The authors show in their young multidisciplinary program that time from referral to evaluation, evaluation by appropriate specialists, satisfaction scoring and accessibility to clinic trials all were affected favorably by the development of two multidisciplinary clinics.
Abstract
Multidisciplinary care refers to a practice in which physicians from multiple specialties attend to the same patient population. There are many advantages to the model, including reduced time to treatment, coordinated treatment plans, increased patient and physician satisfaction, and increased enrollment onto clinical trials. At Central Dupage Hospital, multidisciplinary clinics have been instituted in lung and gynecologic cancer. We describe the structure and operation of each clinic and highlight their considerable success in improving patient care.
Introduction
A multidisciplinary approach to care refers to caring for a patient through the work of multiple practitioners, and creating a consolidated plan that includes the recommendations of all. The most important reason to do a multidisciplinary clinic is that many people working together my reach more intelligent solutions than an individual working alone.
Other reasons for multidisciplinary care include the following:
Decrease the time from presentation to treatment.
Decrease fragmentation, with better communication, decreased errors and duplicate tests, and clarified treatment plan.
Decrease variability between physicians, ensuring application of good clinical practice.
Increase patient satisfaction through fewer visits and consistent communication.
Enable doctors to focus on multiple aspects of a patients care (socio-emotional, nutrition, etc).
Decrease medico-legal risk.
Improve quality of life.
Foster the setting wherein complex treatment plans can be created and sustained.
Increase enrollment in research studies.
Improve the education and support of family members.
Provide a marketable service for an institution.
Create a unique experience for graduate medical education.
Decrease the number of procedures needed to make a diagnosis.
Align programs.
Improve survival.
The Multidisciplinary Concept: Data for Utility
One of the clearest reasons, and simplest to define, for multidisciplinary cancer care is the failure to diagnose or delay in diagnosis (medico-legal risk). Studies have shown that time from presentation to treatment can range from 68 to 203 days without multidisciplinary care.1–3 Some of the reasons for this delay have been reliance on chest x-ray for diagnosis, false-negative biopsy, patient refusal to follow up, comorbidities, waiting times for tests, and too little detail regarding follow-up.4–6 In an analysis of lung cancer malpractice cases, the vast majority of cases were initiated in response to failure to diagnose, not the treatment plan.7 Most breast cancer misdiagnoses are based on a triad of error: young patients, self-discovered breast masses, and negative mammograms.8,9 Another review that found diagnostic errors were due to failure to order the appropriate test, failure to create a follow-up plan, failure to do adequate history and physical, and incorrect interpretation of tests.10 A multidisciplinary team can decrease the time to both diagnosis and treatment, as well as increase accuracy of diagnosis.
Another reason for multidisciplinary care is that many cancers involve complex treatment plans that require extensive discussions between specialists in real time. Cancers that have been studied in this regard include head and neck cancer, GI cancers, and sarcomas, all of which show improved outcomes in the multidisciplinary setting.11–14 Survivorship also thrives under multidisciplinary care, which increases clinical efficiency and promotes seamless care.15
Improvement in communication is a clear need that can be fulfilled by means of a multidisciplinary approach. Problems identified in a physician survey of traditional interphysician communication were physician dissatisfaction with the referral process, lack of timeliness, and inadequate referral letter content.16 Another study, which looked at having a radiologist as part of a multidisciplinary clinic, found that the presence of a radiologist improved interpretation and patient care.17
Communication between the physician and the patient can also improve in a multidisciplinary clinic setting. A study has cited communication breakdown between patient and physician as a cause of litigation in 80% of lawsuits.18 For follow-up of test results, a study demonstrated that only 64% of patients with abnormal mammograms had appropriate follow-up, as a result of improper documentation or communication.19
Proven Benefits of a Multidisciplinary Clinic
Patient Satisfaction
Prospectively, patients prefer a one-stop diagnostic clinic rather than a multiple-visit approach.20 A comparison of breast cancer patients who were seen in a traditional setting with those seen in a multidisciplinary setting showed a statistically significant improvement in satisfaction scores among those who had received multidisciplinary care.21 Improvement in satisfaction has been associated with the increased psychosocial support and involvement of patient and family in treatment decisions, as found in a multidisciplinary clinic.22,23
Increased Accuracy of Care
