (not risky at all) to 4 (very risky). Half of the participants were randomly assigned to answer the negatively framed question first, while the remaining participants answered the positively framed question first. Between the two scenarios, all participants answered a set of unrelated problems involving risks (for more details on these problems, see75). The order of the questions did not have any effect on the results and the orderings were combined for further analyses.
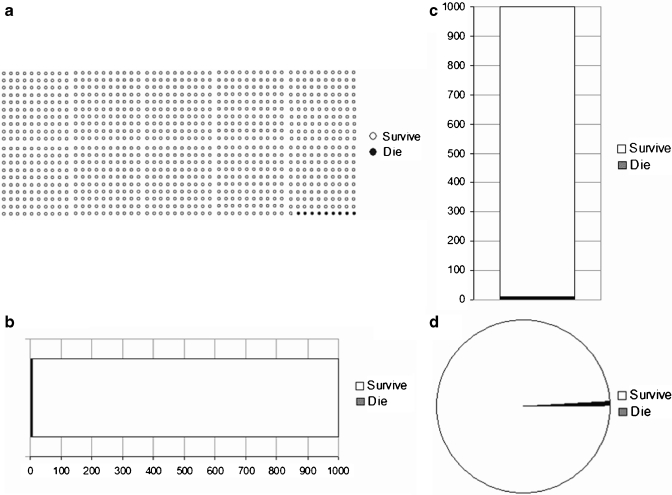
The provision of visual aids—in addition to the numerical information about the risk—was manipulated between groups with five conditions. In the four visual aids conditions, participants were told that the numerical information was also represented in the picture that appeared on the same page, and the number of patients who died and survived from surgery were represented using an icon array, a horizontal bar graph, a vertical bar graph, or a pie chart (see Fig. 1). We used circles to represent patients in the icon arrays because previous research did not find differences in effects of arrays with faces compared to more abstract symbols.86 Finally, participants in the numerical condition did not receive visual aids, but got only the numerical information.
Figure 1.
(a) Icon array presented in Condition 1. (b) Horizontal bar graph presented in Condition 2. (c) Vertical bar graph presented in Condition 3. (d) Pie chart presented in Condition 4. All figures represented the number of people who died (i.e., 9) and survived (i.e., 991) from the surgery. Original material was in either German or English.
RESULTS
Do People Show Framing Effects in Their Risk Perceptions? Do People with Low Numeracy Show More Susceptibility to Framing than Those with High Numeracy?
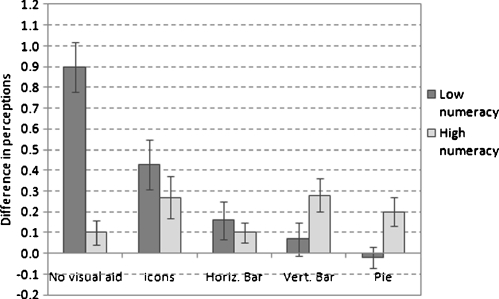
Figure 2 shows the average difference between perceptions of the medical risk expressed in positive and negative terms in participants with low and high numeracy. The larger the difference, the stronger is the framing effect. When only numerical information was provided, participants with low numeracy often perceived the surgical procedure as less risky when the associated risk was presented in positive (i.e., chances of surviving) than in negative (i.e., chances of dying) terms. In contrast, participants with high numeracy often provided equal estimates when the risks were expressed in positive and negative terms. Participants with low numeracy, therefore, were more susceptible to framing than those with high numeracy. Consistent with this result, an analysis of variance (ANOVA) with numeracy as a between-subjects factor on the average difference between perceptions of the medical risk expressed in positive and negative terms showed a significant main effect of numeracy (F1,166 = 34.19, p = 0.001). This effect held in both the German and the American sample.
Figure 2.
Average difference between perceptions of the medical risk expressed in positive and negative terms, by visual aid condition and numeracy. The larger the difference, the stronger is the framing effect and vice versa. Error bars represent one standard error.
Do Visual Aids Help Reduce the Framing Effect? Are Visual Aids Especially Helpful for Participants with Low Numeracy?
