The multidisciplinary clinic approach to prostate cancer may enhance outcomes and reduce “treatment regret” through a coordinated presentation of all therapeutic options. This model serves as an interdisciplinary educational tool for patients and their families, and supports clinical trial participation.
Abstract
Purpose:
To report on the 15-year prostate cancer experience of our multidisciplinary genitourinary cancer clinic established in 1996 at the National Cancer Institute (NCI) –designated Jefferson Kimmel Cancer Center. Patients with genitourinary cancers were evaluated weekly by multiple specialists at a single site, and we focus on the 83% of patients with prostate cancer. To our knowledge, our multidisciplinary genitourinary cancer clinic is the longest continuously operating center of its kind at an NCI Cancer Center in the United States.
Methods:
Data from Jefferson's Oncology Data Services were compared to SEER prostate cancer outcomes. Data on treatment changes in localized disease, patient satisfaction, and related parameters were also assessed.
Results:
Ten-year survival data approach 100% in stage I and II prostate cancer. Ten-year data for stage III (T3 N0M0) and stage IV (T4 N0M0) disease show that our institutional survival rate exceeds SEER. There is a shift toward robotically assisted laparoscopic radical prostatectomy and a slight decrease in brachytherapy relative to external beam radiation therapy in localized disease. Patient satisfaction is high as measured by survey instruments.
Conclusion:
Our long-term experience suggests a benefit of the multidisciplinary clinic approach to prostate cancer, most pronounced for high-risk, locally advanced disease. A high level of satisfaction with this patient-centered model is seen. The multidisciplinary clinic approach to prostate cancer may enhance outcomes and possibly reduce treatment regret through a coordinated presentation of all therapeutic options. This clinic model serves as an interdisciplinary educational tool for patients, their families, and our trainees and supports clinical trial participation.
Introduction
Prostate cancer (PCa) remains the most common nonskin cancer and the second leading cause of cancer mortality in men in the United States. PCa will effect 217,730 men in 2010, with 32,050 deaths.1 The optimal management for localized PCa is controversial, with options including active surveillance, surgery, radiotherapy, cryotherapy, or other investigational methods. In deciding on a treatment for localized PCa, patients must be informed of the risks and benefits of each option. All specialists must provide patients with up-to-date information on the options and be aware of the different influences that surround these men during the decision-making process.2
Since 1996, the Kimmel Cancer Center (KCC) of Thomas Jefferson University (TJU) has offered newly diagnosed genitourinary cancer patients and those needing additional consultation the opportunity to be evaluated in a multidisciplinary clinic. Our team works with patients and referring physicians to devise treatment plans that are tailored to the individual needs of each patient. The goals of this weekly multidisciplinary genitourinary cancer clinic (MDGUCC) are to provide state-of-the-art oncology care and to serve as an educational resource for patients, their families, and physicians in training.
We published our initial multidisciplinary clinic protocol in 2000.3 Since that time, several other centers have developed similar programs.4–6 Herein we report on findings from our KCC/TJU oncology data to explore the impact of our multidisciplinary efforts over the last 15 years and to describe changes to our original program.
Methods
The Cancer Registry database was queried, and a retrospective review was performed to compare the overall survival of patients treated at KCC/TJU with that of patients treated nationally according to the NCI Surveillance, Epidemiology, and End Results (SEER) Program for the year 2006, 10 years after the establishment of MDGUCC. Log-rank and Wilcoxon statistical analysis were performed, and P < .05 was considered as statistically significant. We reviewed anonymous surgical and radiation oncology data and an institutional review board–approved radical prostatectomy and laparoscopy database. Patient satisfaction was analyzed from a simple blinded six-item questionnaire.
Results
Over the past 10 years, the number of patients evaluated at the MDGUCC averaged 434 per year, with PCa patients representing 83% of the total number (approximately 384 PCa patients per year). Established patients were re-evaluated in MDGUCC when necessary, comprising 10% to 22% patient visits over this period. The most recent 6-month data showed that the percentage of PCa patients who present for rising prostate-specific antigen or adverse surgical pathology has increased, possibly as a result of the growth of medical oncology presence in the clinic.
We reviewed the percentage of PCa patients who came to our center for a second opinion and the percentage of patients who continued treatment at TJU. The majority of patients with PCa at the KCC/TJU have been referred to our MDGUCC since 1996. In 1995, 91 patients (65%) sought a second opinion for treatment, and among them, 55 (60%) received all or part of the first treatment at TJU. By 2008, 244 patients (75%) diagnosed elsewhere and 211 (99%) diagnosed at our institution elected to receive all or part of the first treatment at TJU, suggesting the positive influence of the multidisciplinary programs on patient care at TJU.