A study found that the radiographic review by the multidisciplinary radiologist found additional abnormalities in 23% of cases.24
Alterations in the treatment plan are seen with regularity in multidisciplinary clinics. Multidisciplinary discussion resulted in alterations of treatment plan for 53 of 153 patients, in 52% of breast cancer presurgical cases, in 43% of second opinions, and in another study in 24% of patients.25–29 Multidisciplinary settings also enable practitioners to increase the number of patients with lung cancer who are treated with curative intent,30 and to more appropriately select patients best suited for palliative strategy.31
An analysis of the reasons for treatment decision change found that comorbidity, patient choice, new information, and doctor discretion all caused changes in treatment plans in a multidisciplinary setting.32
Improved Survival
Some studies have shown improvements in survival rates in multidisciplinary clinics compared with rates in traditional treatment, but these improvement do not occur in the same time frame. Many studies compare multidisciplinary clinics to historical controls. A brain tumor multidisciplinary clinic found that patients enrolled in the clinic had a survival time of 18.7 months compared with 11.9 months for patients in traditional treatment.33 Survival benefit in multidisciplinary care for breast cancer can be related to the presence of a surgeon as part of the team.34 A colorectal study found that survival improved from 58% to 66% as a result of more adjuvant chemotherapy in the multidisciplinary clinic.35
Decreased Time to Treatment
A pilot program for lung lesions compared patients in a rapid diagnosis clinic with those in a conventional clinic and found that time to treatment decreased by 4 weeks in the rapid diagnosis clinic.36 A French study found improvements in time to treat with multidisciplinary lung cancer care,37 as did another study.38 A breast cancer study found that multidisciplinary care reduced the time from diagnosis to treatment from 42.2 to 29.6 days.23
Quality of Life
Quality of life can be well addressed by a multidisciplinary approach to palliative care.39 A randomized study of multidisciplinary versus standard intervention showed that patients who received multidisciplinary care maintained their quality of life during treatment; those with standard treatment had their quality of life worsen.40 This was especially prevalent in the geriatric population, in which patients appeared to benefit from the social worker intervention.41,42
In lung cancer, patients who received interdisciplinary care had better improvements in pain and fatigue.39 A head-to-head trial that compared standard care with multidisciplinary care showed better symptom control and satisfaction with the multidisciplinary approach.43 Another study found improvement in dyspnea, anxiety, and spiritual well-being with a multidisciplinary approach.44
Graduate Medical Education and Research
Multidisciplinary tumor boards have been shown to enhance graduate medical education by providing a unique experience not seen in the typical residency and fellowship.25 One study found that they enrolled 29% more patients with the use of a multidisciplinary clinic.29
Decreased Variability
One study demonstrated that the multidisciplinary lung cancer group strongly adhered to national guidelines.38 Another study found that patients treated by a non-lung cancer specialist received less lung-specific therapy.45
An Introduction to Our Program
Central Dupage Hospital (CDH) is located in the western suburbs of Chicago. Founded in 1964, it has grown into a tertiary care center with more than 900 staff physicians. Thus far, two multidisciplinary programs have been created at CDH. The two are actually quite different, with the lung program involving a rotation of patients between multiple different practices, and the gynecologic program using the same physicians at each clinic. They are both weekly live clinics where patients are discussed and seen by physicians, but that is the only similarity between the two. In the lung program, there are two codirectors, one of whom is a medical oncologist, and the other a pulmonologist. The clinics are staffed in the areas of medical oncology, radiation oncology, pulmonary, interventional pulmonary, cardiothoracic surgery, interventional radiology, and pain and palliative care. They are also staffed by advance practice nurses who provide navigation services and patient education, staff nurses, social workers, nutritionists, research staff, and pharmacists. The participating physicians come from different practices within CDH. Medical oncology, for example, includes an academic outreach group and a private practice group. A rotating calendar was set up from initiation, which also has paired physicians along the lines of their typical referral patterns. Each week, a different doctor from a different practice staffs the clinic, and each physician is assigned to a clinic on a biweekly, monthly, or every other month basis, depending on the number of physicians in the specialty who staff the clinic. In gynecology, the clinic is staffed by the same gynecologic oncologist, medical oncologist, and radiation oncologist every week. The three are all from different practices.