As Figure 2 shows, when visual aids were added to the numerical information, the effect of framing was reduced or disappeared in low-numeracy participants. Not all visual aids, however, were equally effective: Pie charts and vertical and horizontal bars almost completely removed the effect of framing. Icon arrays, however, led to a smaller decrease in the framing effect. Furthermore, in contrast to participants with low numeracy, participants more skilled in using quantitative information benefitted less from visual aids: For these participants, the average difference between perceptions of the risk expressed in positive and negative terms was similar when they received and did not receive visual aids. Similar results were obtained regardless of which visual aid was provided. Consistent with these findings, the ANOVA with visual aids and numeracy as between-subjects factors on the average difference between perceptions of the risk expressed in positive and negative terms showed a main effect of visual aids (F4,967 = 8.15, p = 0.001), and a significant interaction between numeracy and visual aids (F4,967 = 12.23, p = 0.001). These effects were present in both the US and Germany. For all the analyses, the inclusion of participants’ sex, age, and level of education as covariates did not systematically influence the pattern of results.
DISCUSSION
Informed consent laws mandate that patients must be informed about risks before any treatment can be implemented. Our research confirms that problems in communicating these risks result from the effects of using different information frames, especially in people who are more vulnerable to having difficulty when making decisions. Low numeracy participants both in the US and Germany perceived a surgical procedure as less risky when the associated risk was expressed as chance of surviving than of dying, whereas participants with high numeracy did not differ in their perceptions. These results are in line with previous research showing that people with low numeracy also have less accurate perceptions of the risks and benefits of screening83,87,88 and are more susceptible to biases in judgments and decisions than those with high numeracy,44,70,71,89,90 which reduces medication compliance, impedes access to treatments, impairs risk communication, and adversely affects medical outcomes.44 Our results are also consistent with previous literature supporting the notion that gain frames induce greater compliance for surgical procedures than loss frames.10,35–38 Our research extended this literature. In particular, it revealed the significant influence of people’s numeracy skills on the effects of framing information about health, which could shed light on the mixed results in the literature on the issue. Differences between studies in participants’ numeracy skills because of the use of convenience samples and nonprobabilistic sampling methods could possibly explain why some reported no framing effects,48–54 whereas others found strong effects of message frames.10,35–38
More importantly, our study is unique in its efforts to investigate whether visual aids can overcome framing effects when communicating important health information in participants who were disadvantaged by their lack of numerical skills: When visual aids were added to the numerical information about the risk of the surgical procedure, framing was reduced or disappeared in participants with low numeracy. These results extend our own and others’ previous findings about the usefulness of visual aids to enhance comprehension of medical risks, especially in people with low numeracy.1,46,61–65,68–71,73,75,76 They also support the notion that problems in communicating risks occur because inappropriate information formats are often used and not because of cognitive biases.91,92 Similar reductions in what superficially looked like biased thinking were observed in the case of conditional probabilities (when expressed as natural frequencies,93), relative risk reductions (when expressed as absolute risk reductions,94), and single-event probabilities.95
In line with previous research,46 our results also show that not all visual aids are equally effective in communicating risk information: Although all visual aids were useful, larger reductions in the effect of message frames were achieved when low‐numeracy participants were provided with pie charts or bar graphs than when they received icon arrays. This result is in contrast with our previous research75 in which we measured participants’ accuracy of risk understanding after reading a medical scenario about the usefulness of a new hypothetical drug. In this research, icon arrays and bar graphs were equally useful. A possible explanation of these contradictory findings is that pie charts and bar graphs might have promoted “gist” processing (e.g., the relative size of different areas in the visual aid), whereas icon arrays might have encouraged more precise, quantitative processing (e.g., the number of patients who died and survived after the surgery96). Although equally precise in the short run (i.e., after reading the health information; a61,70,71,75), the latter type of processing may make it more difficult to retain the information over a long period (i.e., in the second phase of the current study)—in particular for participants with low numeracy. Consequently, the low numeracy participants who received icon arrays, compared to those who received pie and bar charts might have been less likely to recognize that the information presented was the same in both scenarios in the current study.
At the same time, our research has several limitations. Our research focused on the factors that moderate the effect of framed messages. However, it did not investigate the processes that mediate the influence of framed messages on people’s risk perceptions and risky behaviors and why visual aids reduce the effect of framed messages. Preliminary research by Garcia-Retamero and Cokely97 suggested that visual aids might modify the effect that the message frame has on people’s attitudes, which ultimately impact their behavioral intentions. More research in this line is needed. Another limitation relates to the fact that our study did not involve real patient-doctor interactions. Although our experiment enabled us to draw clear conclusions, it is possible that visual aids would show additional benefits in clinical settings. Finally, in our experiment we only focused on attribute framing. That is, the object of the framed message was an attribute of the decision options (e.g., the risk associated with a surgical procedure) and measured risk perceptions. It would be interesting to explore the effectiveness of visual aids in goal framing, that is, when the health message frames the relationship between certain behaviors and goal attainments—e.g., a message promoting condom use can emphasize either the benefits of this practice or the costs of avoiding this practice4,14,15; see also98—and in choice behavior (i.e., the standard dependent variable in previous studies on the issue). Future research could also explore whether the impact of visual aids on the effect of framed messages depends on other important factors such as people’s topic knowledge99 or graphical skills,62 and on the target of the behavior (i.e., whether people make decisions for themselves or for others100).
