Abstract
Objectives
To evaluate the efficacy of behavioral weight control intervention combined with a peer-enhanced activity intervention versus structured aerobic exercise in decreasing BMI and z-BMI in overweight adolescents.
Study design
Participants were randomized to one of two group-based treatment conditions: 1) cognitive behavioral treatment combined with peer enhanced adventure therapy (CBT+PEAT) or 2) cognitive behavioral weight control treatment combined with supervised aerobic exercise (CBT+EXER). Participants included 118 overweight adolescents, ages 13 – 16 years, and a primary caregiver. Changes in body mass index (BMI), standardized BMI, percent over BMI, and waist circumference were examined.
Results
Analysis of variance based on intent to treat (ITT) indicated significant decreases in all weight change outcomes at end of treatment, with significant decreases maintained at 12-month follow-up. No differences between treatment conditions were observed. Secondary analyses indicated that adherence with attendance and completion of weekly diet records contributed significantly to reductions in BMI.
Conclusions
A cognitive behavioral weight control intervention combined with supervised aerobic exercise or peer-enhanced adventure therapy is equally effective in short-term reduction of BMI and z-BMI among overweight adolescents. Adherence, as measured by session attendance and self-monitoring, is a key dimension of weight change.
Overweight children and adolescents face a multitude of medical and psychosocial challenges, including type 2 diabetes, significant impairments in quality of life8, 9, self-concept10, and relations with peers.11 Comprehensive weight control interventions, including dietary and physical activity prescription combined with cognitive-behavioral treatment, have been found effective with school age children.12,13 Notably fewer lifestyle weight control interventions have been conducted with adolescents, although these do show promise in decreasing adolescent obesity rates.14,15 Novel intervention approaches for weight loss in adolescents are needed.
One promising adjunct to cognitive-behavioral treatment (CBT) for adolescent weight control involves peer-based ‘adventure therapy’. Intervention based on adventure therapy is designed to increase self-confidence and support within the peer group as well as to develop a greater level of physical agility, constructs that have been found to relate to increased levels of physical activity in adolescents.16 In a previously reported randomized trial evaluating the efficacy of group based cognitive-behavioral treatment (CBT) plus a peer-based physical activity intervention compared with CBT plus supervised exercise for overweight adolescents, we noted an average reduction of 1.75 BMI units across both intervention conditions.17 Although there was no significant difference between the two treatments, a greater percentage of adolescents receiving peer-based intervention maintained an absolute weight loss of ten pounds or more at 10-month follow-up.
The objectives of the current study were to evaluate the efficacy of this same peer intervention in a second study with a larger sample size, as well as to evaluate the role of treatment adherence on weight related outcomes. The peer intervention, “adventure therapy”, is based on the principles of Outward Bound@, and was expected to impact weight status through a positive effect on self-concept. It was hypothesized that adolescents randomized to CBT combined with peer enhanced adventure therapy (CBT+PEAT) would demonstrate greater reduction in BMI and z-BMI than adolescents randomized to CBT with exercise (CBT+EXER). It was also hypothesized that adolescents randomized to CBT+PEAT would demonstrate greater improvements in self-concept than those randomized to CBT+EXER. Finally, treatment adherence, as reflected by session attendance and completion of diet records, was expected to be positively associated with weight-related outcomes across treatment conditions.