In terms of the structure of the actual clinic day, the two clinics are also very different. In the lung clinic, all patients arrive within a 30-minute time frame. They are checked in at the front desk, escorted to rooms by the care tech, and undergo a medication reconciliation and symptom check by the nurse. While that process is occurring, the physicians and other staff meet in a 1-hour multidisciplinary tumor board, at which a case overview, radiology, and pathology are presented and a tentative plan is discussed. The opinions of multiple medical oncologists, radiation oncologists, pulmonologists, cardiothoracic surgeons, and the palliative care team are all solicited and discussed at this time. There have been multiple occasions in which the radiographic read has been changed as a result of this meeting, and opinions of treating physicians have also been changed.
After the board meeting, the physicians and staff of the day go to the clinic. The physicians go in one by one and see each patient. So, physician A sees patient number 1 while physician B sees patient number 2, and so on. The physicians then come together and have a final discussion about the cases in the conference room. During this time, the patients are seen by the ancillary staff, such as nutritionists and social workers. The navigators write up an official treatment plan, which lists the plan of each individual doctor in a cohesive format. The patient is given all contact numbers for physicians and staff. Then the patient goes to scheduling and all tests are scheduled. Patients who have not yet had a diagnostic procedure performed often go on to either interventional pulmonology or interventional radiology that same day to receive a diagnostic procedure.
Patients in follow-up are also seen in the lung clinic. For example, patients with stage IIIA lung cancer are often seen back in the clinic when they reach the point where they have completed neoadjuvant therapy and a surgical decision needs to be made. This is done to continue to facilitate complete discussion between the physicians and to get the opinions of the other physicians that make up the tumor board.
The gynecology clinic is entirely different in structure and function. First, the clinic is staffed by the same three physicians every week, with support provided by staff. The nurse navigator and medical oncologist review the clinic schedule a day in advance to determine whether all data are ready, screen patients according to which physician they need to see, and screen patients as potential research candidates. On the day of the clinic, patients check in at the front desk, are escorted to rooms by care technicians, undergo symptom check and medication reconciliation by nursing staff, and meet the nurse navigator. The physicians then rotate through the rooms, with the gynecologic oncologist seeing all patients first, the medical oncologist seeing patients second if needed, and the radiation oncologist being called in if appropriate. Ancillary staff such as the nutritionist, social worker, and research nurse then see the patient if needed. Patients are discussed by the physicians, and orders are written and given to the nurse, who guides the patient through scheduling. The nurse navigator also sees the patient at checkout and ensures that they have her contact information should issues arise that require communication with the clinic. Once an individual becomes a patient in the gynecology clinic, she remains there for treatment and follow-up. During chemotherapy, she may be seen outside of the clinic for toxicity and treatment visits. In comparison with the lung clinic, the gynecologic clinic tends to be a more intimate, closed setting, because of the needs of the patient population.
CDH supported this clinic initiative in multiple ways. First, administration dedicated staff to the organization of the clinics. Second, the nonphysician staff that attends the clinics (nursing, research, nutrition, social work, care technicians, schedulers, front desk staff) are all employees of CDH. Also, the clinic takes place on site in a hospital-owned space. The administration provides a marketing budget that supports production of a letter to referring physicians, letters to patients, brochures, and signage. Also, clinic personnel attended community outreach events and staffed booths that informed the public about the clinics. The physician leaders in the lung clinic gave a community presentation to the public explaining the value and workings of the clinic. For gynecology, a symposium on gynecologic cancers was given for the physicians and hospital staff. For both clinics, phone trees were created so patients could call the multidisciplinary clinic directly, and the patients were given a “lifeline,” the number to the nurse navigator for the clinic. The navigator was their link between testing, physician visits, and other issues, providing support and guidance.
With regard to billing, each physician bills as an individual consultant. Because the hospital provides the physicians with space and staff at no charge, this was felt to be fair and equitable. There was no physician resistance to the billing structure, but by nature a multidisciplinary clinic can be less efficient in terms of the number of patients seen in the amount of time the practitioner has available. We have worked on this issue by having continued follow-up meetings to discuss the workings of the clinics, and we continually adjust the model to achieve the highest standard of care. At our last meeting, for example, it was determined that we would be better served by having the nurse navigator complete the history on the patient and give it to the physicians in typed format before the clinic to streamline the process.