Our findings have important implications for medical practice as they suggest suitable ways to communicate quantitative medical data to people who are more disadvantaged by their lack of numerical skills: To communicate information about risks in a way that is truly consistent with informed decision making, health information could be framed in either positive or negative terms as long as visual aids representing the information are provided. In contrast, if the goal is to persuade patients rather than enhance their informed decision making (e.g., cessation of smoking), framing the risk information in positive terms for disease prevention or treatment selection, and in negative terms for disease detection would be most effective.4 Perhaps this is justifiable in some situations to achieve the greatest health gain.
Acknowledgments
We thank Anita Todd for editing the manuscript. This study is part of two projects, “Helping people with low numeracy to understand medical information,” funded by the Foundation for Informed Medical Decision Making (US) and the Max Planck Society (Germany), and “How to improve understanding of risks about health (PSI2008-02019),” funded by the Ministerio de Ciencia e Innovación (Spain).
Conflict of Interests None disclosed.
Contributor Information
Rocio Garcia-Retamero, Email: rretamer@ugr.es.
Mirta Galesic, Email: galesic@mpib-berlin.mpg.de.
REFERENCES
- 1.Garcia-Retamero R, Galesic M. Risk communication and medical decision making: a cross-cultural perspective. Springer, Berlin-Heidelberg, in press.
- 2.Edwards A, Elwyn G, Covey J, Matthews E, Pill R. Presenting risk information—a review of the effects of “framing” and other manipulations on patient outcomes. J Health Commun. 2001;6:61–82. doi: 10.1080/10810730150501413. [DOI] [PubMed] [Google Scholar]
- 3.Kuhberger A. The influence of framing on risky decisions: a meta-analysis. Organ Behav Hum Decis Process. 1998;75:23–55. doi: 10.1006/obhd.1998.2781. [DOI] [PubMed] [Google Scholar]
- 4.Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behaviour: the role of message framing. Psychol Bull. 1997;121:3–19. doi: 10.1037/0033-2909.121.1.3. [DOI] [PubMed] [Google Scholar]
- 5.Wilson DK, Purdon SE, Wallston KA. Compliance to health recommendations: a theoretical overview of message framing. Health Educ Res. 1988;3:161–71. doi: 10.1093/her/3.2.161. [DOI] [Google Scholar]
- 6.Salovey P, Williams-Piehota P. Field experiments in social psychology: message framing and the promotion of health protective behaviors. Am Behav Sci. 2004;47:488–505. doi: 10.1177/0002764203259293. [DOI] [Google Scholar]
- 7.Kahneman D, Tversky A. Prospect theory: an analysis of decision making under risk. Econometrica. 1979;6:621–30. [Google Scholar]
- 8.Kahneman D, Tversky A. The psychology of preferences. Sci Am. 1982;46:160–73. doi: 10.1038/scientificamerican0182-160. [DOI] [Google Scholar]
- 9.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–8. doi: 10.1126/science.7455683. [DOI] [PubMed] [Google Scholar]
- 10.McNeil BJ, Pauker SG, Sox HC, Tversky A. On the elicitation of preferences for alternative therapies. N Engl J Med. 1982;306:1259–62. doi: 10.1056/NEJM198205273062103. [DOI] [PubMed] [Google Scholar]
- 11.Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ. 2002;324:827–30. doi: 10.1136/bmj.324.7341.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jarlais DC, Sloboda Z, Friedman SR, Tempalski B, McKnight C, Braine N. Diffusion of the D.A.R.E. and syringe exchange programs. Am J Public Health. 2006;96:1354–58. doi: 10.2105/AJPH.2004.060152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rothman AJ, Martino SC, Bedell BT, Detweiler JB, Salovey P. The systematic influence of gain- and loss-framed messages on interest in and use of different types of health behavior. Pers Soc Psychol Bull. 1999;25:1355–69. doi: 10.1177/0146167299259003. [DOI] [Google Scholar]
