Abstract
Objective
This study examined the effects (affective reactions, cognitive reactions and processing, perceived benefits and barriers and intent to screen) of targeted Peripheral + Evidential (PE) and Peripheral+Evidential+Socio-cultural (PE+SC) colorectal cancer communications.
Methods
This study was a two-arm randomized control study of cancer communication effects on affective, cognitive processing, and behavioral outcomes over a 22-week intervention. There were 771 African American participants, 45 to 75 years, participating in the baseline survey related to CRC screening. Three follow-up interviews that assessed intervention effects on affective response to the publications, cognitive processing, and intent to obtain CRC screening were completed.
Results
There were no statistically significant differences between PE and PE+SC intervention groups for affect, cognitive processing or intent to screen. However, there were significant interactions effects on outcome variables.
Conclusions
The advantages and disadvantages of PE+SC targeted cancer communications and implications of sex differences are considered.
Practice Implications
While there do not appear to be significant differences in behavioral outcomes when using PE and PE+SC strategies, there appear to be subtle differences in affective and cognitive processing outcomes related to medical suspicion and ethnic identity, particularly as it relates to gender.
1. Introduction
Colorectal cancer (CRC) is the third most common cancer among African American men and women, and the third most common cause of cancer death among African Americans [1]. African American CRC age-adjusted incidence and mortality rates are higher than any other racial/ethnic group [2, 3]. Additionally, while the 5-year CRC survival rates for 1999-2005 improved for African American men and women (55.5% and 56.7% respectively), this improvement was less than that of whites over the same time period (66.3% and 65.9% respectively) [3]. CRC disparity may be partly attributable to differences in African Americans’ screening utilization, which has been linked to later stage CRC diagnosis among African Americans [1, 3]. While the rate of CRC screening has increased, 2005 data indicate that African American screening rates remain below the national objective of 50% established by Healthy People 2010 [4]. In 2005, screening rates were: FOBT, 10.3% for African Americans and any endoscopic procedure (colonoscopy or sigmoidoscopy), 36.9% for African Americans [1]. This illustrates an underutilization of important screening tools, particularly considering the higher African American CRC incidence and mortality rates [5]. Thus, improved CRC screening among African Americans may be a key element in decreasing this health disparity.
The NCI's CECCR initiative recognizes that effective communication can and should be used to help eliminate cancer disparities, including CRC [6]. The specific strategies used to realize this potential could take many forms, but there is widespread agreement that “culturally appropriate” screening information will play a role [7-9]. Brach & Fraser [7] identify nine major cultural competency techniques: interpreter services, recruitment and retention policies, training, coordinating with traditional healers, use of community health workers, culturally competent health promotion, including family/community members, immersion into another culture, and administrative and organizational accommodations. Culturally competent health promotion is believed to involve incorporating culture-specific attitudes and values into messages and materials. Resnicow et al. [8] refer to the “deep structure” of cultural sensitivity, which conveys salience to the target population when incorporated in health promotion programs. Using these approaches, a group's cultural values, beliefs and behaviors are recognized, reinforced, and built upon to provide context and meaning to information and messages about cancer. Yet, surprisingly little is known about what communication effects can be attributed to cultural appropriateness, and whether different approaches to cultural appropriateness will have different effects.
Of the various strategies for targeting health communication [10-11], peripheral, evidential, and socio-cultural strategies have the greatest relevance for printed cancer communication materials. Peripheral approaches enhance effectiveness of communication by packaging content in colors, fonts, images, photographs or declarative titles (e.g., “A guide for African Americans”) likely to appeal to a given group; while evidential approaches [9] provide and discuss data specific to a group. An evidential approach might include statements like “In the U.S., the incidence and mortality rates for colorectal cancer are higher among Blacks than other groups”. Finally, socio-cultural approaches discuss disease in the context of specific social and/or cultural characteristics of the group [10]. “Taking care of your family has always come first. But you have to keep yourself healthy if you're going to be there to help your family in the years ahead.” is an example of a socio-cultural message.
Weinstein's Precaution Adoption Process Model [12] suggests that convincing someone that a risk affects people like him/ her is important in moving them towards precautionary action. Providing race-specific data and/or disparity data in a way designed to communicate risk by appealing to the population may be one way to accomplish this goal, if the data are perceived as more meaningful. However, the addition of positive and the reframing of negative cultural themes have the potential to stimulate the desired sense of relevance, and subsequent movement to precautionary action. Thus, while a peripheral + evidential (PE) approach might be sufficient, a peripheral+evidential+socio-cultural (PE+SC) approach should produce a stronger effect. This may be particularly true among those for whom culture and ethnic identity are very salient [8].
This study reports on the effect of targeted PE and PE+SC cancer communications on affective, cognitive processing, and behavioral outcomes over a 22-week intervention designed to encourage CRC screening. Specifically, this study examines how PE and PE+SC cancer communication strategies effect affective reactions to the publication, cognitive reactions and processing (motivation to process, sense of, and identification), perceived benefits and barriers and intent to screen. In addition, the study relevance examines whether gender and/or cultural attitudes modify these effects.
2. Methods
This research protocol was originally approved by the Saint Louis University Institutional Review Board, with final data collection approved by the Washington University in St. Louis Institutional Review Board. All participants received a detailed explanation of the study before providing signed consent.
2.1 Intervention Materials
Formative research indicated that males reported unique information seeking and communication needs and preferences; thus, separate male and female publications were developed [13]. Publications were full-color and 12 pages in length. The three publications provided core content in three areas related to CRC risk reduction, as follows: (P 1) beliefs about colorectal cancer and screening; (P 2) fruit and vegetable intake to reduce the risk of colorectal cancer; and, (P 3) CRC screening recommendations. For the PE and PE+SC groups, this content was presented in ways that reflected each approach to achieving cultural appropriateness. Evidential screening messages emphasized comparative statistics related to incidence, mortality and screening rates in the African American community, as usually seen in the media. Socio-cultural messages focused on ideals of collectivism and ethnic identity through screening appeals that suggested family and community benefit, and countered issues of mistrust and the desire for privacy by emphasizing how these undermined health and thus the community. Socio-cultural peripherals used localized photos to heighten relevance, as well as those that depicted church, family and community scenes. PE and PE+SC intervention materials did not differ on a scale assessing quality graphics, fonts, paper, etc. (PE Mean, FU1= 4.3, FU2= 4.4, FU3= 4.3 and PE+SC Mean, FU1= 4.3, FU2= 4.4, FU3= 4.3).
