This Lung Cancer Multidisciplinary Clinic (MDC) included medical and radiation oncologists, a thoracic surgeon, and a pulmonologist and met every third week. Establishment of the clinic resulted in improvements in quality of care, patient satisfaction, and patient retention.
Abstract
A community cancer clinic, through cooperation with its parent health care system, developed a lung cancer multidisciplinary clinic (MDC) to enhance patient care and prevent out-migration to competing health care systems. The local medical and radiation oncologists collaborated with a thoracic surgeon from the tertiary care hospital in establishing the lung MDC. All the participating physicians are employed by the health care system. A cancer care coordinator assured that all necessary tests were obtained and available to the physicians at least 1 day before the clinic. The multidisciplinary team also included a pulmonologist and met every third week. Other sub-specialists were involved as necessary. Final treatment recommendations using National Comprehensive Cancer Network guidelines were made for each patient at the MDC visit. This clinic, once established, resulted in significant improvements in the quality of care, patient satisfaction and retention of patients. Time from diagnosis to initiation of treatment was reduced to a mean of 18 days from a mean of 24 days. The community cancer clinic had an increase in lung cancer patient care by 28% and a 9.1% increase in gross revenue. The tertiary care hospital benefited by providing all patients with definitive surgery, including minimally invasive surgery. The tertiary hospital thoracic surgeon had a 75% increase in referrals from the lung MDC geographic area over the previous year. This collaboration in the development of MDCs demonstrates how patients, caregivers, and the health care system benefit from MDCs.
Introduction
The increasing complexity of cancer diagnosis and treatment has resulted in establishment of multidisciplinary clinics (MDCs) across the country. A great deal of information on MDCs has been published, and most sites treating cancer publicize the use of MDCs, but little is published documenting the benefits of MDCs in cancer treatment. Lung cancer is an example of a disease in which affected persons benefit from multidisciplinary care. All professional disciplines are required for cancer diagnosis, treatment, supportive care, family and psychological support, and survivorship. Cancer of the lung and bronchus is the third most commonly diagnosed cancer in Wisconsin, following prostate and breast cancers.1 It is the leading cause of cancer-related death for both men and women in Wisconsin.1 Local disease can be cured with proper surgical intervention, but fewer than one third of patients present with localized disease. To provide the best care and improve survival, it is critical that nurses, pulmonologists, radiologists, medical oncologists, radiation oncologists, and surgeons formulate a unified, evidenced-based management plan.
A problem in the development of MDCs in nonacademic centers is the effective use of busy physicians who are compensated according to a work relative value units methodology and have concerns about travel and nonproductive time. We established a MDC in a community cancer clinic and measured the impact of the clinic on quality of care, patient satisfaction, patient loyalty, and financial performance.
Background and Methods
Aurora Sheboygan Medical Center is a full-service community hospital serving a predominantly rural county population of 114,561. It is part of a large integrated nonprofit health care system, Aurora Health Care, serving all of eastern Wisconsin through 14 acute care hospitals, including other regional and tertiary hospitals. Before implementation of the MDC, our integrated health system had 13 medical and radiation oncology sites located throughout eastern Wisconsin. For 3 years before cancer became a system service line focus, physicians from across the system would gather informally to share best practices and advance the integration of National Comprehensive Cancer Network (NCCN) guidelines2 at their local/regional sites. It was through these informal meetings that the Sheboygan medical and radiation oncologists, the Milwaukee-based thoracic surgeon, and the director of growth and market development for cancer began to strategize the development of the thoracic MDC.