- 14.Rothman AJ, Wlaschin JT, Bartels RD, Latimer A, Salovey P. How persons and situations regulate message framing effects: the study of health behavior. In: Eliot A, editor. Handbook of Approach and Avoidance Motivation. Mahwah, NJ: LEA; 2008. pp. 475–86. [Google Scholar]
- 15.Rothman AJ, Bartels RD, Wlaschin J, Salovey P. The strategic use of gain- and loss-framed messages to promote healthy behavior: how theory can inform practice. J Commun. 2006;56:S202–20. doi: 10.1111/j.1460-2466.2006.00290.x. [DOI] [Google Scholar]
- 16.Jones LW, Sinclair RC, Courneya KS. The effects of source credibility and message framing on exercise intentions, behaviors, and attitudes: an integration of the elaboration likelihood model and Prospect Theory. J Appl Soc Psychol. 2003;33:179–96. doi: 10.1111/j.1559-1816.2003.tb02078.x. [DOI] [Google Scholar]
- 17.Gerend MA, Cullen M. Effects of message framing and temporal context on college student drinking behavior. J Exp Soc Psychol. 2008;44:1167–73. doi: 10.1016/j.jesp.2008.02.007. [DOI] [Google Scholar]
- 18.Christophersen ER, Gyulay JE. Parental compliance with car seat usage: a positive approach with long term follow-up. J Pediatr Psychol. 1981;6:301–12. doi: 10.1093/jpepsy/6.3.301. [DOI] [PubMed] [Google Scholar]
- 19.Treiber FA. A comparison of positive and negative consequences approaches upon car restraint usage. J Pediatr Psychol. 1986;11:15–24. doi: 10.1093/jpepsy/11.1.15. [DOI] [PubMed] [Google Scholar]
- 20.Rothman AJ, Salovey P, Antone C, Keough K, Martin C. The influence of message framing on health behavior. J Exp Soc Psychol. 1993;29:408–33. doi: 10.1006/jesp.1993.1019. [DOI] [Google Scholar]
- 21.Detweiler JB, Bedell BT, Salovey P, Pronin E, Rothman AJ. Message framing and sunscreen use: gain-framed messages motivate beach-goers. Health Psychol. 1999;18:189–96. doi: 10.1037/0278-6133.18.2.189. [DOI] [PubMed] [Google Scholar]
- 22.Linville PW, Fischer GW, Fischhoff B. AIDS risk perceptions and decision biases. In: Pryor JB, Reeder GD, editors. The Social Psychology of HIV Infection. Hillsdale, NJ: Erlbaum; 1993. pp. 421–432. [Google Scholar]
- 23.Meyerowitz BE, Chaiken S. The effect of message framing on breast self-examination attitudes, intentions, and behavior. J Pers Soc Psychol. 1987;52:500–10. doi: 10.1037/0022-3514.52.3.500. [DOI] [PubMed] [Google Scholar]
- 24.Williams T, Clarke V, Borland R. Effects of message framing on breast-cancer-related beliefs and behaviors: the role of mediating factors. J Appl Soc Psychol. 2001;31:925–50. doi: 10.1111/j.1559-1816.2001.tb02656.x. [DOI] [Google Scholar]
- 25.Abood DA, Black DR, Coster DC. Loss-framed minimal intervention increases mammography use. Womens Health Issues. 2005;15:258–64. doi: 10.1016/j.whi.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 26.Abood DA, Coster DC, Mullis AK, Black DR. Evaluation of a “loss-framed” minimal intervention to increase mammography utilization among medically un- and under-insured women. Cancer Detect Prev. 2002;26:394–400. doi: 10.1016/S0361-090X(02)00120-4. [DOI] [PubMed] [Google Scholar]
- 27.Banks SM, Salovey P, Greener S, et al. The effects of message framing on mammography utilization. Health Psychol. 1995;14:178–84. doi: 10.1037/0278-6133.14.2.178. [DOI] [PubMed] [Google Scholar]
- 28.Cox D, Cox AD. Communicating the consequences of early detection: the role of evidence and framing. J Marketing. 2001;65:91–103. doi: 10.1509/jmkg.65.3.91.18336. [DOI] [Google Scholar]
- 29.Finney LJ, Iannotti RJ. Message framing and mammography screening: a theory-driven intervention. Behav Med. 2002;28:5–14. doi: 10.1080/08964280209596393. [DOI] [PubMed] [Google Scholar]