2.2 Procedure
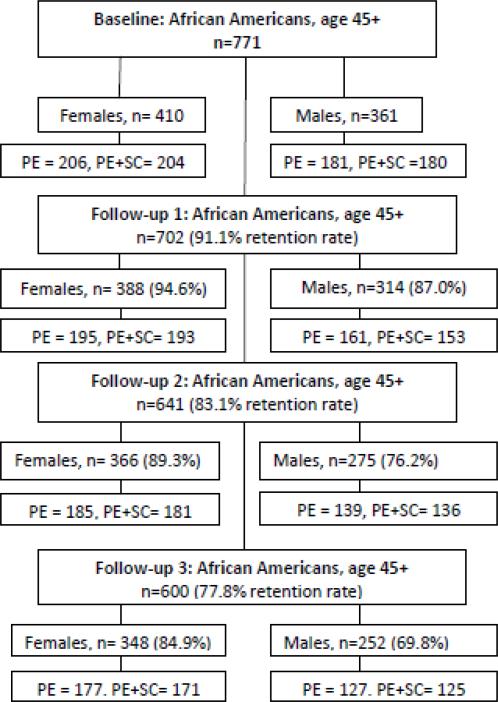
The Elimika Project (“elimika” is Swahili for “to get knowledge”) was a 2-arm randomized controlled trial. Recruitment for the Elimika Project took place between September 2006 and May 2008. Study participants were African-Americans, between the ages of 45 and 75 years, U.S. born, and residents of the targeted recruitment areas. Exclusion criteria included previous diagnosis of CRC and difficulty reading and/or comprehending health literature. There were 771 participants in the study at baseline, with 702, at follow-up 1, 641 at follow-up 2, and 600 at follow-up 3. (See Figure 1 for respondent recruitment and retention rates by gender and study group).
Figure 1.
Respondent recruitment and retention rates by gender and study group
Participants were randomly assigned to receive either: PE or PE+SC publications. Assessments tracked the progression of affective and cognitive effects that resulted from exposure to three CRC reduction publications. The first was given to participants after completing the baseline survey, with an assessment at 2 weeks; and subsequent publications mailed at 10 weeks and 20 weeks, with follow-up (FU) telephone calls at 12- and 22-weeks, respectively post-enrollment.
Participants were recruited from residences located on randomly selected census blocks in urban and suburban segments of a large Midwestern city. To facilitate this community recruitment strategy, only census tracts that were at least 70% African American and had at least 50 residential houses were included (N=500). Some census blocks in segments of the metropolitan area were excluded in order to avoid recruiting individuals participating in other cancer related studies conducted within the same center. Once census blocks were selected, trained recruiters randomized each side of the block to experimental groups to either the PE or the PE+SC experimental group. A random numbers table was used to determine which residence would be approached first. Each residence in the assigned experimental group was approached. Individuals answering their door received the project description and were queried to determine their eligibility; if ineligible they were asked if the recruiter could speak with any household member who might eligible for participation. Recruiters documented those not home, refusals, ineligibility, as well as participation. Only one participant per household was permitted to participate. Each block was visited three times, varied by time of day and day of the week. Due to low enrollment of male participants, the sampling strategy was modified to include a group recruitment strategy beginning in July 2007 (N=177). Predominantly African American group recruitment locations, located within the census blocks selected for individual recruitment, included churches, fraternal organizations, nursing homes, and health fairs where men might be contacted. The experimental condition was determined by coin toss at the time of recruitment. Another 93 participants self-referred for participation through newspaper ads and referrals from family, friends, and organizations that permitted recruitment; and were assigned via coin toss or consistent with the assignment of the referring organization/family/friend.
All recruited individuals were screened for literacy and eligibility was confirmed. To test for literacy, we modified an item used in the 2001 Survey on Disparities in Quality of Health Care. Potential participants were asked to read aloud and respond to the item on a pre-printed eligibility card. [14] Individuals who agreed to participate reviewed and signed an informed consent form and received a demographic form and baseline survey to complete. The demographic survey took 5 to 10 minutes and the baseline survey took approximately 45 to 60 minutes to complete. Immediately after completion of the baseline survey, research assistants hand delivered the first colorectal cancer publication. Participants were instructed to read the publication prior to the telephone follow-up call. Participants received follow-up telephone interviews, which took 30 to 45 minutes to complete, two to three weeks after receiving a publication. Participants received $15 gift certificates for completion of the baseline survey and each subsequent telephone interview.
2.3 Measures
Self-reported baseline data collected for this study included CRC screening history for FOBT, Sigmoidoscopy (Sig), and Colonoscopy (Col), intent to screen, CRC benefits, barriers, sociocultural attitudes (religiosity, fatalism, collectivism, mistrust, ethnic identity) and demographic information. Information was also obtained on diet, physical activity, social desirability, information seeking, family history, healthcare contact, but is not reported for this study. Follow-up data addressed affective response to the publications, cognitive processing, and intent to obtain CRC screening.
The self-reported CRC screening items administered on the baseline survey were adapted from the National Cancer Institute colorectal cancer screening questionnaire developed by Vernon, et al. [15]. The survey queried CRC screening generally, and FOBT, Sig, or Col, specifically. A description of each screening test was provided before its corresponding question. Response options were “yes,” “no,” or “don't know.” Participants who responded “yes” to a test were asked to select a time range for their most recent test and to report the month and year of this test. These items were used to identify participants who never screened, or were screened and adherent or non-adherent [16] based on U. S. Preventive Services Task Force screening guidelines for colorectal cancer [17]. Hood et al. [15] provide a summary of reliability and validity data for the measure when used with African Americans. Intent to screen was assessed by a single item, which asked whether participants had decided against screening, were considering it, planning to or discussing it with a physician, or actively scheduling and seeking screening.
Positive and negative affective responses to the publication were measured using three and four items scales, respectively. Items asked about feelings of interest, motivation, vulnerability, and upset in response to publications. Items were measured on a 5 point Likert scale. Alpha coefficients for the positive affect scale were .70, .69, and .75 at FU 1-3 and .68, .69 and .73 for the negative affect scale.
Cognitive processing responses were measured using a scale that assessed motivation to process (alpha =.75, FU1; .75, FU2; .85, FU3) or participants’ perceptions of the impact, ability to remember, and use the information contained in the publications. Ease of understanding was assessed using two items that queried the ability to understand and follow the content of the publications. Engagement (alpha =.69, FU1; .75, FU2; .71, FU3) addressed participants reported ability to remain free from distraction and focused on publication content. Relevance of publication content (alpha =.68, FU1; .78, FU2; .76, FU3) attempted to capture the participants’ perceptions that the content of the publications was meaningful to them as African Americans. Finally, identification with characters (alpha =.72, FU1; .78, FU2; .85, FU3) addressed the extent to which the images depicted in publications were perceived as similar to participants.
Items assessing benefits and barriers to screening were based on the measure by Rawl, Champion, Menon, Loehrer, Vance, and Skinner [18]. Factor analysis confirmed unidimensionality of the constructs and item loadings. Alpha coefficients for FOBT barriers were .87, FU1; .77, FU2; .82, FU3 and .92, FU1; .84, FU2; .87, FU3 for Scope barriers. CRC screening benefits had alpha coefficients of .82, FU1; .71, FU2; .64, FU3.