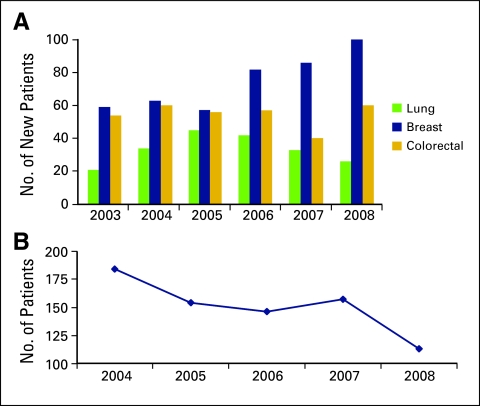
Internal analysis of the patient volume and care provided to patients with cancer identified a selective decrease in the number of patients with lung cancer being treated in the community hospital (Fig 1A). There appeared to be a 33% reduction of such patients from 2006 to 2008. Lung cancer incidence in Sheboygan County was reported as 333 cases between 2000 and 2004.1 On the basis of these data, we estimated that 32.8% of patients in Sheboygan County with a primary diagnosis of lung cancer leave the county for some or all aspects of their cancer care. Our data also suggest a higher proportion of patients with lung cancer leave the market compared with patients with other major cancer types (Figure 1B). On review, we identified that 77% of the patients with lung cancer in this market presented with stage III or IV disease, which requires multimodality treatment. The review also suggested that an MDC for lung cancer might be possible and the simplest solution. We concluded that there was an opportunity to improve care to patients with lung cancer and thereby permit some to be cared for closer to home.
Figure 1.
(A) Number of patients with cancer treated by year in the local hospital by cancer type before the implementation of the multidisciplinary clinic for lung cancer. (B) Lung cancer patients treated in the study geographic area.
Focused review indicated a community perception that the expertise was not available in Sheboygan County for comprehensive care of patients with lung cancer. A strategic plan was developed to establish a lung cancer MDC with dedicated staffing and expertise in lung cancer.
The objectives of the MDC were:
Use an evidence-based approach to the evaluation and treatment of lung cancer patients on the basis of NCCN guidelines.
Provide a setting in which more timely diagnosis and earlier intervention can occur.
Provide a prospective multidisciplinary approach to the diagnosis, staging, and treatment of lung cancer and provide evidence-based treatment recommendations to patients at the time of their MDC visit.
Use a cancer care coordinator to facilitate personalized patient/family navigation, education, and plan of care.
Local Sheboygan leadership was engaged in the planning process, as were their key physician stakeholders in pulmonology, primary care, and general surgery. Communication strategies included presentations at the Sheboygan Management Committee, local tumor board, and staff meetings. Electronic communications were also targeted toward the health system–employed physicians and key office staff, announcing the implementation of the MDC and process for referring patients. The Sheboygan breast care coordinator expanded her role to include care coordination of patients with primary or metastatic lung cancer. Scheduling and billing accountability stayed at the local level, with tracking of local and tertiary center metrics managed by the system cancer program via the growth and market development director The plan included tracking such metrics as impact on quality of care, patient satisfaction, physician satisfaction, retention of patients in the system, and revenue to determine the benefits of this MDC.
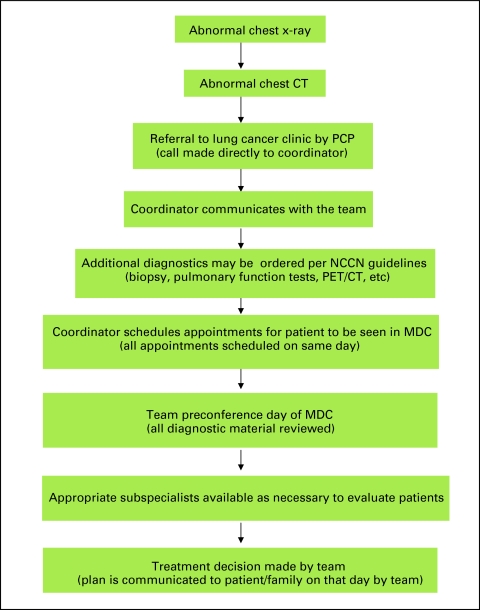
One of the physician champions for this MDC clinic was an expert in minimally invasive thoracic surgery with quality outcomes equal to or better than those benchmarked by the Society of Thoracic Surgeons (STS). The presence of this surgeon provided local specific lung cancer surgical expertise. The radiation oncologists and medical oncologists agreed to staff the MDC and adhere to NCCN guidelines, which ensure compliance with national treatment guidelines. Access to National Cancer Institute (NCI) cooperative clinical trials was also provided to patients in the MDC. The cancer care coordinator was identified to staff the clinic and communicate with patients/families and all medical providers, including the referring physician. The coordinator was a critical element in the success of the MDC. A patient pathway was developed (Fig 2) as part of the implementation plan for facilitating referral and decision making for nononcology primary care providers in this local market.
