Abstract
Optic neuritis (ON) is a rare neurological complication of measles infection. Little is known about measles-associated retrobulbar ON. Here, we report a distinct patient with unilateral retrobulbar ON due to measles infection. A 26-year-old woman developed maculopapular rash and Koplik spots. On the following 3 days, she noticed blurred vision in the left eye. A Goldmann visual field test showed inferior nasal quadrantanopsia in the left eye. Visual acuity was 20/20 in OD and 20/100 in OS. Pupillary size was 2.0 mm in the right eye and 4.0 mm in the left eye. Light reflexes were slightly sluggish in the left eye. Ophthalmoscopy showed mild pallor of the left optic disc. Central critical flicker fusion frequency (CFF) was 40.7 Hz in the right eye and 10.1 Hz in the left eye (normal =29.0). Visual evoked potentials showed that P100 latencies were delayed on the left side (133 ms). Brain and spinal cord MRI was normal. Orbital MRI displayed abnormal enhancement in the left optic nerve. Serum and cerebrospinal fluid IgG titers of anti-measles antibodies were increased. Left measles-associated ON was diagnosed. Methylprednisolone pulse therapy followed by oral administration of prednisolone ameliorated visual acuity, visual field and CFF. The neuroophthalmic profile of our patient indicated that measles infection triggered isolated retrobulbar ON, leading to unusual visual deficits. Thus, physicians should pay more attention to variable patterns of measles-associated ON.
Key Words: Measles virus, Optic nerve MRI, Quadrantanopsia, Retrobulbar optic neuritis
Introduction
Measles virus, a neurotrophic virus, is known to cause various kinds of neurological complications [1, 2], with a frequency of 4 neurological insults per 1,000 cases of measles infection. Measles encephalitis or impaired consciousness was observed in 1 per 1,000 cases [1] and commonly in children or adults >10 years of age [1]. Acute optic neuritis (ON) was described in patients with measles encephalitis [3, 4], whereas isolated ON was found in patients without measles encephalomyelitis [4,5,6,7,8]. Based on lesion topography, measles-associated ON could be divided into anterior and retrobulbar types. Anterior ON or papillitis due to measles infection was reported previously in several patients without other neurological deficits [4,5,6,7]. Little is known about measles-associated retrobulbar ON [2, 3, 8]. Here, we report a distinct patient with unilateral measles-associated retrobulbar ON.
Case Report
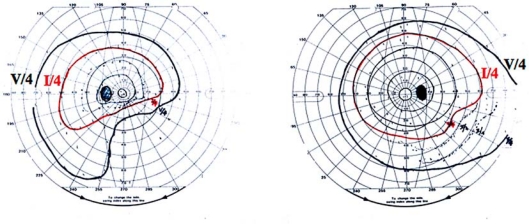
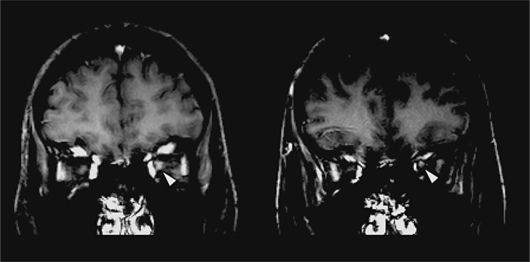
A 26-year-old healthy woman developed fever and maculopapular rash expanding from the face to the trunk and the four limbs. Subsequently, Koplik spots were present and measles was diagnosed. Three days after the onset of rash, she noticed blurred vision in the left eye. One week later, she visited a neighboring hospital and quadrantanopsia was found in her left eye. She was admitted to our department. Physical examination was normal. A Goldmann visual field test revealed inferior nasal quadrantanopsia without central scotomas in her left eye. The visual field of her right eye was normal (fig. 1). The corrected visual acuity was 20/20 in OD and 20/100 in OS. Pupillary size was 2.0 mm in the right eye and 4.0 mm in the left eye. Light reflexes were slightly sluggish in her left eye. Ophthalmoscopy showed mild pallor of the left optic disc. Neurological examination was normal except for visual dysfunction. Routine laboratory tests, electrocardiogram and chest X-ray were normal. Serum IgG titers of anti-measles antibodies were increased to 1:94.8 in an enzyme immunoassay (normal <1:2.0). Cerebrospinal fluid (CSF) examination disclosed a cell count of 1 mononuclear cell/mm3, protein levels of 38 mg/dl and cytology of class II. Myelin basic protein and oligoclonal IgG bands were negative. CSF IgG titers of anti-measles antibodies were elevated to 1:0.64 (normal <1:0.20). Serum anti-aquaporin 4 antibodies were not detected. In electrophysiological studies, sensory and auditory evoked potential tests were normal. An electroencephalogram was normal. Central critical flicker fusion frequency (CFF) showed 40.7 Hz in her right eye and 10.1 Hz in her left eye (normal =29.0). P100 latencies of visual evoked potentials disclosed 90.6 ms on the right side and 133 ms on the left side. Brain and spinal cord MRI revealed no pathognomonic lesions. Orbital MRI displayed abnormal enhancement in the left optic nerve (fig. 2). Our patient had seropositive and CSF-positive anti-measles antibodies, neuroophthalmic findings and abnormal enhancement of the left optic disc. These findings supported the diagnosis of unilateral measles-associated retrobulbar ON. Methylprednisolone pulse therapy (1,000 mg/day for 3 days, i.v.) and subsequent administration of prednisolone (1 mg/kg per day, p.o.) were performed. Prednisolone was tapered off within 1 month. After steroid treatment, left quadrantanopsia was improved and left visual acuity also normalized to 20/20. CFF was increased to 36.4 Hz in her left eye.