Cultural attitudes and ethnic identity were measured to determine the relative effectiveness of targeted publications using different strategies for cultural appropriateness among a diverse African Americans target audience. Ethnic identity was measured at baseline using an adaptation of the ideology dimension of the Multidimensional Model of Racial Identity (MMRI). Factor analysis of the items used yielded four components similar to the original measure.[19-22] A nationalist (alpha= .75) philosophy is described as the ideal that emphasizes the importance and uniqueness of African heritage and descent, an oppressed minority (alpha= .65) ideology addresses the commonalities among oppressed groups, an assimilationist (alpha= .77) philosophy stresses the links between African Americans and the larger American society, and a humanist (alpha= .71) philosophy emphasizes the relationship and similarities among humankind. Evidence for the construct validity of the MMRI was found in an investigation of its corresponding measure, the Multidimensional Inventory of Black Identity (MIBI).[19-20] Other researchers have provided support for the validity of the model and the measure.[21]
Religiosity was defined as the internal manifestation of belief in a higher power, and the genuine, consistent commitment to its attendant values. This construct was measured using five items previously used in similar work [22] with African American females (alpha =.88). The alpha coefficient for the scale in this study was .94. Collectivism was defined as the belief and tendency to subordinate personal goals to those of the group [23]. Three items previously used to measure this construct among African American females (alpha =.85) were modified for this study [21]. The alpha coefficient for the scale in this study was .77. Inequity in healthcare and suspicion of the healthcare system were also measured at baseline. Items assessed the belief that individuals and institutions will act appropriately and perform competently, responsibly, and in a manner consistent with patients’ interests. This construct was measured using three items from the Group Based Medical Mistrust Scale (alpha =.83) [24], developed on a sample that included African American participants. The alpha coefficient for the Inequity in healthcare scale was .73. Suspicion of modern medicine was measured by a single item.
Demographic variables measured included age, sex, highest educational level, employment, marital status, and income. Participants were asked to report their age on their last birthday. Response options for education included “some high school or less,” “high school graduate or GED,” “some college,” or “a least college degree.” Current employment status was indicated by a “yes” or “no” response to a query of status. Participants were asked to report a household income range for the previous year in categories including “< $10,000,” “$10,000 to < $19,999,” “$20,000 to < $39,999,” “$40,000 to < $59,999,” and “≥ $60,000.” In addition, participants reported their marital status as “single,” “married or living with a partner,” “divorced or separated,” or “widowed.” Participants’ insurance status was measured by asking how they paid for health care during the past 12 months.
2.4 Analysis
Participant demographic characteristics and predictor variables between the two intervention groups were described separately among males and females. Comparisons of categorical variables were performed using Pearson's chi-square test, while normally distributed continuous variables were compared using t-test and those not normally distributed using Wilcoxon Mann Whitney test. Factor analysis of the modified scales were performed using appropriate rotations and index scores of the constructs were computed if not more than 25% of the items were missing. Repeated measures, such as affective response, cognitive processing, and intent to screen variables were compared in a similar way at each follow up. After baseline, subsequent measurements were taken at less regular time intervals. Multi-level modeling (MLM) was used to model time as a linear predictor of these outcomes, while possibility of time being a quadratic predictor was also explored. The advantage of MLM (using likelihood-based estimations) is that it incorporates all available time-variant and correlated data regardless of missing data between unequally spaced time intervals. Time-invariant predictors such as fatalism, medical mistrust, religiosity, collectivism and ethnic identity variables were entered into the models as possible moderators. Analysis was carried out using SAS 9.1.2 and all tests were carried out using a two-sided alpha level of 5%. MLM was performed using PROC MIXED with time as level 1 predictor and individual-level covariates were level 2 predictors. Predicted mean of the outcomes across time in each intervention group was presented in graphs.
3. Results
3.1 Sample Characteristics
The demographic characteristics of the sample by sex are presented in Table 1. The mean age was about 56 years for women and 55 years for men. Educational attainment was nearly the same for both groups except having attended some college. More women reported having attended some college (n=160, 39.1%) than men (n=122, 33.8%). Approximately half of participants in both sexes were employed (n=198, 48.4% and n=182, 50.4%, respectively). Women were less likely to earn an income of $40,000 a year or greater (n= 124, 30.2%) compared to men (n=160; 44.2%). An overwhelming majority of participants reported having insurance, with more women being insured (n=310; 75.5%) than men (n=229; 63.4%). While only 29.2% (n=120) of women reported being currently married or living with a partner, more than half of the men (n=184; 51.1%) were married or partnered. Experimental groups were not significantly different by demographic characteristics.
Table 1.
Demographics of the study population by gender, N=771
| Demographics | Male =361 |
Female =410 |
||||||
|---|---|---|---|---|---|---|---|---|
| E | SC | Total | p | E | SC | Total | p | |
| Age, mean (SD) | 55.1 (7.6) | 54.2 (7.7) | 54.7 (7.6) | .29 | 56.6 (8.0) | 55.9 (8.4) | 56.3 (8.2) | .43 |
| 32-50, % | 32.8 | 38.8 | 35.7 | .24 | 27.0 | 31.5 | 29.2 | .31 |
| 51-79, % | 67.2 | 61.2 | 61.2 | 73.0 | 68.5 | 70.8 | ||
| Education,% | ||||||||
| Not completed HS | 14.1 | 13.5 | 13.8 | .88 | 9.4 | 12.6 | 11.0 | .12 |
| Graduated HS | 24.9 | 28.7 | 26.8 | 22.3 | 30.2 | 26.2 | ||
| Some college | 35.0 | 32.5 | 33.8 | 41.1 | 37.2 | 39.1 | ||
| College/ graduate degree | 26.0 | 25.3 | 25.6 | 27.2 | 20.1 | 23.7 | ||
| Income, % | ||||||||
| <$10,000 | 16.7 | 17.9 | 17.3 | .77 | 16.3 | 16.3 | 16.3 | .99 |
| $10,000-$19,999 | 14.8 | 18.5 | 16.7 | 22.3 | 23.4 | 22.8 | ||
| $20,000-$39,999 | 24.1 | 20.1 | 21.9 | 31.0 | 30.4 | 30.7 | ||
| $40,000-$59,999 | 17.9 | 15.4 | 16.7 | 18.5 | 16.8 | 17.7 | ||
| >$60,000 | 26.5 | 28.4 | 27.5 | 12.0 | 13.0 | 12.5 | ||
| Employed, | ||||||||
| No | 52.8 | 46.3 | 49.6 | .22 | 50.3 | 53.0 | 51.6 | .58 |
| Yes | 47.2 | 53.7 | 50.4 | 49.7 | 47.0 | 48.4 | ||
| Marital status, % | ||||||||
| Single | 26.8 | 27.7 | 27.3 | .94 | 25.0 | 27.0 | 26.0 | .65 |
| Married/ partnered | 50.8 | 51.4 | 51.1 | 27.9 | 30.5 | 29.2 | ||
| Divorced/ separated/ widowed | 22.4 | 20.9 | 21.6 | 47.0 | 42.5 | 44.8 | ||
| Insurance status, % | ||||||||
| Out of pocket/ Govt. clinics/ un-insured | 33.1 | 40.4 | 36.6 | .20 | 26.4 | 22.6 | 24.5 | .42 |
| Some insurance | 66.9 | 59.6 | 63.4 | 73.6 | 77.4 | 75.5 | ||
All values presented are in percentages except age (as mean and standard deviation) P-values: Pearson's chi-square test for categorical variables (Fisher's exact test when cell sizes are small) and student t-test for comparing age
3.2 Intervention Effects
There were no statistically significant main effects of intervention group for positive and negative affect, motivation to process, ease of understanding and engagement, relevance, identification with characters, and counter-arguing, or intent to screen. At FU2 (PE Mean =3.7 vs. PE+SC Mean 3.8, p<.05) and FU3 (PE Mean =3.6 vs. PE+SC Mean 3.8, p<.01), female participants reported greater “likelihood to pick up and read” PE+SC publications vs. PE publications. Two-level models examining the effects of interventions (study groups), time in days after intervention, socio-cultural variables, interaction of time and intervention, interaction of time and socio-cultural variables, interaction of intervention and socio-cultural variables, interaction of time, intervention and socio-cultural variables were developed. The models examined indicated that change in CRC screening status between the two intervention groups across time were not significant; however, models indicated that there were significant interaction effects.