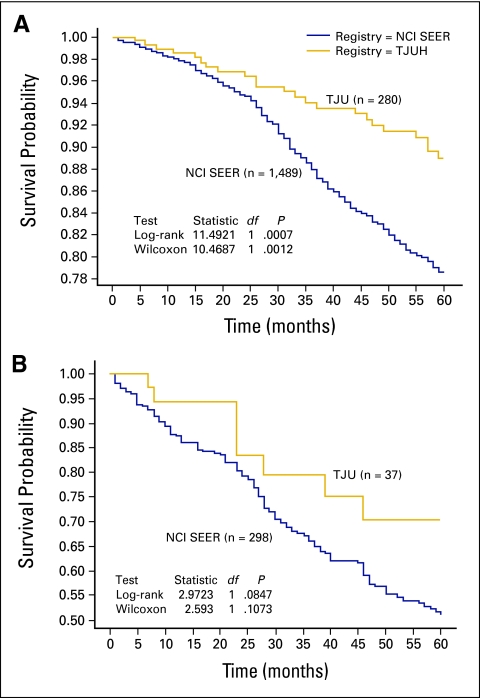
The stage distribution of our newly diagnosed PCa patients was comparable to those of NCI SEER and the National Cancer Database (NCDB). However, a slightly higher proportion of the TJU/KCC patients had intermediate stage (II/III) disease (90.8% v 87.7% in SEER and 84.2% in NCDB; Table 1). Five- and 10-year survival for stage I/II disease approached 100%, similar to other reports. The graphs in Figure 1 display overall survival of stage III and IV disease (11.5% of the total PCa patients were stage III and IV) comparing two survival curves, 1995 to 2006 for KCC patients and 1997 to 2003 with data available from NCI SEER. There is an age difference between the TJUH/KCC and SEER (for stages III and IV, the TJUH/KCC median age was 62 years v 73 years in SEER). Survival was recalculated stratifying by age (< 65, > 65), and the survival advantage seen in the TJU/KCC cohort remained after this adjustment (data not shown). The TJU/KCC cohort includes more members of racial/ethnic minorities (eg, African Americans = 21.3% v 15.7% in SEER). Overall, patients with locally advanced PCa treated at TJUH/KCC appeared to have better outcomes when benchmarked against national SEER data.
Table 1.
AJCC Stage at Diagnosis Over the Last 4 Year Period at Our Center Compared to SEER and NCDB Data
| Stage | TJU/KCC (%) | NCI SEER (2004) (%) | NCDB (2004) (%) |
|---|---|---|---|
| I | 0.7% | 0.2% | 1.3% |
| II | 84.1% | 80.9% | 76.5% |
| III | 6.7% | 6.8% | 7.7% |
| IV | 4.8% | 6.2% | 4.8% |
| Unknown | 3.6% | 5.9% | 9.7% |
Abbreviations: AJCC, American Joint Committee on Cancer; NCI, National Cancer Institute; SEER, Surveillance, Epidemiology, and End Results; NCDB, National Cancer Data Base.
Figure 1.
Kaplan-Meier survival of patients with newly diagnosed prostate cancer at the TJUH/KCC (1996-2008) and patients in NCI SEER (1997-2003). (A) Stage III (T3 N0 M0); (B) T4 N0 M0. TJUH, Thomas Jefferson University Hospital; KCC, Kimmel Cancer Center; NCI, National Cancer Institite; SEER, Surveillance, Epidemiology, and End Results.
There are many reasons for this observed survival improvement in patients with locally advanced disease. Technical expertise from fellowship-trained urologic oncologists and robotically assisted surgeons, radiation oncologists with specific academic interest in PCa supported by strong dosimetry and radiation physicists, appropriate medical management and other supportive care, patient education, and patient's socioeconomic status all may subtly contribute to this improved outcome. The close real-time interaction may more appropriately identify patients who may benefit from combined modalities such as radiation with hormonal therapy or postoperative adjuvant radiation therapy, or clinical trials. It is our belief that the coordination of care provided by the multidisciplinary team is a factor to strongly consider in assessing the reasons for improved patient outcomes.
We recognize limitations in this analysis. The data were gathered prospectively, and analysis is retrospective. It is not possible to provide definitive PCa-specific survival from our database. Lastly, although the majority of patients with PCa were evaluated in our MDGUCC, it is possible that a few other patients were included in the institutional tumor registry data set.