Data From the CDH Multidisciplinary Program
Lung Clinic
Time from initial referral to evaluation.
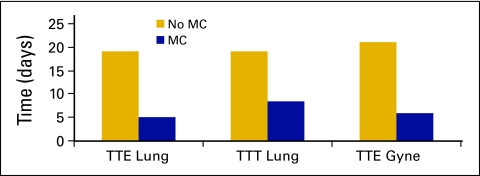
Previously, the primary delay in the workup and case management for lung cancer patients at CDH was prolonged time to be seen by a surgeon. With the development of the multidisciplinary lung clinic, the average time from initial phone call to evaluation by a chest surgeon and the entire team was reduced to 5 days. This was previously on the order of 2 to 3 weeks. The time to initial evaluation by medical oncology before initiation of the multidisciplinary clinic was 5 days (Fig 1).
Figure 1.
Multidisciplinary clinic (MC) improves speed of service. TTE, time to evaluation; TTT, time to treatment; Gyne, gynecologic.
Early referral to palliative care.
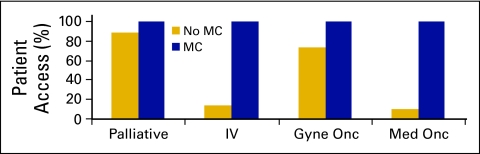
In the clinic, pain and palliative care staff, consisting of a board-certified physician in pain/palliative care and two nurses, are in attendance at all times. All patients who have a need for their services are seen by the palliative care team in the clinic. In contrast, before development of the clinic, 88% of lung cancer patients were seen by palliative care. Therefore the clinic has improved access to palliative services, which improves patient's quality of life (Fig 2).
Figure 2.
Multidisciplinary clinic (MC) expands access to specialty services. IV, seen by two interventional services; Gyne Onc, gynecologic oncology; Med Onc, medical oncology.
Involvement of interventional pulmonologist or radiologist.
The multidisciplinary clinic staff includes both an interventional radiologist and an interventional pulmonologist. Before development of the clinic, patients generally were reviewed by only one of these specialists, but not both (14% were reviewed by both). Now, all patients benefit from the opinion of both of these specialists in decisions regarding the type of procedure to be performed. This has been facilitated by having both specialists attend the tumor board to hear the case presentation. Then both discuss which type of procedure would be most suitable in making a diagnosis. For a simple example, a patient with a peripheral nodule is usually recommended for radiology, and a patient with central nodule for pulmonology. Both the radiologist and pulmonologist are on call for the day and perform procedures on the patients in clinic that day. Therefore the clinic has vastly increased the number of patients who benefit from a discussion between service lines as to which procedure would be best to perform (Fig 2).
Time to treatment.
Patients seen in the multidisciplinary lung clinic started their treatment in 8.5 days, on average. This treatment included surgery, radiation, or chemotherapy, whichever the first indicated treatment was. Before the creation of the clinic, average time to treatment for lung cancer was 19 days (Fig 1).
Gynecologic Cancer Clinic
Evaluation by appropriate specialists.
Before the multidisciplinary clinic, 73% of patients were evaluated by a gynecologic oncologist between 2006 and 2009 (56% in 2006, 84% in 2008). According to projections based on tumor board presentations and referral patterns, approximately 100% of appropriate patients have been seen by gynecologic oncology since inception of the clinic. With regard to medical oncology, 100% of appropriate patients have been seen since the inception of the multidisciplinary clinic, as compared with only 10% of such patients in the prior year (Fig 2).
Time from initial referral to evaluation.
The time from initial referral to initial visit in the gynecologic oncology clinic is 5.8 days on average. Before inception of the multidisciplinary clinic, the time to be seen was 21 days on average (Fig 1).
