Abstract
The authors outline the process through which the infectious diseases department at The M. D. Anderson Cancer Center successfully integrated physician assistants into patient care services, as judged by an overall increase in departmental productivity, broadened patient care coverage, and physician satisfaction with midlevel services.
Introduction
The primary goal of the recently passed health care reform bill is to increase access to affordable care for Americans. One limitation to achieving this goal is the predicted shortages of health care professionals in the future.1–3 The delivery of cancer care will also be affected by increasing demand caused by an aging population, expanding treatment options, and increased numbers of cancer survivors with complicated medical needs.4–7 The Workforce Statement by ASCO recommended the development of a workforce that includes increased utilization of midlevel providers such as physician assistants (PAs) and nurse practitioners (NPs) to help alleviate this burden and ensure delivery of quality cancer care.6 Two reports addressed this idea and reported on the use of PAs and NPs in the field of oncology.7,8
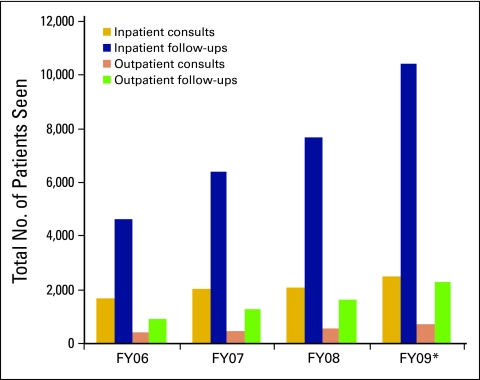
Cancer care is delivered not only by oncologists, but by a variety of personnel in multispecialty disciplines including infectious diseases (ID). Infection is the most common complication of cancer and its treatment.9 The University of Texas, M. D. Anderson Cancer Center (MDACC) is one of the largest comprehensive cancer centers in the nation. Currently, 18% to 22% of all hospital admissions to this center are infection related. The Department of Infectious Diseases provides inpatient and outpatient consultations to all requesting oncology services. Although MDACC has employed PAs and NPs for over 30 years, with the numbers of providers increasing annually, until recently, all of the ID services were provided by faculty and clinical fellows. Fellows rotate at several institutions and are not always available to provide support at MDACC. Over the past several years, ID interventions at MDACC have increased substantially (Fig 1) and put a severe strain on our clinical faculty to meet this demand. The rest of this report deals with the development of the ID PA workforce at MDACC.
Figure 1.
Increases in clinical infectious diseases (ID) activity with the initiation of the ID physician assistant program. Hospital admissions increased by 9.8% for fiscal year (FY) 06 to 09. In the ID service, a 48% increase was noted for inpatient consults, a 125% increase for inpatient follow-ups, a 74% increase for outpatient consults, and a 145% increase for outpatient follow-ups.
The MDACC ID Service
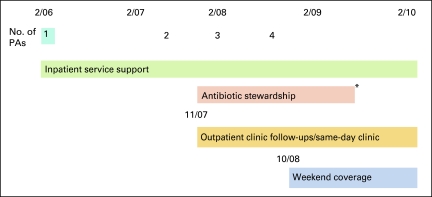
Before PAs were hired, the inpatient ID services consisted of hematology ID service, intensive care unit ID service, and solid tumor ID service. One faculty and one fellow, when available, managed each ID service, performed all new consultations, and provided follow-up care. Frequently, there were periods when fellows were not available depending on the rotation schedule. In addition, each ID faculty performed outpatient consultations and follow-ups one morning a week. Other activities included the development of institutional guidelines for the prevention, diagnosis, and treatment of infections, and interactions with the microbiology/laboratory regarding new diagnostic methods, susceptibility testing, and the institutional antibiogram. The need for developing a multidisciplinary antimicrobial stewardship team was also recognized and initiated through a quality improvement project in 2006 but could not be sustained after completion of the project. Finally, it was recognized that education in the fellowship training program was being negatively affected by increased clinical activity, as was the time available for faculty to conduct research, which is an academic requirement. Consequently, the ID PA workforce was developed and the first PA was hired in February 2006 (Fig 2).
Figure 2.
Timeline showing number of physician assistants (PAs) and services provided. PA start dates were February 2006, July 2007, February 2008, and August 2008. (*) Antibiotic stewardship service ended in April 2009.
Evolution of the ID PA Workforce
Inpatient ID service.