- 30.Schneider TR, Salovey P, Apanovitch AM, et al. The effects of message framing and ethnic targeting on mammography use among low-income women. Health Psychol. 2001;20:256–66. doi: 10.1037/0278-6133.20.4.256. [DOI] [PubMed] [Google Scholar]
- 31.Maheswaran D, Meyers-Levy J. The influence of message framing and issue involvement. J Marketing Res. 1990;27:361–7. doi: 10.2307/3172593. [DOI] [Google Scholar]
- 32.Apanovitch AM, McCarthy D, Salovey P. Using message framing to motivate HIV testing among low-income, ethnic minority women. Health Psychol. 2003;22:60–7. doi: 10.1037/0278-6133.22.1.60. [DOI] [PubMed] [Google Scholar]
- 33.Kalichman SC, Coley B. Context framing to enhance HIV-antibody-testing messages targeted to African American women. Health Psychol. 1995;14:247–54. doi: 10.1037/0278-6133.14.3.247. [DOI] [PubMed] [Google Scholar]
- 34.Block LG, Keller PA. When to accentuate the negative: the effects of perceived efficacy and message framing on intentions to perform a health-related behavior. J Marketing Res. 1995;32:192–203. doi: 10.2307/3152047. [DOI] [Google Scholar]
- 35.Marteau TM. Framing of information: its influence upon decisions of doctors and patients. Br J Soc Psychol. 1989;28:89–94. doi: 10.1111/j.2044-8309.1989.tb00849.x. [DOI] [PubMed] [Google Scholar]
- 36.Haward MF, Murphy RO, Lorenz JM. Message framing and perinatal decisions. Pediatrics. 2008;122:109–118. doi: 10.1542/peds.2007-0620. [DOI] [PubMed] [Google Scholar]
- 37.Wilson DK, Kaplan RM, Schneiderman LJ. Framing of decisions and selections of alternatives in health care. Soc Behav. 1987;2:51–9. [Google Scholar]
- 38.Levin IP, Schnittjer SK, Thee SL. Information framing effects in social and personal decisions. J Exp Soc Psychol. 1988;24:520–9. doi: 10.1016/0022-1031(88)90050-9. [DOI] [Google Scholar]
- 39.Mann TL, Sherman DK, Updegraff JA. Dispositional motivations and message framing: a test of the congruency hypothesis in college students. Health Psychol. 2004;23:330–4. doi: 10.1037/0278-6133.23.3.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sherman DK, Updegraff JA, Mann T. Improving oral health behavior. J Am Dent Assoc. 2008;139:1382–7. doi: 10.14219/jada.archive.2008.0050. [DOI] [PubMed] [Google Scholar]
- 41.Latimer AE, Rivers SE, Rench TA, et al. A field experiment testing the utility of regulatory fit messages for promoting physical activity. J Exp Soc Psychol. 2008;44:826–32. doi: 10.1016/j.jesp.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Armstrong K, Schwartz JS, Fitzgerald G, Putt M, Ubel PA. Effect of framing as gain versus loss on understanding and hypothetical treatment choices: survival and mortality curves. Med Decis Making. 2002;22:76–83. doi: 10.1177/0272989X0202200108. [DOI] [PubMed] [Google Scholar]
- 43.Ancker JS, Kaufman D. Rethinking health numeracy: a multidisciplinary literature review. J Am Med Inform Assoc. 2007;14:713–21. doi: 10.1197/jamia.M2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reyna VR, Nelson WL, Han P, Dieckmann NF. How numeracy influences risk comprehension and medical decision making. Psychol Bull. 2009;135:943–73. doi: 10.1037/a0017327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Galesic M, Garcia-Retamero R. Statistical numeracy for health: A cross-cultural comparison with probabilistic national samples. Arch Intern Med. 2010;170:462–8. doi: 10.1001/archinternmed.2009.481. [DOI] [PubMed] [Google Scholar]
- 46.Fagerlin A, Ubel PA, Smith DM, Zikmund-Fisher BJ. Making numbers matter: present and future research in risk communication. Am J Health Behav. 2007;31:47–56. doi: 10.5555/ajhb.2007.31.supp.S47. [DOI] [PubMed] [Google Scholar]
- 47.Peters E, Västfjäll D, Slovic P, Mertz CK, Mazzocco K, Dickert S. Numeracy and decision making. Psychol Sci. 2006;17:407–13. doi: 10.1111/j.1467-9280.2006.01720.x. [DOI] [PubMed] [Google Scholar]