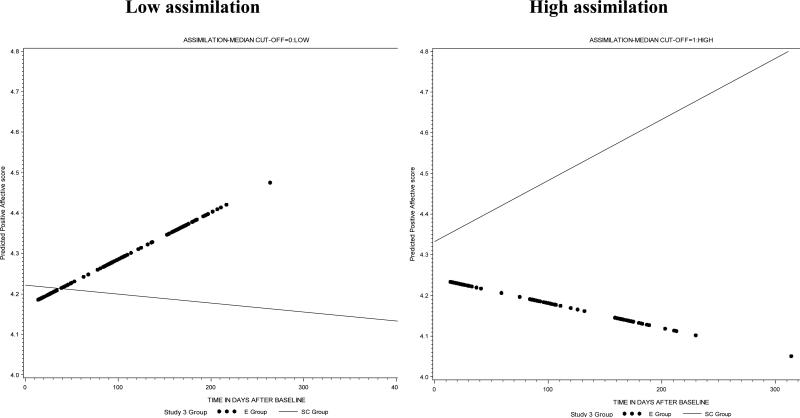
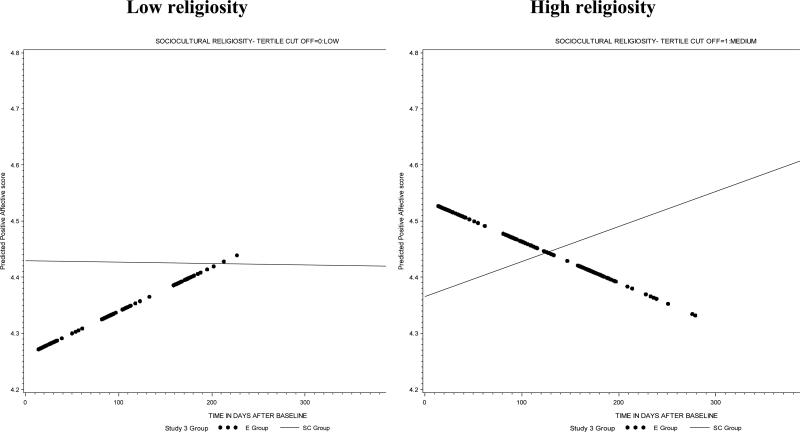
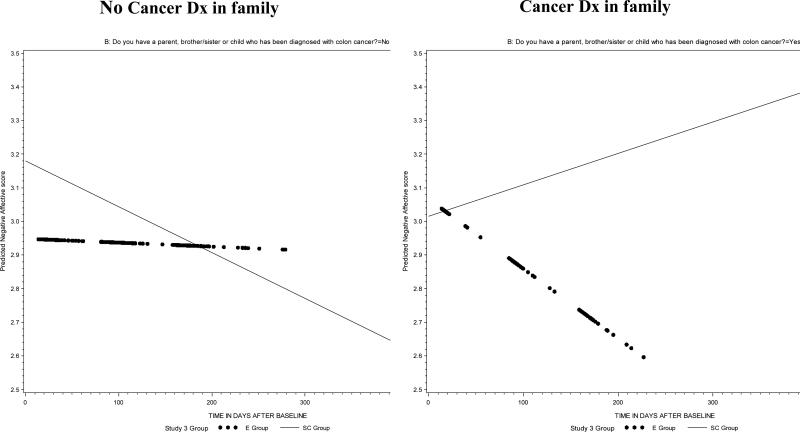
After adjusting for religiosity, among men who reported low assimilation, the PE group showed a marked increase in positive affective score across time and the PE+SC group scores decreased. There was a reverse association among men who reported high assimilation scores, where an increase was seen in positive affect scores in the PE+SC group and scores decreased in the PE group. After adjusting for assimilation, among women who reported low religiosity, an increase in the positive affect score was observed in the PE group. Among those who reported higher religiosity, the PE group showed a reduction in positive affect scores while an increase in positive affect scores was observed in the PE+SC group (Table 2). Among women, reports of negative emotions reduced with time in both groups if there was no family history of cancer; the decrease was greater in the PE+SC than the PE group. If there was a family history of cancer, negative emotions decreased with time in the PE group but increased in the PE+SC group (Table 3).
Table 2.
Positive affective score among men who have never had any CRC screening test or are not adherent to CRC screening guidelines, N=346
| Model 1 |
Model 2 |
|||||
|---|---|---|---|---|---|---|
| Coefficient |
SE |
p |
Coefficient |
SE |
p |
|
| Fixed effects | ||||||
| Mean positive affective score | 4.20 | 0.06 | <.01 | 3.86 | 0.15 | <.01 |
| Intervention | ||||||
| Evidential | Reference | Reference | ||||
| Socio-cultural | 0.05 | 0.09 | 0.58 | 0.04 | 0.11 | 0.73 |
| Time | 0.0005 | 0.0004 | 0.27 | 0.0002 | 0.0005 | <.05 |
| Time × Intervention | 0.0001 | 0.001 | 0.93 | -0.001 | 0.001 | 0.07 |
| Assimilation | 0.08 | 0.13 | 0.53 | |||
| Intervention × Assimilation | 0.04 | 0.18 | 0.82 | |||
| Time × Assimilation | -0.002 | 0.001 | 0.08 | |||
| Time × Intervention × Assimilation | 0.003 | 0.001 | <.01 | |||
| Sociocultural: Religiosity | 0.10 | 0.04 | <.05 | |||
| Random effects | Variance | SE | p | Variance | SE | p |
| Level 1 effect (within person) | 0.20 | 0.02 | <.01 | 0.19 | 0.02 | <.01 |
| Level 2 effects | ||||||
| In initial status | 0.32 | 0.05 | <.01 | 0.31 | 0.05 | <.01 |
| Model fit | ||||||
| -2LL/ Deviance | 1529.8 | 1445.6 | ||||
| AIC | 1537.8 | 1453.6 | ||||
Table 3.