Methods
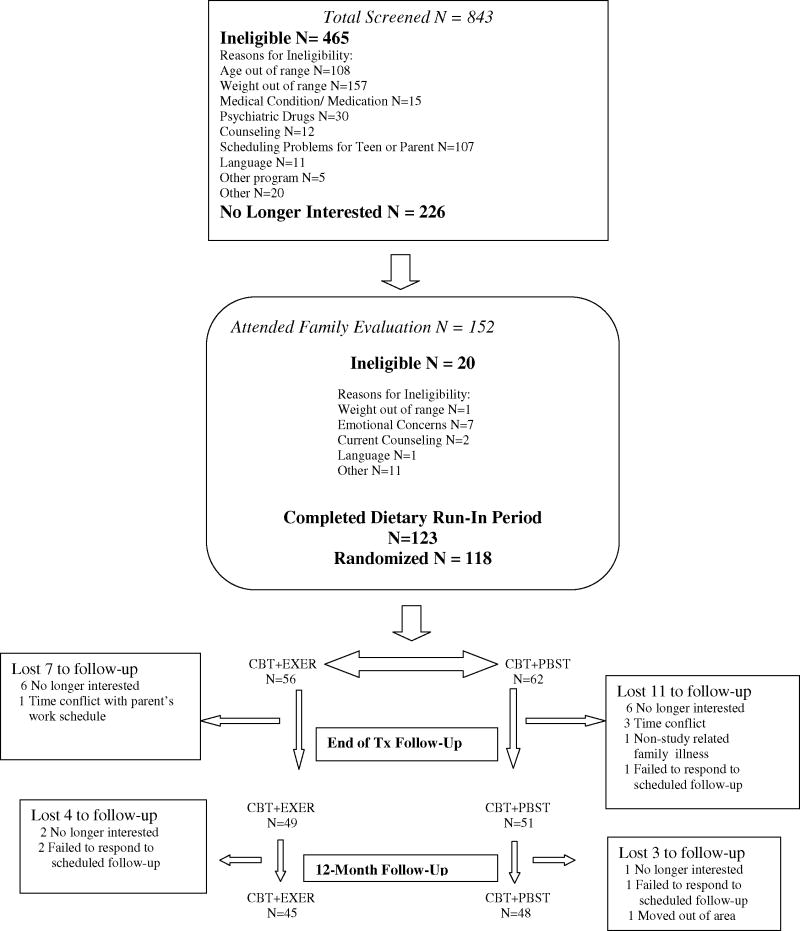
A total of 118 overweight adolescents were randomized to treatment (Figure; available at www.jpeds.com). Participants were recruited from local newspaper advertisements, as well as referrals from area pediatricians. Eligibility requirements included adolescents between the ages of 13 and 16 years; between 30 and 90% overweight as defined with reference to median body mass index for age and sex; at least one parent available to participate; and English speaking. Adolescents were excluded if they met criteria for major psychiatric disorder; were already enrolled in a weight loss program; or had a condition that prevented them from following the diet or physical activity prescription. Participants were offered monetary compensation for completing initial and follow-up evaluations. Dyads were reimbursed a total of $50 at the initial evaluation, $75 for completing the end of treatment evaluation, and $100 for the 1-year follow up. The study protocol was approved by the hospital institutional review board. Parents of all participants provided written informed consent and adolescents provided assent. Baseline data were collected between August 2003 and May 2006.
Figure 1.
Consort Diagram
Adolescents and their parents were randomized to one of two treatment conditions, occurring over six cohorts: cognitive behavioral treatment with aerobic exercise (CBT+EXER) or cognitive behavioral treatment with peer enhanced adventure therapy (CBT+PEAT). Participants were randomized after completing the baseline assessment battery and a one-week dietary record run-in period. An urn randomization procedure18 with percent over BMI (dichotomized as high vs. low) and sex (male vs. female) as covariates, was used to assign adolescents to treatment condition. Urn randomization assigns participants in a given subgroup to intervention conditions, but systematically biases the randomization in favor of balance between the intervention conditions. Although urn randomization reduces the probability of imbalance between groups and is less susceptible to experimenter bias, it may introduce the risk of violating assumptions of population models in analyses.19
Assessment of anthropometric and psychosocial measures was obtained at baseline, end of the 16-week intervention (end-of-treatment), and 12-months following randomization (12-month follow-up).
Common Treatment Components
Both group-based interventions included 16 one-hour weekly sessions, with parents and adolescents attending separate concurrent meetings, followed by four bi-weekly maintenance sessions. Adolescents were prescribed a balanced deficit diet (1400–1600 calories) and asked to gradually increase physical activity to an ideal of 60 minutes on most days of the week. Treatment groups consisted of didactic material and educational activities illustrating a range of behavioral topics – e.g. self-monitoring, motivation for weight loss, goal setting, stimulus control, and relapse prevention. Treatment groups were led by master’s and doctoral-level psychologists with experience in adolescent weight management and a registered dietician. The content of co-occurring parent meetings paralleled that for adolescents. Parents were also provided guidance regarding implementing family-level change and supporting positive eating and physical activity habits in their adolescents.