Percentage of Patients Screened for Research Studies
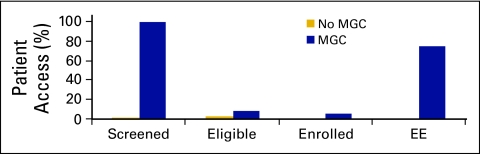
Of the patients seen in the multidisciplinary gynecologic oncology clinic, 100% were screened for clinical trials, and 8% were deemed eligible. Previously at CDH, approximately 1% of patients with gynecologic malignancies were screened for clinical trials, and no patients were enrolled onto clinical trials. After initiation of the multidisciplinary clinic, 75% of eligible patients were enrolled onto clinical trials (ie, 6% of the total case load). Clearly, the problem here is not whether we are screening or whether patients want to go on trials, the issue is having patients that fit the trials. The reason is initially we did not know which patients would be seen in the clinic. We had mostly ovarian cancer trials opened, but the majority of patients seen are uterine cancer patients. Therefore, we opened three uterine trials recently and hope to have better matches. It is encouraging to note that our enrollments have all been in the past 3 months. We are members of the Gynecologic Oncology Group and have opened their major trials. We also have three industry-funded trials open, and one investigator-initiated trial for gynecology. Overall, development of the clinic has dramatically expanded access to clinical trials for a population in need (Fig 3).
Figure 3.
The Multidisciplinary Gynecologic Clinic (MGC) expands patient access to clinical research trials. EE, percentage of eligible patients enrolled onto clinical trials.
Programmatic Issues
Improvement in Patient Satisfaction
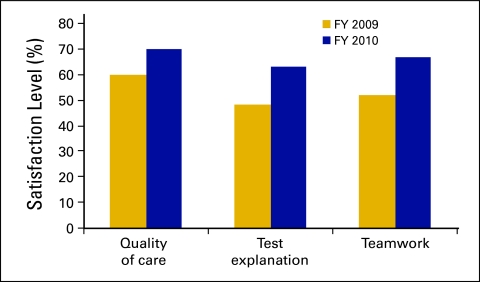
The oncology program conducts phone surveys with all patients who are seen for general clinic, infusion, and multidisciplinary clinic care. Surveys have shown improvement in key drivers: quality of care, explanation of tests, and teamwork (Fig 4). Part of this improvement is due to the institution of multidisciplinary clinics. We have received patient comments stating that they have found value in the success of the multidisciplinary clinic system in streamlining their care.
Figure 4.
Patient satisfaction. FY, fiscal year.
Presentation at Cancer Conferences
With the development of the multidisciplinary clinics, we found that presentation of cases at oncology conferences reached an all-time high. Lung cases were presented at 149% of previous annual levels. Of the annual caseload at CDH, 15% of the uterine cases were presented; before the advent of the multidisciplinary clinics, this rate was 0%. For our tumor board conferences, attendance by multidisciplinary clinic personnel was 95.5%, and 87.3% of cases were presented in prospective format—that is, before any treatment was initiated.
Practitioner Satisfaction
When surveyed, the practitioners in the lung cancer clinic did express concerns regarding efficiency and financial loss. This concern has been discussed in multiple initial and follow-up meetings. The concern has been minor as most of the physicians involved have been dedicated to the clinic and have put the needs of the clinic first. Also, each physician rotates through, so each is committing a half day per month, or even less frequently for some physicians (some are once every 2 months), thus reducing the commitment level. Another identified problem was that clinic physicians were repeating the same patient history and physical examinations. This problem has been addressed by having the APN navigator take the initial history, allowing for individual practitioners to take an abbreviated history and then perform a complete physical. On the positive side, practitioners expressed satisfaction with the level of communication, decrease in errors, and decrease in duplicative tests.