The first PA was used almost exclusively on the inpatient services. This resulted in approximately100 patients per month being seen by the PA with faculty supervision. By October 2008, as the PA workforce increased to four, approximately 400 patients per month were being seen by the ID PAs. The PAs primarily provided follow-up care but occasionally performed the initial consultation, with the final decision making being the responsibility of the faculty. The PAs were able to help see patients that would have not been seen on a daily basis because of time and resource constraints of the faculty/fellow teams. As Figure 1 reveals, the number of patients seen overall increased with the addition of the PAs. Before the PAs, education in the fellowship program was suffering as a result of an increased clinical load. With the addition of the PAs, more time was available for the faculty to teach the clinical fellows, and an expansion in the fellowship program was obtained through an affiliation with Baylor College of Medicine.
Outpatient Clinic
Before the establishment of the ID PA outpatient clinic, patients were seen one half day per week only on the faculty's assigned clinic day. Due to the increasing numbers of consultations, limited availability of clinic slots and scheduling/logistic issues, many patients were lost to follow-up after being discharged. The second PA was hired to staff the PA outpatient clinic which became fully operational by November 2007. Patients can now still be seen during the faculty's assigned clinic, but there is an additional PA run clinic available to see patients. The number of patients seen in this clinic has risen from 9 during the first month of operation to a current average of 71 per month. The clinic has enabled the department to provide adequate follow-up after hospital discharge, and is also a great convenience to patients who live in another city or state and cannot keep appointments on their ID physicians assigned clinic day.
Antimicrobial Stewardship Program
Antimicrobial resistance is a major problem, especially in patients with cancer, as a result of the high volume of antimicrobial use.9,10 With the pipeline for new drug development being relatively dry, judicious usage of currently available agents has been recommended by organizations such as the Infectious Diseases Society of America.11–13 The creation of multidisciplinary teams to implement these programs is strongly recommended.11–13 The first attempt at developing such a program at MDACC was through a quality improvement project in 2006 but was not sustained.14 In November 2007, a pilot program was launched in our intensive care unit, with PAs and fellows playing a key role along with ID faculty. The PAs, with faculty support, monitored the daily use of restricted agents (carbapenems and vancomycin) and made recommendations to stop, change, or continue these agents after 5 days. Data from 2007 to 2008 documented a decrease in the frequency of multidrug-resistant Pseudomonas aeruginosa from 85% to 22%, and of vancomycin-resistant enterococci from 64% to 22%. Reduced mortality was also documented.15 The PAs played a pivotal role in monitoring and implementing this program, which has now been expanded to the rest of the institution and is being comanaged by the ID and Pharmacy departments.
Weekend Service
With the addition of the fourth PA in October 2008, the weekend service was initiated. Before this, a faculty and one fellow were in charge of all of the ID patients, including new consults on the weekend. Most patients could not be observed over the weekend. The PA weekend service allowed up to an additional 30 patient follow-ups to be performed. These patients are seen by the ID PA covering the weekend service. Over the past several months, the PA weekend service has helped ensure quality and continuity of care throughout the weekend. This has relieved the pressure on the faculty/fellow team considerably, allowing them to focus on new consultations and care of critically ill patients over the weekend.
Additional Activities
MDACC is an academic institution with a mission to develop programs that integrate patient care, research, and prevention through education of health care professionals, trainees, and the public. Our PAs actively participate in our clinical training program, mentor students, are members of important hospital committees, and are active in PA organizations. They are now being encouraged to collaborate with research projects within the department.
Discussion
The delivery of quality cancer care has become more complex than in the past. Much of this is due to the discovery and development of new treatment modalities leading to increased survivorship in an aging population. Many patients receiving antineoplastic therapy develop complex medical problems, requiring the expertise of nononcological specialties. Many cancer survivors have prolonged periods of immune suppression and other consequences of antineoplastic therapy that also require such expertise on an ongoing basis. An increasing number of cancer patients prefer to receive all their care at their primary oncology centers. As outlined by Polansky et al, with regard to the ASCO Workforce study, by year 2020 a shortage of oncologists and an increasing demand for oncology services will exist. The roles of PAs and NPs working in oncology was described as well as the observations made by oncologists. Increased efficiency, improved patient care, and overall improvement in professional satisfaction among physicians were some of the contributions observed.6–8 As an ID department within a cancer institution, we will most likely face the same workforce shortage in the coming years. With PAs in our department, we feel that we have been able to achieve results comparable to those described in the articles above.