Following completion of the 20 group sessions, periodic (i.e. bi-monthly) activities were scheduled to encourage continued participant involvement with the study through the end of 12 months. Activities were offered to adolescents in both treatment conditions at separate times and included events such as apple picking, bowling, and miniature golf.
In addition to the CBT intervention described above, adolescents participated in weekly activity sessions.
Aerobic Exercise
Activities for the supervised exercise intervention included use of treadmills, stationary bicycles, as well as other aerobic activities selected by participants, including dance videos and brisk walking within the clinic setting. The format for each session followed the same sequence, beginning with a brief warm-up period, progressing to approximately 35 minutes of sustained physical activity, and ending with a wrap up period consisting of “cool down” and review of weekly physical activity goals.
Peer-Enhanced Adventure Therapy
The peer-based activity session consisted of an initial “warm-up” activity that included physical activity, followed by the primary challenge for the group, processing of the activity, and establishing weekly personal activity goals. Similar to Outward Bound adventure therapy, group activities consisted of both physical and mental challenges that were aimed at development of social skills, problem solving abilities, and self-confidence. A more detailed description of the adventure therapy component is provided elsewhere.17
Anthropometric Variables
Trained research assistants obtained each participant’s weight and height. Weight was measured on a balance beam scale in hospital gown without shoes. Height was measured with a stadiometer (Perspective Enterprises). Height and weight were used to calculate body mass index (BMI; kg/m2), standardized BMI score (z-BMI), as well as percent over BMI. The latter is defined as an adolescent’s percent above the 50th% BMI for age and sex and is calculated as {(teen BMI − BMI at 50th% for age and sex)/BMI at 50th%} × 100. Percent over BMI has demonstrated some advantage with regard to sensitivity to changes in BMI across a range of overweight20 and is easily interpreted. Waist circumference was assessed with participant wearing hospital gown, measuring horizontally from the right iliac crest around the abdomen at the umbilicus.
Self-Monitoring
Adolescent participants were asked to maintain weekly records to monitor daily dietary intake and physical activity. Self-monitoring records included food consumed, preparation and portion size, calorie estimates, fat grams and time of day for each item recorded. Number of minutes engaged in daily physical activity was also recorded. Of primary interest for this paper is the number of weekly self-monitoring records completed.
Physical Activity
Participation in physical activity was assessed at baseline and end of treatment using the ACTIVITYGRAM.21 Adolescents were prompted to provide information on three days of physical activity, including one weekend and two weekdays through a computer-assisted assessment. Information was obtained for participation in various activities in 30-minute increments throughout the day. Given that our primary interest was in voluntary activity, we include here only activity that occurred in the hour immediately before school (allowing for adolescents who may be choosing to walk to school) and the eight hours between the end of the school day and 11:00 p.m. during weekdays. The variable of primary interest was amount of time spent in moderate to vigorous physical activity (MVPA). The ACTIVITYGRAM has demonstrated reliability22 and validity.23
Self-Perception
The Self-Perception Profile for Adolescents (SPPA)24 is a widely used self-report measure of adolescents’ perceptions of competence in eight specific domains. Dimensions of physical appearance, close friendship, athletic competence, social acceptance, and global self-worth were included in the current study. Internal consistency for the individual subscales ranges from .74 to .92 and factor analysis indicates identification of a unique factor for each of the eight subscales.24 Additional assessment of physical self-worth was obtained through a brief scale, The Physical Self-Perception Profile for Children (PSPP-C).25, 26
Data Analysis
Primary outcomes were examined using mixed factor analysis of variance (ANOVA) conducted with all randomized participants (intent to treat; N = 118), with treatment condition as the between subjects factor and time (baseline, end of treatment, and 12 months) as the repeated measure. The study was powered to detect significant differences in percent overweight between the treatment conditions. With an anticipated N of 120, power was .82 to detect a difference as small as 5.4% in percent overweight between the groups, or about 1/3 SD. Intent to treat analyses assumed return to baseline values for non-completers. Secondary analyses included mixed factor ANOVA on participants available through the 12-month evaluation (completers; N=93). Given the divergence of perspectives regarding appropriate measurement of change in weight status in pediatric samples,20 multiple outcomes were evaluated, including absolute weight, absolute body mass index (BMI), z-BMI, and percent over BMI. Changes in waist circumference were also examined. Mixed factor ANOVA was also conducted to evaluate changes in MVPA from baseline to end of treatment. Multivariate analysis of variance (MANOVA) on completers was conducted on dimensions of self-concept from the SPPA and the Physical Self Worth Scale to examine changes in dimensions of self-concept over time. Given the theoretical relationship among subscales, MANOVA was conducted first to decrease the risk of Type I error and account for the correlation among dependent variables. Significant MANOVA findings were followed by univariate ANOVA. First order correlations and hierarchical regression analyses were conducted to evaluate the contribution of attendance and completion of diet records to BMI change.