Summary
Overall, multidisciplinary clinics present a wealth of opportunities for patients and physicians in the private setting. We have shown in our young program that multiple factors, such as time from referral to evaluation, evaluation by appropriate specialists, satisfaction scoring, accessibility to clinic trials, and time from evaluation to treatment all were affected favorably by the development of two multidisciplinary clinics. We have been so enthused by this success that we are next moving to other disease sites to continue to advance the level of care in our hospital.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Laura Elise Horvath, Ileana Leyva, Marianne Huml, Christy Kesslering, Jeffrey Huml
Provision of study materials or patients: Laura Elise Horvath, Edgardo Yordan, Deepak Malhotra, Ileana Leyva, Marianne Huml
Collection and assemble of data: Laura Elise Horvath, Katy Bortel, Denise Schalk, Patricia Mellinger, Marianne Huml
Data analysis and interpretation: Laura Elise Horvath, Edgardo Yordan, Deepak Malhotra, Marianne Huml, Jeffrey Huml
Manuscript writing: Laura Elise Horvath
Final approval of manuscript: Laura Elise Horvath, Edgardo Yordan, Deepak Malhotra, Ileana Leyva, Katy Bortel, Denise Schalk, Patricia Mellinger, Marianne Huml, Christy Kesslering, Jeffrey Huml
References
- 1.Koyi H, eHillerdal G, Brandén E, et al. Patients' and doctors' delays in the diagnosis of chest tumors. Lung Cancer. 2002;35:53–537. doi: 10.1016/s0169-5002(01)00293-8. [DOI] [PubMed] [Google Scholar]
- 2.Billing JS, Wells FC, et al. Delays in the diagnosis and surgical treatment of lung cancer. Thorax. 1996;51:903–906. doi: 10.1136/thx.51.9.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salomaa ER, Sällinen S, Hiekkanen H, et al. Delays in the diagnosis and treatment of lung cancer. Chest. 2005;128:2282–2288. doi: 10.1378/chest.128.4.2282. [DOI] [PubMed] [Google Scholar]
- 4.Bjerager M, Palshof T, Dahl R, et al. Delay in diagnosis of lung cancer in general practice. Br J Gen Pract. 2006;56:863–868. [PMC free article] [PubMed] [Google Scholar]
- 5.Farag SS, Green MD, Morstyn G, et al. Delay by internists in obtaining diagnostic biopsies in patients with suspected cancer. Ann Intern Med. 1992;116:473–478. doi: 10.7326/0003-4819-116-6-473. [DOI] [PubMed] [Google Scholar]
- 6.Yoshimoto A, Tsuji H, Takazakura E, et al. Reasons for the delays in the definitive diagnosis of lung cancer for more than one year from the recognition of abnormal chest shadows. Inter Med. 2002;41:95–102. doi: 10.2169/internalmedicine.41.95. [DOI] [PubMed] [Google Scholar]
- 7.McLean TR. Why do physicians who treat lung cancer get sued? Chest. 2004;126:1672–1679. doi: 10.1378/chest.126.5.1672. [DOI] [PubMed] [Google Scholar]
- 8.Kern KA. The delayed diagnosis of breast cancer: Medico legal implications and risk prevention for surgeons. Breast. 2001;Dis12:145–158. doi: 10.3233/bd-2001-12115. [DOI] [PubMed] [Google Scholar]
- 9.Goodson WH, III, Moore DH., II Causes of physician delay in the diagnosis of breast cancerl. Arch Intern Med. 2002;162:1343–1348. doi: 10.1001/archinte.162.12.1343. [DOI] [PubMed] [Google Scholar]
- 10.Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnosis in the ambulatory setting: A study of closed malpractice claims. Ann Intern Med. 2006;145:488–496. doi: 10.7326/0003-4819-145-7-200610030-00006. [DOI] [PubMed] [Google Scholar]
- 11.Haddad R. Current and future directions in the treatment of squamous cell carcinoma of the head and neck: Multidisciplinary symposium on head and neck cancer. Expert Opin Ther Targets. 2006;10:333–336. doi: 10.1517/14728222.10.2.333. [DOI] [PubMed] [Google Scholar]