Negative affective score among women who have never had any CRC screening test or are not adherent to CRC screening guidelines, N=386
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | p | Coefficient | SE | p | Coefficient | SE | p | |
| Fixed effects | |||||||||
| Mean negative affective score | 2.99 | 0.08 | <.01 | 2.57 | 0.18 | <.01 | 2.63 | 0.21 | <.01 |
| Intervention | |||||||||
| Evidential | Reference | Reference | Reference | ||||||
| Socio-cultural | 0.19 | 0.11 | .09 | 0.20 | 0.12 | 0.10 | 0.19 | 0.19 | .32 |
| Time | -0.001 | 0.0005 | <.05 | -0.0002 | 0.001 | .78 | -0.001 | 0.001 | .14 |
| Time × Intervention | -0.001 | 0.001 | .30 | -0.001 | 0.001 | .11 | 0.001 | 0.001 | .22 |
| Cancer Dx in family | 0.14 | 0.20 | .49 | ||||||
| Intervention × Cancer Dx in family | -0.29 | 0.32 | .37 | ||||||
| Time × Cancer Dx in family | -0.002 | 0.001 | 0.11 | ||||||
| Time × Intervention × Cancer Dx in family | 0.004 | 0.002 | <.05 | ||||||
| Religiosity | 0.03 | 0.16 | .87 | ||||||
| Intervention × Religiosity | 0.04 | 0.23 | .87 | ||||||
| Time × Religiosity | 0.001 | 0.001 | .31 | ||||||
| Time × Intervention × Religiosity | -0.003 | 0.001 | <.05 | ||||||
| Fatalism | 0.25 | 0.11 | <.05 | 0.21 | 0.11 | <.05 | |||
| Random effects | Variance | SE | p | Variance | SE | p | Variance | SE | p |
| Level 1 effect (within person) | 0.46 | 0.03 | <.01 | 0.45 | 0.03 | <.01 | 0.46 | 0.03 | <.01 |
| Level 2 effects | |||||||||
| In initial status | 0.53 | 0.08 | <.01 | 0.53 | 0.08 | <.01 | 0.54 | 0.08 | <.01 |
| Model fit | |||||||||
| -2LL/ Deviance | 2673.4 | 2560.8 | 2534.1 | ||||||
| AIC | 2679.4 | 2566.8 | 2540.1 | ||||||
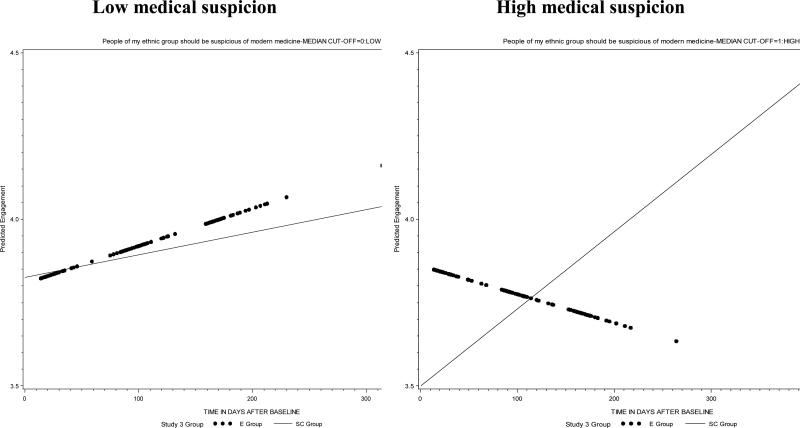
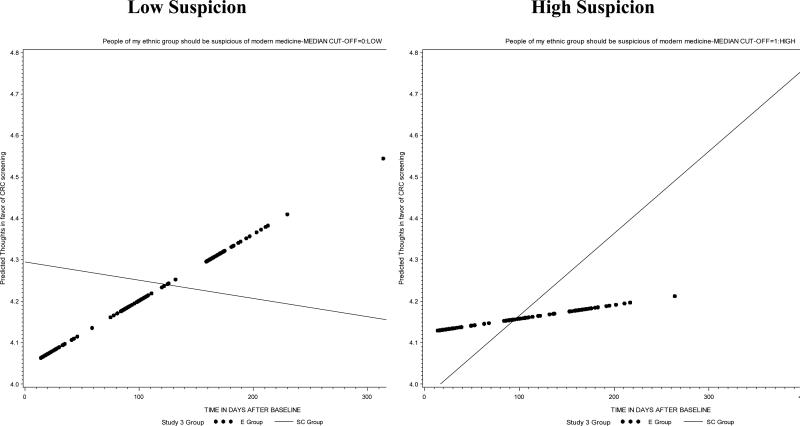
Among men who report low medical suspicion, PE and PE+SC groups showed an increase in engagement while reading the publication; however, among those who reported a higher degree of medical suspicion, the PE intervention considerably decreased their engagement as compared to PE+SC intervention, which showed a significant increase in engagement while reading the publication (Table 4). Among women who reported low medical suspicion, after adjusting for fatalism, the PE+SC group showed an increase in engagement while the PE group did not show a significant increase after reading the publication. Among those who reported a higher degree of medical suspicion, the PE intervention considerably increased their engagement while reading the publication as compared to PE+SC intervention which showed a reduction in engagement while reading the publication (Table 4B). Among participants who reported high medical suspicion, those in the PE+SC intervention reported increased thoughts that favored CRC screening; while those low suspicion reported fewer favorable thoughts across time. The effect was reversed in the PE condition. Among the PE group, a general increase was noted, but favorable thoughts increased among those who had low suspicion compared to those who had high suspicion (Table 5).
Table 4.
Cognitive measure: Engagement among men who have never had any CRC screening test or are not adherent to CRC screening guidelines, N=346
| Model 1 |
Model 2 |
|||||
|---|---|---|---|---|---|---|
| Coefficient |
SE |
p |
Coefficient |
SE |
p |
|
| Fixed effects | ||||||
| Mean engagement score | 3.84 | 0.08 | <.01 | 3.78 | 0.38 | <.01 |
| Intervention | ||||||
| Evidential | Reference | Reference | ||||
| Socio-cultural | -0.10 | 0.11 | .34 | -0.31 | 0.27 | 0.25 |
| Time | 0.0002 | 0.0005 | .73 | -0.002 | 0.001 | 0.16 |
| Time × Intervention | 0.001 | 0.001 | .27 | 0.003 | 0.002 | 0.08 |
| Medical suspicion | -0.46 | 0.23 | <.05 | |||
| Intervention × Medical suspicion | 0.69 | 0.33 | <.05 | |||
| Time × Medical suspicion | 0.004 | 0.002 | <.05 | |||
| Time × Intervention × Medical suspicion | -0.01 | 0.002 | <.05 | |||
| Information seeking satisfaction | 0.28 | 0.09 | <.01 | |||
| Oppressed minority | -0.09 | 0.04 | <.05 | |||
| Random effects | Variance | SE | p | Variance | SE | p |
| Level 1 effect (within person) | 0.33 | 0.03 | <.01 | 0.28 | 0.04 | <.01 |
| Level 2 effects | ||||||
| In initial status | 0.45 | 0.08 | <.01 | 0.34 | 0.10 | <.01 |
| Model fit | ||||||
| -2LL/ Deviance | 1846.4 | 651.6 | ||||
| AIC | 1854.4 | 659.6 | ||||
Table 5.