Results
Participant demographic and baseline weight status data are presented in Table I. There were no significant differences between adolescents randomized to the two treatment conditions on baseline variables of body mass index, percent over BMI, or demographics.
Table 1.
Sample Baseline Characteristics
| Total Sample (n=118) | CBT + EXER (n=56) | CBT + PEAT (n=62) | |
|---|---|---|---|
| Age (months) | 171.92 (12.19) | 170.23 (11.1) | 173.44 (12.99) |
| Sex | Female = 68% | Female = 69% | Female = 66% |
| Race | |||
| Caucasian | 92 (76%) | 46 (82.1%) | 46 (72.2%) |
| African American | 16 (13.6%) | 6 (10.7%) | 10 (16.1%) |
| Other/Multiracial | 10 (8.3%) | 4 (7.1%) | 6 (9.7%) |
| Ethnicity | |||
| Non-Latino | 107 (90.7%) | 52 (92.9%) | 55 (88.7%) |
| Latino | 11 (9.3%) | 4 (7.1%) | 7 (11.3%) |
| Weight (lbs) | 187.39 (30.91) | 187.78 (31.17) | 187.04 (30.91) |
| Height (in) | 64.66 (3.24) | 64.79 (3.27) | 64.54 (3.27) |
| BMI | 31.41 (3.33) | 31.33 (3.1) | 31.49 (3.55) |
| z-BMI | 1.62 (.38) | 1.64 (.41) | 1.63 (.40) |
| Percent over BMI | 161.22 (16.79) | 162.12 (18.34) | 161.21 (17.80) |
| Waist Circumference | 103.51 (9.39) | 103.04(9.20) | 103.94(9.61) |
One hundred (85%) of the 118 participants randomized to treatment conditions completed the end of treatment assessment and 93 (79%) were available for 12-month follow-up. Participants in both treatment conditions who completed the 12-month evaluation did not differ with regard to the number of treatment sessions attended, with those randomized to CBT+PEAT as well as CBT+EXER attending an average of 83% of sessions.
Participants were compared on a number of weight status measures including absolute weight, BMI, z-BMI and percent over BMI, as well as waist circumference, to evaluate treatment outcomes. A summary of findings for intent to treat analysis is presented in Table II. Results for all outcome measures and for both intent to treat and completer analyses converged in demonstrating significant reductions over time, with no significant group by time interactions observed. Intent to treat analyses indicated significant decreases in BMI (p<.01), z-BMI (p<.01), percent over BMI (p<.01), as well as waist circumference (p<.01). The same pattern of results was observed in completer analyses, with significant reductions over time in each measure of weight status. Follow-up analyses indicated that significant changes in BMI, percent over BMI, z-BMI, and waist circumference were accounted for primarily by reductions from baseline to end of treatment. Although significant increases in BMI and z-BMI were observed between end of treatment and 12-months, the follow-up values continued to be significantly reduced from baseline.