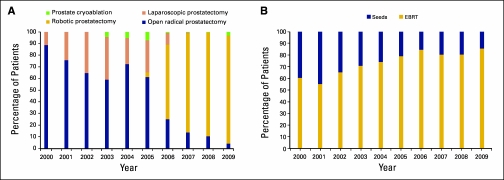
Treatment Changes Over Time
There has been a dramatic shift in the surgical management of localized disease to robotically assisted laparoscopic radical prostatectomy, similar to nationwide trends (Fig 2A). In patients choosing radiation therapy, the relative percentage choosing brachytherapy versus external beam has declined slightly over the past 10 years (Fig 2B).
Figure 2.
Treatment changes over time, in surgical method (A) and radiation treatment type (B). EBRT, external beam radiation therapy.
Patient Satisfaction
Periodically, patients are asked to complete an anonymous six-item satisfaction questionnaire after the clinic visit. More than 90% of patients reported the experience as “good” or “very good” and would recommend the MDGUCC. Other specific comments from patients are: “one day, wealth of info, thank you”; “everyone knowledgeable”; “would recommend to others,” and so on (Table 2).
Table 2.
Patient Satisfaction Survey Concerning the Multidisciplinary Clinic Experience: Percentage of “Good” and “Very Good” Responses
| Survey Item | Percentage of Responses |
||
|---|---|---|---|
| Nov 2008 to Jan 2009 | June 2009 to Sept 2009 | Oct 2009 to Jan 2010 | |
| Waiting time for appointment | 94 | 95 | 90 |
| Explanation of what to expect | 94 | 96 | 93 |
| Waiting time in center | 91 | 90 | 86 |
| Treatment with respect and dignity | 97 | 98 | 100 |
| Treatment option explained by doctors | 100 | 98 | 100 |
| Likelihood of recommending | 93 | 98 | 93 |
Discussion
For men with clinically localized PCa, a major issue is the lack of conclusive comparative studies demonstrating superiority of one modality over another.7 In the decision-making process for a man with localized disease, this is one major area in which the multidisciplinary clinic approach can improve patient care. A SEER-based study of 85,088 men with localized PCa evaluated how visits to specialists and primary care physicians related to treatment choice.8 The type of specialist visit related strongly to the choice of treatment, and the authors noted the importance of men having access to balanced information. A similar study demonstrated that treatment decisions had little relation to patient preferences but were associated with the specialty of the counseling clinician.9 A primary goal of the MDGUCC approach to PCa is to provide this balanced information in an open and interactive fashion, with all clinical specialists present at the same time. Shared decision making through a discussion with different specialists about the risk and benefits of each treatment can decrease distress and post-treatment regret.10,11 For example, the Walter Reed Army Medical Center clinic features small-group lectures on the specific treatment modalities.5 Reports from other multidisciplinary clinics indicate high patient satisfaction similar to the levels at our clinic.6
In establishing a multidisciplinary clinic, the need for the long-term commitments of all participants and the institution cannot be underestimated. Although the multidisciplinary setting is often viewed as an “inefficient” use of time in terms of the numbers of patients that can be seen by an individual clinician, we have demonstrated that there is a potential outcome benefit to many patients with this approach. Patients in our multidisciplinary clinic who elect to receive longitudinal care at our hospital can increase hospital volumes and bring critical downstream benefits to the institutions that support these programs. Furthermore, the patient satisfaction and interdisciplinary educational aspects cannot be underestimated. There are several essential features of our MDGUCC:
Synchronous multidisciplinary counseling for patients and their families.
Half-day clinic with lengthy visit slots (≥ 60 minutes.) so that ample time is provided for the multidisciplinary session (families are requested to dedicate at least 3 to 4 hours for the entire visit).
- Fully integrated multidisciplinary specialty oncology team composed of the following physicians and staff:
- Urologic surgical oncologists.
- Radiation oncologists.
- Medical oncologists.
- Dedicated pathologist who participates in preclinic conference.
- On call radiology consultants.
- Full-time prostate cancer care coordinator (primarily responsible for data acquisition, scheduling, and following up with patients and referring physicians).
- Dedicated oncology nurses.
- On-call protocol coordinators to assist with clinical trials accrual.
- Genetic counseling consultant available outside of regular clinic hours.
Discussion and assessment of eligibility for clinical trials.
Optimal, real-time communication among the specialists.
Intensive social work support, including the “Buddy Program” (age- and treatment modality–matched patients who are trained to counsel other patients).
Follow-up visits in the similar setting are available when necessary.
Use of patient satisfaction surveys and outcome data to improve quality care.
Supporting educational conference schedules.