Fig. 1.
Goldmann visual field test shows inferior nasal quadrantanopsia in the left eye.
Fig. 2.
Orbital MRI shows abnormal enhancement in the left optic nerve (arrowhead).
Discussion
The neuroophthalmologic profile and MRI of our patient suggested unilateral measles-associated retrobulbar ON without CNS involvement.
Measles virus can generate various types of neurological complications [1, 2]. This neurotrophic virus is known to provoke acute ON together with CNS deficits or encephalitis [3, 8]. Twelve patients with measles-induced acute ON were reviewed previously [4]. Of the 12 patients, 7 had no signs of CNS involvement [5, 6, 9,10,11,12,13]. The age at onset was 6-14 years [6, 9,10,11,12,13]. Previously published reports of 10 patients with isolated measles-associated ON are listed in table 1. Bilateral visual deficits were found in 9 patients and unilateral disturbance in 1 patient [5]. Visual loss occurred commonly within the first weeks after rash. Two patients experienced visual disturbance several days before cutaneous symptoms [5, 10]. Ophthalmoscopy was performed in 9 patients. Fundus findings exhibited edematous optic disc in 6 patients, pallor optic disc in 1 patient and normal results in 2. Therefore, anterior ON or papillitis most often occurs in patients with measles-associated ON. Occurrence of retrobulbar ON is extremely rare, with only 4 cases being reported previously [2, 3, 8]. In a Japanese article, 2 patients (a 4-year-old girl and a 18-year-old boy) developed retrobulbar ON after measles encephalitis [3]. In another study, a Japanese female patient with measles had retrobulbar ON, Guillain-Barré syndrome and asymptomatic brain MRI lesions [5]. Another case (a 25-year-old woman) had retrobulbar ON without CNS lesions after measles. Her visual acuity of both eyes was counting fingers at 2 m whereas optic discs were normal on ophthalmoscopy [8].
Table 1.
Previous reports of isolated measles-associated ON
| First author | Year | Patient age | Onset after rash | Visual acuity | Optic disc | Visual recovery |
|---|---|---|---|---|---|---|
| Shlossberg [9] | 1940 | 6 years | 5 days | no light perception in OU | edema in OU | 4/200 in OD, 3/200 in OS |
| Wagener [10] | 1952 | 7 years | −6 days | 13/200 in OU | edema in OU | 20/20 in OU |
| Bedrossian [11] | 1955 | 6 years | 6 days | light perception in OU | edema in OU | 20/30 in OU |
| Tyler [12] | 1957 | 8 years | 12 days | 1/500 in OU | pallor in OU | normal in OU |
| Kennedy [13] | 1960 | 6 years | 2 days | hand movements in OU | edema in OU | 20/20 in OU |
| Srivastava [5] | 1963 | 8 years | −1 day | hand movements in OS | edema in OS | 20/30 in OS |
| Walsh [6] | 1969 | 14 years | 5 days | blindness in OU | 20/200 in OD, hand movements in OS | |
| Totan [8] | 1999 | 25 years | 11 days | counting fingers in OU | normal1 | 20/20 in OD, 20/25 in OS |
| Azuma [7] | 2002 | 31 years | 6 days | counting fingers in OU | edema in OU | 20/20 in OU |
| Tomiyasu [2] | 2009 | 28 years | 8 days | 2/200 in OD, 6/200 in OS | normal1 | 20/40 in OD, 20/16 in OS |
| Present case | 2010 | 26 years | 3 days | 20/20 in OD, 20/100 in OS | pallor in OS1 | 20/20 in OS |
Retrobulbar ON.