Table 2.
Intent to Treat Analyses for Weight Related Outcomes (N=118)
| CBT+PEAT | CBT+EXER | |||||
|---|---|---|---|---|---|---|
| Baseline | End of Tx | 12 Month | Baseline | End of Tx | 12 Month | |
| Absolute Weight | 187.04 (30.91) | 179.73a (30.57) | 183.67b (29.45) | 187.78 (31.17) | 181.69a (32.31) | 187.74b (34.82) |
| BMI | 31.49 (3.54) | 29.99a (3.78) | 30.31bc (3.91) | 31.33 (3.10) | 30.02a (3.41) | 30.58bc (3.77) |
| z-BMI | 1.63 (.40) | 1.42a (.47) | 1.46c (.50) | 1.61 (.35) | 1.45a (.46) | 1.50c (.52) |
| Percent overBMI | 161.21 (17.80) | 151.85a (18.77) | 151.45c (19.56) | 161.23 (15.75) | 152.77a (17.10) | 153.53c (18.16) |
| Waist Circumference | 103.94 (9.61) | 100.99a (10.62) | 101.14c (10.66) | 103.04 (9.20) | 100.16a (10.36) | 101.18c (10.72) |
BMI = Body Mass Index. Z-BMI = standardized BMI score.
p<.01 baseline to end of treatment
p<.01 end of treatment to 12 months
p<.01 baseline to 12 months
Mixed factor analysis of variance was conducted on average daily minutes of MVPA during the 3-day period. There were no significant changes in the amount of MVPA reported over time, F(1,85) =.66 and no significant time by group interaction, F(1,85) =.15.
Adolescents randomized to both treatment conditions demonstrated significant improvements in self-concept over time (p<.01), with no significant differences observed between groups. Univariate tests indicated significant improvements on dimensions of global self-concept (p<.05), physical appearance (p<.01), social acceptance (p<.01), and physical self-worth (p<.01). Follow-up tests indicated that improvements on dimensions of global self-concept, physical appearance, and physical self-worth occurred during active treatment and were maintained at 12-month follow-up, and changes in social acceptance were observed only through the end of treatment. Improvements in global self-worth and physical appearance related self-worth were both related to significant reductions in BMI at the end of treatment, r=−.25 and r=−.28, respectively.
Analyses were conducted to determine the extent to which measures of treatment adherence, including attendance and completion of self-monitoring logs, were related to weight outcomes for completers. Percent of group sessions attended and records completed were highly correlated, r= .69, p<.01. The relationship between end of treatment BMI reduction and number of weekly records completed was significant across the sample, r=−.41, p<.01. This relationship held for participants assigned to CBT+EXER, r=−.53, p<.01, as well as those randomized to CBT+PEAT, r=−.37, p<.01. Evaluating predictors of BMI change at end of treatment, adherence was added as a final step in hierarchical regression analyses, following group status, demographic variables, and baseline BMI. Adherence was the only significant step in the model, with total R2 = .28 (Table III).
Table 3.
Hierarchical Linear Regression Analysis Predicting BMI Change at 16 Weeks
| Predictor | β | t | R2 |
|---|---|---|---|
| Step 1: | 0.01 | ||
| Group | 0.107 | 1.06 | |
| Step 2: | 0.01 | ||
| Age at Start of Program | 0.04 | 0.35 | |
| Sex | 0.03 | −0.27 | |
| Ethnicity | −0.03 | −0.29 | |
| Step 3: | 0.02 | ||
| Baseline BMI | −0.07 | −0.64 | |
| Step 4: | 0.28 | ||
| % Diet Records Completed | −0.36± | −3.40 | |
| % Group Sessions Attended | −0.24* | −2.38 |
p <.05
p <.01
Discussion
BMI reductions in the current study were comparable with those observed in a small 10- week trial comparing CBT with a control condition among overweight adolescents,15 and to findings based on prescription of a reduced glycemic index diet for obese adolescents.27 A lifestyle intervention that reported superior outcomes with adolescents required greater weekly time commitment combined with a longer active intervention phase.28 Thus, the current study adds to an increasing body of evidence demonstrating significant short-term changes in weight status in adolescent samples associated with lifestyle interventions. Moreover, the findings are consistent with a recent review suggesting that integrated interventions that include attention to diet, physical activity, and behavioral treatment are promising weight control interventions and superior to no treatment.29
Of note, although participation in weekly supervised activity was a key component of both treatment conditions, neither group of adolescents increased their participation in leisure time moderate to vigorous physical activity following the intervention. These findings suggest that participating in structured activity as a component of treatment did not result in adolescents electing increased involvement in physical activity on their own. Although planning for physical activity involvement outside of and following the intervention was a treatment focus, it appears that these efforts were not effective. Given that assessment of physical activity was conducted at the end of the intervention, it is possible that an increase in activity during treatment was not captured. Regardless, it is critical for future research to identify strategies for generalizing adolescent physical activity involvement beyond the scope of intervention.