As mentioned previously, PAs or NPs were formerly not part of the ID workforce. ID faculty and fellows have, however, interacted closely with them on the oncology services, as PAs and NPs are often the ones who initiate ID consultations and implement the resulting recommendations. These interactions built up a level of comfort and trust that enabled the ID department to incorporate PAs and NPs into its workforce. An informal survey was distributed to the 11 ID faculty this year, revealing the following information: (1) faculty and fellows have a greater understanding of the role of PAs, (2) PAs have improved the quality of patient care by absorbing a substantial portion of the clinical load and streamlining follow-up visits and continuity of care, (3) PAs have played a pivotal role in expanding existing clinical programs and creating new ones (eg, the weekend service and the ID PA same-day clinic), and (4) the ID department would strongly recommend PAs or NPs to other disciplines within the institution.
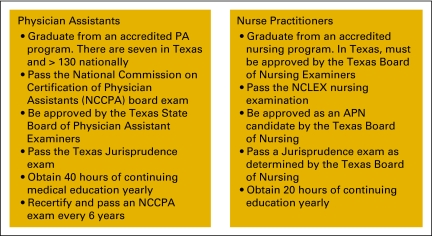
We also sought to determine whether ID departments at other cancer centers had PAs or NPs as part of their workforce. Telephone calls were placed to 40 cancer centers designated by the National Comprehensive Cancer Network.16 The majority of these centers worked with an ID group affiliated with a university and did not have an ID department within their center. Only seven (17.5%) reported that they had PAs or NPs as part of their workforce. Furthermore, most of these providers worked primarily in an outpatient setting and dealt mainly with HIV/AIDS patients. None of these centers used PAs or NPs the same way that they are being used at MDACC. We believe that our model makes effective use of PAs and NPs and is well within the scope of practice (Fig 3).17,18
Figure 3.
Licensing and regulatory issues in Texas for physician assistants (PAs) and nurse practitioners (NPs). NCLEX, National Council Licensure Examination; APN, advanced practice nurse.
An issue that merits some discussion is the measurement of a PA's or an NP's productivity. Quantifying their billing alone is not an accurate measure as patients are often treated both by PAs and physicians who bill for these services. In fiscal year 2009, PA charges accounted for 29% of all follow-up visits across the department. From March to December of 2009, PAs posted charges for 69% of all the patients they saw, and the supervising physician treated and billed for 31% of the patients the PAs saw. The PAs have also allowed the faculty to increase their productivity with regard to the number of publications over the last several years. A recent study aimed to further investigate productivity for PAs and NPs in the field of oncology.19 Although it did seem the providers increased productivity, it was hard to measure on the basis of billing alone. This is a dilemma faced by PAs and NPs at our institution and many others.19
The PAs also contribute by performing important nonbillable activities. These include triage of requests for same-day outpatient consultations, clinic visits and consultations with other services, and returning phone calls from patients. In addition, participation in stewardship program is a team effort and is difficult to quantify. Nevertheless, the institutional monetary value of the presence of PAs can be estimated in terms of reduction in overall antimicrobial usage; reduction in the frequency of resistant organisms; and decreases in morbidity, mortality, and length of stay.
The decision to use PAs in a specialty ID service took into consideration the training commitment necessary to develop competent health care providers. Most receive an abbreviated level of ID education during their formal training. Most of their clinical knowledge is acquired during on-the-job training. The four PAs in the MDACC ID department were hired with varying levels of experience. MDACC is an academic institution that has a multitude of educational opportunities. The ID department has a fellowship training program that provides weekly lectures, case presentations, and direct physician oversight for the fellows. Appropriate integration of the PAs into selected aspects of the training program ensured PA competency with ID issues. We wish to explore developing a curriculum for an ID PA training program.