- 12.Adams R, Morgan M, Mukherjee S, et al. A prospective comparison of multidisciplinary treatment of oesophageal cancer with curative intent in a UK cancer network. Eur J Surg Oncol. 2007;33:307–313. doi: 10.1016/j.ejso.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 13.Shimoda M, Kubota K. Multi-disciplinary treatment for cholangiocellular carcinoma. World J Gastroenterol. 2007;13:1500–1504. doi: 10.3748/wjg.v13.i10.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ye YJ, Gao ZD, Poston GJ, et al. Diagnosis and multi-disciplinary management of hepatic metastases from gastrointestinal stromal tumour (GIST) Eur J Surg Oncol. 2009;35:787–792. doi: 10.1016/j.ejso.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 15.Carlson CA, Hobbie WL, Brogna M, et al. A multidisciplinary model of care for childhood cancer survivors with complex medical needs. J Pediatr Oncol Nurs. 2008;25:7–13. doi: 10.1177/1043454207311741. [DOI] [PubMed] [Google Scholar]
- 16.Gandhi TK, Sittig DF, Franklin M, et al. Communication breakdown in the outpatient referral process. J Gen Intern Med. 2000;15:626–631. doi: 10.1046/j.1525-1497.2000.91119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silverman SG, Khorasani R, Adams DF, et al. “Multidisciplinary gastrointestinal cancer clinic: Abdominal radiologist as active participant. Acad Radiol. 1998;5:694–697. doi: 10.1016/s1076-6332(98)80564-3. [DOI] [PubMed] [Google Scholar]
- 18.Levinson W. Physician-patient communication. A key to malpractice prevention. JAMA. 1994;272:1619–1620. [PubMed] [Google Scholar]
- 19.Poon EG, et al. Communication factors in the follow-up of abnormal mammograms. J Gen Intern Med. 2004;19:390–391. doi: 10.1111/j.1525-1497.2004.30357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Berry MG, Chan SY, Engledow A, et al. An audit of patient acceptance of one-stop diagnosis for symptomatic breast disease. Eur J Surg Oncol. 1998;24:492–495. doi: 10.1016/s0748-7983(98)93248-6. [DOI] [PubMed] [Google Scholar]
- 21.Frost MH, Arvizu RD, Jayakumar S, et al. A multidisciplinary healthcare delivery model for women with breast cancer: Patient satisfaction and physical and psychosocial adjustment. Oncol Nurs Forum. 1999;26:1673–1680. [PubMed] [Google Scholar]
- 22.Walker MS, Ristvedt SL, Haughey BH, et al. Patient care in multidisciplinary cancer clinics: Does attention to psychosocial needs predict patient satisfaction? Psycho-oncology. 2003;12:291–300. doi: 10.1002/pon.651. [DOI] [PubMed] [Google Scholar]
- 23.Gabel M, Hilton NE, Nathanson SD, et al. Multidisciplinary breast cancer clinics. Do they work? Cancer. 1997;79:2380–2384. [PubMed] [Google Scholar]
- 24.Singh J, Fairbairn KJ, Williams C, et al. Expert radiological review of skeletal surveys identifies additional abnormalities in 23% of cases: Further evidence for the value of myeloma multidisciplinary teams in the accurate staging and treatment of myeloma patients. Br J Haematol. 2007;137:172–173. doi: 10.1111/j.1365-2141.2007.06536.x. [DOI] [PubMed] [Google Scholar]
- 25.Gatcliffe TA, Coleman RL. Tumor board: More than treatment planning-a 1 year prospective survey. J Cancer Educ. 2008;23:235–237. doi: 10.1080/08858190802189014. [DOI] [PubMed] [Google Scholar]
- 26.Wright FC, De Vito C, Langer B, et al. Multidisciplinary cancer conferences: A systematic review and development of practice standards. Eur J Cancer. 2007;43:1002–1010. doi: 10.1016/j.ejca.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 27.Newman EA, Guest AB, Helvie MA, et al. Changes in surgical management resulting from case review at a breast cancer multidisciplinary tumor board. Cancer. 2006;107:2346–2351. doi: 10.1002/cncr.22266. [DOI] [PubMed] [Google Scholar]
- 28.Chang JH, Vines E, Bertsch H, et al. The impact of a multidisciplinary breast cancer center on recommendations for patient management: The University of Pennsylvania experience. Cancer. 2001;91:1231–1237. doi: 10.1002/1097-0142(20010401)91:7<1231::aid-cncr1123>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 29.Pawlik TM, Laheru D, Hruban RH, et al. Evaluating the impact of a single-day multidisciplinary clinic on the management of pancreatic cancer. Ann Surg Oncol. 