Several aspects of measles-associated ON are thought to mimic acute ON in patients with multiple sclerosis or neuromyelitis optica. A variety of visual field defects occur in optic neuropathies, including central, centrocecal, arcuate, altitudinal and nasal step field defects. The cardinal field defect of acute ON is a widespread depression of sensitivity and a central scotoma. However, other visual field changes such as bitemporal hemianopsia, a paracentral scotoma and altitudinal deficits may be observed in some ON patients. Non-central scotoma or atypical defects in the visual field have been found in neuromyelitis optica patients [14]. A recent quantitative study of laser polarimetry was performed in 25 patients with a single episode of ON. Superior and inferior quadrant retinal nerve fiber layer thinning was correlated with corresponding regional visual field loss [15]. Our patient developed inferior nasal quadrantanopsia in the left eye. Visual evoked potentials and orbital MRI clarified the left optic nerve lesion. The possibility was suspected that damage to the inferior quadrant retinal nerve fibers could cause corresponding quadrantanopsia.
In conclusion, unilateral measles-associated retrobulbar ON was noted in a patient without CNS lesions. Thus, physicians should pay more attention to variable patterns of acute ON triggered by measles virus.
Disclosure Statement
All authors declare no conflict of interest.
References
- 1.Miller DL. Frequency of complications of measles, 1963. Report on a National Inquiry by the Public Health Laboratory Service in Collaboration with the Society of Medical Officers of Health. Br Med J. 1964;ii:75–78. doi: 10.1136/bmj.2.5401.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tomiyasu K, Ishiyama M, Kato K, Komura M, Ohnuma E, Inamasu J, Takahashi T. Bilateral retrobulbar optic neuritis, Guillain-Barré syndrome and asymptomatic central white matter lesions following adult measles infection. Intern Med. 2009;48:377–381. doi: 10.2169/internalmedicine.48.1585. [DOI] [PubMed] [Google Scholar]
- 3.Inokuchi N, Nishikawa N, Fujikado T. Optic neuritis and measles infection. Nippon Rinsho. 1997;56:861–864. [PubMed] [Google Scholar]
- 4.Selbst RG, Selhorst JB, Harbison JW, Myer EC. Parainfectious optic neuritis. Report and review following varicella. Arch Neurol. 1983;40:347–350. doi: 10.1001/archneur.1983.04050060047007. [DOI] [PubMed] [Google Scholar]
- 5.Srivastava SP, Nema HV. Optic neuritis in measles. Br J Ophthalmol. 1963;47:180–181. doi: 10.1136/bjo.47.3.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walsh FB, Hoyt WF. Clinical Neuro-Ophthalmology. Baltimore: Williams & Wilkins; 1969. pp. 1338–1375. [Google Scholar]
- 7.Azuma M, Morimura Y, Kawahara S, Okada AA. Bilateral anterior optic neuritis in adult measles infection without encephalomyelitis. Am J Ophthalmol. 2002;134:768–769. doi: 10.1016/s0002-9394(02)01632-x. [DOI] [PubMed] [Google Scholar]
- 8.Totan Y, Cekiç O. Bilateral retrobulbar neuritis following measles in an adult. Eye. 1999;13:383–384. doi: 10.1038/eye.1999.102. [DOI] [PubMed] [Google Scholar]
- 9.Shlossberg FR, Prizer M. Retinal changes with marked impairment of vision in measles: report of a case. Am J Ophthalmol. 1940;23:998–1000. [Google Scholar]
- 10.Wagener HP. Edema of the optic discs in cases of encephalitis. Am J Med Sci. 1952;223:205–216. [PubMed] [Google Scholar]
- 11.Bedrossian RH. Neuroretinitis following measles. J Pediatr. 1955;46:329–331. doi: 10.1016/s0022-3476(55)80292-2. [DOI] [PubMed] [Google Scholar]
- 12.Tyler HR. Neurological complication of rubeola (measles) Medicine. 1957;36:147–167. doi: 10.1097/00005792-195705000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy C, Carroll FD. Optic neuritis in measles. Trans Am Acad Ophthalmol Otolaryngol. 1960;64:700–712. [PubMed] [Google Scholar]
- 14.Nakajima H, Hosokawa T, Sugino M, Kimura F, Sugasawa J, Hanafusa T, Takahashi T. Visual field defects of optic neuritis in neuromyelitis optica compared with multiple sclerosis. BMC Neurol. 2010;10:45. doi: 10.1186/1471-2377-10-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trip SA, Schlottmann PG, Jones SJ, Kallis C, Altmann DR, Garway-Heath DF, Thompson AJ, Plant GT, Miller DH. Scanning laser polarimetry quantification of retinal nerve fiber layer thinning following optic neuritis. J Neuroophthalmol. 2010;30:235–242. doi: 10.1097/WNO.0b013e3181dbfeac. [DOI] [PubMed] [Google Scholar]