Findings related to self-concept mirror those observed for weight status. Despite one treatment condition (CTB+PEAT) being designed to address the construct of self-concept, results indicate that adolescents randomized to both treatment conditions demonstrated significant improvements on dimensions of global self-concept, physical appearance, and physical self-worth. Furthermore, these differences were observed at the completion of active treatment and maintained at 12-month follow-up. It is possible that the structure of the group supervised exercise sessions in CBT+EXER served to unknowingly facilitate informal processes of group cohesion and support among the participating teens. Additionally, improvements in global self-worth and physical appearance related self-worth during the course of treatment were related to greater reductions in BMI. Although these data do not allow for interpretation of directionality, they clearly support previous studies indicating a relationship between weight status changes and improvement in self-concept.30
Weekly attendance and completion of diet records contributed significantly to BMI reduction during the course of the active intervention, above and beyond demographic variables and baseline BMI. These findings are consistent with other pediatric studies documenting a relationship between weight loss and self-monitoring in pediatric samples.31–33 It is noteworthy that the measure of dietary recording included here focused on whether or not a diet record was completed, without assessment of accuracy, suggesting that the process of recording may be in and of itself beneficial to adolescents. This is consistent with recent pediatric weight control interventions demonstrating a relationship between frequency of self-monitoring and change in weight-related outcomes.32
Taken together, these findings suggest that self-monitoring of diet and physical activity is key to weight control outcomes for adolescents. This research also indicates that there is considerable room for improvement with regard to enhancing the frequency with which adolescents monitor diet and physical activity. Future weight control interventions with adolescents would be well focused on identifying innovative strategies to enhance self-monitoring.
A number of limitations need to be considered when interpreting findings from the current study. First, the study did not include a no-treatment control and length of follow-up is limited to 12 months. Second, measures utilized are limited in a couple of ways: Even though we included a measure of self-reported physical activity, the study would have benefited from a more objective assessment of physical activity (i.e., accelerometer) and assessment at 12-month follow-up. There are additional challenges to measuring physical activity in adolescents, including aiming to better understand the seasonal variations in physical activity. Finally, the measure of adherence was limited, involving assessment only of quantity of monitoring records completed, and not quality of recording.
A number of directions are suggested for future research efforts. First, our findings highlight the potential utility of novel approaches for both increasing physical activity, as well as enhancing adherence to key behavioral strategies, such as self-monitoring. A second direction is the need for studies that examine the extent to which subgroups of adolescents may respond better to one or another intervention. Finally, of high importance is translating key components of behavioral weight control interventions for implementation in “real world” settings, moving to effectiveness studies that can serve to inform clinical practice.34
The authors would like to thank Holly Favell Gray, Donald Morse, and Patrick Cozzolino for their tremendous dedication and tireless efforts on this study.
Acknowledgments
Supported by the National Institute of Diabetes and Digestive and Kidney Diseases (grant R01DK062916 to E.J.) and the National Institutes of Health and the National Heart, Lung, and Blood Institute (grant K23HL069987 to ELR).