Institutional commitment to support necessary resources for this activity.
Other practical aspects are useful to review when considering this type of operation. All physicians are on the full-time faculty of Jefferson Medical College and KCC and are assigned to the clinic by their respective department chairs. The site of service is a hospital-based clinic facility, with provider-based billing and no charge back to the departments. As a hospital-based facility, the clinic receives a slightly lower insurance reimbursement for the physicians who are not hospital based from some carriers. The 10 examinations rooms are part of the Bodine Center for Cancer Treatment, a clinical area of the Department of Radiation Oncology. Plans are underway for a new clinical facility on our Jefferson Campus that will have space specifically designed for this and other cancer center multidisciplinary clinics.
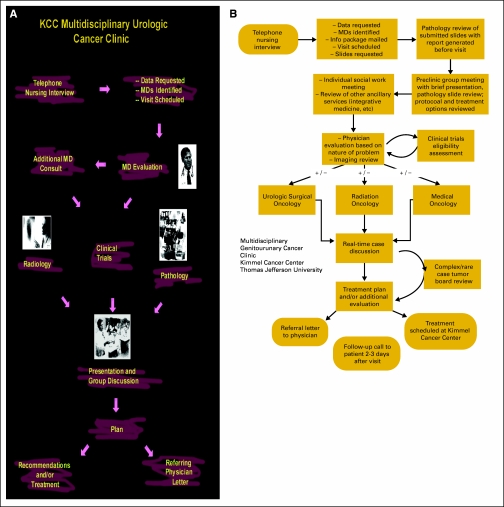
Over the last 15 years, we have implemented changes to improve the efficiency and patient experience. Because the clinic is a patient-centered program, patients and families remain in the examination/consultation room, and members of the professional staff come to the patient. When initiated in 1996, the clinic had a formal postconference management session (Fig 3A).3 Wide variations in the ending time of the clinic resulted in some modifications that are graphically illustrated in Figure 3B.
Figure 3.
(A) Initial 1996 to 2008 clinic process; (B) patient flow through the multidisciplinary genitourinary cancer clinic based on the current model.
Currently, the clinicians meet before the clinic to review the case histories, images, and biopsy slides in a multidisciplinary genitourinary pathology conference with a dedicated urologic pathologist. This operational change took place in 2008 and has been well received, as it allows each specialist to have the necessary time with the patient to avoid rushing to attend the postclinic conference. We discuss potential treatment strategies and clinical trials eligibility. All data are collected beforehand by our dedicated prostate cancer care coordinator, who designs the schedule, and the physicians who will evaluate the patient. At the weekly clinic, two urologic oncologists, two radiation oncologists, and one to two medical oncologists are usually on site in addition to the support staff. A social worker visits with each patient to address any nonmedical issues and to introduce the Buddy Program. Our cancer support services, such as Jefferson's Brind Center for Integrative Medicine, are also offered. The clinical trial support staff is readily available. Medical students, residents, and fellows participate.
In another change to our procedures, a brief real-time discussion specific to each patient is now held after the clinical specialty evaluations to decide on the management recommendations and follow-up plans. Treatment recommendations are communicated to the patient and referring physician immediately, with follow-up by the prostate care coordinator later. Where complicated cases are involved, a traditional bimonthly tumor board is now held, with literature review and additional specialists providing input as needed. A clinical trials protocol review and a formal bimonthly prostate cancer lecture series are also part of this unified multidisciplinary clinic approach.
Similar to other cancers, there has been a decrease in PCa death rates in the United States from 38.6 to 23.6 per 100,000 from 1990 to 2006 (38.9% reduction).12 Although the reasons for this decline are debated, improvements in early diagnosis and treatments for all stages of disease are likely candidates. Our institutional data were benchmarked to national standards such as SEER and showed further improvement in several areas. Coordinated care of the cancer patient at all disease stages has been an increasing theme in oncology, and this multidisciplinary clinic model improves outcomes in other malignancies such as breast cancer.13
Summary
The optimum management for an individual patient with PCa is not well defined. Our 15-year experience with a multidisciplinary approach for patients with PCa through the MDGUCC is successful in terms of both patient satisfaction and our institutional data, which suggest improved outcomes in many men with locally advanced high-risk disease. A team of committed urologists, radiation oncologists, medical oncologists, and other specialists, in partnership with dedicated coordinators, is essential for the success of this patient-centered program.