- 48.Lerman C, Ross E, Boyce A, et al. The impact of mailing psychoeducational materials to women with abnormal mammograms. Am J Public Health. 1992;82:729–30. doi: 10.2105/AJPH.82.5.729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cormier O’Connor AM, Boyd NF, Tritchler DL, Kriukov Y, Sutherland H, Till JE. Eliciting preferences for alternative cancer drug treatments: the influence of framing, medium, and rater variables. Med Decis Making. 1985;5:453–63. doi: 10.1177/0272989X8500500408. [DOI] [PubMed] [Google Scholar]
- 50.Llewellyn-Thomas HA, McGreal MJ, Thiel EC. Cancer patients’ decision making and trial-entry preferences: the effects of “framing” information about short-term toxicity and long-term survival. Med Decis Making. 1995;15:4–12. doi: 10.1177/0272989X9501500103. [DOI] [PubMed] [Google Scholar]
- 51.O’Connor AM, Pennie RA, Dales RE. Framing effects on expectations, decisions, and side effects experienced: the case of influenza immunization [published erratum appears in J Clin Epidemiol. 1997;50:747−8] J Clin Epidemiol. 1996;49:1271–6. doi: 10.1016/S0895-4356(96)00177-1. [DOI] [PubMed] [Google Scholar]
- 52.Siminoff LA, Fetting JH. Effects of outcome framing on treatment decisions in the real world: impact of framing on adjuvant breast cancer decisions. Med Decis Making. 1989;9:262–71. doi: 10.1177/0272989X8900900406. [DOI] [PubMed] [Google Scholar]
- 53.Steffen VJ, Sternberg L, Teegarden LA, Shepherd K. Practice and persuasive frame: effects on beliefs, intention, and performance of a cancer self-examination. J Appl Soc Psychol. 1994;24:897–925. doi: 10.1111/j.1559-1816.1994.tb02365.x. [DOI] [Google Scholar]
- 54.Tykocinski OE, Higgins T, Chaiken S. Message framing, self-discrepancies, and yielding to persuasive messages: the motivational significance of psychological situations. Pers Soc Psychol Bull. 1994;20:107–15. doi: 10.1177/0146167294201011. [DOI] [Google Scholar]
- 55.O’Keefe DJ, Jensen JD. The relative persuasiveness of gain-framed and loss-framed messages for encouraging disease prevention behaviors: a meta-analytic review. J Health Commun. 2007;12:623–44. doi: 10.1080/10810730701615198. [DOI] [PubMed] [Google Scholar]
- 56.O’Keefe DJ, Jensen JD. The relative persuasiveness of gain-framed and loss-framed messages for encouraging disease detection behaviors: a meta-analytic review. J Commun. 2009;59:296–316. doi: 10.1111/j.1460-2466.2009.01417.x. [DOI] [PubMed] [Google Scholar]
- 57.Edwards AGK, Pill RM, Stott NCH. Communicating risk: use of standard terms is unlikely to result in standard communication. BMJ. 1996;313:1483. doi: 10.1136/bmj.313.7070.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Redelmeier DA. The cognitive psychology of missed diagnoses. Ann Intern Med. 2005;142:115–20. doi: 10.7326/0003-4819-142-2-200501180-00010. [DOI] [PubMed] [Google Scholar]
- 59.Almashat S, Ayotte B, Edelstein B, Margrett J. Framing effect debiasing in medical decision making. Patient Educ Couns. 2008;71:102–7. doi: 10.1016/j.pec.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 60.Ancker JS, Senathirajah Y, Kukafka R, Starren JB. Design features of graphs in health risk communication: a systematic review. J Am Med Inform Assoc. 2006;13:608–18. doi: 10.1197/jamia.M2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Galesic M, Garcia-Retamero R, Gigerenzer G. Using icon arrays to communicate medical risks: overcoming low numeracy. Health Psychol. 2009;28:210–6. doi: 10.1037/a0014474. [DOI] [PubMed] [Google Scholar]
- 62.Galesic M, Garcia-Retamero R. Graph literacy: a cross-cultural comparison. Med Decis Making, in press, doi:10.1177/0272989X10373805. [DOI] [PubMed]
- 63.Lipkus IM. Numeric, verbal, and visual formats of conveying health risks: suggested best practices and future recommendations. Med Decis Making. 2007;27:696–713. doi: 10.1177/0272989X07307271. [DOI] [PubMed] [Google Scholar]