Footnotes
Clinical Trial #: NCT00285558
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 2.Cruz ML, Shaibi GQ, Weigensberg MJ, Spruijt-Metz D, Ball GD, Goran MI. Pediatric obesity and insulin resistance: chronic disease risk and implications for treatment and prevention beyond body weight modification. Annual Reviews in Nutrition. 2005;25:435–68. doi: 10.1146/annurev.nutr.25.050304.092625. [DOI] [PubMed] [Google Scholar]
- 3.Daniels SR. The consequences of childhood overweight and obesity. Future of Child. 2006;16:47–67. doi: 10.1353/foc.2006.0004. [DOI] [PubMed] [Google Scholar]
- 4.Hannon TS, Rao G, Arslanian SA. Childhood obesity and type 2 diabetes mellitus. Pediatrics. 2005;116:473–80. doi: 10.1542/peds.2004-2536. [DOI] [PubMed] [Google Scholar]
- 5.Nathan BM, Moran A. Metabolic complications of obesity in childhood and adolescence: more than just diabetes. Current Opinions in Endocrinology, Diabetes & Obesity. 2008;15:21–9. doi: 10.1097/MED.0b013e3282f43d19. [DOI] [PubMed] [Google Scholar]
- 6.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9:474–88. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 7.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 8.Fallon EM, Tanofsky-Kraff M, Norman AC, McDuffie JR, Taylor ED, Cohen ML, et al. Health-related quality of life in overweight and nonoverweight black and white adolescents. J Pediatr. 2005;147:443–50. doi: 10.1016/j.jpeds.2005.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–9. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 10.Wardle J, Cooke L. The impact of obesity on psychological well-being. Best Practice and Research Clinical Endocrinology and Metabolism. 2005;19:421–40. doi: 10.1016/j.beem.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Pearce MJ, Boergers J, Prinstein MJ. Adolescent obesity, overt and relational peer victimization, and romantic relationships. Obes Res. 2002;10:386–93. doi: 10.1038/oby.2002.53. [DOI] [PubMed] [Google Scholar]
- 12.Jelalian E, Saelens BE. Empirically supported treatments in pediatric psychology: pediatric obesity. J Pediatr Psychol. 1999;24:223–48. doi: 10.1093/jpepsy/24.3.223. [DOI] [PubMed] [Google Scholar]
- 13.Wilfley DE, Tibbs TL, Van Buren DJ, Reach KP, Walker MS, Epstein LH. Lifestyle interventions in the treatment of childhood overweight: a meta-analytic review of randomized controlled trials. Health Psychol. 2007;26:521–32. doi: 10.1037/0278-6133.26.5.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsiros MD, Sinn N, Coates AM, Howe PR, Buckley JD. Treatment of adolescent overweight and obesity. Eur J Pediatr. 2008;167:9–16. doi: 10.1007/s00431-007-0575-z. [DOI] [PubMed] [Google Scholar]
- 15.Tsiros MD, Sinn N, Brennan L, Coates AM, Walkley JW, Petkov J, et al. Cognitive behavioral therapy improves diet and body composition in overweight and obese adolescents. Am J Clin Nutr. 2008;87:1134–40. doi: 10.1093/ajcn/87.5.1134. [DOI] [PubMed] [Google Scholar]
- 16.Strauss RS, Rodzilsky D, Burack G, Colin M. Psychosocial correlates of physical activity in healthy children. Arch Pediatr Adolesc Med. 2001;155:897–902. doi: 10.1001/archpedi.155.8.897. [DOI] [PubMed] [Google Scholar]
- 17.Jelalian E, Mehlenbeck R, Lloyd-Richardson EE, Birmaher V, Wing RR. ‘Adventure therapy’ combined with cognitive-behavioral treatment for overweight adolescents. Int J Obes (Lond) 2006;30:31–9. doi: 10.1038/sj.ijo.0803069. [DOI] [PubMed] [Google Scholar]