2008;15:2081–2018. doi: 10.1245/s10434-008-9929-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coory M, Gkolia P, Yang IA, et al. Systematic review of multidisciplinary teams in the management of lung cancer. Lung Canc. 2008;60:14–21. doi: 10.1016/j.lungcan.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 31.Penel N, Grosjean J, Pichon-Watelle F, et al. Factors favouring palliative treatment multidisciplinary decisions for newly diagnosed visceral and soft tissue sarcomas. Clin Oncol. 2008;20:523–527. doi: 10.1016/j.clon.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 32.Wood JJ, Metcalife C, Paes A, et al. An evaluation of treatment decisions at a colorectal cancer multidisciplinary team. Colorectal Dis. 2008;10:769–72. doi: 10.1111/j.1463-1318.2007.01464.x. [DOI] [PubMed] [Google Scholar]
- 33.Back MF, Ang EL, Ng WH, et al. Improvements in quality of care resulting from a formal multidisciplinary tumour clinic in the management of high-grade gliomas. Ann Acad Med Singapore. 2007;36:347–351. [PubMed] [Google Scholar]
- 34.Houssami N, Sainsbury R. Breast cancer: Multidisciplinary care and clinical outcomes. Eur J Cancer. 2006;42:2480–2491. doi: 10.1016/j.ejca.2006.05.023. [DOI] [PubMed] [Google Scholar]
- 35.MacDermid E, Hooton G, MacDonald M, et al. Improving patient survival with the colorectal cancer multidisciplinary team. Colorectal Dis. 2009;11:291–295. doi: 10.1111/j.1463-1318.2008.01580.x. [DOI] [PubMed] [Google Scholar]
- 36.Murray PV, O'Brien ME, Sayer R, et al. The pathway study: Results of a pilot feasibility study in patients suspected of having lung carcinoma investigated in a conventional chest clinic setting compared to a centralized two-stop pathway. Lung Cancer. 2003;42:283–290. doi: 10.1016/s0169-5002(03)00358-1. [DOI] [PubMed] [Google Scholar]
- 37.Leo F, Venissac N, Poudenx M, et al. Multidisciplinary management of lung cancer: How to test its efficacy? J Thorac Oncol. 2007;2:69–72. doi: 10.1097/JTO.0b013e31802bff56. [DOI] [PubMed] [Google Scholar]
- 38.Conron M, Phuah S, Steinfort D, et al. Analysis of multidisciplinary lung cancer practice. Intern Med J. 2007;37:18–25. doi: 10.1111/j.1445-5994.2006.01237.x. [DOI] [PubMed] [Google Scholar]
- 39.Borneman T, Kocywas M, Cristea M, et al. An interdisciplinary care approach for integration of palliative care in lung cancer. Clin Lung Cancer. 2008;9:352–360. doi: 10.3816/CLC.2008.n.051. [DOI] [PubMed] [Google Scholar]
- 40.Rummans TA, Clark MM, Sloan JA, et al. Impacting quality of life for patients with advanced cancer with a structured multidisciplinary intervention: A randomized controlled trial. J Clin Oncol. 2006;24:635–642. doi: 10.1200/JCO.2006.06.209. [DOI] [PubMed] [Google Scholar]
- 41.Lapid MI, Rummans TA, Brown PD, et al. Improving the quality of life of geriatric cancer patients with a structured multidisciplinary intervention: A randomized controlled trial. Palliat Support Care. 2007;5:107–114. doi: 10.1017/s1478951507070174. [DOI] [PubMed] [Google Scholar]
- 42.Miller JJ, Frost MH, Rummans TA, et al. Role of a medical social worker in improving quality of life for patients with advanced cancer with a structured multidisciplinary intervention. J Psychosoc Oncol. 2007;25:105–119. doi: 10.1300/J077v25n04_07. [DOI] [PubMed] [Google Scholar]
- 43.Strasser F, Sweeney C, Willey J, et al. Impact of a half-day multidisciplinary symptom control and palliative care outpatient clinic in a comprehensive cancer center on recommendations, symptom intensity, and patient satisfaction: A retrospective descriptive study. J Pain Symptom Manage. 2004;27:481–491. doi: 10.1016/j.jpainsymman.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 44.Rabow MW, Dibble SL, Pantilat SZ, et al. The comprehensive care team: A controlled trial of outpatient palliative medicine consultation. Arch Intern Med. 2004;164:83–91. doi: 10.1001/archinte.164.1.83. [DOI] [PubMed] [Google Scholar]
- 45.Vinod SK, O'Connell DL, Simonella L, et al. Gaps in optimal care for lung cancer. J Thorac Oncol. 2008;3:871–879. doi: 10.1097/JTO.0b013e31818020c3. [DOI] [PubMed] [Google Scholar]