- 64.Lipkus IM, Hollands JG. The visual communication of risk. J Natl Cancer Inst Monogr. 1999;25:149–63. doi: 10.1093/oxfordjournals.jncimonographs.a024191. [DOI] [PubMed] [Google Scholar]
- 65.Paling J. Strategies to help patients understand risks. BMJ. 2003;327:745–8. doi: 10.1136/bmj.327.7417.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Volk RJ, Spann SJ. Decision-aids for prostate cancer screening. J Fam Pract. 2000;49:425–7. [PubMed] [Google Scholar]
- 67.Timmermans DRM, Ockhuysen-Vermey CF, Henneman L. Presenting health risk information in different formats: the effect on participants’ cognitive and emotional evaluation and decisions. Patient Educ Couns. 2008;73:443–7. doi: 10.1016/j.pec.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 68.Waters EA, Weinstein ND, Colditz GA, Emmons KM. Reducing aversion to side effects in preventive medical treatment decisions. J Exp Psychol Appl. 2007;13:11–21. doi: 10.1037/1076-898X.13.1.11. [DOI] [PubMed] [Google Scholar]
- 69.Fagerlin A, Wang C, Ubel PA. Reducing the influence of anecdotal reasoning on people’s health care decisions: is a picture worth a thousand statistics? Med Decis Making. 2005;25:398–405. doi: 10.1177/0272989X05278931. [DOI] [PubMed] [Google Scholar]
- 70.Garcia-Retamero R, Galesic M. Communicating treatment risk reduction to people with low numeracy skills: A cross-cultural comparison. Am J Public Health. 2009;99:2196–202. doi: 10.2105/AJPH.2009.160234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Garcia-Retamero R, Galesic M, Gigerenzer G. Do icon arrays help reduce denominator neglect? Med Decis Making, in press. doi:10.1177/0272989X10369000. [DOI] [PubMed]
- 72.Goodyear-Smith F, Arroll B, Chan L, Jackson R, Wells S, Kenealy T. Patients prefer pictures to numbers to express cardiovascular benefit from treatment. Ann Fam Med. 2008;6:213–7. doi: 10.1370/afm.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Garcia-Retamero R, Galesic M, Gigerenzer G. Enhancing understanding and recall of quantitative information about medical risks: a cross-cultural comparison between Germany and Spain. Spanish J Psychol. in press. [DOI] [PubMed]
- 74.Schirillo JA, Stone ER. The greater ability of graphical versus numerical displays to increase risk avoidance involves a common mechanism. Risk Anal. 2005;25:555–66. doi: 10.1111/j.1539-6924.2005.00624.x. [DOI] [PubMed] [Google Scholar]
- 75.Garcia-Retamero R, Galesic M. Who profits from visual aids: overcoming challenges in people’s understanding of risks. Soc Sci Med. 2010;70:1019–25. doi: 10.1016/j.socscimed.2009.11.031. [DOI] [PubMed] [Google Scholar]
- 76.Hawley ST, Zikmund-Fisher B, Ubel P, Jancovic A, Lucas T, Fagerlin A. The impact of the format of graphical representation on health-related knowledge and treatment choices. Patient Educ Couns. 2008;73:448–55. doi: 10.1016/j.pec.2008.07.023. [DOI] [PubMed] [Google Scholar]
- 77.Baker L, Wagner TH, Singer S, Bundorf MK. Use of the Internet and e-mail for health care information: results from a national survey. JAMA. 2003;289:2400–6. doi: 10.1001/jama.289.18.2400. [DOI] [PubMed] [Google Scholar]
- 78.Jacoby WG. Value choices and American public opinion. Am J Pol Sci. 2006;50:706–23. doi: 10.1111/j.1540-5907.2006.00211.x. [DOI] [Google Scholar]
- 79.Lerner JS, Gonzalez RM, Small DA, Fischoff B. Effects of fear and anger on perceived risks of terrorism: a national field experiment. Psychol Sci. 2003;14:144–50. doi: 10.1111/1467-9280.01433. [DOI] [PubMed] [Google Scholar]
- 80.Miller JD, Scott EC, Okamoto S. Public acceptance of evolution. Science. 2006;313:765–6. doi: 10.1126/science.1126746. [DOI] [PubMed] [Google Scholar]
- 81.Schlenger WE, Caddell JM, Ebert L, et al. Psychological reactions to terrorist attacks: findings from the national study of Americans’ reactions to September 11. JAMA. 2002;288:581–8. doi: 10.1001/jama.288.5.581. [DOI] [PubMed] [Google Scholar]