Summary
This article describes the use of PAs and NPs in an ID specialty service at a comprehensive cancer center. We have outlined the process through which the ID department at MDACC successfully integrated PAs and NPs into patient care services as judged by an overall increase in departmental productivity, broadened patient care coverage, and ID physician satisfaction with midlevel services. This article provides one model of practice for integrating PAs and NPs into oncology IDs.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Candice N. White, Victor E. Mulanovich, Kenneth V. Rolston
Administrative support: Candice N. White
Collection and assembly of data: Candice N. White, Roy A. Borchardt, Mary L. Mabry, Kathleen M. Smith, Kenneth V. Rolston
Data analysis and interpretation: Candice N. White, Roy A. Borchardt, Victor E. Mulanovich, Kenneth V. Rolston
Manuscript writing: Candice N. White, Roy A. Borchardt, Mary L. Mabry, Kathleen M. Smith, Victor E. Mulanovich, Kenneth V. Rolston
Final approval of manuscript: Candice N. White, Roy A. Borchardt, Mary L. Mabry, Kathleen M. Smith, Victor E. Mulanovich, Kenneth V. Rolston
References
- 1.Erikson C, Salsberg E, Forte G, et al. Future supply and demand for oncologists: Challenges to assuring access to oncology services. J Oncol Pract. 2007;3:79–86. doi: 10.1200/JOP.0723601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colwill JM, Cutice JM, Kruse RL. Will generalist physician supply meet demands of an increasing aging population? Health Affairs. 2008;27:232–241. doi: 10.1377/hlthaff.27.3.w232. [DOI] [PubMed] [Google Scholar]
- 3.Bodenheimer T, Pham HH. Primary care: Current problems and proposed solutions. Health Affairs. 2010;29:799–805. doi: 10.1377/hlthaff.2010.0026. [DOI] [PubMed] [Google Scholar]
- 4.Rolston KV, Bodey GP. Infections in patients with cancer. In: Holland JF, Frei E, editors. Cancer Medicine. ed 6. Hamilton, Canada: BC Decker; 2003. pp. 2633–2658. [Google Scholar]
- 5.Cooksley CD, Avritscher EB, Rolston KV, et al. Hospitalizations for infection in cancer patients: Impact of an aging population. Support Care Cancer. 2009;17:547–554. doi: 10.1007/s00520-008-0520-3. [DOI] [PubMed] [Google Scholar]
- 6.American Society of Clinical Oncology. 2008-2013 Workforce Strategic Plan: To ensure continuing access to quality cancer care. http://www.asco.org/ASCO/Downloads/Research%20Policy/Workforce%20Page/ASCO%20Workforce%20Strategic%20Plan.pdf.
- 7.Polansky M, Ross AC, Coniglio D. Physician assistant perspective on the ASCO workforce study regarding the use of physician assistants and nurse practitioners. J Oncol Pract. 2010;6:31–33. doi: 10.1200/JOP.091063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ross AC, Polansky MN, Parker PA, et al. Understanding the role of physician assistants in oncology. J Oncol Pract. 2010;6:26–30. doi: 10.1200/JOP.091062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hughes WT, Armstrong D, Bodey GP, et al. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis. 2002;34:730–751. doi: 10.1086/339215. [DOI] [PubMed] [Google Scholar]
- 10.Rolston KV. Challenges in the treatment of infections caused by gram-positive and gram-negative bacteria in patients with cancer and neutropenia. Clin Infect Dis. 2005;40(suppl 4):S246–S252. doi: 10.1086/427331. [DOI] [PubMed] [Google Scholar]
- 11.Talbot GH, Bradley J, Edwards JE, Jr, et al. Bad bugs need drugs: An update on the development pipeline from the Antimicrobial Availability Task Force of the Infectious Diseases Society of America. Clin Infect Dis. 2006;42:657–668. doi: 10.1086/499819. [DOI] [PubMed] [Google Scholar]
- 12.Boucher HW, Talbot GH, Bradley JS, et al. Bad bugs, no drugs:no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2008;48:1–12. doi: 10.1086/595011. [DOI] [PubMed] [Google Scholar]
- 13.Dellit TH, Owens RC, McGowan JE, Jr, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44:159–177. doi: 10.1086/510393. [DOI] [PubMed] [Google Scholar]
- 14.Adachi J, Perego C, Vigil K, et al. Antibiotic stewardship initiative in the intensive care unit (ICU): Evidence from a quality improvement project supporting the development of a multidisciplinary antimicrobial stewardship team (MAST). Multinational Association for Supportive Care in Cancer 2008 International Symposium; June 26-28, 2008; Houston, Texas. (abstr 08-059) [Google Scholar]
- 15.Mulanovich VE, Chemaly RF, Borchardt RA, et al. Antimicrobial stewardship project in the intensive care unit (ICU) of a comprehensive cancer center: Impact on quality of care and patient safety. Presented at the Society for Healthcare Epidemiology of America; March 19-22, 2009; San Diego, CA. [Google Scholar]
- 16.National Comprehensive Cancer Network. www.nccn.org.
- 17.Texas Medical Board. Physician Assistants. www.tmb.state.tx.us/professionals/physicianassist.
- 18.Texas Board of Nursing. Nursing education information. www.bon.state.tx.us/nursingeducation.
- 19.Hinkel JM, Vandergrift JL, Perkel SJ, et al. Practice and productivity of physician assistants and nurse practitioners in outpatient oncology clinics at National Comprehensive Cancer Network institutions. J Oncol Pract. 2010;6:182–187. doi: 10.1200/JOP.777001. [DOI] [PMC free article] [PubMed] [Google Scholar]