Acknowledgment
We thank our current support staff members: Ellen Clancy, Barbara Daulerio, Renee Zalinsky, Theresa Morsa, Jennifer Fleischmann, Jillian Brown, Melisa Mordenti, Amanda Peterson, Kate Rehm, Cindy Caruso, and Emily Feeney; the Bodine Clinical staff; Office of Oncology Data Services; and all of the former staff members who have contributed to this effort over the last 15 years.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Leonard G. Gomella, Jean Hoffman-Censits, Costas D. Lallas, Peter McCue, Adam Dicker, Edouard J. Trabulsi
Administrative support: Patricia Dugan
Provision of study materials or patients: Jean Hoffman-Censits, Costas D. Lallas, Peter McCue, Timothy Showalter, Richard K. Valicenti, Adam Dicker, Edouard J. Trabulsi
Collection and assembly of data: Jianqing Lin, Patricia Dugan, Fran Guiles, Jaspreet Singh, Peter McCue, Timothy Showalter, Adam Dicker
Data analysis and interpretation: Jianqing Lin, Jaspreet Singh, Timothy Showalter, Adam Dicker, Edouard J. Trabulsi
Manuscript writing: Leonard G. Gomella, Jianqing Lin, Edouard J. Trabulsi
Final approval of manuscript: Leonard G. Gomella, Jianqing Lin, Jean Hoffman-Censits, Patricia Dugan, Fran Guiles, Costas D. Lallas, Jaspreet Singh, Peter McCue, Timothy Showalter, Richard K. Valicenti, Adam Dicker, Edouard J. Trabulsi
References
- 1.Jemal A, Siegel R, Xu J, et al. Cancer Statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Cox J, Amling CL. Current decision-making in prostate cancer therapy. Curr Opin Urol. 2008;18:275–278. doi: 10.1097/MOU.0b013e3282fba5f2. [DOI] [PubMed] [Google Scholar]
- 3.Valicenti RK, Gomella LG, El-Gabry EA, et al. The multidisciplinary clinic approach to prostate cancer counseling and treatment. Semin Urol Oncol. 2000;18:188–191. [PubMed] [Google Scholar]
- 4.Basler JW, Jenkins C, Swanson G. Multidisciplinary management of prostate malignancy. Curr Urol Rep. 2005;6:228–234. doi: 10.1007/s11934-005-0012-7. [DOI] [PubMed] [Google Scholar]
- 5.Hudak JL, McLeod DG, Brassell SA, Gant DA, Shaar S, Hudak RP, Dean RC, McGarvey MD, Tulin SJ, Dozier R. The design and implementation of a multidisciplinary prostate cancer clinic. Urol Nurs. 2007;27:491–498. [PubMed] [Google Scholar]
- 6.Madsen LT, Craig C, Kuban D. A multidisciplinary prostate cancer clinic for newly diagnosed patients: Developing the role of the advanced practice nurse. Clin J Oncol Nurs. 2009;13:305–309. doi: 10.1188/09.CJON.305-309. [DOI] [PubMed] [Google Scholar]
- 7.Singh J, Trabulsi EJ, Gomella LG. Is there an optimal management for localized prostate cancer? Clin Interv Aging. 2010;5:187–197. doi: 10.2147/cia.s6555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jang TL, Bekelman JE, Liu Y, et al. Physician visits prior to treatment for clinically localized prostate cancer. Arch Intern Med. 2010;170:440–450. doi: 10.1001/archinternmed.2010.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sommers BD, Beard CJ, D'Amico AV, et al. Predictors of patient preferences and treatment choices for localized prostate cancer. Cancer. 2008;113:2058–2067. doi: 10.1002/cncr.23807. [DOI] [PubMed] [Google Scholar]
- 10.Diefenbach MA, Mohamed NE. Regret of treatment decision and its association with disease-specific quality of life following prostate cancer treatment. Cancer Invest. 2007;25:449–457. doi: 10.1080/07357900701359460. [DOI] [PubMed] [Google Scholar]
- 11.Hu JC, Kwan L, Krupski TL, et al. Determinants of treatment regret in low-income, uninsured men with prostate cancer. Urology. 2008;72:1274–1249. doi: 10.1016/j.urology.2007.11.066. [DOI] [PubMed] [Google Scholar]
- 12.Jemal A, Ward E, Thun M. Declining death rates reflect progress against cancer. PLoS ONE. 5:e9584. doi: 10.1371/journal.pone.0009584. http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0009584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pichert G, Jacobs C, Jacobs I, et al. Novel one-stop multidisciplinary follow-up clinic significantly improves cancer risk management in BRCA1/2 carriers. Fam Cancer. 2010;9:313–319. doi: 10.1007/s10689-010-9333-x. [DOI] [PubMed] [Google Scholar]