- 82.Chang L, Krosnick JA. National surveys via RDD telephone interviewing versus the Internet: comparing sample representativeness and response quality. Public Opin Q. 2009;73:641–8. doi: 10.1093/poq/nfp075. [DOI] [Google Scholar]
- 83.Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127:966–72. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 84.Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- 85.Schwartz LM, Woloshin S, Welch G. Can patients interpret health information? An assessment of the medical data interpretation test. Med Decis Making. 2005;25:290–300. doi: 10.1177/0272989X05276860. [DOI] [PubMed] [Google Scholar]
- 86.Stone ER, Yates JF, Parker AM. Effects of numerical and graphical displays on professed risk-taking behavior. J Exp Psychol Appl. 1997;3:243–56. doi: 10.1037/1076-898X.3.4.243. [DOI] [Google Scholar]
- 87.Woloshin S, Schwartz LM, Black WC, Welch HG. Women’s perceptions of breast cancer risk: how you ask matters. Med Decis Making. 1999;19:221–9. doi: 10.1177/0272989X9901900301. [DOI] [PubMed] [Google Scholar]
- 88.Davids SL, Schapira MM, McAuliffe TL, Nattinger AB. Predictors of pessimistic breast cancer risk perceptions in a primary care population. J Gen Intern Med. 2004;19:310–5. doi: 10.1111/j.1525-1497.2004.20801.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Reyna VF, Brainerd CJ. The importance of mathematics in health and human judgment: numeracy, risk communication, and medical decision making. Learn Individ Differ. 2007;17:147–59. doi: 10.1016/j.lindif.2007.03.010. [DOI] [Google Scholar]
- 90.Reyna VF, Brainerd CJ. Numeracy, ratio bias, and denominator neglect in judgments of risk and probability. Learn Individ Differ. 2008;18:89–107. doi: 10.1016/j.lindif.2007.03.011. [DOI] [Google Scholar]
- 91.Garcia-Retamero R, Heuristics GM. In: The Encyclopedia of Medical Decision Making. Kattan MW, editor. Thousand Oaks, CA: SAGE; 2009. pp. 596–9. [Google Scholar]
- 92.Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S. Helping doctors and patients make sense of health statistics. Psychol Sci Public Interest. 2008;8:53–96. doi: 10.1111/j.1539-6053.2008.00033.x. [DOI] [PubMed] [Google Scholar]
- 93.Gigerenzer G, Hoffrage U. How to improve Bayesian reasoning without instruction: frequency formats. Psychol Rev. 1995;102:684–704. doi: 10.1037/0033-295X.102.4.684. [DOI] [Google Scholar]
- 94.Covey JA. Meta-analysis of the effects of presenting treatment benefits in different formats. Med Decis Making. 2007;27:638–54. doi: 10.1177/0272989X07306783. [DOI] [PubMed] [Google Scholar]
- 95.Gigerenzer G, Hertwig R, Broek E, Fasolo B, Katsikopoulos K. “A 30% chance of rain tomorrow”: How does the public understand probabilistic weather forecasts? Risk Anal. 2005;25:623–9. doi: 10.1111/j.1539-6924.2005.00608.x. [DOI] [PubMed] [Google Scholar]
- 96.Reyna VF, Brainerd CJ. Fuzzy-trace theory and framing effects in choice: gist extraction, truncation, and conversion. J Behav Decis Making. 1991;4:249–62. doi: 10.1002/bdm.3960040403. [DOI] [Google Scholar]
- 97.Garcia-Retamero R, Cokely E. Effective communication of risks to young adults: using message framing and visual aids to increase condom use and STD screening. Manuscript under review. [DOI] [PubMed]
- 98.Levin IP, Schneider SL, Gaeth GJ. All frames are not created equal: a typology and critical analysis of framing effects. Organ Behav Hum Decis Process. 1998;76:149–88. doi: 10.1006/obhd.1998.2804. [DOI] [PubMed] [Google Scholar]
- 99.Bruine W, Fischhoff B. The effect of question format on measured HIV/AIDS knowledge: detention center teens, high school students, and adults. AIDS Educ Prev. 2000;12:187–98. [PubMed] [Google Scholar]
- 100.Hsee CK, Weber EU. A fundamental prediction error: self-other discrepancies in risk preference. J Exp Psych. 1997;126:45–53. [Google Scholar]