Thoughts favoring CRC screening among men who have never had any CRC screening test or are not adherent to CRC screening guidelines, N=346
| Model 1 |
Model 2 |
|||||
|---|---|---|---|---|---|---|
| Coefficient |
SE |
p |
Coefficient |
SE |
p |
|
| Fixed effects | ||||||
| Mean of thoughts favor CRC screening | 4.19 | 0.06 | <.01 | 4.26 | 0.08 | <.01 |
| Intervention | ||||||
| Evidential | -0.11 | 0.09 | .21 | -0.23 | 0.12 | <.05 |
| Socio-cultural | Reference | Reference | ||||
| Time | 0.0004 | 0.0005 | .44 | -0.0005 | 0.001 | .45 |
| Time × Intervention | 0.001 | 0.001 | .30 | 0.002 | 0.001 | <.05 |
| Medical mistrust: Suspicion | -0.27 | 0.14 | <.05 | |||
| Intervention × Suspicion | 0.39 | 0.19 | <.05 | |||
| Time × Suspicion | 0.002 | 0.001 | <.05 | |||
| Time × Intervention × Suspicion | -0.004 | 0.002 | <.01 | |||
| Diagnosis of polyps | 0.25 | 0.09 | <.01 | |||
| Random effects | Variance | SE | p | Variance | SE | p |
| Level 1 effect (within person) | 0.27 | 0.03 | <.01 | 0.27 | 0.03 | <.01 |
| Level 2 effects | ||||||
| In initial status | 0.19 | 0.05 | <.01 | 0.18 | 0.05 | <.01 |
| In rate of change | 7.28 | 3.80 | <.05 | 7.11 | 3.79 | <.05 |
| Covariance | -0.001 | 0.0004 | <.05 | -0.001 | 0.0004 | <.05 |
| Model fit | ||||||
| -2LL/ Deviance | 1466.5 | 1325.1 | ||||
| AIC | 1474.5 | 1333.1 | ||||
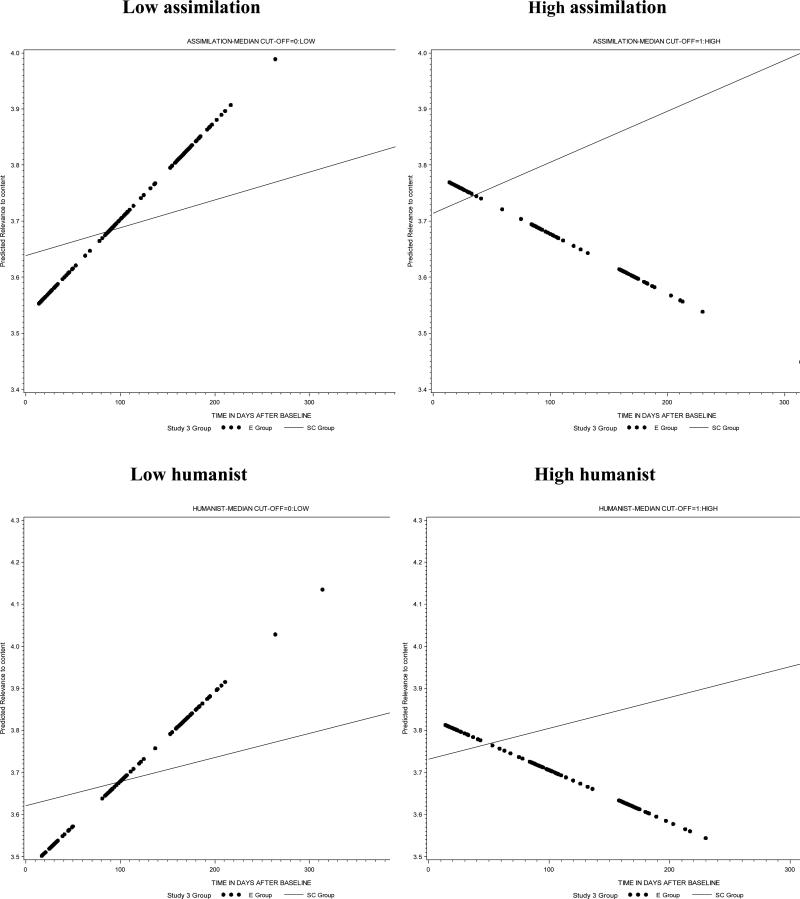
There was an increase in relevance of content scores for the PE+SC group across time, after adjusting for religiosity irrespective of assimilation. The PE group demonstrated an increase in relevance of content scores when reported assimilation was low and decreased scores when reporting higher assimilation. Similarly, the PE+SC group showed an increase in relevance of content score across time, after adjusting for religiosity, irrespective of humanist score; however, the content relevance scores for the PE group increased when there were low humanists score and a decreased when reporting higher humanist scores (Table 6).
Table 6.
Relevance to content among men who have never had any CRC screening test or are not adherent to CRC screening guidelines, N=346
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | p | Coefficient | SE | p | Coefficient | SE | p | |
| Fixed effects | |||||||||
| Mean relevance to content score | 3.63 | 0.07 | <.01 | 3.02 | 0.16 | <.01 | 3.0 | 0.16 | <.01 |
| Intervention | |||||||||
| Evidential | Reference | Reference | Reference | ||||||
| Socio-cultural | 0.06 | 0.10 | .54 | 0.10 | 0.14 | .46 | 0.11 | 0.14 | .43 |
| Time | 0.001 | 0.001 | .19 | 0.001 | 0.001 | <.01 | 0.002 | 0.001 | <.01 |
| Time × Intervention | -0.0001 | 0.001 | .88 | -0.001 | 0.001 | .21 | -0.002 | 0.001 | .13 |
| Assimilation | 0.28 | 0.15 | .06 | ||||||
| Intervention × Assimilation | -0.23 | 0.22 | .29 | ||||||
| Time × Assimilation | -0.003 | 0.002 | <.01 | ||||||
| Time × Intervention × Assimilation | 0.003 | 0.002 | <.05 | ||||||
| Humanist | 0.32 | 0.15 | <.05 | ||||||
| Intervention × Humanist | -0.23 | 0.21 | .28 | ||||||
| Time × Humanist | -0.003 | 0.001 | <.01 | ||||||
| Time × Intervention × Humanist | 0.004 | 0.002 | <.05 | ||||||
| Sociocultural: | 0.16 | 0.04 | <.05 | 0.16 | 0.04 | <.01 | |||
| Religiosity | |||||||||
| Random effects | Variance | SE | p | Variance | SE | p | Variance | SE | p |
| Level 1 effect (within person) | 0.23 | 0.02 | <.01 | 0.25 | 0.02 | <.01 | 0.25 | 0.02 | <.01 |
| Level 2 effects | |||||||||
| In initial status | 0.47 | 0.07 | <.01 | 0.46 | 0.07 | <.01 | 0.46 | 0.07 | <.01 |
| Model fit | |||||||||
| -2LL/ Deviance | 1638.7 | 1586.9 | 1578.1 | ||||||
| AIC | 1646.7 | 1594.9 | 1586.1 | ||||||
4. Discussion and Conclusion
4.1 Discussion
While there were no effects of cultural appropriateness strategy, there were important interactions between socio-cultural variables and cultural appropriateness strategy. The cultural attitudes that proved most important to intervention response were medical suspicion and ethnic identity status. The interaction effects were more prevalent among men. Both men and women with higher assimilationist and humanist identity scores reported increased positive affect in PE+SC condition. The family appeals of the PE+SC publications may have overcome the anticipated antipathy toward racial group appeals expected from those high in these two racial identity attitudes. In general, men high in medical suspicion reported greater publication engagement in the PE condition; however, favorable thoughts related to screening and positive affect were in response to PE+SC publications. Perhaps males reporting high medical suspicion were more engrossed because they were distrustful of the factual data presented. It may be that culturally familiar PE+SC strategies that consider the family and group benefit of CRC screening help men to put aside suspicions and concerns related to medical recommendations. The fact that over half of the men in the sample were married or partnered might have also influenced their family feelings and therefore the appeal of the PE+SC material. Of note, content relevance was high among male participants in the PE+SC condition, regardless of ethnic identity status and varied in the PE group by humanistic and assimilationist identity status.