- 18.Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Suppl. 1994;12:70–5. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- 19.Hedden SL, Woolson RF, Malcolm RJ. Randomization in substance abuse clinical trials. Subst Abuse Treat Prev Policy. 2006;1:6. doi: 10.1186/1747-597X-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paluch RA, Epstein LH, Roemmich JN. Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. Am J Hum Biol. 2007;19:487–94. doi: 10.1002/ajhb.20608. [DOI] [PubMed] [Google Scholar]
- 21.Welk GJ, Dzewaltowski DA, Ryan GJ, Sepulvedajowers EM, Hill JL. Convergent validity of the previous day physical activity recall and the activitygram assessment. Medicine and Science in Sports and Exercise. 2001;33:s144. [Google Scholar]
- 22.Treuth MS, Sherwood NE, Butte NF, McClanahan B, Obarzanek E, Zhou A, et al. Validity and reliability of activity measures in African-American girls for GEMS. Med Sci Sports Exerc. 2003;35:532–9. doi: 10.1249/01.MSS.0000053702.03884.3F. [DOI] [PubMed] [Google Scholar]
- 23.Welk GJ, Dzewaltowski DA, Hill JL. Comparison of the computerized ACTIVITYGRAM instrument and the previous day physical activity recall for assessing physical activity in children. Res Q Exerc Sport. 2004;75:370–80. doi: 10.1080/02701367.2004.10609170. [DOI] [PubMed] [Google Scholar]
- 24.Harter S. Manual for the Self-Perception Profile for Adolescents. Denver, CO: University of Denver Department of Psychology; 1988. [Google Scholar]
- 25.Whitehead JR. A study of children’s physical self-perceptions using an adapted physical self-perception profile questionnaire. Pediatric Exercise Science. 1995;7:132–51. [Google Scholar]
- 26.Eklund RC, Whitehead JR, Welk GJ. Validity of the children and youth physical self-perception profile: a confirmatory factor analysis. Research Quarterly for Exercise and Sport. 1997;68:249–56. doi: 10.1080/02701367.1997.10608004. [DOI] [PubMed] [Google Scholar]
- 27.Ebbeling CB, Leidig MM, Sinclair KB, Hangen JP, Ludwig DS. A reduced-glycemic load diet in the treatment of adolescent obesity. Arch Pediatr Adolesc Med. 2003;157:773–9. doi: 10.1001/archpedi.157.8.773. [DOI] [PubMed] [Google Scholar]
- 28.Savoye M, Berry D, Dziura J, Shaw M, Serrecchia JB, Barbetta G, et al. Anthropometric and psychosocial changes in obese adolescents enrolled in a Weight Management Program. J Am Diet Assoc. 2005;105:364–70. doi: 10.1016/j.jada.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 29.Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury vA, O’Malley C, Strolk RP, et al. Art. No.: CD001872. 1. 2009. Interventions for treating obesity in children. [DOI] [PubMed] [Google Scholar]
- 30.Lowry KW, Sallinen BJ, Janicke DM. The effects of weight management programs on self-esteem in pediatric overweight populations. Journal of Pediatric Psychology. 2007;32:1179–95. doi: 10.1093/jpepsy/jsm048. [DOI] [PubMed] [Google Scholar]
- 31.Kirschenbaum DS, Germann JN, Rich BH. Treatment of morbid obesity in low-income adolescents: effects of parental self-monitoring. Obesity Research. 2005;13:1527–9. doi: 10.1038/oby.2005.187. [DOI] [PubMed] [Google Scholar]
- 32.Germann JN, Kirschenbaum DS, Rich BH. Child and parental self-monitoring as determinants of success in the treatment of morbid obesity in low-income minority children. J Pediatr Psychol. 2007;32:111–21. doi: 10.1093/jpepsy/jsl007. [DOI] [PubMed] [Google Scholar]
- 33.Saelens BE, McGrath AM. Self-monitoring adherence and adolescent weight control efficacy. Children’s Health Care. 2003;32:137–52. [Google Scholar]
- 34.Robinson TN. Treating pediatric obesity: generating the evidence. Arch Pediatr Adolesc Med. 2008;162:1191–2. doi: 10.1001/archpedi.162.12.1191. [DOI] [PubMed] [Google Scholar]