Figure 2.
Lung cancer multidisciplinary clinic (MDC) patient flow. CT, computed tomography; PCP, primary care provider; NCCN, National Comprehensive Cancer Network; PET, positron emission tomography.
Before the patient visit, the cancer care coordinator retrieves all the necessary diagnostic information then schedules a team conference. At the conference, all the participating physicians review the patient information. NCCN guidelines are reviewed, a preliminary treatment recommendation is developed, and the lead physician is identified. The lead physician, who performs the consultation with the patient/family and other specialists essential to care, meets with the patient at the same clinic visit. Patients are provided with clear, evidence-based treatment recommendations and are then able to make informed decisions, be referred for second opinions if requested, and start therapy. If surgery is part of the treatment plan, the thoracic surgeon who staffs the MDC performs surgery at the health system's tertiary hospital, which is located 60 miles away. The high-volume operating room and nursing support of the tertiary hospital support clinical outcomes that exceed the STS benchmarks for margins and length of stay (LOS), as well as minimize intensive care unit use. All other care, for example, postsurgery follow-up, chemotherapy, and radiation therapy, are given in the local community setting.
Metrics
Time to Treatment
The most striking improvement was the significant reduction of time from diagnosis to definitive treatment. The time from diagnosis (biopsy) to treatment was reduced to a mean of 18 days (range, 2 to 112 days) compared with a mean of 24 days (range, 2 to 81 days) before implementation of the MDC; the traditional benchmarks in the literature are 32.5 to 79.5 days.3–12
Retention of Patients
The patients who participated in the lung MDC reported extremely high satisfaction. Of the 46 patients that participated in the Lung MDC during the defined time period, 94% stayed within the system for their care, which compared favorable to 86% of the Sheboygan lung cancer patients that stayed in the system the year prior (2008). A critical element of the patient's satisfaction was seamless cancer care coordination that was facilitated by and between the local cancer care coordinator and the tertiary center lung cancer coordinator. The surgical staff of the system's tertiary center was completely informed about the patient status and background before the patient arrived for admission. All postoperative outpatient care was provided back in the local community. Because all the preoperative work-up was performed locally and all subsequent care provided locally, the patients were able to receive care in their own community. The overall mean for patient satisfaction of the Lung MDC was 98% “very satisfied,” on the basis of a simple eight-item questionnaire. Before implementation of the MDC, patient satisfaction of the care at the Sheboygan oncology clinic was reported at 95% “very satisfied” on a similar questionnaire.
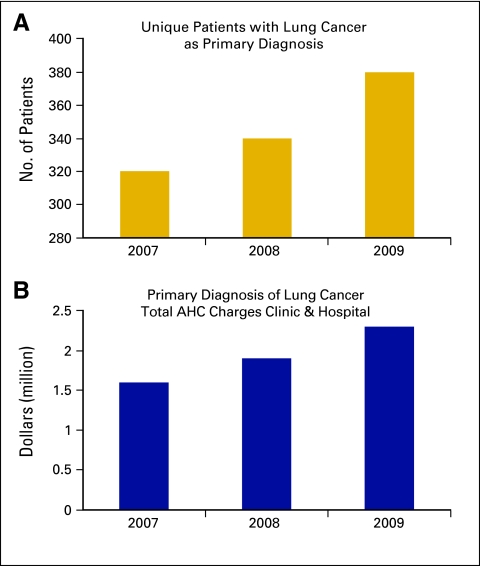
Financial Results
There appeared to be financial improvements locally. Although follow-up was short, there was an approximately 28% increase in care provided to the lung cancer patients and a 9.1% growth in gross revenue (Figs 3A and 3B) at the community based hospital. The health care system benefited by having in-system patient referral to the tertiary care center rather than to another system. The increase in local community health system revenues did not increase the overall health care expenditures to the patient. Rather, the revenue increase was due to retention of patients who would otherwise have migrated out of the system. Although not measured, this rapid work-up and therapy within an integrated health care system potentially avoided duplications of expensive testing or review of diagnostic biopsy material. This approach may have the potential to decrease health care expenses, and we plan to measure this impact in future analysis of MDCs.