After adjusting for assimilation, among women who reported low religiosity, an increase in the positive affect score was observed in the PE group, while who reported higher religiosity showed a reduction in positive affect scores. There was an increase in positive affect scores observed in the PE+SC group. Inherent in African American cultural beliefs/values is a religious perspective, which was reflected in the PE+SC; thus, it would make sense that more religious African American women would have an increased positive affect toward PE+SC material.
Perceived relevance of content was significant in both the PE and PE+SC intervention groups, under different conditions of individual religiosity and ethnic identity. However, relevance of content was not associated with any outcomes; although theoretically is should serve as a mechanism of action [7-8]. It is plausible that the diversity of religiosity and ethnic identity observed in a targeted sample makes it difficult to discern this mechanism of action, which might be more readily observed in response to tailored communication materials. It is likely that while some elements of culture used to increase perceptions of relevance were salient, others were not. Thus, responses to those that are salient may mute responses to those that are not.
Interestingly, family history of cancer also interacted with cultural appropriateness strategy. Women with no family history of cancer reported less negative affect related to cancer screening in the PE+SC group, while those with a family history of cancer reported less negative affect in the PE condition and greater negative affect in the PE+SC condition. PE+SC appeals are personal and relate strongly to group and family protection against cancer, which may be distressful in cases where a family member already has a diagnosis.
The limitations of these findings must be considered. First, while the group recruitment strategy introduced some bias, we believe that by adhering to inclusion/exclusion and block criteria and varying the locations used to recruit, we minimized this bias as much as possible. In addition, the resulting sample is more representative because we were able to include more male participants.
Additionally, the effect sizes of the interactions observed, while statistically significant, were small. There were also a number of cognitive processing variables, motivation to process, attention, and ease of understanding for which there were no main or interaction effects. The relative importance of these cognitive processing variables is unknown and the lack of effect on the cognitive outcomes may be as important as the effects on those cognitive processing variables previously noted. Lastly, a socio-cultural variable associated with outcomes, medical suspicion, was measured using a single item. A more comprehensive measure of this construct might yield different findings.
4.2 Conclusion
Although subtle and dependent upon the individual cultural attitudes and beliefs of members of the target audience, there are differential affective and cognitive processing responses to PE and PE+SC cancer communications. However, this intervention failed to demonstrate that these differences in positive and negative affect related to screening, engagement with the publication, relevance of content, and counter-arguing resulted in changes in intent to obtain CRC screening or screening status. The data do suggest several benefits of PE+SC strategies over PE strategies. First, PE+SC strategies produced a sense of content relevance across ethnic identity statuses, which was not true of PE strategies. For this reason, PE+SC strategies may have greater utility when ethnic identity status is known to be highly variable in a community. In addition, the PE+SC publications demonstrated some capacity to generate positive affective reactions to screening messages among individuals whose racial identity attitudes would suggest the opposite response. Thus, they may be capable of appealing to those for whom medical suspicion is an issue without offending those for whom racial identity is not a major issue. Finally, previous studies of the role of culture in cancer communication demonstrated its importance in communications to women [10]. In this study, PE+SC effects were stronger among men. For this reason, future research should consider whether there are specific cultural constructs related to gender and masculinity/femininity that are important to address when promoting screening for male or female specific cancers (e.g., prostate and testicular or breast and cervical cancers), in addition to examining gender specific responses to religious, spiritual, and fatalistic, etc. messages. In addition, research should explore responses to publications when gender specific cultural constructs are incorporated into cancer communication messages, as well as how these might interact with gender specific barriers that influence cancer screening among African American older adults.
4.2 Practice Implications
The findings of this study suggest the role that a socio-cultural strategy to cultural appropriateness can play in targeted cancer communications. While there do not appear to be significant differences in behavioral outcomes when using PE and PE+SC strategies, there appear to be subtle differences in affective and cognitive processing outcomes related to medical suspicion and ethnic identity, particularly as it relates to gender. Because there may be ways that affective and cognitive processing variables effect CRC screening behavior over a longer time than examined in this study, these differences may be prove important. A more clinical implication of these findings relates to the use of PE+SC strategies to convey the importance and benefits of early screening targeted to those with a family history of cancer. For example, PE+ SC publications may have more appeal in showing the relevance of screening among first degree relatives and in conveying the ability to care for a family member with cancer. For this reason and because of the strengths of PE+SC publications noted above, they are a preferred targeted cancer communication strategy unless time and/or cost make them prohibitive.
Fig 2.
Based on model 2 of table 2
Fig 2B.
Based on model 2 of table 2B
Fig 3.
Based on model 2 of table 3
Fig 4.
Based on model 2 of table 4
Fig 5.
Based on model 2 of table 5
Fig 6.
Based on model 2 of table 6
Table 2B.
Positive affective score among women who have never had any CRC screening test or are not adherent to CRC screening guidelines, N=386
| Model 1 |
Model 2 |
Model 3 |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Coefficient |
SE |
p |
Coefficient |
SE |
p |
Coefficient |
SE |
p |
|
| Fixed effects | |||||||||
| Mean positive affective score | 4.45 | 0.05 | <.01 | 3.94 | 0.16 | <.01 | 4.18 | 0.23 | <.01 |
| Intervention | |||||||||
| Evidential | Reference | Reference | Reference | ||||||
| Socio-cultural | -0.09 | 0.07 | .20 | 0.17 | 0.11 | .12 | -0.35 | 0.3 | .17 |
| Time | -0.0002 | 0.003 | .57 | 0.001 | 0.001 | .20 | -0.003 | 0.002 | <.01 |
| Time × Intervention | -0.001 | 0.0005 | .25 | -0.001 | 0.001 | .37 | 0.004 | 0.002 | <.01 |
| Religiosity | 0.25 | 0.10 | 0.40 | ||||||
| Intervention × Religiosity | -0.32 | 0.14 | <.05 | ||||||
| Time × Religiosity | -0.001 | 0.001 | <.05 | ||||||
| Time × Intervention × Religiosity | 0.002 | 0.001 | <.05 | ||||||
| Age | -0.06 | 0.1 | .58 | ||||||
| Intervention × Age | 0.18 | 0.1 | .22 | ||||||
| Time × Age | 0.002 | 0.001 | <.01 | ||||||
| Time × Intervention × Age | -0.002 | 0.001 | <.05 | ||||||
| Assimilation | 0.06 | 0.03 | <.05 | 0.06 | 0.03 | <.05 | |||
| Random effects | Variance | SE | p | Variance | SE | p | Variance | SE | p |
| Level 1 effect (within person) | 0.20 | 0.02 | <.01 | 0.20 | 0.02 | <.01 | 0.20 | 0.02 | <.01 |
| Level 2 effects | |||||||||
| In initial status | 0.18 | 0.04 | <.01 | 0.14 | 0.04 | <.01 | 0.15 | 0.04 | <.01 |
| Model fit | |||||||||
| -2LL/ Deviance | 1817.2 | 1691.9 | 1720.6 | ||||||
| AIC | 1825.2 | 1699.9 | 1728.6 | ||||||
Acknowledgements
We wish to acknowledge the role of our scientific team in the conception and design of this project: Debra Haire Joshu, Eddie Clark, Anjali Deshpande, and Robert Nicholson.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Vetta L. Sanders Thompson, Washington University in St. Louis, George Warren Brown School St. Louis, MO, United States.