Figure 3.
(A) Impact of MDC as measured by number of patients. (B) Volume of care provided as measured by charges. AHC, Aurora Health Care.
Clinical Quality
Possibly most important, the initial work-up met national guidelines, with no duplication of testing necessary because the medical records, pathology, imaging, and laboratory data were available to all sites of care. Work-up and all therapy were consistent with NCCN guidelines, and patients had access to clinical trials. Surgical care continued to meet or exceed STS benchmarks and will be monitored on an ongoing basis by the MDC.
Summary
Participating physicians involved in this lung MDC quickly embraced patient-centered collaborative care as a superior model for cancer care. Implementation of this MDC resulted in significant improvements in the quality of care, patient retention, and health system financial growth. It also appeared to enhance the local reputation of lung cancer care in the community and may have reduced overall costs.
Acknowledgment
We thank the Vince Lombardi Charitable Funds Board for all their support in helping patients and their families in their fight against cancer. We also thank Joseph Mirro, MD for his assistance in the preparation of this article.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Marija Bjegovich-Weidman, Max Haid, Jean McDonald, Santosh Krishnan
Administrative support: Marija Bjegovich-Weidman
Provision of study materials or patients: Max Haid, Santosh Kumar, Jean McDonald, Santosh Krishnan
Collection and assembly of data: Marija Bjegovich-Weidman, Carol Huibregtse, Jean McDonald
Data analysis and interpretation: Marija Bjegovich-Weidman, Max Haid
Manuscript writing: Marija Bjegovich-Weidman, Max Haid, Santosh Kumar, Jean McDonald, Santosh Krishnan
Final approval of manuscript: Marija Bjegovich-Weidman, Max Haid, Santosh Kumar, Carol Huibregtse, Jean McDonald, Santosh Krishnan
References
- 1.Wisconsin Department of Health Services. Madison, WI: Wisconsin Department of Health Services, Division of Public Health; 2009. Wisconsin cancer incidence and mortality 2002-2006; p. 69. [Google Scholar]
- 2.National Comprehensive Cancer Network. Clinical practice guidelines in oncology. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- 3.Bjerager M. Delay in diagnosis and treatment of lung cancer. Danish Med Bull. 2001;53:453. [Google Scholar]
- 4.Association of Community Cancer Centers Cancer Program Guidelines. Rockville, MD: 2009. Mar, [Google Scholar]
- 5.Bozcuk H, Martin C. Does treatment delay affect survival in non-small lung cancer? A retrospective analysis from a single UK centre. Lung Cancer. 2001;34:243–252. doi: 10.1016/s0169-5002(01)00247-1. [DOI] [PubMed] [Google Scholar]
- 6.Cancer Care Ontario. Toronto, Ontario, Canada: 2004. Nov, Cancer surgery wait times measurement in greater Toronto area. [Google Scholar]
- 7.Cent M, Shivers K. Physician collaboration and quality improvement outcomes. Oncol Issues. 2010;25:30–37. [Google Scholar]
- 8.Fleissig A, Jenkins V, Catt S, et al. Multidisciplinary teams in cancer care: Are they effective in the UK? Lancet Oncol. 2006;7:935–943. doi: 10.1016/S1470-2045(06)70940-8. [DOI] [PubMed] [Google Scholar]
- 9.Salomaa ER, Sällinen S, Hiekkanen H, et al. Delays in the diagnosis and treatment of lung cancer. Chest. 2005;128:2282–2288. doi: 10.1378/chest.128.4.2282. [DOI] [PubMed] [Google Scholar]
- 10.Skokie, IL: 2007. Sg2 Clinical Intelligence. Multidisciplinary Cancer Clinics: Reinventing Treatment Planning. [Google Scholar]
- 11.Valdés S, García E, Pérez H, et al. Length of diagnostic delay in patients with non-small cell lung cancer. MEDICC Rev. 2010;12:29–32. doi: 10.37757/MR2010.V12.N1.6. [DOI] [PubMed] [Google Scholar]
- 12.Presant C, Whitworth P, Salom E, et al. Personalized cancer care: A new paradigm in oncology. Oncol Issues. 2010;25:18–23. [Google Scholar]