Bindu Kalesan, Washington University in St. Louis, Health Communication Research Laboratory St. Louis, MO, United States.
Anjanette Wells, Washington University in St. Louis, George Warren Brown School of Social Work St. Louis, MO, United States.
Sha-Lai Williams, Washington University in St. Louis, George Warren Brown School of Social Work St. Louis, MO United States.
Nicole M. Caito, Washington University in St. Louis, Health Communication Research Laboratory St. Louis, MO, United States
References
- 1.American Cancer Society . Cancer Facts & Figures for African Americans 2009. American Cancer Society; Atlanta, GA: 2009. [Google Scholar]
- 2.Centers for Disease Control and Prevention Comparing Colorectal Cancer by Race and Ethnicity. http://www.cdc.gov/CANCER/colorectal/statistics/race.htm, October 20, 2009.
- 3.Horner MJ, Ries LAG, Krapcho M, Neyman N, Aminou R, Howlader N, Altekruse SF, Feuer EJ, Huang L, Mariotto A, Miller BA, Lewis DR, Eisner MP, Stinchcomb DG, Edwards BK, editors. SEER Cancer Statistics Review, 1975-2006. National Cancer Institute; Bethesda, MD: 2009. http://seer.cancer.gov/csr/1975_2006/, based on November 2008 SEER data submission, posted on the SEER web site. [Google Scholar]
- 4.Byers T, Levin B, Rothenberger D, Dodd G, Smith R. American Cancer Society guidelines for screening and surveillance for early detection of colorectal polyps and cancer: Update 1997. American Cancer Society Detection and Treatment Advisory Group on Colorectal Cancer. CA - Cancer J Clin. 1997;47:154–60. doi: 10.3322/canjclin.47.3.154. [DOI] [PubMed] [Google Scholar]
- 5.U. S. Department of Health and Human Services . Healthy People 2010 Objectives. US Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 6.National Cancer Institute . NIH Guide: Centers of Excellence in Cancer Communications Research - Request for Applications (CA-03-007) National Cancer Institute; Bethesda, MD: 2002. [Google Scholar]
- 7.Brach C, Fraser I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med Care Res Rev. 2000;57:181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Resnicow K, Baranowski T, Ahluwalia J, Braithwaite R. Cultural sensitivity in public health: Defined and demystified. Ethnic Dis. 1999;9:10–21. [PubMed] [Google Scholar]
- 9.Bechtel G, Davidhizar R. Integrating cultural diversity in patient education. Semin Nurs Manage. 2000;7:193–7. [PubMed] [Google Scholar]
- 10.Kreuter M, Lukwago S, Bucholtz D, Clark E, Thompson Sanders V. Achieving cultural appropriateness in health promotion programs: Targeted and tailored approaches. Health Educ Behav. 2003;30:133–46. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- 11.Rogler LH, Malgady RG, Costantino G, et al. What do culturally sensitive mental health services mean? Am Psychol. 1987;42:565–70. doi: 10.1037//0003-066x.42.6.565. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein N, Sandman P. A model of the precaution adoption process: Evidence from home radon testing. Health Psychol. 1992;11:170–80. doi: 10.1037//0278-6133.11.3.170. [DOI] [PubMed] [Google Scholar]
- 13.Thompson Sanders V, Talley M, Caito N, Kreuter M W. African American Men: Perceptions of Factors Influencing Health Information Seeking. Am J Mens Health. 2009;3:6–15. doi: 10.1177/1557988307304630. DOI:10.1177/1557988307304630. [DOI] [PubMed] [Google Scholar]
- 14.Princeton Survey Research Associates for the Commonwealth Fund [June 2007];Survey on Disparities in Quality of Health Care: Spring 2001. http://www.commonwealthfund.org/usr_doc/qualitysurvey_2001_questionnaire.pdf.
- 15.Vernon SM, Meissner H, Klabunde C, Rimer BK, Ahnen DJ, Bastani R, Mandelson MT, Nadel MR, Sheinfeld-Gorin S, Zapka J. Measures for ascertaining use of colorectal cancer screening in behavioral, health services, and epidemiologic research. Cancer Epidem Biomar. 2004;13:898–905. [PubMed] [Google Scholar]
- 16.Hood S, Thompson Sanders VL, Cogbill S, Arnold L, Talley M, Caito N. African American's Self-Report Patterns Using the National Cancer Institute Colorectal Cancer Screening Questionnaire. J Cancer Educ. 2010 doi: 10.1007/s13187-010-0068-z. DOI: 10.1007/s13187-010-0068-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S. Preventive Services Task Force . Screening for colorectal cancer: Recommendations and rationale. Agency for Healthcare Research and Quality; Rockville, MD: Jul, 2002. [Google Scholar]
- 18.Rawl S, Champion V, Menon U, Loehrer PJ, Vance GH, Skinner CS. Validation of scales to measure benefits of and barriers to colorectal cancer screening. J Psychosoc Oncol. 2001;19:47–63. [Google Scholar]
- 19.Sellers RM, Rowley S, Chavous T, Shelton N, Smith M. Multidimensional Model of Racial Identity: A reconconceptualization of African American racial identity. Pers Soc Psychol Rev. 1998;2:18–39. doi: 10.1207/s15327957pspr0201_2. [DOI] [PubMed] [Google Scholar]
- 20.Sellers RM, Rowley S, Chavous T, Shelton N, Smith M. Multidimensional Inventory of Black Identity: A preliminary investigation of reliability and construct validity. J Pers Soc Psychol. 1997;73:805–15. [Google Scholar]
- 21.Cokley K, Helm K. Testing the construct validity of scores on the multidimensional inventory of black identity. Meas Eval Couns Dev. 2001;34:80–95. [Google Scholar]
- 22.Lukwago SN, Kreuter MW, Bucholtz DC. Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Fam Community Health. 2001;24:63–71. doi: 10.1097/00003727-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Triandis H. Culture and social behavior. McGraw-Hill, Inc.; New York, NY: 1994. [Google Scholar]
- 24.Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The group-based medical mistrust scale: psychometric properties and association with breast cancer screening. Prev Med. 2004;38:209–18. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]